Abstract
Hydrogen sulfide (H2S), a gas with the characteristic odor of rotten eggs, is known for its toxicity and as an environmental hazard, inhibition of mitochondrial respiration resulting from blockade of cytochrome c oxidase being the main toxic mechanism. Recently, however, H2S has been recognized as a signaling molecule of the cardiovascular, inflammatory and nervous systems, and therefore, alongside nitric oxide and carbon monoxide, is referred to as the third endogenous gaseous transmitter. Inhalation of gaseous H2S as well as administration of inhibitors of its endogenous production and compounds that donate H2S have been studied in various models of shock. Based on the concept that multiorgan failure secondary to shock, inflammation and sepsis may represent an adaptive hypometabolic reponse to preserve ATP homoeostasis, particular interest has focused on the induction of a hibernation-like suspended animation with H2S. It must be underscored that currently only a limited number of data are available from clinically relevant large animal models. Moreover, several crucial issues warrant further investigation before the clinical application of this concept. First, the impact of hypothermia for any H2S-related organ protection remains a matter of debate. Second, similar to the friend and foe character of nitric oxide, no definitive conclusions can be made as to whether H2S exerts proinflammatory or anti-inflammatory properties. Finally, in addition to the question of dosing and timing (for example, bolus administration versus continuous intravenous infusion), the preferred route of H2S administration remains to be settled – that is, inhaling gaseous H2S versus intra-venous administration of injectable H2S preparations or H2S donors. To date, therefore, while H2S-induced suspended animation in humans may still be referred to as science fiction, there is ample promising preclinical data that this approach is a fascinating new therapeutic perspective for the management of shock states that merits further investigation.
Similar content being viewed by others
Introduction
Hydrogen sulfide (H2S), a colorless, flammable and water-soluble gas with the characteristic odor of rotten eggs, has been known for decades because of its toxicity and as an environmental hazard [1, 2]. Inhibition of mitochondrial respiration – more potent than that of cyanide [3] – resulting from blockade of cytochrome c oxidase is the main mechanism of H2S toxicity [4, 5]. During recent years, however, H2S has been recognized as an important signaling molecule of the cardiovascular system, the inflammatory system and the nervous system. Alongside nitric oxide (NO) and carbon monoxide, therefore, H2S is now known as the third endogenous gaseotransmitter [1, 6].
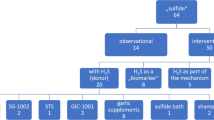
Since H2S is a small ubiquitous gaseous diffusible molecule, its putative interest for intensive care research is obvious. Consequently, inhibitors of its endogenous production as well as compounds that donate H2S have been studied in various models of shock resulting from hemorrhage [7–9], ischemia/reperfusion [10–18], endotoxemia [19–21], bacterial sepsis [22–25] and nonmicrobial inflammation [26–29] – which, however, yielded rather controversial data with respect to the proinflammatory or anti-inflammatory properties of H2S. The present article reviews the current literature on the therapeutic potential of H2S, with a special focus on clinically relevant studies in – if available – large animal models.
Biological chemistry
In mammals, H2S is synthesized from the sulfur-containing amino acid L-cysteine by either cystathionine-β-synthase or cystathionine-γ-lyase, both using pyridoxal 5'-phosphate (vitamin B6) as a cofactor [30–32]. This synthesis results in low micromolar H2S levels in the extracellular space, which can be rapidly consumed and degraded by various tissues. Similarly to NO and carbon monoxide, H2S is a lipophilic compound that easily permeates cell membranes without using specific transporters. Via direct inhibition, NO as well as carbon monoxide are involved in the regulation of cystathionine-β-synthase, but not cystathionine-γ-lyase, which can be activated by lipopolysaccharide (LPS) [1, 6].
There are three known pathways of H2S degradation: mitochondrial oxidation to thiosulfate, which is further converted to sulfite and sulfate; cytosolic methylation to dimethylsulfide; and sulfhemoglobin formation after binding to hemoglobin [6]. Similar to NO and carbon monoxide, H2S can also bind to hemoglobin – which was therefore termed the common sink for the three gaseous transmitters [33]. Consequently, saturation with one of these gases might lead to enhanced plasma concentrations and, subsequently, to biological effects of the other gases [1]. Table 1 summarizes the physicochemistry of H2S in mammalian tissues.
Mechanisms of H2S
H2S exerts its effects in biological systems through a variety of interrelated mechanisms (for a review see [1]). Our current knowledge of the biology of H2S predominantly stems from in vitro studies in various cell and isolated organ systems, either using cystathionine-γ-lyase inhibitors such as D,L-propargylglycine (PAG) and β-cyanoalanine, or administration of H2S gas or H2S donors such as sodium disulfide (Na2S) and sodium hydrogen sulfide (NaHS). While high (high micromolar to millimolar) levels are invariably accompanied with cytotoxic effects [34] – which result from free radical generation, glutathione deletion, intracellular iron release and pro-apoptotic action through both the death receptor and mitochondrial pathways [35] – lower (low micromolar) levels have been shown to exert either cytoprotective (antinecrotic or antiapoptotic) effects [10–13, 36] or proapoptotic properties [37–39], depending on the cell type and on the experimental conditions.
Cytochrome c oxidase, a component of the oxidative phosphorylation machinery within the mitochondrium, is one intracellular target of H2S [4, 5]. Both the toxic effects of H2S as well as the induction of a so-called "suspended animation" [40, 41] are referred to in this inhibition of mitochondrial respiration [42, 43], and thus may represent a possible mechanism for the regulation of cellular oxygen consumption [44].
Activation of potassium-dependent ATP channels is another major mechanism of H2S, which in turn causes vasodilation, preconditioning against ischemia/reperfusion injury and myocardial protection [45]. Various findings support this concept [1, 6, 46]: potassium-dependent ATP channel blockers (sulfonylurea derivates – for example, glibenclamide) attenuated the H2S-induced vasodilation both in vivo and in vitro [47, 48], and stimulation of potassium-dependent ATP channels was demonstrated in the myocardium, pancreatic β cells, neurons and the carotid sinus [6]. Moreover, glibenclamide reversed the otherwise marked Na2S-related increase of the hepatic arterial buffer response capacity that counteracts reduction of portal venous flow, whereas PAG decreased this compensatory mechanism [49].
An endothelium-dependent effect seems to contribute to these vasodilatory properties: in human endothelial cells, H2S caused direct inhibition of the angiotensin-converting enzyme [50], and, finally, H2S can enhance the vasorelaxation induced by NO [51, 52]. The interaction between H2S and NO with respect to vascular actions is, however, fairly complex: low H2S concentrations may cause vasoconstriction as a result of an attenuated vasorelaxant effect of NO due to scavenging of endothelial NO and formation of an inactive nitrosothiol [52–54]. The local oxygen concentration apparently assumes importance for the vasomotor properties of H2S as well [55]: while H2S had vasodilator properties at 40 μM oxygen concentration (that is, an oxygen partial pressure of approximately 30 mmHg), it exerted vaso-constrictor effects at a 200 μM oxygen concentration (that is, aan oxygen partial pressure of approximately 150 mmHg) [56]. Finally, the H2S-related inhibition of oxidative phosphorylation also contributes to the vasodilatation [57].
Owing to its SH group that allows reduction of disulfide bonds and radical scavenging, H2S also exerts biological effects as an antioxidant [9], in particular as an endogenous peroxynitrite scavenger [58], which is consistent with its cytoprotective effects in various cell-based experiments [59, 60]. In this context the effect of H2S on intracellular signal pathways assumes particular importance: in LPS-stimulated macrophages, pretreatment with physically dissolved gaseous H2S or the H2S-donor NaHS was affiliated with diminished activation of the nuclear transcription factor NF-κB and inhibition of the inducible isoform of the NO synthase. This effect coincided with increased expression of heme oxygenase-1, and co-incubation with carbon monoxide mimicked the cytoprotection exerted by H2S [61].
Conflicting data are available on the effects of H2S on other intracellular signal transduction pathways; for example, the mitogen-activated protein kinase pathway and the phosphatidyinositol-3-kinase/Akt pathway [20, 61–65]. Depending on the cell lines used, both inhibitory [20] and activating [36, 61, 64] effects on p38 mitogen-activated protein kinase were reported, whereas H2S seems not to affect the stress-activated protein kinase c-Jun N-terminal kinase [61, 65]. In contrast, activation of the extracellular signal-regulated kinase 1/2 pathway has been implicated in the H2S-related ischemic preconditioning [48], both its proinflammatory [63, 65] and anti-inflammatory [20, 61] effects, as well as in the induction of apoptosis [62]. While the influence of H2S on extracellular signal-regulated kinase seems to be rather comprehensible [25], studies exploring the effect on downstream pathways result in conflictive statements.
Jeong and colleagues reported that H2S enhances NO production and inducible NO synthase expression by potentiating IL-1β-induced NF-κB in vascular smooth muscle cells [63], which is consistent with the H2S-induced NF-κB activation and subsequent proinflammatory cytokine production in IFNγ-primed monocytes [65]. Nevertheless, any H2S effect on NF-κB and its transcription-regulated mediators (for example, inducible NO synthase, cytokines and apoptotic factors) may be cell-type dependent and stimulus dependent. In fact, in addition to the above-mentioned decreased NF-κB activation and inducible NO synthase expression in LPS-stimulated macrophages [61], H2S administration also attenuated inducible NO synthase expression, NO production, as well as TNFα secretion in microglia exposed to LPS [20].
In the context of these contradictory findings, the doses of the H2S donors administered may assume particular importance. Even the physiologically relevant concentrations [36, 64] might have to be reconsidered due to overestimation of basal H2S levels: murine plasma sulfide levels are reported between 10 and 34 μM [21, 22], and are increased up to 20 to 65 μM after endotoxin injection [21] or cecal ligation and puncture [22]. A reduction of plasma sulfide concentration from 50 μM to ~25 μM, finally, was reported in patients with coronary heart disease [1], whereas plasma sulfide levels increased from 44 to 150 μM in patients with sepsis [21]. It should be noted, however, that the distinct techniques used by various groups to determine sulfide levels may account for the marked variability in the baseline values reported. The various derivatization methods, which are inherent to the analytic procedures, are likely to liberate sulfide from its bound forms so that the exact amount of free and bioavailable sulfide may be lower than frequently reported [66]. In fact, Mitsuhashi and colleagues reported that the blood sulfite concentrations (that is, the product of mitochondrial sulfide oxidation) were 3.75 ± 0.88 μM only in patients with pneumonia (versus 1.23 ± 0.48 μM in healthy control individuals) [67]. Infusing 2.4 and 4.8 mg/kg/hour in anesthetized and mechanically ventilated pigs over 8 hours resulted in maximum blood sulfide levels of 2.0 and 3.5 μM, respectively (baseline levels 0.5 to 1.2 μM) in our experiments [16].
Metabolic effects of H2S: induction of suspended animation
Suspended animation is a hibernation-like metabolic status characterized by a marked yet reversible reduction of energy expenditure, which allows nonhibernating species to sustain environmental stress, such as extreme changes in temperature or oxygen deprivation [41, 68].
In landmark work, the Roth's group provided evidence that inhaled H2S can induce such a suspended animation [40, 41]: in awake mice, breathing 80 ppm H2S caused a dose-dependent reduction of both the respiratory rate and the heart rate as well as of oxygen uptake and carbon dioxide production, which was ultimately associated with a drop in body core temperature to levels ~2°C above ambient temperature [40]. All these effects were completely reversible after H2S washout, and thereafter animals presented with a totally normal behavior. A follow-up study confirmed these observations, and the authors demonstrated using telemetry and echocardiography that the bradycardia-related fall in cardiac output coincided with an unchanged stroke volume and blood pressure. These physiologic effects of inhaled H2S were present regardless of the body core temperature investigated (27°C and 35°C) [69].
It is noteworthy that anesthesia may at least partially blunt the myocardial effect of inhaled H2S. In mechanically ventilated mice instrumented with left ventricular pressure volume conductance catheters and assigned to 100 ppm inhaled H2S, we found that hypothermia alone (27°C) but not normothermic H2S inhalation (38°C) decreased the cardiac output due to a fall in heart rate, whereas both the stroke volume as well as the parameters of systolic and diastolic function remained unaffected (Table 2) [70]. Interestingly, inhaled H2S in combination with hypothermia, however, was concomitant with the least stimulation of oxygen flux induced by addition of cytochrome c during state 3 respiration with combined complex I and complex II substrates (Figure 1) [71]. Since stimulation by cytochrome c should not occur in intact mitochondria, this finding suggests better preservation of mitochondrial integrity under these conditions [72].
Cytochrome c-stimulated mitochondrial oxygen flux in livers from anesthetized and mechanically ventilated mice. Ratio of mitochondrial oxygen flux in homogenized livers from anesthetized and mechanically ventilated mice after addition in relation to before addition of cytochrome c. Since stimulation by cytochrome c should not occur in intact mitochondria, the smallest value (that is, a ratio close to 1.00) suggests preservation of mitochondrial integrity. Animals were subjected to inhaled hydrogen sulfide (H2S) (100 ppm over 5 hours) or vehicle gas during normothermia (38°C) and hypothermia (27°C) [63]. Data presented as mean ± standard deviation, n = 8 in each group. #P < 0.05 versus control, 38°C.
In good agreement with the concept that a controlled reduction in cellular energetic expenditure would allow maintenance of ATP homoeostasis [41] and thus of improving outcome during shock states due to preserved mitochondrial function [73, 74], the group of Roth and colleagues subsequently demonstrated that pretreatment with inhaled H2S (150 ppm) for only 20 minutes markedly prolonged survival without any apparent detrimental effects for mice exposed to otherwise lethal hypoxia (5% oxygen) [75] and for rats undergoing lethal hemorrhage (60% of the calculated blood volume over 40 minutes) [8]. It is noteworthy that in the latter study the protective effect was comparable when using either inhaled H2S or a single intravenous bolus of Na2S [75]: parenteral sulfide administration has a number of practical advantages (ease of administration, no need for inhalation delivery systems, no risk of exposure to personnel, no issues related of the characteristic odor of H2S gas) and, in particular, avoids the pulmonary irritant effects of inhaled H2S, which can be apparent even at low inspiratory gaseous concentrations [76]. Finally, it is noteworthy that hypothermia is not a prerequisite of H2S-related cytoprotection during hemorrhage: the H2S donor NaHS improved hemodynamics, attenuated metabolic acidosis, and reduced oxidative and nitrosative stress in rats subjected to controlled hemorrhage at a mean blood pressure of 40 mmHg (Figure 2) [9].
Hydrogen sulfide-related hemodynamic effects in rats subjected to hemorrhage and subsequent retransfusion. Time course of the difference in (a) mean blood pressure (ΔMAP) and (b) carotid blood flow (ΔCBF) in rats subjected to 60 minutes of hemorrhage (MAP 40 mmHg) and subsequent retransfusion of shed blood. Ten minutes prior to retransfusion, animals received vehicle (n = 11; open circles) or the hydrogen sulfide donor sodium hydrogen sulfide (bolus 0.2 mg/kg, n = 11; closed circles) [9]. Data presented as mean (standard deviation). #P < 0.05 versus controls.
The clinical relevance of murine models may be questioned because, due to their large surface area/mass ratio, rodents can rapidly drop their core temperature [77]. In fact, other authors failed to confirm the metabolic effect of inhaled H2S in anesthetized and mechanically ventilated piglets (body weight ~6 kg) or in H2S-sedated and spontaneously breathing sheep (body weight ~74 kg) exposed to up to 80 or 60 ppm H2S, respectively [78, 79]. These findings may be due to the dosing or timing of H2S, and are in contrast to recent data from our own group: in anesthetized and mechanically ventilated swine (body weight ~45 kg) that underwent transient thoracic aortic balloon occlusion, infusing the intravenous H2S donor Na2S over 10 hours reduced the heart rate and cardiac output without affecting the stroke volume, thereby reducing oxygen uptake and carbon dioxide production and, ultimately, core temperature [16]. The metabolic effect of H2S coincided with an attenuation of the early reperfusion-related hyperlactatemia – suggesting a reduced need for anaerobic ATP generation during the ischemia period – and an improved noradrenaline responsiveness, indicating both improved heart function and vasomotor response to catecholamine stimulation [16].
H2S-induced cytoprotection during ischemia–reperfusion
Deliberate hypothermia is a cornerstone of the standard procedures to facilitate neurological recovery after cardiac arrest and to improve postoperative organ function after cardiac and transplant surgery. Consequently, several authors investigated the therapeutic potential of H2S-induced suspended animation after ischemia–reperfusion injury – and H2S protected the lung [14], the liver [12], the kidney (Figure 3) [17, 80], and, in particular, the heart [10, 11, 13, 15, 18, 62, 81–83]. H2S administered prior to reperfusion therefore limited the infarct size and preserved left ventricular function in mice [10] and in swine [11].
Hydrogen sulfide attenuation of oxidative DNA damage in the kidney after organ ischemia–reperfusion. Oxidative DNA damage (tail moment in the alkaline version of the comet assay [89]) in kidney tissue biopsies prior to (left panel) and after 2 hours of organ ischemia and 8 hours of reperfusion (right panel) in control swine (n = 7; open box plots) and in animals treated with the hydrogen sulfide donor sodium disulfide (Na2S) (n = 8; grey box plots). Renal ischemia was induced by inflating the balloon of an intra-aortic catheter positioned at the renal artery orifices. Na2S infusion was infused before kidney ischemia (2 mg/kg/hour over 2 hours) as well as during the first 4 hours of reperfusion (1 mg/kg/hour) [72]. Data presented as median (quartiles, range). #P < 0.05 versus before ischemia, §P < 0.05 versus control.
While these findings were obtained without induction of hypothermia, preserved mitochondrial function documented by an increased complex I and complex II efficiency assumed major importance for the H2S-induced cytoprotection [10]. The important role of preserved mitochondrial integrity was further underscored by the fact that 5-hydroxydeconoate, which is referred to as a mitochondrial potassium-dependent ATP-channel blocker, abolished the anti-apoptotic effects of H2S [18]. Clearly, anti-inflammatory and anti-apoptotic effects also contributed to the improved postischemic myocardial function: treatment with H2S was associated with reduced myocardial myeloperoxidase activity and an absence of the increase in the IL-1β levels (that is, attenuated tissue inflammation [10, 18]), as well as complete inhibition of thrombin-induced leukocyte rolling, a parameter for leukocyte–endothelium interaction [10]. Moreover, the ischemia–reperfusion-induced activation of p38 mitogen-activated protein kinase, of c-Jun N-terminal kinase and of NF-κB was also attenuated by H2S [18]. Finally, H2S exerted anti-apoptotic effects as shown by reduced TUNEL staining [10, 11] and by expression of cleaved caspase-9 [18], caspase-3 [10, 11], poly-ADP-ribose-polymerase [11] and the cell death-inducing proto-oncogene c-fos [13].
Controversial role of H2S in animal models of inflammation
Despite the promising data mentioned above, it is still a matter of debate whether H2S is a metabolic mediator or a toxic gas [84] – particularly given the rather controversial findings on the immune function reported in various models of systemic inflammation. In fact, H2S exerted both marked proinflammatory effects [19, 21–25, 27, 85] and anti-inflammatory effects [9, 10, 18, 20, 28–30]. Studies using inhibitors of endogenous H2S production such as PAG demonstrated pro-nounced proinflammatory effects of H2S: PAG attenuated organ injury, blunted the increase of the proinflammatory cytokine and chemokine levels as well as the myeloperoxidase activity in the lung and liver, and abolished leukocyte activation and trafficking in LPS-induced endotoxemia [19, 21] or cecal ligation and puncture-induced sepsis [22–25, 86]. In good agreement with these findings, the H2S donor NaHS significantly aggravated this systemic inflammation [21–25, 86]. Although similar results were found during caerulin-induced pancreatitis [27, 87], the role of H2S during systemic inflammatory diseases is still a matter of debate. Zanardo and colleagues reported reduced leukocyte infiltration and edema formation using the air pouch and carrageenan-induced hindpaw edema model in rats injected with the H2S donors NaHS and Na2S [30]. Moreover, in mice with acute lung injury induced by combined burn and smoke levels, inhalation, a single Na2S bolus decreased tissue IL-1β increased IL-10 levels, and attenuated protein oxidation in the lung, which ultimately resulted in markedly prolonged survival [28].
Variable dosing and timing make it difficult to definitely conclude on the proinflammatory and/or anti-inflammatory effects of H2S: while the median sulfide lethal dose in rats has been described to be approximately 3 mg/kg intravenously [1], studies in the literature report on doses ranging from 0.05 to 5 mg/kg. In addition, there are only a small number of reports on continuous intravenous infusion rather than bolus administration. Finally, the role of the suspended animation-related hypothermia per se remains a matter of debate. While some studies report that spontanoues hypothermia and/or control of fever may worsen the outcome [88], other authors describe decreased inflammation [89] and improved survival after inducing hypothermia in sepsis [90].
We found in anesthetized and mechanically ventilated mice undergoing sham operation for surgical instrumentation that normothermic H2S (100 ppm) inhalation (38°C) over 5 hours and hypothermia (27°C) alone comparably attenuated the inflammatory chemokine release (monocyte chemotactic protein-1, macrophage inflammatory protein-2 and growth-related oncogen/keratinocyte-derived chemokine) in the lung tissue. While H2S did not affect the tissue concentrations of TNFα, combining hypothermia and inhaled H2S significantly decreased tissue IL-6 expression (Table 3) [91].
Conclusion
Based on the concept that multiorgan failure secondary to shock, inflammation and sepsis may actually be an adaptive hypometabolic reponse to preserve ATP homoeostasis [92] – such as has been demonstrated for the septic heart [93] – and thus represent one of the organism's strategies to survive under stress conditions, the interest of inducing a hibernation-like suspended animation with H2S is obvious. Investigations have currently progressed most for the treatment of myocardial ischemia [94]. It must be underscored, however, that only a relatively small proportion of the published studies was conducted in clinically relevant large animal models [11, 16, 95], and, furthermore, that the findings reported are controversial [16, 78, 79].
Moreover, several crucial issues warrant further investigation before the clinical application of this concept. First, the role of hypothermia for any suspended animation-related organ protection is well established [96], but its impact remains a matter of debate for H2S-related organ protection. Clearly, in the rodent studies [10, 12, 18, 28], any cytoprotective effect was apparent without a change in core body temperature, but localized metabolic effects cannot be excluded [10]. In addition, the role of any H2S-related hypothermia remains controversial in the context of systemic inflammation [88]. Second, similar to the friend and foe character of NO, no definitive conclusions can be made as to whether H2S exerts proinflammatory or anti-inflammatory properties [1, 6, 85]. Finally, in addition to the question of dosing and timing (for example, bolus administration versus continuous intravenous infusion), the preferred route of H2S administration remains to be settled: while inhaling gaseous H2S probably allows easily titrating target blood concentrations, it is well established that this method can also directly cause airway irritation [76].
While H2S-induced suspended animation in humans to date may still be referred to as science fiction, there are ample promising preclinical data that this approach is a fascinating new therapeutic perspective for the management of shock states that merits further investigation.
Note
This article is part of a review series on Gaseous Mediators, edited by Peter Radermacher.
Other articles in the series can be found online at http://www.ccforum.com/series/gaseous_mediators
Abbreviations
- H2S:
-
hydrogen sulfide
- IFN:
-
interferon
- IL:
-
interleukin
- LPS:
-
lipopolysaccharide
- Na2S:
-
sodium disulfide
- NaHS:
-
sodium hydrogen sulfide
- NF:
-
nuclear factor
- NO:
-
nitric oxide
- PAG:
-
D,L-propargylglycine
- TNF:
-
tumor necrosis factor
- TUNEL:
-
terminal deoxynucleotidyltransferase-mediated dUTP nick-end labeling.
References
Szabó C: Hydrogen sulphide and its therapeutic potential. Nat Rev Drug Discov 2007, 6: 917-935.
Beauchamp RO, Bus JS, Popp JA, Boreiko CJ, Andjelkovich DA: A critical review of the literature on hydrogen sulfide toxicity. Crit Rev Toxicol 1984, 13: 25-97.
Reiffenstein RJ, Hulbert WC, Roth SH: Toxicology of hydrogen sulfide. Annu Rev Pharmacol Toxicol 1992, 32: 109-134.
Khan AA, Schuler MM, Prior MG, Yong S, Coppock RW, Florence LZ, Lillie LE: Effects of hydrogen sulfide exposure on lung mitochondrial respiratory chain enzymes in the rat. Toxicol Appl Pharmacol 1990, 103: 482-490.
Dorman DC, Moulin FJM, McManus BE, Mahle KC, James RA, Struve MF: Cytochrome oxidase inhibition induced by acute hydrogen sulfide inhalation: correlation with tissue sulfide concentrations in the rat brain, liver, lung, and nasal epithelium. Toxicol Sci 2002, 65: 18-25.
Lowicka E, Beltowski J: Hydrogen sulfide (H 2 S) – the third gas of interest for pharmacologists. Pharmacol Rep 2007, 59: 4-24.
Mok YY, Atan MS, Yoke PC, Zhong JW, Bhatia M, Moochhala S, Moore PK: Role of hydrogen sulphide in haemorrhagic shock in the rat: protective effect of inhibitors of hydrogen sulphide biosynthesis. Br J Pharmacol 2004, 143: 881-889.
Morrison ML, Blackwood JE, Lockett SL, Iwata A, Winn RK, Roth MB: Surviving blood loss using hydrogen sulfide. J Trauma 2008, 65: 183-188.
Ganster F, Burban M, de la Bourdonnaye M, Fizanne L, Douay O, Mercat A, Calès P, Radermacher P, Henrion D, Asfar P, Meziani F: Intérêt d'un donneur de H 2 S (NaHS) dans le choc hémorragique chez le rat [abstract]. Réanimation 2009,18(Suppl 18):S45.
Elrod JW, Calvert JW, Morrison J, Doeller JE, Kraus DW, Tao L, Jiao X, Scalia R, Kiss L, Szabó C, Kimura H, Chow CW, Lefer DJ: Hydrogen sulfide attenuates myocardial ischemia–reperfusion injury by preservation of mitochondrial function. Proc Natl Acad Sci USA 2007, 104: 15560-15565.
Sodha NR, Clements RT, Feng J, Liu Y, Bianchi C, Horvath EM, Szabó C, Sellke FW: The effects of therapeutic sulfide on myocardial apoptosis in response to ischemia–reperfusion injury. Eur J Cardiothorac Surg 2008, 33: 906-913.
Jha S, Calvert JW, Duranski MR, Ramachandran A, Lefer DJ: Hydrogen sulfide attenuates hepatic ischemia–reperfusion injury: role of antioxidant and antiapoptotic signaling. Am J Physiol Heart Circ Physiol 2008, 295: H801-H806.
Zhu XY, Yan XH, Chen SJ: H 2 S protects myocardium against ischemia/reperfusion injury and its effect on c-Fos protein expression in rats. Sheng Li Xue Bao 2008, 60: 221-227.
Fu Z, Liu X, Geng B, Fang L, Tang C: Hydrogen sulfide protects rat lung from ischemia–reperfusion injury. Life Sci 2008, 82: 1196-1202.
Ji Y, Pang QF, Xu G, Wang L, Wang JK, Zeng YM: Exogenous hydrogen sulfide postconditioning protects isolated rat hearts against ischemia–reperfusion injury. Eur J Pharmacol 2008, 587: 1-7.
Simon F, Giudici R, Duy CN, Schelzig H, Öter S, Gröger M, Wachter U, Vogt J, Speit G, Szabó C, Radermacher P, Calzia E: Hemodynamic and metabolic effects of hydrogen sulfide during porcine ischemia/reperfusion injury. Shock 2008, 30: 359-364.
Tripatara P, Sa PN, Collino M, Gallicchio M, Kieswich J, Castiglia S, Benetti E, Stewart KN, Brown PA, Yaqoob MM, Fantozzi R, Thiemermann C: Generation of endogenous hydrogen sulfide by cystathionine-γ-lyase limits renal ischemia/reperfusion injury and dysfunction. Lab Invest 2008, 88: 1038-1048.
Sivarajah A, Collino M, Yasin M, Benetti E, Gallicchio M, Mazzon E, Cuzzocrea S, Fantozzi R, Thiemermann C: Antiapoptotic and anti-inflammatory effects of hydrogen sulfide in a rat model of regional myocardial I/R. Shock 2009, 31: 267-274.
Collin M, Anuar FB, Murch O, Bhatia M, Moore PK, Thiemermann C: Inhibition of endogenous hydrogen sulfide formation reduces the organ injury caused by endotoxemia. Br J Pharmacol 2005, 146: 498-505.
Hu LF, Wong PT, Moore PK, Bian JS: Hydrogen sulfide attenuates lipopolysaccharide-induced inflammation by inhibition of p38 mitogen-activated protein kinase in microglia. J Neurochem 2007, 100: 1121-1128.
Li L, Bhatia M, Zhu YZ, Zhu YC, Ramnath RD, Wang ZJ, Anuar FB, Whiteman M, Salto-Tellez M, Moore PK: Hydrogen sulfide is a novel mediator of lipopolysaccharide-induced inflammation in the mouse. FASEB J 2005, 19: 1196-1198.
Zhang H, Zhi L, Moore PK, Bhatia M: Role of hydrogen sulfide in cecal ligation and puncture-induced sepsis in the mouse. Am J Physiol Lung Cell Mol Physiol 2006, 290: L1193-L1201.
Zhang H, Zhi L, Moochhala SM, Moore PK, Bhatia M: Endogenous hydrogen sulfide regulates leukocyte trafficking in cecal ligation and puncture-induced sepsis. J Leukoc Biol 2007, 82: 894-905.
Zhang H, Zhi L, Moochhala S, Moore PK, Bhatia M: Hydrogen sulfide acts as an inflammatory mediator in cecal ligation and puncture-induced sepsis in mice by upregulating the production of cytokines and chemokines via NF-κB. Am J Physiol Lung Cell Mol Physiol 2007, 292: L960-L971.
Zhang H, Moochhala SM, Bhatia M: Endogenous hydrogen sulfide regulates inflammatory response by activating the ERK pathway in polymicrobial sepsis. J Immunol 2008, 181: 4320-4331.
Sidhapuriwala J, Li L, Sparatore A, Bhatia M, Moore PK: Effect of S-diclofenac, a novel hydrogen sulfide releasing derivative, on carrageenan-induced hindpaw oedema formation in the rat. Eur J Pharmacol 2007, 569: 149-154.
Tamizhselvi R, Moore PK, Bhatia M: Inhibition of hydrogen sulfide synthesis attenuates chemokine production and protects mice against acute pancreatitis and associated lung injury. Pancreas 2008, 36: e24-e31.
Esechie A, Kiss L, Olah G, Horvath EM, Hawkins H, Szabó C, Traber DL: Protective effect of hydrogen sulfide in a murine model of acute lung injury induced by combined burn and smoke inhalation. Clin Sci (Lond) 2008, 115: 91-97.
Li T, Zhao B, Wang C, Wang H, Liu Z, Li W, Jin H, Tang CS, Du J: Regulatory effects of hydrogen sulfide on IL-6, IL-8 and IL-10 levels in the plasma and pulmonary tssue of rats with acute lung injury. Exp Biol Med (Maywood) 2008, 233: 1081-1087.
Zanardo RC, Brancaleone V, Distrutti E, Fiorucci S, Cirino G, Wallace JL: Hydrogen sulfide is an endogenous modulator of leukocyte-mediated inflammation. FASEB J 2006, 20: 2118-2120.
Fiorucci S, Distrutti E, Cirino G, Wallace JL: The emerging roles of hydrogen sulfide in the gastrointestinal tract and liver. Gastroenterology 2006, 131: 259-271.
Miles EW, Kraus JP: Cystathionine-β-synthase: structure, function, regulation, and location of homocystinuria-causing mutations. J Biol Chem 2004, 279: 29871-29874.
Suematsu M: Quartet signal transducers in gas biology. Antioxid Redox Signal 2003, 5: 435-437.
Cheung NS, Peng ZF, Chen MJ, Moore PK, Whiteman M: Hydrogen sulfide induced neuronal death occurs via glutamate receptor and is associated with calpain activation and lysosomal rupture in mouse primary cortical neurons. Neuropharmacology 2007, 53: 505-514.
Yang G, Yang W, Wu L, Wang R: H 2 S, endoplasmic reticulum stress, and apoptosis of insulin-secreting beta cells. J Biol Chem 2007, 282: 16567-16576.
Rose P, Moore PK, Ming SH, Nam OC, Armstrong JS, Whiteman M: Hydrogen sulfide protects colon cancer cells from chemo-preventative agent β-phenylethyl isothiocyanate induced apoptosis. World J Gastroenterol 2005, 11: 3990-3997.
Cao Y, Adhikari S, Ang AD, Moore PK, Bhatia M: Mechanism of induction of pancreatic acinar cell apoptosis by hydrogen sulfide. Am J Physiol Cell Physiol 2006, 291: C503-C510.
Baskar R, Li L, Moore PK: Hydrogen sulfide-induces DNA damage and changes in apoptotic gene expression in human lung fibroblast cells. FASEB J 2007, 21: 247-255.
Adhikari S, Bhatia M: H 2 S-induced pancreatic acinar cell apoptosis is mediated via JNK and p38 MAP kinase. J Cell Mol Med 2008, 12: 1374-1384.
Blackstone E, Morrison M, Roth MB: H 2 S induces a suspended animation-like state in mice. Science 2005, 308: 518.
Roth MB, Nystul T: Buying time in suspended animation. Sci Am 2005, 292: 48-55.
Hill BC, Woon TC, Nicholls P, Peterson J, Greenwood C, Thomson AJ: Interactions of sulphide and other ligands with cytochrome c oxidase. An electron-paramagnetic-resonance study. Biochem J 1984, 224: 591-600.
Cooper CE, Brown GC: The inhibition of mitochondrial cytochrome c oxidase by the gases carbon monoxide, nitric oxide, hydrogen cyanide and hydrogen sulfide: chemical mechanism and physiological significance. J Bioenerg Biomembr 2008, 40: 533-539.
Leschelle X, Goubern M, Andriamihaja M, Blottiere HM, Couplan E, Gonzalez-Barroso MD, Petit C, Pagniez A, Chaumontet C, Mignotte B, Bouillaud F, Blachier F: Adaptative metabolic response of human colonic epithelial cells to the adverse effects of the luminal compound sulfide. Biochim Biophys Acta 2005, 1725: 201-212.
Zhang Z, Huang H, Liu P, Tang C, Wang J: Hydrogen sulfide contributes to cardioprotection during ischemia–reperfusion injury by opening K ATP channels. Can J Physiol Pharmacol 2007, 85: 1248-1253.
Pryor WA, Houk KN, Foote CS, Fukuto JM, Ignarro LJ, Squadrito GL, Davies KJ: Free radical biology and medicine: it's a gas, man! Am J Physiol Regul Integr Comp Physiol 2006, 291: R491-R511.
Tang G, Wu L, Liang W, Wang R: Direct stimulation of K ATP channels by exogenous and endogenous hydrogen sulfide in vascular smooth muscle cells. Mol Pharmacol 2005, 68: 1757-1764.
Zhao W, Zhang J, Lu Y, Wang R: The vasorelaxant effect of H 2 S as a novel endogenous gaseous K ATP channel opener. EMBO J 2001, 20: 6008-6016.
Siebert N, Cantré D, Eipel C, Vollmar B: H 2 S contributes to the hepatic arterial buffer response and mediates vasorelaxation of the hepatic artery via activation of K ATP channels. Am J Physiol Gastrointest Liver Physiol 2008, 295: G1266-G1273.
Laggner H, Hermann M, Esterbauer H, Muellner MK, Exner M, Gmeiner BM, Kapiotis S: The novel gaseous vasorelaxant hydrogen sulfide inhibits angiotensin-converting enzyme activity of endothelial cells. J Hypertens 2007, 25: 2100-2104.
Hosoki R, Matsuki N, Kimura H: The possible role of hydrogen sulfide as an endogenous smooth muscle relaxant in synergy with nitric oxide. Biochem Biophys Res Commun 1997, 237: 527-531.
Ali MY, Ping CY, Mok YY, Ling L, Whiteman M, Bhatia M, Moore PK: Regulation of vascular nitric oxide in vitro and in vivo ; a new role for endogenous hydrogen sulphide? Br J Pharmacol 2006, 149: 625-634.
Whiteman M, Li L, Kostetski I, Chu SH, Siau JL, Bhatia M, Moore PK: Evidence for the formation of a novel nitrosothiol from the gaseous mediators nitric oxide and hydrogen sulphide. Biochem Biophys Res Commun 2006, 343: 303-310.
Webb GD, Lim LH, Oh VM, Yeo SB, Cheong YP, Ali MY, El Oakley R, Lee CN, Wong PS, Caleb MG, Salto-Tellez M, Bhatia M, Chan ES, Taylor EA, Moore PK: Contractile and vasorelaxant effects of hydrogen sulfide and its biosynthesis in the human internal mammary artery. J Pharmacol Exp Ther 2008, 324: 876-882.
Bhatia M: Hydrogen sulfide as a vasodilator. IUBMB Life 2005, 57: 603-606.
Koenitzer JR, Isbell TS, Patel HD, Benavides GA, Dickinson DA, Patel RP, Darley-Usmar VM, Lancaster JR Jr, Doeller JE, Kraus DW: Hydrogen sulfide mediates vasoactivity in an O 2 -dependent manner. Am J Physiol Heart Circ Physiol 2007, 292: H1953-H1960.
Kiss L, Deitch EA, Szabó C: Hydrogen sulfide decreases adenosine triphosphate levels in aortic rings and leads to vasorelaxation via metabolic inhibition. Life Sci 2008, 83: 589-594.
Whiteman M, Armstrong JS, Chu SH, Jia-Ling S, Wong BS, Cheung NS, Halliwell B, Moore PK: The novel neuromodulator hydrogen sulfide: an endogenous peroxynitrite 'scavenger'? J Neurochem 2004, 90: 765-768.
Kimura Y, Kimura H: Hydrogen sulfide protects neurons from oxidative stress. FASEB J 2004, 18: 1165-1167.
Ohsawa I, Ishikawa M, Takahashi K, Watanabe M, Nishimaki K, Yamagata K, Katsura K, Katayama Y, Asoh S, Ohta S: Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat Med 2007, 13: 688-694.
Oh GS, Pae HO, Lee BS, Kim BN, Kim JM, Kim HR, Jeon SB, Jeon WK, Chae HJ, Chung HT: Hydrogen sulfide inhibits nitric oxide production and nuclear factor-κB via heme oxygenase-1 expression in RAW264.7 macrophages stimulated with lipopolysaccharide. Free Radic Biol Med 2006, 41: 106-119.
Hu Y, Chen X, Pan TT, Neo KL, Lee SW, Khin ES, Moore PK, Bian JS: Cardioprotection induced by hydrogen sulfide preconditioning involves activation of ERK and PI3K/Akt pathways. Pflugers Arch 2008, 455: 607-616.
Jeong SO, Pae HO, Oh GS, Jeong GS, Lee BS, Lee S, Kim dY, Rhew HY, Lee KM, Chung HT: Hydrogen sulfide potentiates interleukin-1β-induced nitric oxide production via enhancement of extracellular signal-regulated kinase activation in rat vascular smooth muscle cells. Biochem Biophys Res Commun 2006, 345: 938-944.
Yang G, Sun X, Wang R: Hydrogen sulfide-induced apoptosis of human aorta smooth muscle cells via the activation of mitogen-activated protein kinases and caspase-3. FASEB J 2004, 18: 1782-1784.
Zhi L, Ang AD, Zhang H, Moore PK, Bhatia M: Hydrogen sulfide induces the synthesis of proinflammatory cytokines in human monocyte cell line U937 via the ERK-NF-κB pathway. J Leukoc Biol 2007, 81: 1322-1332.
Ubuka T: Assay methods and biological roles of labile sulfur in animal tissues. J Chromatogr B Analyt Technol Biomed Life Sci 2002, 781: 227-249.
Mitsuhashi H, Ikeuchi H, Yamashita S, Kuroiwa T, Kaneko Y, Hiromura K, Ueki K, Nojima Y: Increased levels of serum sulfite in patients with acute pneumonia. Shock 2004, 21: 99-102.
Bickler PE, Buck LT: Hypoxia tolerance in reptiles, amphibians, and fishes: life with variable oxygen availability. Annu Rev Physiol 2007, 69: 145-170.
Volpato GP, Searles R, Yu B, Scherrer-Crosbie M, Bloch KD, Ichinose F, Zapol WM: Inhaled hydrogen sulfide: a rapidly reversible inhibitor of cardiac and metabolic function in the mouse. Anesthesiology 2008, 108: 659-668.
Baumgart K, Simkova V, Weber S, Barth E, Albuszies G, Radermacher P, Calzia E: Myocardial effects of hypothermia and inhaled H 2 S in ventilated mice [abstract]. Shock 2008,29(Suppl 1):58.
Simkova V, Baumgart K, Barth E, Albuszies G, Weber S, Radermacher P, Calzia E: Cytochrome c stimulated respiration in liver mitochondria of anesthetised mice: effects of body temperature and H 2 S [abstract]. Shock 2008,29(Suppl 1):59.
Kuznetsov AV, Schneeberger S, Seiler R, Brandacher G, Mark W, Steurer W, Saks V, Usson Y, Margreiter R, Gnaiger E: Mitochondrial defects and heterogeneous cytochrome c release after cardiac cold ischemia and reperfusion. Am J Physiol Heart Circ Physiol 2004, 286: H1633-H1641.
Protti A, Singer M: Bench-to-bedside review: potential strategies to protect or reverse mitochondrial dysfunction in sepsis-induced organ failure. Crit Care 2006, 10: 228.
Protti A, Singer M: Strategies to modulate cellular energetic metabolism during sepsis. Novartis Found Symp 2007, 280: 7-16.
Blackstone E, Roth MB: Suspended animation-like state protects mice from lethal hypoxia. Shock 2007, 27: 370-372.
Couch L, Martin L, Rankin N: Near death episode after exposure to toxic gases from liquid manure. NZ Med J 2005, 118: U1414.
Leslie M: Nothing rotten about hydrogen sulfide's medical promise. Science 2008, 320: 155-157.
Li J, Zhang G, Cai S, Redington AN: Effect of inhaled hydrogen sulfide on metabolic responses in anesthetized, paralyzed, and mechanically ventilated piglets. Pediatr Crit Care Med 2008, 9: 110-112.
Haouzi P, Notet V, Chenuel B, Chalon B, Sponne I, Ogier V, Bihain B: H 2 S induced hypometabolism in mice is missing in sedated sheep. Respir Physiol Neurobiol 2008, 160: 109-115.
Gröger M, Simon F, Öter S, Speit G, Szabó C, Radermacher P, Calzia E: H 2 S attenuates oxidative DNA-damage during renal ischemia/reperfusion injury [abstract]. Shock 2008,29(Suppl 1):57.
Johansen D, Ytrehus K, Baxter GF: Exogenous hydrogen sulfide (H 2 S) protects against regional myocardial ischemia–reperfusion injury – evidence for a role of K ATP channels. Basic Res Cardiol 2006, 101: 53-60.
Lefer DJ: A new gaseous signaling molecule emerges: cardio-protective role of hydrogen sulfide. Proc Natl Acad Sci USA 2007, 104: 17907-17908.
Sivarajah A, McDonald MC, Thiemermann C: The production of hydrogen sulfide limits myocardial ischemia and reperfusion injury and contributes to the cardioprotective effects of preconditioning with endotoxin, but not ischemia in the rat. Shock 2006, 26: 154-161.
Tisherman SA, Drabek T: Hydrogen sulfide: metabolic mediator or toxic gas? Pediatr Crit Care Med 2008, 9: 129-130.
Zhang H, Bhatia M: Hydrogen sulfide: a novel mediator of leukocyte activation. Immunopharmacol Immunotoxicol 2008, 30: 631-645.
Zhang H, Hegde A, Ng SW, Adhikari S, Moochhala SM, Bhatia M: Hydrogen sulfide up-regulates substance P in polymicrobial sepsis-associated lung injury. J Immunol 2007, 179: 4153-4160.
Bhatia M, Wong FL, Fu D, Lau HY, Moochhala SM, Moore PK: Role of hydrogen sulfide in acute pancreatitis and associated lung injury. FASEB J 2005, 19: 623-625.
Remick DG, Xioa H: Hypothermia and sepsis. Front Biosci 2006, 11: 1006-1013.
Hagiwara S, Iwasaka H, Matsumoto S, Noguchi T: Changes in cell culture temperature alter release of inflammatory mediators in murine macrophagic RAW264.7 cells. Inflamm Res 2007, 56: 297-303.
L'Her E, Amerand A, Vettier A, Sebert P: Effects of mild induced hypothermia during experimental sepsis. Crit Care Med 2006, 34: 2621-2623.
Baumgart K, SImkova V, Perl M, Seitz DH, Huber-Lang M, Weber S, Radermacher P, Knöferl MW: Inhaled H 2 S and hypothermia comparably attenuate surgery-related inflammation [abstract]. Shock 2008,29(Suppl 1):72.
Singer M, De SV, Vitale D, Jeffcoate W: Multiorgan failure is an adaptive, endocrine-mediated, metabolic response to overwhelming systemic inflammation. Lancet 2004, 364: 545-548.
Levy RJ, Piel DA, Acton PD, Zhou R, Ferrari VA, Karp JS, Deutschman CS: Evidence of myocardial hibernation in the septic heart. Crit Care Med 2005, 33: 2752-2756.
Baumgart K, Georgieff M, Radermacher P, Calzia E: Cardioprotection by hydrogen sulfide: suspended animation, inflammation, and apoptosis. Shock 2009, 31: 218-219.
Szabó C, Veres G, Radovits T, Karck M, Szabó G: Infusion of sodium sulfide improves myocardial and endothelial function in a canine model of cardiopulmonary bypass [abstract]. Crit Care 2007,11(Suppl 2):S1.
Tisherman SA: Suspended animation for resuscitation from exsanguinating hemorrhage. Crit Care Med 2004,32(Suppl):S46-S50.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
CS is an officer and stockholder of Ikaria (Seattle, WA, USA), a company involved in the commercial development of hydrogen sulfide. PR received research grants from Ikaria. FW, PA and EC declare that they have no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
About this article
Cite this article
Wagner, F., Asfar, P., Calzia, E. et al. Bench-to-bedside review: Hydrogen sulfide – the third gaseous transmitter: applications for critical care. Crit Care 13, 213 (2009). https://doi.org/10.1186/cc7700
Published:
DOI: https://doi.org/10.1186/cc7700