Abstract
Background
For people with dementia, patient-centred care should involve timely explanation of the diagnosis and its implications. However, this is not routine. Theoretical models of behaviour change offer a generalisable framework for understanding professional practice and identifying modifiable factors to target with an intervention. Theoretical models and empirical work indicate that behavioural intention represents a modifiable predictor of actual professional behaviour. We identified factors that predict the intentions of members of older people's mental health teams (MHTs) to perform key behaviours involved in the disclosure of dementia.
Design
Postal questionnaire survey.
Participants
Professionals from MHTs in the English National Health Service.
Methods
We selected three behaviours: Determining what patients already know or suspect about their diagnosis; using explicit terminology when talking to patients; and exploring what the diagnosis means to patients. The questionnaire was based upon the Theory of Planned Behaviour (TPB), Social Cognitive Theory (SCT), and exploratory team variables.
Main outcomes
Behavioural intentions.
Results
Out of 1,269 professionals working in 85 MHTs, 399 (31.4%) returned completed questionnaires. Overall, the TPB best explained behavioural intention. For determining what patients already know, the TPB variables of subjective norm, perceived behavioural control and attitude explained 29.4% of the variance in intention. For the use of explicit terminology, the same variables explained 53.7% of intention. For exploring what the diagnosis means to patients, subjective norm and perceived behavioural control explained 48.6% of intention.
Conclusion
These psychological models can explain up to half of the variation in intention to perform key disclosure behaviours. This provides an empirically-supported, theoretical basis for the design of interventions to improve disclosure practice by targeting relevant predictive factors.
Trial Registration
ISRCTN15871014.
Similar content being viewed by others
Background
The early care of people with dementia ideally involves a sensitive and accurate explanation of the diagnosis to individuals and informal carer-givers, and information about the likely prognosis and possible packages of care [1]. Timely disclosure can facilitate decisions about treatment – increasingly important with the advent of therapies to slow disease progression – and allows opportunities to plan family, fiscal and long-term care arrangements. In the context of recognised aspects of quality of care, disclosure therefore needs to be patient-centred and timely [2].
From an ethical perspective, people with dementia have a right to know their diagnosis. Furthermore, many want to know their diagnosis or more information about their illness [3–7]. The majority of people with dementia found it helpful to have been told their diagnosis [3]. Specific benefits include validating their perception that something is wrong [8] and helping them make sense of their experience [5]. Recent qualitative studies have highlighted the range of coping strategies used by people with dementia to adjust to their diagnosis [9–13]. In contrast, lack of information can cause distress and forestall opportunities to engage in grief work to cope with loss.
Yet disclosure practice by healthcare professionals varies widely [14]. The diagnosis is often disclosed to caregivers but not to people with dementia themselves [15]. There is therefore substantial scope for improving professional practice. A considerable body of literature suggests that a range of interventions (e.g., reminder systems, interactive education) can be effective in changing professional behaviour [16]. But there is little empirical evidence on which strategy is most appropriate in the light of a given context or targeted clinical behaviour [17] due to problems understanding the generalisability of the strategies used. One way forward is to use a generalisable framework such as that offered by theory [18–20]. Many factors may influence disclosure: patient characteristics (e.g., age, ability to retain the diagnosis); nature of the dementia (e.g., severity, diagnostic uncertainty); structural factors (e.g., time); and clinician factors (e.g., perceived value of disclosure) [14, 21–27]. Some of these may be amenable to change and hence targeted in efforts to improve disclosure practice. Theoretical models of behaviour change allow identification of potentially modifiable factors to target with an intervention [28]. While it would be useful to identify factors that predict professionals' actual disclosure behaviour, there are several problems in measuring behaviour, such as poor recall of events by people with dementia [29]. However, one potentially modifiable factor that can predict actual behaviour is behavioural intention (or motivation).
Behavioural intention is a valid proxy for behaviour predicting 27–28% of the variance in actual behaviour across a wide range of contexts [30, 31]. A recent systematic review of the relationship between clinical behaviours and behavioural intention found that the proportion of variance in behaviour explained by intention was of a similar magnitude to that found in the literature relating to non-health professionals [32]. Further, behaviour change rarely occurs in those lacking the intention to change their behaviour [33]. In other words, intention is a necessary but not sufficient condition for action. Knowing whether intentions are low is an important part of identifying barriers to action. It is in this spirit that we used intention as an important proximal determinant of behaviour. Therefore, explaining variation in behavioural intention represents a useful step in efforts to improve disclosure practice, consistent with the initial phases recommended for the development and evaluation of complex interventions [34]. This paper describes the first stages of a larger study to develop an intervention to promote appropriate disclosure [35]. We surveyed members of mental health teams (MHTs) for older people to identify factors that predict their intention to disclose a diagnosis of dementia to patients.
Methods
Participants
Eligible participants were members of MHTs for older people from 35 National Health Service (NHS) Trusts in the North of England that provided mental health services and a random sample of Trusts from elsewhere in England. Although disclosure of dementia might predominantly be regarded as the responsibility of specialist old age psychiatrists, other professionals (e.g., community psychiatric nurses, clinical psychologists) have various roles in this process. Therefore, we invited all professionals in each team to participate.
Selection of theories
We selected two theories, the Theory of Planned Behaviour (TPB) [36] and Social Cognitive Theory (SCT) [37]; both have been rigorously evaluated in other settings and they explain behaviour in terms of factors amenable to change (e.g., beliefs, perceived external constraints). There were economies of measurement inherent in using both theories because of overlapping constructs. According to the TPB, the strength of a behavioural intention is predicted by attitudes towards the behaviour (in this case disclosure), subjective norms based on the perceived views of other individuals or groups (i.e., perceived social pressure), and perceived behavioural control, encompassing beliefs about self-efficacy (an individual's confidence about being able to perform an action) and wider environmental factors that enable or inhibit performance [36]. SCT considers self-efficacy, outcome expectancy (an individual's estimate that a given behaviour will lead to certain outcomes) and individuals' goals in explaining behaviour, including proximal goals (such as intentions) [37].
The above theories are concerned with individual behaviour. Factors such as the lack of clarity of roles and responsibilities within teams may also influence disclosure practice [38]. Therefore we planned to include some exploratory questions around these factors.
Selection of behaviours
Appropriate disclosure encompasses multiple actions taken by professionals, usually over a period of time, tailored to individuals' receptiveness and information needs. We identified key behavioural components from a literature review, interviews with people with dementia and caregivers, and a consensus panel including a range of professionals and a patient advocate.
We judged that, based on likely length, a theory-based questionnaire could explore up to three specific behaviours. We used a Delphi process to select three behaviours based on the following criteria: covering different stages of the disclosure process; the earlier consensus panel rankings; importance to people with dementia and caregivers; evidence of benefit; and potential for change. The behaviours were:
-
1.
Determining what the patient already knows or suspects about their diagnosis;
-
2.
Using the actual words 'dementia' or 'Alzheimer's disease' when talking to the patient; and
-
3.
Exploring what the diagnosis means to the patient.
Questionnaire development
Items measuring variables from the TPB and SCT were initially derived from previously recommended scales and items [36, 37, 39, 40] as well as a qualitative analysis of interviews with people with dementia and caregivers. The items and format were then iteratively developed during cognitive interviews with a convenience sample of six mental health professionals.
The main questionnaire constructs are summarised below. The items (Additional File 1) and the full questionnaire in (Additional File 2) are also available. To reduce response set bias, some items were reverse-worded and responses reverse-scored.
-
1.
Behavioural intentions for both the TPB and (as a measure of proximal goals) SCT were measured by two items for each behaviour in the context of a given scenario in which the professional was confident of the diagnosis of dementia.
-
2.
Attitude items related to expected consequences (for both patient and professional) of performing the behaviour. Three items measured the emotional impact on professionals of performing each disclosure behaviour (hereafter referred to as 'emotional attitude'). The seven to ten attitude items for each behaviour also served to measure outcome expectancies for SCT.
-
3.
Subjective norm comprises normative beliefs (about whether specific reference groups or individuals think a person should perform a behaviour) weighted by the person's motivation to comply with these views. Three items assessed normative beliefs for each behaviour as professionals may perceive different levels of approval or disapproval from a range of groups (e.g., other team colleagues, patients). The three items measuring motivation to comply with these sources of pressure related to disclosure of a diagnosis of dementia in general. Answers to these items provided weights (i.e., multipliers) for normative belief scores. Weighted normative beliefs were summed to produce subjective norm scores and standardised to a one to seven score to facilitate comparisons with other scores. A fourth subjective norm item included the idea of motivation to comply in the form of specifying 'people who are important to me professionally' and so weighting was not required [36].
-
4.
Perceived behavioural control. There were three control items per behaviour, using recommended stems [36]. e.g., 'It is easy to ...'; 'I feel I have the skills to ....'; 'The decision to ... is beyond my control'.
-
5.
Self-efficacy. There were four to eight self-efficacy items per behaviour, specifying situations where professionals might feel different levels of confidence in their ability to enact each behaviour.
-
6.
Team role. We included the following exploratory items as they may influence intention to perform disclosure behaviours:
-
a)
Perceived reliability/role of colleagues, e.g., "I can rely on my colleagues in my mental health team to use the actual words 'dementia' or 'Alzheimer's Disease' when talking to the patient".
-
b)
Role responsibility. Items concerning which team members were responsible for each behaviour: psychiatrist; social worker; clinical psychologist; community psychiatric nurse; occupational therapist; care or nursing assistant; in-patient or day hospital nurse; or other (giving details). These provided data about whether each respondent's own professional group was regarded as responsible for the behaviour and, when aggregated for each team, the number of professional groups in each team perceived as being responsible for the behaviour.
Survey administration
We ascertained the composition of MHTs from local contacts, usually service managers. We then wrote to all professionals via these contacts and asked those who agreed to participate to complete an 'opt-in' form. All potential participants were offered a small financial incentive (a £20 gift voucher), enclosed with the questionnaire subsequently sent out. We asked respondents to complete questionnaires independently (i.e., not together in teams). We posted up to three reminders to non-respondents who had opted in earlier.
Sample Size
Power calculations for multiple regression analysis depend on the number of cases per predictor variable. A minimum sample size of 50 + 8 m, where m is the number of predictor variables, is recommended for testing the multiple correlation, and 104 + m for testing individual predictors [41, 42]. With approximately 10 predictor variables for each behaviour, minimum sample sizes of 130 and 114 subjects were required to test the multiple correlation and individual predictors respectively. Taking the larger figure as the target sample size and conservatively assuming a 30% response rate from individuals, we planned to approach an estimated 420 individuals from 120 MHTs.
Analysis
The internal reliability of the constructs was assessed using Cronbach's alpha coefficient and by considering the correlation of each item with the construct score calculated without the inclusion of that item (item-total correlation). A figure of 0.6 was specified as an appropriate threshold below which internal reliability was considered to be unsatisfactory. In these cases, either a subset of items was identified that did have adequate reliability or a single item was selected on the basis of face validity. We compared differences in mean construct scores between the three behaviours using the variance ratio test. Pearson product moment correlation coefficients were used to examine the bivariate relationships between constructs.
The relationships between intention and TPB, SCT, and team constructs were investigated using multiple regression with intention specified as the dependent variable. This was done in two stages. In the first stage, the relationship between intention and the set of constructs from each theoretical model was assessed separately. For each variable set the predictor variables were added using a stepwise procedure. The variable most highly correlated with intention was added first. On subsequent steps the variable explaining the greatest amount of the residual variation was added provided that the improvement in the fit of the model was significant at the 5% level.
In the second stage, all constructs that significantly predicted intention in parallel regression analyses for the three behaviours were simultaneously entered into a stepwise regression analysis.
Ethical approval
The study was approved by the Multi-Centre Research Ethics Committee for Scotland and by the Research and Development offices of the participating NHS Trusts.
Results
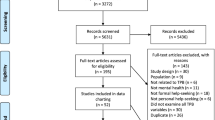
Response rates
Out of the 35 trusts approached, four did not provide team information or distribute opt-in letters and eight were excluded due to delays in obtaining research governance approval. In the remaining 23 trusts, we identified 114 MHTs for older people and 1,269 individual professionals. Out of these individuals, 420 (33.1%) from 85 teams opted in and 399 (31.4%) returned completed questionnaires (Table 1). The number of teams per trust professionals per team was higher than anticipated, contributing to a larger number of responses than we had anticipated.
Psychometric properties of measured constructs
For the TPB variables, measures relating to intention, emotional attitudes and subjective norms achieved acceptable internal consistency (alpha ≥ 0.6) for all three behaviours (Table 2). For other constructs, removal of some items improved internal consistency. (Removed items are indicated in Additional File 1.)
As we had no a priori basis for combining the exploratory team items as a single construct, we did not attempt reliability analyses for them.
Descriptive data
Table 2 shows the mean values for each of the five psychological variables for the three disclosure behaviours. Mean behavioural intention significantly differed between the three behaviours (F = 105.80; df = 2; p < 0.001), being highest for determining what the patient already knows and lowest for the use of explicit terminology.
The other mean construct scores for the TPB, SCT and team variables also varied significantly between the three behaviours. The following mean scores were all lowest for the use of explicit terminology: attitude; subjective norm; self-efficacy and outcome expectancies. In contrast, mean PBC was highest for the use of explicit terminology.
For the team variables, approximately four professional groups were involved in each behaviour. Fewer (68.2%) respondents considered that using explicit terminology was consistent with their roles compared with determining what the patient knows and exploring the meaning of the diagnosis (74.9% and 76.9% respectively; F = 14.28; p < 0.001). Respondents reported being less able to rely on other colleagues to use explicit terminology compared with the other two behaviours (F = 39.86; p < 0.001).
Correlations
For all three behaviours, all psychological variables were significantly correlated (Table 3). The high correlations between the TPB attitude and SCT outcome expectancy are due to overlapping items.
In general, respondents reported greater ability to rely on colleagues to perform a disclosure behaviour where they thought that a greater number of professional groups were responsible for the behaviour (correlation coefficients 0.122, p = 0.02 for determining what patient knows; 0.259, p < 0.001 for use of explicit terminology; 0.150, p = 0.003 for exploring meaning of the diagnosis).
Prediction of intention
For exploring what the patient already knows, the TPB variables of subjective norm, perceived behavioural control, emotional attitude and attitude explained 29.4% of behavioural intention (Table 4). In comparison, SCT explained 24.2% of intention whilst the team variables explained 15.5%. When all constructs were combined, taking into account the overlap between the TPB and SCT constructs, the prediction of intention modestly improved to 35.6%.
For the use of explicit terminology, the TPB variables of subjective norm, perceived behavioural control, emotional attitude and attitude explained 53.7% of intention. Notably, both SCT and two of the team variables (perceived role and being able to rely on colleagues) also explained high proportions of intention (47.5% and 42.2% respectively). Combining all constructs improved prediction to 63.5%.
For exploring what the diagnosis means to the patient, the TPB variables of subjective norm and perceived behavioural control explained 48.6% of intention. The SCT explained 31.1% of intention, whilst the team variables explained 18%. The combined constructs model added little to prediction (52.7%).
Discussion
Appropriate disclosure of dementia requires a number of interrelated steps and multi-disciplinary input. Most mental health professionals surveyed recognised their roles in and had positive intentions towards performing three disclosure behaviours. The TPB explained between 28.6% and 53.3% of variation in intentions, with subjective norm consistently representing an important explanatory variable. Intention to use explicit terminology was also explained by attitude but – unlike both other behaviours – not by perceived behavioural control.
The TPB tended to explain a greater proportion of variance in intentions than constructs from SCT and the team variables. This was not simply due to the greater number of predictors (four compared with two for SCT and three for team variables): taking only the first two predictor variables from each model, the TPB still accounted for more variance in each behaviour than either of the other two theoretical approaches. The TPB also was relatively parsimonious compared with the regression model which combined all constructs and modestly improved prediction. We did not conduct an analysis that allows the TPB and SCT to compete directly. Instead we added sets of predictors hierarchically, so for the overlapping constructs (e.g., self-efficacy with perceived behavioural control and outcome expectancies with attitude), beta weights were expected to reflect both some of the predictive value of each variable and also the order of entry of variables.
The team variables accounted for considerably more variance in the use of explicit terminology compared with both other behaviours, with the lone variable of being able to rely on colleagues explaining over a third of intention (37.4%). However, this variable explained less variation in the combined constructs model, suggesting that its effects may be mediated through other predictors. For example, subjective norm for the use of explicit terminology may incorporate aspects of teamwork (i.e., 'Members of my MHT would approve of my using the actual words 'dementia' or 'Alzheimer's disease' when talking to the patient.')
Our findings have several implications for improving the quality of disclosure practice. On a 7-point scale, mean intention was 5.72 (SD 1.17) for determining what the patient already knows. This suggests modest scope for further improving intention (and hence actual behaviour) [43]. According to results based on the TPB, interventions predominantly targeting subjective norm and perceived behavioural control may have the greatest impact in changing intention (as these are the strongest predictors of intention), with lesser effects expected by targeting attitudes. While there is no guarantee that changing a significant predictor will result in changed behaviour, this approach uses an evidence base in a systematic way to select intervention components and thus to move forward from correlational designs and test plausible hypotheses using experimental designs.
For the use of explicit terminology, the mean intention score was 4.66 (SD 1.47) and lowest out of the three behaviours. This suggests relatively greater potential exists for changing intention and hence practice. Interventions targeting subjective norm, attitudes relating to outcomes for the patient and professional and, possibly, emotional attitude may represent key targets for intervention. However, the team variables – whether professionals perceived they could rely on colleagues to use explicit terminology and whether professionals also believed this behaviour to be compatible with their own roles – explained over 40% of variation in intention. Interventions around clarifying and revising team roles may offer promising means of changing intention, potentially also operating via influencing subjective norms.
For exploring what the diagnosis means to the patient, the mean intention score of 5.41 (SD 1.32) suggests modest scope for changing intention and hence behaviour. Interventions targeting subjective norms and perceived behavioural control offer the most promising means of achieving this.
Consistent with the predictions of SCT, both self-efficacy and outcome expectancies explained intention for all three behaviours, albeit less than the TPB variables did. Given the overlap with attitude, the pattern of outcome expectancies predicting intention across the three behaviours is expected. However, strategies to improve disclosure practice should also consider means of enhancing self-efficacy.
Earlier studies have investigated reasons why mental health professionals do or do not disclose dementia [3–6]. Their methods have several limitations which have been addressed by this study. First, the interpretation of these and studies in other contexts that attempt to understand clinical practice or improve quality of care is often hampered by the lack of an underlying robust theoretical model that explains behaviour in terms of cognitive factors. The assumption that clinical practice is a form of human behaviour and can be described in terms of general theories relating to human behaviour offers the basis for a generalisable framework for understanding and developing interventions to change professional behaviour. Second, professionals' reported reasons for their actions may not explain their actual practice. Social desirability bias may explain why respondents to our survey rated their own intentions, attitudes and beliefs in a relatively favourable light. However, other studies have demonstrated that measuring behavioural intention using similar methods can usefully predict actual behaviour [30–32]. Third, many previously reported barriers to appropriate disclosure are less amenable to change within the present healthcare context and resources, e.g., severity of dementia or lack of time. We examined potentially modifiable variables, namely, behavioural intention and its predictors.
One limitation to this study was the relatively low response rate (31%) from the eligible sample. This was probably partly attributable to the staged 'opt-in' process necessary to comply with data protection legislation. Most (95%) professionals who opted in to do the survey did complete questionnaires. However, external validity may be undermined if respondents differed systematically from non-respondents, e.g., had more positive attitudes towards disclosure.
We did not explore the contribution of professional roles in predicting intention, largely because it was beyond the scope of this paper. We are presently addressing this issue in another survey, within a subsequent stage of this programme of work, using a much larger sample which will allow better precision for exploring differences between professional groups.
We do not claim that other intervention strategies, such as restructuring teams or care delivery processes, would be of lesser effectiveness than any intervention developed using the approach we describe. Such environmental or organisational changes may also change underlying psychological factors – so that changes in beliefs or attitudes following 'forced' changes in practice. The perspective of social cognitive theories is that external influences on behaviour are mediated through perceptions of individuals (i.e., the predictor variables in the theories we have used). They do not claim that external influences do not 'drive' behaviour; merely that they are unlikely to drive behaviour without the awareness of the person who is behaving. We have made the assumption that the disclosure behaviours under investigation are enacted voluntarily, with low levels of automatism.
Our findings provide an empirically-supported, theoretical basis for the design of interventions to improve the quality of disclosure practice by targeting relevant predictive factors. It is uncertain whether the causal relationships predicted by theory would be seen in a subsequent intervention study. For example, the factors that determine current behaviour may differ from those that determine change in behaviour. The next step is therefore to evaluate whether interventions targeting the key predictive variables identified in this study do increase intention.
References
Department of Health: National Service Framework for Older People. 2001, London , Department of Health
Institute of M: Crossing the Quality Chasm: A New Health System for the 21st Century. 2001, Washington , National Academy Press
Jha A, Tabet N, Orrell M: To tell or not to tell - comparison of older patients' reaction to their diagnosis of dementia and depression. International Journal of Geriatric Psychiatry. 2001, 16: 879-885.
Marzanski M: Would you like to know what is wrong with you? On telling the truth to patients with dementia. Journal of Medical Ethics. 2000, 26: 108-113.
McWilliams E: The process of giving and receiving a diagnosis of dementia: an in-depth study of sufferers', carers' and consultants' experiences. PSIGE Newsletter. 1998, 64: 18-25.
Dautzenberg PLJ, van Marum RJ, van der Hammen R, Paling HA: Patients and families desire a patient to be told the diagnosis of dementia: a survey by questionnaire on a Dutch memory clinic. Int J Geriatr Psychiatry. 2003, 2003 (18): 777-779.
Elson P: Do older adults presenting with memory complaints wish to be told if later diagnosed with Alzhimer's disease?. Int J Geriatr Psychiatry. 2006, 21: 419-442.
Robinson P, Ekman SL, Wahlund LO: Unsettled, uncertain and striving to understand: toward an understanding of the situation of persons with suspected dementia. Int J Aging Hum Dev. 1998, 47: 143-161.
Young RF, Harris PB: Medical experiences and concerns of people with Alzheimer's disease. The person with Alzheimer's disease: pathways to understanding the experience. 2002, Baltimore & London , The John Hopkins University Press, 29-46.
Pratt R, Wilkinson H: A psychosocial model of understanding the experience of receiving a diagnosis of dementia. Dementia. 2003, 2: 181-191.
Derksen E, Vernooij-Dassen M, Gillissen F, Olde Rikkert M, Scheltens P: Impact of diagnostic disclosure in dementia on patients and carers: qualitative case series analysis. Aging and Mental Health. 2006, 10: 525-531.
Preston L, Marshall A, Bucks RS: Investigating the ways that older people cope with dementia: a qualitative study. Aging and Mental Health. 2007, 11: 131-143.
MacQuarrie CM: Experiences in early stage Alzheimer's disease: understanding the paradox of acceptance and denial. Aging and Mental Health. 2005, 9: 430-441.
Bamford C, Lamont S, Eccles M, Robinson L, May C, Bond J: Disclosing a diagnosis of dementia: a systematic review. Int J Geriatr Psychiatry. 2004, 19: 151-169.
Audit C: Forget Me Not 2002. 2002, London
Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, Whitty P, Eccles MP, Matowe L, Shirran L, Wensing M, Dikstra R, Donaldson C, Hutchison A: Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004, 8 (6):
Foy R, Eccles M, Jamtvedt G, Young J, Grimshaw J, Baker R: What do we know about how to do audit and feedback? Pitfalls in applying evidence from a systematic review. BMC Health Serv Res. 2005, 5: 50-
Eccles M, Grimshaw J, Walker A, Johnston M, Pitts N: Changing the behaviour of healthcare professionals: the use of theory in promoting the uptake of research findings. J Clin Epidemiol. 2005, 58: 107-112.
Oxman AD, Fretheim A, Flottorp S: The OFF theory of research utilization. J Clin Epidemiol. 2005, 58 (2): 113-116.
The Improved Clinical Effectiveness through Behavioural Research G: Designing theoretically-informed implementation interventions. BMC Implementation Science. 2006, 4-
Vassilas CA, Donaldson J: Telling the truth: what do general practitioners say to patients with dementia or terminal cancer?. BJGP. 1998, 48: 1081-1082.
Heal HC, Husband HJ: Disclosing a diagnosis of dementia: is age a factor?. Aging and Mental Health. 1998, 2: 144-150.
Johnson H, Bouman WP, Pinner G: On telling the truth in Alzheimer's disease: a pilot study of current practice and attitudes. International Psychogeriatrics. 2000, 12: 221-229.
Rice K, Warner N: Breaking the bad news: what do psychiatrists tell patients with dementia about their illness?. International Journal of Geriatric Psychiatry. 1994, 9: 467-471.
Downs M, Clibbens R, Rae C, Cook A, Woods R: What do general practitioners tell people with dementia and their families about the condition?. Dementia. 2002, 1: 47-58.
Fortinsky RH, Leighton A, Wasson JH: Primary care physicians' diagnostic, management and referral practices for older persons and families affected by dementia. Research on Aging. 1995, 17: 124-148.
Vernooij-Dassen MJ, Moniz-Cook ED, Woods RT, De Lepeleire J, Leuschner A, Zanetti O, de Rotrou J, Kenny G, Franco M, Peters V, Iliffe S: Factors affecting timely recognition and diagnosis of dementia across Europe: from awareness to stigma. Int J Geriatr Psychiatry. 2005, 20: 377-386.
Michie S, Abraham C: Identifying techniques that promote health behaviour change: Evidence based or evidence inspired?. Psychology & Health. 2004, 19: 29-49.
Chodosh J, Berry E, Lee M, Connor K, DeMonte R, Ganaits T, Heikoff L, Rubenstein L, Mittman B, Vickery B: Effect of a dementia care management intervention on primary care provider knowledge, attitudes, and perceptions of quality of care. J Am Geriatr Soc. 2006, 54 (2): 311-317.
Sheeran P: Intention-behavior relations: A conceptual and empirical review. European Review of Social Psychology. 2002, 12: 1-36.
Armitage CJ, Conner M: Efficacy of the theory of planned behaviour: a meta-analytic review. British Journal of Social Psychology. 2001, 40: 471-499.
Eccles MP, Hrisos S, Francis J, Kaner EF, Dickinson HO, Beyer F, Johnston M: Do self- reported intentions predict clinicians behaviour: a systematic review. Implementation Science. 2006, 1: 28-
Orbell S, Sheeran P: 'Inclined abstainers': a problem for predicting health-related behaviour. Br J Soc Psychol. 1998, 37: 151-165.
Medical Research C: A framework for development and evaluation of RCTs for complex interventions to improve health. 2000, London
Eccles MP, Foy R, Bamford CH, Hughes JC, Johnson M, Whitty PM, Steen N, Grimshaw JG: A trial platform to develop a tailored theory based intervention to improve professional practice in the disclosure of a diagnosis of dementia. BMC Implementation Science. 2006, 1: 7-
Ajzen I: The theory of planned behaviour. Organizational Behaviour and Human Decision Processes. 1991, 50: 179-211.
Bandura A: Social foundations of thought and action: A social cognitive theory. 1986, Upper Saddle River, NJ , Prentice-Hall
Keightley J, Mitchell A: What factors influence mental health professionals when deciding whether or not to share a diagnosis of dementia with the person?. Aging and Mental Health. 2004, 8: 13-20.
Conner M, Sparks P, Conner M, Norman P: The theory of planned behaviour and health behaviours. Predicting health behaviour. 1996, Open University Press, 121-162.
Francis JJ, Eccles MP, Johnston M, Walker AE, Grimshaw JM, Foy R, Kaner EFS, Smith L, Bonetti D: Constructing questionnaires based on the theory of planned behaviour. A manual for health services researchers. 2004, Cetnre for Health Services Research, University of Newcastle upon Tyne
Tabachnik B, Fidell L: Using multivariate statistics. 1996, New York , Harper Collins
Green S: "How many subjects does it take to do a regression analysis?". Multivariate Behavioural Research. 1991, 26: 499-510.
Acknowledgements
We are grateful to all members of MHTs who participated in the survey. This project is funded by UK Medical Research Council, Grant reference number G0300999. Jeremy Grimshaw holds a Canada Research Chair in Health Knowledge Transfer and Uptake. The views expressed in this study are those of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Martin Eccles is Co-Editor in Chief of Implementation Science and Robbie Foy is Associate Editor; all editorial decisions on this article were made by Co-Editor in Chief Brian Mittman.
Authors' contributions
ME and MJ conceived the original idea for this study. ME, RF, CB, MJ, NS and JG obtained grant funding. JL, CB and RF led the conduct of the survey. NS and CB analysed the survey data which was interpreted by all authors. RF and CB wrote the first draft of the manuscript and all authors participated in subsequent revisions. All authors read and approved the final manuscript.
Electronic supplementary material
13012_2007_60_MOESM2_ESM.doc
Additional file 2: Talking to people with dementia about their diagnosis – can we do it better? The survey questionnaire. (DOC 628 KB)
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Foy, R., Bamford, C., Francis, J.J. et al. Which factors explain variation in intention to disclose a diagnosis of dementia? A theory-based survey of mental health professionals. Implementation Sci 2, 31 (2007). https://doi.org/10.1186/1748-5908-2-31
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1748-5908-2-31