Abstract
Background
Over the last few years, accumulating data have implicated a role for ferritin as a signaling molecule and direct mediator of the immune system. Hyperferritinemia is associated with a multitude of clinical conditions and with worse prognosis in critically ill patients.
Discussion
There are four uncommon medical conditions characterized by high levels of ferritin, namely the macrophage activation syndrome (MAS), adult onset Still’s disease (AOSD), catastrophic antiphospholipid syndrome (cAPS) and septic shock, that share a similar clinical and laboratory features, and also respond to similar treatments, suggesting a common pathogenic mechanism. Ferritin is known to be a pro-inflammatory mediator inducing expression of pro-inflammatory molecules, yet it has opposing actions as a pro-inflammatory and as an immunosuppressant. We propose that the exceptionally high ferritin levels observed in these uncommon clinical conditions are not just the product of the inflammation but rather may contribute to the development of a cytokine storm.
Summary
Here we review and compare four clinical conditions and the role of ferritin as an immunomodulator. We would like to propose including these four conditions under a common syndrome entity termed “Hyperferritinemic Syndrome”.
Similar content being viewed by others
Background
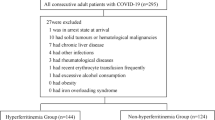
For most clinicians dealing with inflammatory diseases, serum ferritin levels are a rather non-specific marker of the acute phase response, which is often ignored or not measured when the patient presents acutely. In some diseases, ferritin levels may be extremely high and, while not specific, these very high levels may be helpful diagnostically. Four uncommon immune mediated conditions may be associated with high ferritin levels: macrophage activation syndrome (MAS), adult onset Still’s disease (AOSD), catastrophic antiphospholipid syndrome (cAPS) and septic shock. These disorders share similar clinical and laboratory presentations and they also respond to similar treatments, suggesting that hyperferritinemia may be involved in a common pathogenic mechanism.
There is increasing evidence that circulating ferritin levels may not only reflect an acute phase response but may play a critical role in inflammation [1]. Its secretion is regulated by pro-inflammatory cytokines and ferritin has immunosuppressive effects possibly mediated by binding to its receptor [2]. Different mechanisms may inhibit the ferritin-mediated suppression of the immune cells, and in turn, this impaired immunosuppression may favor the loss of tolerance and the development of autoimmune diseases [2]. Moderate levels of hyperferritinemia are associated with autoimmune diseases, including systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), multiple sclerosis (MS) [3–7] and antiphospholipid syndrome (APS) [8]. Although it is generally accepted that circulating ferritin levels may reflect an acute phase response, the explanation for why and how serum ferritin is elevated is unknown.
We hypothesize that the huge levels of ferritin seen in these four clinical conditions are not just a secondary product of the inflammatory process but rather they are part of the pathogenic mechanism. Therefore, we propose to include them under a single nomenclature: “The Hyperferritinemic Syndrome”.
Ferritin
Ferritin is an iron-binding molecule that stores iron in a biologically available form for vital cellular processes while protecting proteins, lipids and DNA from the potential toxicity of this metal element. Ferritin plays a role in a large number of other conditions, including inflammatory, neurodegenerative and malignant diseases [9].
Ferritin is a major intracellular iron storage protein in all organisms, and its structural properties are largely conserved through species (Figure 1). Each apoferritin (iron-free ferritin) shell comprises 24 subunits of two kinds: H-subunit and L-subunit. Depending on the tissue type and physiologic status of the cell, the ratio of H- to L-subunits in ferritin can vary widely, from a predominantly L-subunit rich ferritin in tissues such as liver and spleen, to H-subunit rich ferritin in the heart and kidneys [10]. The expression of ferritin is under delicate control (Figure 2). The amount of cytoplasmic ferritin is regulated by the translation of H- and L-ferritin mRNAs in response to an intracellular pool of “chelatable” or “labile” iron. In addition to iron, ferritin synthesis is regulated by cytokines at various levels (transcriptional, post-transcriptional and translational) during development, cellular differentiation, proliferation and inflammation [1]. Expression of ferritin is also regulated by oxidative stress, hormones (thyroid hormone), growth factors, second messengers, and hypoxia-ischemia and hyperoxia. Lipopolysaccharide (LPS - endotoxin), a component of the outer membrane of gram negative bacteria, elicits a variety of reactions that involve ferritin; in animal models the administration of LPS can increase ferritin expression. Also, cyclopentenone prostaglandins, which are involved in inflammatory and febrile responses as well as viral replication, induced L chain ferritin in human monocytes [1].
Ferritin structure and function. Ferritin is a major intracellular iron storage protein in all organisms, and its structural properties are largely conserved through species. Apoferritin refers to the iron-free form of the protein; the iron-containing form is termed holoferritin or simply ferritin. Each apoferritin shell comprises 24 subunits of two kinds: a H-subunit and a L-subunit. Depending on the tissue type and physiologic status of the cell, the ratio of H- to L-subunits in ferritin can vary widely. Ferritin H- and L-subunits are mapped on chromosomes 11q23 and 19q13.3, respectively, and both have multiple pseudogenes [1]. H-ferritin plays a major role in the rapid detoxification of iron, while the L-subunit is involved in nucleation, mineralization and long-term storage of iron [10].
Control of ferritin expression. The expression of ferritin is regulated at both the transcriptional and post-transcriptional levels by iron, cytokine release, chemokine production, lipopolysaccharide, prostaglandins, hormones, growth factors, second messengers, hyperoxia and hypoxia, and oxidative stress [5]. Cytokines may also affect ferritin translation indirectly through their ability to induce nitric oxide synthase and, hence, increase nitric oxide (NO) (Figure 2) [11, 12]. NO, in turn, causes inhibition of ferritin translation. Complex feedback mechanisms between ferritin and cytokines in the control of pro-inflammatory and anti-inflammatory mediators: cytokines can induce ferritin expression; otherwise, ferritin can induce the expression of pro- and anti-inflammatory cytokines.
Hyperferritinemia is associated with several inflammatory conditions, such as sepsis, systemic inflammatory response syndrome (SIRS), multiorgan dysfunction syndrome (MODS), and MAS. In critically ill patients, hyperferritinemia is associated with the severity of the underlying disease [13–16]. In one study [14], very high levels of ferritin (>3,000 ng/ml) were associated with increased mortality in a dose response fashion.
The detailed secretory pathway of serum ferritin is not completely understood. Hepatocytes, macrophages and Kupffer cells secrete ferritin [2, 17, 18]. Serum ferritin is iron-poor and mainly consists of L-subunits [2]. So far, iron incorporation is the only L-ferritin function established by in vitro studies, but more recent studies showed that L-ferritin may have a stimulatory effect on cell proliferation, independent of iron availability. These findings suggest that L-ferritin may affect some cellular pathways that remain to be identified [19].
Moreover, there is still the paradox that circulating ferritin mainly consists of L-subunits, whereas most of the evidence supporting the existence of ferritin receptors indicates specificity for H-subunits [2].
The role of ferritin as a signaling molecule requires the presence of a specific receptor. Only the ferritin receptors expressed on hepatic cells bind both H- and L-ferritin, while those expressed on the other tissues are for the H-chain [20]. In an experimental murine model, the T-cell immunoglobulin and mucin domain (TIM)-2 was identified as a receptor for H-ferritin endocytosis in B and T cells, liver and kidney [21]. TIM-2 is a member of the T-cell TIM gene family, which is a family of cell surface molecules involved in the regulation of immune responses [17, 21]. Recently, another cell surface receptor for ferritin, Scara5, was identified. Scara5 is a scavenger receptor that can bind various ligands, and, in contrast to TIM-2, it preferentially binds L-ferritin [22]. It is apparent that additional ferritin receptors may exist and have specific roles in different cell populations.
Ferritin and immunity
Ferritin as an immunosuppressant
H-ferritin has immunomodulatory effects, including suppression of the delayed type of hypersensitivity to induce anergy [23], suppression of antibody production by B lymphocytes [24], decreasing the phagocytosis by granulocytes [25], and regulating granulomonocytopoiesis [25]. Nevertheless, another ferritin-like molecule, a cloned human chimeric H-ferritin chain, PLIF (placenta immunomodulator ferritin), suppresses myelopoiesis and T cells, supporting the evidence that H-ferritin may have immunosuppressive functions [26]. The mechanisms underlying the inhibitory functions of H-ferritin are largely unknown, and they may include direct or indirect signaling via specific receptors for H-ferritin on lymphocytes [20] or the down-regulation of CD2, which acts as a cofactor for lymphocyte stimulation [27]. More recent data suggest that H-ferritin may suppress immune responses by its ability to induce production of the anti-inflammatory cytokine IL-10 in lymphocytes [28].
In addition to its suppressive effects on hematopoietic cell proliferation and differentiation, there is also evidence that H-ferritin plays an important role in chemokine receptor signaling and receptor-mediated cell migration. H-ferritin is a negative regulator of the CXC-chemokine receptor 4 (CXCR4). Thus, H-ferritin binding to CXCR4 impairs the signaling leading to the activation of mitogen-activated protein kinase (MAPK), a kinase that is known to play an important role in cell proliferation, differentiation and migration [29].
Ferritin as a pro-inflammatory mediator
A novel role for extracellular ferritin as a pro-inflammatory signaling molecule in hepatic stellate cells has been proposed by Ruddell et al.[30]. Cells treated with ferritin activated a TIM-2-independent pathway comprising PI3 kinase phosphorylation, protein kinase C zeta activation and MAPK activation, ultimately culminating in activation of nuclear factor-κB (NF-κB). Activation of NF-κB in turn enhanced the expression of pro-inflammatory mediators, including IL-1β, inducible nitric oxide synthase and others. Of great relevance is the fact that this function was independent of the iron content of ferritin, suggesting that exogenous ferritin may assume roles entirely independent of its classic role as an iron binding protein. Moreover, this study showed that L-chain-rich tissue ferritin, and recombinant H- and L-ferritin, all initiated the activation of signaling pathways, which clearly suggests a role for serum ferritin (that is constituted mainly of L-ferritin subunits) as a pro-inflammatory mediator. Also, it was proposed that ferritin may play a role in an array of inflammatory/fibrogenic states associated with infection in organs, such as the heart, lungs, kidney and pancreas, all of which have cell types similar to hepatic stellate cells that mediate the fibrogenic response to injury [17, 30].
A comprehensive analysis of the role of ferritin as a signaling molecule via TIM-2, Scara5 or via as yet unidentified receptors, will be of great interest and may lead to a better understanding of the precise role of circulating ferritin in inflammation.
Ferritin in autoimmune diseases
Hyperferritinemia is known to be associated with autoimmune diseases, such as SLE, RA and MS [3–7], and also in serological antiphospholipid syndrome (APS) [8] (Table 1). The relevance of ferritin in autoimmune diseases is also supported by the finding of autoantibodies against ferritin in different autoimmune diseases: RA [31], giant cell arteritis and polymyalgia rheumatica [32] and Takayasu arteritis [33]. Yet, their importance remains to be established.
The murine TIM gene family is linked to a locus that regulates airway hypersensitivity and the production of Th2 cytokines. Furthermore, in many of the animal autoimmune disease models in which a number of susceptibility loci have been identified, locus 11, which includes the TIM gene family, has been found to be related to susceptibility to autoimmunity [2, 34, 35]. Some polymorphisms in TIM genes are associated with immunity-related diseases, such as RA [34, 35]. Additionally, it is known that TIM-2 is a negative regulator of the cells involved in the Th2 immune reaction [2, 36, 37]. The fact that ferritin acts as an immunosuppressant, together with the finding that TIM-2 is a specific receptor for ferritin, led Recalcati et al.[2] to propose that H-ferritin may have a role in autoimmunity. Different mechanisms involving H-ferritin/TIM-2 interactions can inhibit the H-ferritin-mediated suppression of immune cells. In turn, the impaired immunosuppression may favor the loss of tolerance and the development of autoimmune diseases [2].
Ferritin may also play a role in autoimmunity through its effects on CXCR4. As previously reported, H-ferritin is a negative regulator of CXCR4. This chemokine receptor is known to be significantly up-regulated in monocytes, neutrophils, B cell subsets and plasma cells in murine models of lupus nephritis. Moreover, the treatment of these mice with an antagonist of CXCR4 ameliorated end organ disease [38].
As described above, pro-inflammatory cytokines can induce ferritin expression; in turn, ferritin may induce the expression of pro-inflammatory cytokines. Moreover, ferritin induction of anti-inflammatory cytokines (IL-10) is an important mechanism underlying the immunosuppressive effects of ferritin. There seems, therefore, to be a complex interaction between ferritin and cytokines in the control of pro-inflammatory and anti-inflammatory mediators (Figure 2). So, ferritin can be either an immunosuppressive or a pro-inflammatory molecule. These opposing effects are probably dependent on the activation of different pathways, through different receptors, possibly employing different effectors (that is, L- versus H-ferritin), and maybe different contexts. In fact, this last idea resembles the two-hit hypothesis, for instance, in vivo, for the high levels of ferritin to be pathogenic it may require a second hit, like a pro-inflammatory environment, a specific infection or maybe a particular genetic background. Indeed, this may explain why in the case of hyperferritinemia-cataract syndrome there are high levels of ferritin without an inflammatory response.
MAS, AOSD, cAPS and septic shock are characterized by life-threatening hyperinflammation with multi-organ failure. Below we will review each one of these conditions in turn and Table 2 summarizes their clinical and laboratory features.
Clinical and laboratory features in mas, AOSD, cAPS and septic shock
Macrophage activation syndrome (MAS)
Hemophagocytic syndrome, also referred to as hemophagocytic lymphohistiocytosis (HLH), represents a severe hyperinflammatory condition triggered in most cases by infectious agents. Familial forms of HLH are due to mutations occurring either in the perforin gene or in genes important for the exocytosis of cytotoxic granules. Acquired forms of HLH are encountered in association with infections, autoimmune diseases, malignant diseases and acquired immune deficiency states (for example, after organ transplantation) [62].
An acquired form of HLH that occurs in autoimmune diseases is called MAS, and is most frequently seen complicating systemic juvenile idiopathic arthritis, but this syndrome has been increasingly reported in patients with SLE, AOSD, RA and less commonly in spondyloarthropathy and vasculitis [49]. MAS, like other forms of HLH, is characterized by prolonged fever, hepatosplenomegaly, cytopenias, high levels of ferritin, triglycerides, transaminases and bilirubin, and low fibrinogen [62]. Hemophagocytosis is often absent at the disease onset but is usually found with the progression of the disease. The soluble IL-2 receptor is a valuable disease marker because of consistently increased levels during active HLH [55]. MAS is a prototype of a major immune system activation characterized by enormous levels of ferritin and severe hypercytokinemia: IL-1β, IFN-γ, TNF-α, IL-10, IL-6, IL-18, IL-2 and IL-12 [49].
The pathogenesis is poorly understood, but in both genetic as well as in the acquired cases there is an impaired or absent function in natural killer (NK) and cytotoxic T cells [55, 63].
Despite the close relationship of MAS with other forms of HLH, there are important clinical, laboratory and therapeutic differences that inclusively lead to a proposal of modified criteria for MAS [64]. In contrast to other forms of HLH, in MAS, cytopenias may be less severe initially, severe cardiac impairment appears to be common and coagulopathy is more pronounced, the C-reactive protein tend to be higher and when the cytokine profile is compared, the pro-inflammatory IL-β is elevated and the concentrations of IL-6 and TNF-α tend to be higher [61]. Also, the response to treatment is different and most of the MAS cases respond to less aggressive therapy than do the genetic forms of HLH [55].
Adult onset Still’s disease (AOSD)
AOSD is a systemic inflammatory disorder with unknown etiology, but it is hypothesized that it may be a reactive syndrome where various infectious agents may act as disease triggers in a genetically predisposed host [65]. It is characterized by fever, arthritis and a typical skin rash (non-pruritic, salmon-pink macular lesions on the trunk and extremities) correlating with diurnal fevers. Important laboratory findings include leukocytosis (predominantly neutrophils) and high levels of ferritin [40, 48]. Elevated serum ferritin levels were seen in 89% of these patients in some series, nearly half of whom had levels greater than five times normal [40]. Similarly to MAS, macrophage activation may play an important role in hyperferritinemia as well as in the pathogenesis of AOSD [59]. Heightened soluble IL-2 receptor levels, a marker of T cell activation, were also reported in two distinct studies of AOSD patients, serving as a potential marker of disease activity [66, 67]. Furthermore, reactive hemophagocytic syndrome is not uncommon in AOSD [3, 40]. Recent studies revealed a pivotal role of several pro-inflammatory cytokines on AOSD, such as IL-1, IL-6, IL-8, TNF-α and IL-18 in disease pathogenesis. There are controversial statements concerning the importance of IL-18 in distinguishing AOSD from other diagnoses [68, 69]. NK T cells are numerically and functionally deficient in AOSD, similar to those observed in SLE, RA and MAS [60].
Catastrophic antiphospholipid syndrome (cAPS)
The catastrophic variant of the APS syndrome is characterized by clinical evidence of multiple organ involvement developing over a very short period of time, histopathological evidence of multiple small vessel occlusions and laboratory confirmation of the presence of antiphospholipid antibodies (aPL), usually in high titer. Approximately 55% of cAPS cases are associated with a known trigger, such as infection or trauma [47, 58, 70]. We found that hyperferritinemia was strongly allied to the catastrophic variant of APS, present among 71% of cAPS patients with very high levels of ferritin (>1,000 ng/ml) determined in 36% of patients (although the cohort was small so the ferritin levels may be underestimated) [8]. Although patients with cAPS represent less than 1% of all APS patients, this complication can be life-threatening with a significantly increased mortality rate [46, 56, 58]. The mechanisms of cAPS are not clearly understood. The clinical manifestations of cAPS probably depend both on the organs affected by the thrombotic events, the extent of the thromboses and on the manifestations of the SIRS [47]. It is assumed that this multisystem inflammatory syndrome is caused by cytokine activation, although actual measurements of cytokine levels in very ill patients with cAPS have not been undertaken. Cytokines involved include TNF-α, IL-1, IL-6, IL-18 and macrophage-migration inhibitory factor [46].
Septic shock
Septic shock is thought to be a SIRS that is activated by invasive infection. The definition of septic shock includes sepsis-induced hypotension despite adequate fluid resuscitation, along with the presence of organ perfusion abnormalities, and ultimately cell dysfunction [54]. Hyperferritinemia is also known to be associated with sepsis [39]. Children with septic shock have hyperferritinemia and the levels of ferritin are associated with poor outcome [15]. Pro- and anti-inflammatory hypercytokinemia play a pivotal role in the pathophysiology of sepsis contributing to the dysregulation of the host immune system, inflammatory response and coagulation system [45, 71, 72]. Decreased NK cell activity is found in septic patients and is a predictor of neonatal sepsis [14].
Efficacy of similar treatment modalities for the four clinical conditions
Believing that ferritin may be pathogenic in these diseases, it would be expected that its decrease would ameliorate the clinical condition of the patients with these diseases. In fact, previously, hyperferritinemia in sepsis/MODS/MAS was successfully treated with plasma exchange, intravenous immunoglobulin (IVIG) and methylprednisone [16]. Indeed, these therapies were effective modalities, individually or in combination, in the four clinical conditions as described above (summarized in Table 3).
Corticosteroids harbor anti-inflammatory effects that rely on their ability to repress the activity of immunomodulatory transcriptor factors, such as NF-κB and activator protein (AP)-1 [89]. They are cytotoxic for lymphocytes and inhibit expression of cytokines and differentiation of dendritic cells [55]. For patients with MAS, an acquired form of HLH, it has been proven that a less cytotoxic approach is effective, in contrast to the genetic forms of HLH in which an aggressive chemoimmune therapy is required [16]. In MAS high-dose corticosteroids is often used with good response [55]. Also in AOSD, corticosteroid therapy is effective in approximately two-thirds of patients [41, 48]. Furthermore, in cAPS, corticosteroids may be considered in all patients unless an absolute contraindication exists; of course, that particular caution should be exercised in patients with infection [58]. Although some studies showed promising results with the use of corticosteroids in the treatment of sepsis and septic shock, larger studies and meta-analyses have failed to reproduce these effects. Hence, the utilization of corticosteroids in the treatment of sepsis remains controversial [82].
IVIG therapy is beneficial in a large number of autoantibody-mediated or self-reactive T cell-associated autoimmune diseases [55, 91]. Direct antitoxic effects, as well as the indirect immunomodulatory mechanisms of IVIG are the basis for the rationale to use these substances in life-threatening infections and hyperinflammatory states [84]. IVIG probably acts by cytokine- and pathogen-specific antibodies, possibly including antibodies to ferritin [55, 91]. Moreover, IVIG prevents the release of pro-inflammatory cytokines in human monocytic cells stimulated with procalcitonin [92]. IVIG is an important modality in the treatment of MAS [93], AOSD [65, 76] and cAPS [79, 80]. IVIG is not recommended in adult patients with septic shock, mainly due to the risk-benefit ratio and cost effectiveness [84].
Systemic inflammatory response is responsible for an important immunologic disturbance with the release into the bloodstream of numerous inflammatory mediators, such as cytokines, chemokines, complement components, platelet-activating factor, leukotrienes, thromboxanes and kinins. The overall concept of blood purification is, therefore, to attenuate this overwhelming systemic overflow of pro- and anti-inflammatory mediators released at the early phase of sepsis and to restore a broad-based humoral homeostasis in order to improve outcome [90]. Plasma exchange is an extracorporeal blood purification technique designed to remove various toxic and inflammatory mediators and to replenish essential compounds via the replacement plasma, which is known also to decrease ferritin levels [16]. It is a successful therapy in all four clinical conditions discussed, although in the case of the AOSD, there are only anecdotal cases [59, 73–75, 77, 78, 81, 85–88].
On the other hand, there are also differences in the treatment of these conditions, for instance, Cyclosporin A, as part of the HLH-94 protocol, has been proven to be effective for maintaining remission in genetic HLH and for children with MAS [55], but its results in AOSD are modest [65]. As well, in cAPS the anticoagulation is one of the major therapies and is not indicated in the other conditions.
Discussion
The hyperferritinemic syndrome
The four conditions: MAS, AOSD, cAPS and septic shock share similar clinical signs, symptoms and laboratory parameters (summarized in Table 2). Additionally, they respond to similar modes of therapies (Table 3). Clinically, it is difficult to distinguish between these conditions; in fact, it was previously proposed that severe sepsis, SIRS and MAS could be considered intermediate phenotypes of the same inflammatory process, a spectrum of molecular abnormalities affecting target cells killed by cytotoxic T cells and NK cells [14]. Moreover, the overlap between MAS, cAPS and sepsis has been previously reported [94, 95].
Information is emerging about the biological relevance of ferritin. Ferritin is known to be a pro-inflammatory mediator inducing expression of inflammatory molecules [30]. Yet it has opposing actions as a pro-inflammatory and as an immunosuppressant.
We believe that the very high ferritin levels in these clinical conditions are not just the product of the inflammation but rather may have a pathogenic role. Possibly, in an inflammatory environment, as observed in these diseases, the huge levels of ferritin may be involved in some sort of a loop mechanism where ferritin’s inflammatory proprieties are exacerbated, leading to an extreme expression of additional inflammatory mediators that are characteristic in the cytokine storm.
The good response to treatment with methylprednisolone, plasma exchange and IVIG supports a common pathogenic mechanism, and ferritin may be the link between them. It was previously shown that ferritin levels decreased gradually after each plasma exchange session [16]. Furthermore, IVIG may be relevant not only because antibodies against ferritin may be present, but it may also prevent the release of pro-inflammatory cytokines [92]. It is also very interesting to realize that the inhibition of the cytokines that play a central role in AOSD (IL-1 and IL-6) is an effective treatment, since they are the same cytokines known to induce ferritin expression [48]. Macrophages seem to play a major role in these four conditions. In fact, they are responsible for the production of cytokines and also appear to be of utmost importance in the production and secretion of serum ferritin.
However, not all the patients with these clinical conditions have hyperferritinemia; in fact, in about 10% of the AOSD patients the ferritin levels are normal [40]. Perhaps in this subgroup of patients the disease has a different etiology with a different pathogenesis. On the other hand, there are other diseases characterized by high levels of ferritin, such as hyperferritinemia-cataract syndrome that do not have an inflammatory response. Furthermore, the genetic forms of HLH that share clinical similarities with the four diseases discussed also have several important differences in the clinical, laboratory and, mainly, treatment response, which may suggest a distinct pathogenic features. Another clinical condition resembles these four that we have described, induced by the administration of an anti-CD28 monoclonal antibody. It led to a pro-inflammatory cytokine storm with multiorgan failure that responded to treatment with corticosteroids and hemodiafiltration with high dialysate rates and fresh frozen plasma. We may speculate that in this condition ferritin was also elevated, but it was not measured [96].
Taking this all together, we suggest that the four conditions: MAS, AOSD, cAPS and septic shock, which share common clinical and pathogenic features, should be included under a common syndrome named “Hyperferritinemic Syndrome”.
This concept of hyperferritinemia as a major contributor in the pathogenesis of these conditions may be extremely important in considering more targeted therapy. It is to be hoped that busy clinicians may appreciate the value of ferritin measurements when managing critically ill patients and that these assays may be useful in guiding therapy and predicting prognosis.
Further studies are required to understand the possible pathogenic role of ferritin in these conditions. There are many unsolved questions in this issue, such as why and how the serum ferritin is elevated, what is the composition of ferritin in the different diseases, and whether there are more receptors for ferritin and how ferritin interacts with them.
Summary
● There is increasing evidence that circulating ferritin levels may not only reflect an acute phase response but may play a critical role in inflammation.
● MAS, AOSD, cAPS and septic shock are associated with very high levels of ferritin.
● These disorders share similar clinical and laboratory presentations and respond to similar treatments, suggesting that hyperferritinemia may be involved in a common pathogenic mechanism.
● We hypothesize that the huge levels of ferritin seen in these four clinical conditions are not just a secondary product of the inflammatory process, but rather, they are part of the pathogenic mechanism.
● We propose to include these four disorders under a single nomenclature: “The Hyperferritinemic Syndrome”.
Authors’ information
Cristina Rosário, MD, is a physician (Internist) in a public hospital and has experience with several autoimmune diseases as well as with patients with severe infections. She also did in vivo and in vitro research projects on ferritin and its implications in autoimmune and inflammatory diseases during her fellowship at the Zabludowicz Center for Autoimmune Diseases.
Gisele Zandman-Goddard, MD, is a head of the Department of Medicine and has experience with autoimmune diseases and has worked in several projects of basic research on ferritin and its relevance to autoimmune diseases.
Esther G. Meyron-Holtz, PhD, works on basic research with ferritin.
David P D’Cruz, MD, is head of the Department of Autoimmune Diseases, St Thomas Hospital London, U.K. He has experience with cAPS, vasculitides and other inflammatory autoimmune diseases.
Yehuda Shoenfeld, MD, is head of a center for autoimmune diseases. He has published extensively on autoimmunity and pathogenic factors, as well as on ferritin. Recently, he has coordinated scientific projects on basic research in ferritin and its implications in autoimmune and inflammatory diseases.
Abbreviations
- AOSD:
-
Adult onset Still’s disease
- AP:
-
Activator protein
- aPL:
-
Antiphospholipid antibodies
- APS:
-
Antiphospholipid syndrome
- ARDS:
-
Acute respiratory distress syndrome
- cAPS:
-
Catastrophic antiphospholipid syndrome
- CXCR4:
-
CXC-chemokine receptor 4
- CXCL12:
-
CXC chemokine ligand 12
- DAS28:
-
Disease activity score 28
- DMARDs:
-
Disease-modifying antirheumatic drugs
- HLH:
-
Hemophagocytic lymphohistiocytosis
- IFN-γ:
-
Interferon-γ
- IL:
-
Interleukin
- IVIG:
-
Intravenous immunoglobulin
- LPS:
-
Lipopolysaccharide
- MAPK:
-
Mitogen-activated protein kinase
- MAS:
-
Macrophage activation syndrome
- MODS:
-
Multiorganic dysfunction syndrome
- MS:
-
Multiple sclerosis
- NF-kB:
-
Nuclear factor-kB
- NK:
-
Natural kill
- NO:
-
Nitric oxide
- PLIF:
-
Placenta immunomodulator ferritin
- RA:
-
Rheumatoid arthritis
- SIRS:
-
Systemic Inflammatory Response Syndrome
- SLE:
-
Systemic lupus erythematosus
- Th:
-
T helper
- TIM:
-
T cell immunoglobulin and mucin-domain
- TNF-α:
-
Tumor necrosis factor alpha.
References
Torti FM, Torti SV: Regulation of ferritin genes and protein. Blood. 2002, 99: 3505-3516.
Recalcati S, Invernizzi P, Arosio P, Cairo G: New functions for an iron storage protein: the role of ferritin in immunity and autoimmunity. J Autoimmun. 2008, 30: 84-89.
Zandman-Goddard G, Shoenfeld Y: Ferritin in autoimmune diseases. Autoimmun Rev. 2007, 6: 457-463.
Zandman-Goddard G, Shoenfeld Y: Hyperferritinemia in autoimmunity. Isr Med Assoc J. 2008, 10: 83-84.
Zandman-Goddard G, Orbach H, Agmon-Levin N, Boaz M, Amital H, Szekanecz Z, Szucs G, Rovensky J, Kiss E, Corocher N, Doria A, Stojanovich L, Ingegnoli F, Meroni PL, Rozman B, Gomez-Arbesu J, Blank M, Shoenfeld Y: Hyperferritinemia is associated with serologic antiphospholipid syndrome in SLE patients. Clin Rev Allergy Immunol. 2011, 44: 23-30.
Da Costa R, Szyper-Kravitz M, Szekanecz Z, Csepany T, Danko K, Shapira Y, Zandman-Goddard G, Orbach H, Agmon-Levin N, Shoenfeld Y: Ferritin and prolactin levels in multiple sclerosis. Isr Med Assoc J. 2011, 13: 91-95.
Orbach H, Zandman-Goddard G, Amital H, Barak V, Szekanecz Z, Szucs G, Danko K, Nagy E, Csepany T, Carvalho JF, Doria A, Shoenfeld Y: Novel biomarkers in autoimmune diseases: prolactin, ferritin, vitamin D, and TPA levels in autoimmune diseases. Ann NY Acad Sci. 2007, 1109: 385-400.
Agmon-Levin N, Rosario C, Katz BP, Zandman-Goddard G, Meroni P, Cervera R, Stojanovich L, Blank M, Pierangeli S, Praprotnik S, Meis E, Seguro L, Ruffatti A, Pengo V, Tincani A, Doria A, Shoenfeld Y: Ferritin in the antiphospholipid syndrome and its catastrophic variant (cAPS). Lupus. 2013, In press
Knovich MA, Storey JA, Coffman LG, Torti SV, Torti FM: Ferritin for the clinician. Blood Rev. 2009, 23: 95-104.
Harrison PM, Arosio P: The ferritins: molecular properties, iron storage function and cellular regulation. Biochim Biophys Acta. 1996, 1275: 161-203.
Weiss G, Goossen B, Doppler W, Fuchs D, Pantopoulos K, Werner-Felmayer G, Grünewald K, Wachter H, Hentze MW: Translational regulation via iron-responsive elements by the nitric oxide/NO-synthase pathway. EMBO J. 1993, 12: 3651-3657.
Drapier JC, Hirling H, Wietzerbin J, Kaldy P, Kuhn LC: Biosynthesis of nitric oxide activates iron regulatory factor in macrophages. EMBO J. 1993, 12: 3643-3649.
Bennett TD, Hayward KN, Farris RW, Ringold S, Wallace CA, Brogan TV: Very high serum ferritin levels are associated with increased mortality and critical care in pediatric patients. Pediatr Crit Care Med. 2011, 12: e233-e236.
Castillo L, Carcillo J: Secondary hemophagocytic lymphohistiocytosis and severe sepsis/ systemic inflammatory response syndrome/multiorgan dysfunction syndrome/macrophage activation syndrome share common intermediate phenotypes on a spectrum of inflammation. Pediatr Crit Care Med. 2009, 10: 387-392.
Garcia PC, Longhi F, Branco RG, Piva JP, Lacks D, Tasker RC: Ferritin levels in children with severe sepsis and septic shock. Acta Paediatr. 2007, 96: 1829-1831.
Demirkol D, Yildizdas D, Bayrakci B, Karapinar B, Kendirli T, Koroglu TF, Dursun O, Erkek N, Gedik H, Citak A, Kesici S, Karabocuoglu M, Carcillo JA, Turkish Secondary HLH/MAS Critical Care Study Group: Hyperferritinemia in the critically ill child with secondary hemophagocytic lymphohistiocytosis/sepsis/multiple organ dysfunction syndrome/macrophage activation syndrome: what is the treatment?. Crit Care. 2012, 16: R52.
Wang W, Knovich MA, Coffman LG, Torti FM, Torti SV: Serum ferritin: past, present and future. Biochim Biophys Acta. 2010, 1800: 760-769.
Cohen LA, Gutierrez L, Weiss A, Leichtmann-Bardoogo Y, Zhang DL, Crooks DR, Sougrat R, Morgenstern A, Galy B, Hentze MW, Lazaro FJ, Rouault TA, Meyron-Holtz EG: Serum ferritin is derived primarily from macrophages through a nonclassical secretory pathway. Blood. 2010, 116: 1574-1584.
Cozzi A, Corsi B, Levi S, Santambrogio P, Biasiotto G, Arosio P: Analysis of the biologic functions of H- and L-ferritins in HeLa cells by transfection with siRNAs and cDNAs: evidence for a proliferative role of L-ferritin. Blood. 2004, 103: 2377-2383.
Moss D, Fargion S, Fracanzani AL, Levi S, Cappellini MD, Arosio P, Powell LW, Halliday JW: Functional roles of the ferritin receptors of human liver, hepatoma, lymphoid and erythroid cells. J Inorg Biochem. 1992, 47: 219-227.
Chen TT, Li L, Chung DH, Allen CD, Torti SV, Torti FM, Cyster JG, Chen CY, Brodsky FM, Niemi EC, Nakamura MC, Seaman WE, Daws MR: TIM-2 is expressed on B cells and in liver and kidney and is a receptor for H-ferritin endocytosis. J Exp Med. 2005, 202: 955-965.
Li JY, Paragas N, Ned RM, Qiu A, Viltard M, Leete T, Drexler IR, Chen X, Sanna-Cherchi S, Mohammed F, Williams D, Lin CS, Schmidt-Ott KM, Andrews NC, Barasch J: Scara5 is a ferritin receptor mediating non-transferrin iron delivery. Dev Cell. 2009, 16: 35-46.
Morikawa K, Oseko F, Morikawa S: H- and L-rich ferritins suppress antibody production, but not proliferation, of human B lymphocytes in vitro. Blood. 1994, 83: 737-743.
Hann HW, Stahlhut MW, Lee S, London WT, Hann RS: Effects of isoferritins on human granulocytes. Cancer. 1989, 63: 2492-2496.
Broxmeyer HE, Bognacki J, Dorner MH, de Sousa M: Identification of leukemia-associated inhibitory activity as acidic isoferritins. A regulatory role for acidic isoferritins in the production of granulocytes and macrophages. J Exp Med. 1981, 153: 1426-1444.
Moroz C, Grunspan A, Zahalka MA, Traub L, Kodman Y, Yaniv I: Treatment of human bone marrow with recombinant placenta immunoregulator ferritin results in myelopoiesis and T-cell suppression through modulation of the cytokine-chemokine networks. Exp Hematol. 2006, 34: 159-166.
Wigginton JM: Reversal of ferritin-mediated immunosuppression by levamisole: a rationale for its application to management of the acquired immune deficiency syndrome (AIDS). Med Hypotheses. 1995, 44: 85-88.
Gray CP, Franco AV, Arosio P, Hersey P: Immunosuppressive effects of melanoma-derived heavy-chain ferritin are dependent on stimulation of IL-10 production. Int J Cancer. 2001, 92: 843-850.
Li R, Luo C, Mines M, Zhang J, Fan GH: Chemokine CXCL12 induces binding of ferritin heavy chain to the chemokine receptor CXCR4, alters CXCR4 signaling, and induces phosphorylation and nuclear translocation of ferritin heavy chain. J Biol Chem. 2006, 281: 37616-37627.
Ruddell RG, Hoang-Le D, Barwood JM, Rutherford PS, Piva TJ, Watters DJ, Santambrogio P, Arosio P, Ramm GA: Ferritin functions as a proinflammatory cytokine via iron-independent protein kinase C zeta/nuclear factor kappaB-regulated signaling in rat hepatic stellate cells. Hepatology. 2009, 49: 887-900.
Mewar D, Moore DJ, Young-Min S, Bertolaccini ML, Khamashta MA, Watson PF, Wilson AG: Antiferritin antibodies discovered by phage display expression cloning are associated with radiographic damage in rheumatoid arthritis. Arthritis Rheum. 2005, 52: 3868-3872.
Baerlecken NT, Linnemann A, Gross WL, Moosig F, Vazquez-Rodriguez TR, Gonzalez-Gay MA, Martin J, Kötter I, Henes JC, Melchers I, Vaith P, Schmidt RE, Witte T: Association of ferritin autoantibodies with giant cell arteritis/polymyalgia rheumatica. Ann Rheum Dis. 2012, 71: 943-947.
Baerlecken NT, Grobe K, Moosing F, Gross WL, Schmidt RE, Wittw T: High frequency of ferritin autoantibodies in Takayasu arteritis [abstract]. Arthritis Rheum. 2012, 64: S1003.
Kuchroo VK, Umetsu DT, DeKruyff RH, Freeman GJ: The TIM gene family: emerging roles in immunity and disease. Nat Rev Immunol. 2003, 3: 454-462.
Meyers JH, Sabatos CA, Chakravarti S, Kuchroo VK: The TIM gene family regulates autoimmune and allergic diseases. Trends Mol Med. 2005, 11: 362-369.
Chakravarti S, Sabatos CA, Xiao S, Illes Z, Cha EK, Sobel RA, Zheng XX, Strom TB, Kuchroo VK: Tim-2 regulates T helper type 2 responses and autoimmunity. J Exp Med. 2005, 202: 437-444.
Knickelbein JE, de Souza AJ, Tosti R, Narayan P, Kane LP: Cutting edge: inhibition of T cell activation by TIM-2. J Immunol. 2006, 177: 4966-4970.
Chong BF, Mohan C: Targeting the CXCR4/CXCL12 axis in systemic lupus erythematosus. Expert Opin Ther Targets. 2009, 13: 1147-1153.
Møller HJ, Moestrup SK, Weis N, Wejse C, Nielsen H, Pedersen SS, Attermann J, Nexø E, Kronborg G: Macrophage serum markers in pneumococcal bacteremia: prediction of survival by soluble CD163. Crit Care Med. 2006, 34: 2561-2566.
Uppal SS, Al-Mutairi M, Hayat S, Abraham M, Malaviya A: Ten years of clinical experience with adult onset Still’s disease: is the outcome improving?. Clin Rheumatol. 2007, 26: 1055-1060.
Eisen A, Amital H: Adult still disease. Diagnostic Criteria in Autoimmune Diseases. Edited by: Shoenfeld Y, Cervera R, Gershwin ME. 2008, New York, NY: Humana Press, 25-29. 1
Berkun Y, Pedeh S: Macrophage activation syndrome in juvenile idiopathic arthritis. Diagnostic Criteria in Autoimmune Diseases. Edited by: Shoenfeld Y, Cervera R, Gershwin ME. 2008, New York, NY: Humana Press, 21-24.
Lian F, Wang Y, Yang X, Xu H, Liang L: Clinical features and hyperferritinemia diagnostic cutoff points for AOSD based on ROC curve: a Chinese experience. Rheumatol Int. 2012, 32: 189-192.
Allen CE, Yu X, Kozinetz CA, McClain KL: Highly elevated ferritin levels and the diagnosis of hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2008, 50: 1227-1235.
Cinel I, Opal SM: Molecular biology of inflammation and sepsis: a primer. Crit Care Med. 2009, 37: 291-304.
Cervera R: Update on the diagnosis, treatment, and prognosis of the catastrophic antiphospholipid syndrome. Curr Rheumatol Rep. 2010, 12: 70-76.
Espinosa G, Bucciarelli S, Cervera R, Gomez-Puerta JA, Font J: Laboratory studies on pathophysiology of the catastrophic antiphospholipid syndrome. Autoimmun Rev. 2006, 6: 68-71.
Mavragani CP, Spyridakis EG, Koutsilieris M: Adult-onset Still’s disease: from pathophysiology to targeted therapies. Int J Inflamm. 2012, 2012: 879020.
Atteritano M, David A, Bagnato G, Beninati C, Frisina A, Iaria C, Bagnato G, Cascio A: Haemophagocytic syndrome in rheumatic patients. A systematic review. Eur Rev Med Pharmacol Sci. 2012, 16: 1414-1424.
Takahashi K, Kumakura S, Ishikura H, Murakawa Y, Yamauchi Y, Kobayashi S: Reactive hemophagocytosis in systemic lupus erythematosus. Intern Med. 1998, 37: 550-553.
Shimizu M, Yokoyama T, Yamada K, Kaneda H, Wada H, Wada T, Toma T, Ohta K, Kasahara Y, Yachie A: Distinct cytokine profiles of systemic-onset juvenile idiopathic arthritis-associated macrophage activation syndrome with particular emphasis on the role of interleukin-18 in its pathogenesis. Rheumatology (Oxford). 2010, 49: 1645-1653.
Maruyama J, Inokuma S: Cytokine profiles of macrophage activation syndrome associated with rheumatic diseases. J Rheumatol. 2010, 37: 967-973.
Kumakura S, Ishikura H, Kondo M, Murakawa Y, Kobayashi S: Hemophagocytosis associated with MPO-ANCA positive vasculitis in systemic sclerosis. Clin Exp Rheumatol. 2002, 20: 411-414.
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL: Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med. 2008, 2008: 783-785. Erratum in: Intensive Care Med 2008, 34:783-785
Janka GE: Hemophagocytic syndromes. Blood Rev. 2007, 21: 245-253.
Sciascia S, Lopez-Pedrera C, Roccatello D, Cuadrado MJ: Catastrophic antiphospholipid syndrome (CAPS). Best Pract Res Clin Rheumatol. 2012, 26: 535-541.
Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH, Imashuku S, Ladisch S, McClain K, Webb D, Winiarski J, Janka G: HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007, 48: 124-131.
Cervera R, Bucciarelli S, Plasin MA, Gomez-Puerta JA, Plaza J, Pons-Estel G, Shoenfeld Y, Ingelmo M, Espinos G, Catastrophic Antiphospholipid Syndrome (CAPS) Registry Project Group (European Forum On Antiphospholipid Antibodies: Catastrophic antiphospholipid syndrome (CAPS): descriptive analysis of a series of 280 patients from the “CAPS Registry”. J Autoimmun. 2009, 32: 240-245.
Kato T, Kobayashi T, Nishino H, Hidaka Y: Double-filtration plasmapheresis for resolution of corticosteroid resistant adult onset Still’s disease. Clin Rheumatol. 2006, 25: 579-582.
Lee SJ, Cho YN, Kim TJ, Park SC, Park DJ, Jin HM, Lee SS, Kee SJ, Kim N, Yoo DH, Park YW: Natural killer T cell deficiency in active adult-onset Still’s Disease: correlation of deficiency of natural killer T cells with dysfunction of natural killer cells. Arthritis Rheum. 2012, 64: 2868-2877.
Janka GE: Familial and acquired hemophagocytic lymphohistiocytosis. Eur J Pediatr. 2007, 166: 95-109.
Janka GE: Familial and acquired hemophagocytic lymphohistiocytosis. Annu Rev Med. 2012, 63: 233-246.
Schneider EM, Lorenz I, Muller-Rosenberger M, Steinbach G, Kron M, Janka-Schaub GE: Hemophagocytic lymphohistiocytosis is associated with deficiencies of cellular cytolysis but normal expression of transcripts relevant to killer-cell-induced apoptosis. Blood. 2002, 100: 2891-2898.
Ravelli A, Magni-Manzoni S, Pistorio A, Besana C, Foti T, Ruperto N, Viola S, Martini A: Preliminary diagnostic guidelines for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. J Pediatr. 2005, 146: 598-604.
Efthimiou P, Paik PK, Bielory L: Diagnosis and management of adult onset Still’s disease. Ann Rheum Dis. 2006, 65: 564-572.
Fujii T, Nojima T, Yasuoka H, Satoh S, Nakamura K, Kuwana M, Suwa A, Hirakata M, Mimori T: Cytokine and immunogenetic profiles in Japanese patients with adult Still’s disease. Association with chronic articular disease. Rheumatology. 2001, 40: 1398-1404.
Choi JH, Suh CH, Lee YM, Suh YJ, Lee SK, Kim SS, Nahm DH, Park HS: Serum cytokine profiles in patients with adult onset Still’s disease. J Rheumatol. 2003, 30: 2422-2427.
Priori R, Colafrancesco S, Perriconi C, Minniti A, Alessandri C, Iaiani G, Valesini G: Clinical and laboratory findings in a cohort of Italian patients with adult onset Still’s disease: the role of IL-18 as a disease biomarker [abstract]. Arthritis Rheum. 2012, 64: S82.
Rau M, Schiller M, Krienke S, Heyder P, Lorenz H, Blank N: Clinical manifestations but not cytokine profiles differentiate adult-onset Still’s disease and sepsis. J Rheumatol. 2010, 37: 2369-2376.
Asherson RA: The catastrophic antiphospholipid (Asherson’s) syndrome in 2004 - a review. Autoimmun Rev. 2005, 4: 48-54.
Gogos CA, Drosou E, Bassaris HP, Skoutelis A: Pro- versus anti-inflammatory cytokine profile in patients with severe sepsis: a marker for prognosis and future therapeutic options. J Infect Dis. 2000, 181: 176-180.
Lvovschi V, Arnaud L, Parizot C, Freund Y, Juillien G, Ghillani-Dalbin P, Bouberima M, Larsen M, Riou B, Gorochov G, Hausfater P: Cytokine profiles in sepsis have limited relevance for stratifying patients in the emergency department: a prospective observational study. PLoS One. 2011, 6: e28870.
Nakakura H, Ashida A, Matsumura H, Murata T, Nagatoya K, Shibahara N, Inoue T, Tamai H: A case report of successful treatment with plasma exchange for hemophagocytic syndrome associated with severe systemic juvenile idiopathic arthritis in an infant girl. Ther Apher Dial. 2009, 13: 71-76.
Song KS, Sung HJ: Effect of plasma exchange on the circulating IL-6 levels in a patient with fatal hemophagocytic syndrome associated with bile ductopenia. Ther Apher Dial. 2006, 10: 87-89.
Matsumoto Y, Naniwa D, Banno S, Sugiura Y: The efficacy of therapeutic plasmapheresis for the treatment of fatal hemophagocytic syndrome: two case reports. Ther Apher. 1998, 2: 300-304.
Vignes S, Wechsler B, Amoura Z, Papo T, Francès C, Huong DL, Veyssier P, Godeau P, Piette JC: Intravenous immunoglobulin in adult Still’s disease refractory to non-steroidal anti-inflammatory drugs. Clin Exp Rheumatol. 1998, 16: 295-298.
Ito T, Ozaki Y, Shimamoto K, Amuro H, Tanijiri T, Yokoi T, Son Y, Tajima K, Fukuhara S: Successful treatment with plasma exchange in adult-onset Still’s disease with hyper-IL-18-naemia and hyperallergic state. Mod Rheumatol. 2008, 18: 407-410.
Liu LL, Feng ML, Wang LN, Li XL, Yao L: A case report of successful treatment with plasma exchange for adult-onset Still’s disease with autoimmune hepatitis. J Clin Apher. 2010, 25: 74-76.
Orbach H, Katz U, Sherer Y, Shoenfeld Y: Intravenous immunoglobulin: adverse effects and safe administration. Clin Rev Allergy Immunol. 2005, 29: 173-184.
Katz U, Achiron A, Sherer Y, Shoenfeld Y: Safety of intravenous immunoglobulin (IVIG) therapy. Autoimmun Rev. 2007, 6: 257-259.
Uthman I, Shamseddine A, Taher A: The role of therapeutic plasma exchange in the catastrophic antiphospholipid syndrome. Transfus Apher Sci. 2005, 33: 11-17.
Russell JA: Management of sepsis. N Engl J Med. 2006, 355: 1699-1713.
Batzofin BM, Sprung CL, Weiss YG: The use of steroids in the treatment of severe sepsis and septic shock. Best Pract Res Clin Endocrinol Metab. 2011, 25: 735-743.
Toussaint S, Gerlach H: Immunoglobulins in adult sepsis and septic shock. Curr Infect Dis Rep. 2012, 14: 522-529.
Satomi A, Nagai S, Nagai T, Niikura K, Ideura T, Ogata H, Akizawa T: Effect of plasma exchange on refractory hemophagocytic syndrome complicated with myelodysplastic syndrome. Ther Apher. 1999, 3: 317-319.
Stegmayr BG: Apheresis as therapy for patients with severe sepsis and multiorgan dysfunction syndrome. Ther Apher. 2001, 5: 123-127.
Busund R, Koukline V, Utrobin U, Nedashkovsky E: Plasmapheresis in severe sepsis and septic shock: a prospective, randomised, controlled trial. Intensive Care Med. 2002, 28: 1434-1439.
Stegmayr BG, Banga R, Berggren L, Norda R, Rydvall A, Vikerfors T: Plasma exchange as rescue therapy in multiple organ failure including acute renal failure. Crit Care Med. 2003, 31: 1730-1736.
Coutinho AE, Chapman KE: The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol. 2011, 335: 2-13.
Rimmele T, Kellum JA: High-volume hemofiltration in the intensive care unit: a blood purification therapy. Anesthesiology. 2012, 116: 1377-1387.
Emmenegger U, Schaer DJ, Larroche C, Neftel KA: Haemophagocytic syndromes in adults: current concepts and challenges ahead. Swiss Med Wkly. 2005, 135: 299-314.
Murakami K, Suzuki C, Fujii A, Imada T: Intravenous immunoglobulin prevents release of proinflammatory cytokines in human monocytic cells stimulated with procalcitonin. Inflamm Res. 2012, 61: 617-622.
Emmenegger U, Frey U, Reimers A, Fux C, Semela D, Cottagnoud P, Spaeth PJ, Neftel KA: Hyperferritinemia as indicator for intravenous immunoglobulin treatment in reactive macrophage activation syndromes. Am J Hematol. 2001, 68: 4-10.
Sacks S, Finn J, Sanna G, Khamashta MA, Chowdhury F, Hunt BJ, Bell R, D’Cruz DP: Adult-onset Still’s isease complicated by haemophagocytic syndrome and catastrophic antiphospholipid syndrome resulting in four limb amputation. Isr Med Assoc J. 2013, 15: 192-194.
Zandman-Goddard G, Shoenfeld Y: Hemophagocytic syndrome with hyperferritinemia: a stormy immunological response. Isr Med Assoc J. 2013, 15: 187-188.
Suntharalingam G, Perry MR, Ward S, Brett SJ, Castello-Cortes A, Brunner MD, Panoskaltsis N: Cytokine storm in a phase 1 trial of the anti-CD28 monoclonal antibody TGN1412. N Engl J Med. 2006, 355: 1018-1028.
Acknowledgements
The authors have no acknowledgments to state.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
CR reviewed the literature and wrote the manuscript. GZ-G has experience in clinical research in ferritin and autoimmunity, and reviewed the manuscript. EGM-H has experience in basic research in ferritin and reviewed the manuscript. DPD’C contributed to the main idea and reviewed the manuscript. YS was responsible for the crystallization of the main idea and restructured the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Rosário, C., Zandman-Goddard, G., Meyron-Holtz, E.G. et al. The Hyperferritinemic Syndrome: macrophage activation syndrome, Still’s disease, septic shock and catastrophic antiphospholipid syndrome. BMC Med 11, 185 (2013). https://doi.org/10.1186/1741-7015-11-185
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1741-7015-11-185