Abstract
Background
Hernioplasty is one of the most frequent surgeries in the UK. Light-weight mesh (LWM) has the potential to reduce chronic groin pain but its cost-effectiveness compared with heavy-weight mesh (HWM) is unknown.
Objective
Our objective was to conduct a cost-utility analysis between laparoscopic hernioplasty with HWM and LWM for unilateral inguinal hernias.
Methods
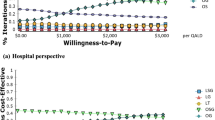
A Markov model simulated costs and health outcomes over a period of 1 year (2012) from the societal and National Health Service (NHS) perspective (England). The main outcome was cost per quality-adjusted life-year (QALY) gained. Surgery results were gleaned from the randomized control trial by Bittner et al. Other input parameters were drawn from the literature and public sources of the NHS.
Results
From the societal perspective, LWM induces lower incremental costs (−£88.85) than HWM but yields a slightly smaller incremental effect (−0.00094 QALYs). The deterministic incremental cost-effectiveness ratio (ICER) for HWM compared with LWM amounts to £94,899 per QALY, while the probabilistic ICER is £118,750 (95 % confidence interval [CI] £57,603–180,920). Owing to the withdrawal of productivity losses from the NHS perspective, LWM causes higher incremental costs (£13.09) and an inferior incremental effect (−0.00093), resulting in a dominance of HWM over LWM (ICER 95 % CI −£12,382 to −£21,590).
Conclusions
There is no support for the adoption of LWM as standard treatment from an NHS perspective. However, given the small differences between HWM and LWM, LWM has at least the potential of improving patient outcomes and reducing expenditure from the societal perspective.




Similar content being viewed by others
References
PubMed Health ADAM Medical Encyclopedia. Hernia [Internet]. 2012 [cited 2013 Jun 17]. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001956/.
PubMed Health ADAM Medical Encyclopedia. Inguinal Hernia Repair [Internet]. 2013. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0004652/.
Kingsnorth AN, Gray MR, Nott DM. Prospective randomized trial comparing the Shouldice technique and plication darn for inguinal hernia. Br J Surg. 1992;79:1068–70.
National Institute for Clinical Excellence (NICE). NICE implementation uptake report: Laparoscopic surgery for inguinal hernia repair [Internet]. 2010. http://guidance.nice.org.uk/TA83.
National Institute for Clinical Excellence (NICE). Laparoscopic surgery for inguinal hernia repair TA83 - 6 Implications for the NHS [Internet]. 2004. http://publications.nice.org.uk/laparoscopic-surgery-for-inguinal-hernia-repair-ta83/implications-for-the-nhs.
Amid PK, Hiatt JR. New understanding of the causes and surgical treatment of postherniorrhaphy inguinodynia and orchalgia. J Am Coll Surg. 2007;205:381–5.
Agency for Health Care Research and Quality (AHCRQ). Evidence-based Practice Center Systematic Review Protocol- Project Title: Comparative Effectiveness of Surgical Options for Inguinal Hernia [Internet]. http://www.effectivehealthcare.ahrq.gov/ehc/products/244/660/Inguinal-Hernia_Protocol%20Amendment_8%2015%2011.pdf.
McCormack K, Scott NW, Go PM, Ross S, Grant AM, EU Hernia Trialists Collaboration. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev. 2003;CD001785.
Aasvang E, Kehlet H. Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth. 2005;95:69–76.
Laparoscopic versus open repair of groin hernia: a randomised comparison. The MRC Laparoscopic Groin Hernia Trial Group. Lancet. 1999;354:185–90.
EU Hernia Trialists Collaboration. Repair of groin hernia with synthetic mesh: meta-analysis of randomized controlled trials. Ann Surg. 2002;235:322–32.
Schmedt CG, Sauerland S, Bittner R. Comparison of endoscopic procedures vs Lichtenstein and other open mesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Surg Endosc. 2005;19:188–99.
Schrenk P, Woisetschläger R, Rieger R, Wayand W. Prospective randomized trial comparing postoperative pain and return to physical activity after transabdominal preperitoneal, total preperitoneal or Shouldice technique for inguinal hernia repair. Br J Surg. 1996;83:1563–6.
National Institute for Clinical Excellence (NICE). Technology Appraisal 83—Laparoscopic surgery for inguinal hernia repair [Internet]. 2004. http://guidance.nice.org.uk/TA83.
Brown CN, Finch JG. Which mesh for hernia repair? Ann R Coll Surg Engl. 2010;92:272–8.
Klosterhalfen B, Junge K, Klinge U. The lightweight and large porous mesh concept for hernia repair. Expert Rev Med Devices. 2005;2:103–17.
Agarwal BB, Agarwal KA, Mahajan KC. Prospective double-blind randomized controlled study comparing heavy- and lightweight polypropylene mesh in totally extraperitoneal repair of inguinal hernia: early results. Surg Endosc. 2009;23:242–7.
Akolekar D, Kumar S, Khan LR, de Beaux AC, Nixon SJ. Comparison of recurrence with lightweight composite polypropylene mesh and heavyweight mesh in laparoscopic totally extraperitoneal inguinal hernia repair: an audit of 1,232 repairs. Hernia. 2008;12:39–43.
Langenbach MR, Schmidt J, Ubrig B, Zirngibl H. Sixty-month follow-up after endoscopic inguinal hernia repair with three types of mesh: a prospective randomized trial. Surg Endosc. 2008;22:1790–7.
Sajid MS, Leaver C, Baig MK, Sains P. Systematic review and meta-analysis of the use of lightweight versus heavyweight mesh in open inguinal hernia repair. Br J Surg. 2012;99:29–37.
Bittner R, Schmedt C-G, Leibl BJ, Schwarz J. Early postoperative and one year results of a randomized controlled trial comparing the impact of extralight titanized polypropylene mesh and traditional heavyweight polypropylene mesh on pain and seroma production in laparoscopic hernia repair (TAPP). World J Surg. 2011;35:1791–7.
Sajid MS, Kalra L, Parampalli U, Sains PS, Baig MK. A systematic review and meta-analysis evaluating the effectiveness of lightweight mesh against heavyweight mesh in influencing the incidence of chronic groin pain following laparoscopic inguinal hernia repair. Am J Surg. 2013;205:726–36.
Chowbey PK, Garg N, Sharma A, Khullar R, Soni V, Baijal M, et al. Prospective randomized clinical trial comparing lightweight mesh and heavyweight polypropylene mesh in endoscopic totally extraperitoneal groin hernia repair. Surg Endosc. 2010;24:3073–9.
Chui LB, Ng WT, Sze YS, Yuen KS, Wong YT, Kong CK. Prospective, randomized, controlled trial comparing lightweight versus heavyweight mesh in chronic pain incidence after TEP repair of bilateral inguinal hernia. Surg Endosc. 2010;24:2735–8.
Currie A, Andrew H, Tonsi A, Hurley PR, Taribagil S. Lightweight versus heavyweight mesh in laparoscopic inguinal hernia repair: a meta-analysis. Surg Endosc. 2012;26:2126–33.
Gao M, Han J, Tian J, Yang K. Vypro II mesh for inguinal hernia repair: a meta analysis of randomized controlled trials. Ann Surg. 2010;251:838–42.
Peeters E, Spiessens C, Oyen R, De Wever L, Vanderschueren D, Penninckx F, et al. Laparoscopic inguinal hernia repair in men with lightweight meshes may significantly impair sperm motility: a randomized controlled trial. Ann Surg. 2010;252:240–6.
Bittner R, Leibl BJ, Kraft B, Schwarz J. One-year results of a prospective, randomised clinical trial comparing four meshes in laparoscopic inguinal hernia repair (TAPP). Hernia. 2011;15:503–10.
Champault G, Bernard C, Rizk N, Polliand C. Inguinal hernia repair: the choice of prosthesis outweighs that of technique. Hernia. 2007;11:125–8.
Bringman S, Wollert S, Osterberg J, Heikkinen T. Early results of a randomized multicenter trial comparing Prolene and VyproII mesh in bilateral endoscopic extraperitoneal hernioplasty (TEP). Surg Endosc. 2005;19:536–40.
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13:343–403.
Gilbert AI, Young J, Graham MF, Divilio LT, Patel B. Combined anterior and posterior inguinal hernia repair: intermediate recurrence rates with three groups of surgeons. Hernia. 2004;8:203–7.
Kehlet H, Bay-Nielsen M, Danish Hernia Database Collaboration. Nationwide quality improvement of groin hernia repair from the Danish Hernia Database of 87,840 patients from 1998 to 2005. Hernia. 2008;12:1–7.
Nikkolo C, Lepner U, Murruste M, Vaasna T, Seepter H, Tikk T. Randomised clinical trial comparing lightweight mesh with heavyweight mesh for inguinal hernioplasty. Hernia. 2010;14:253–8.
O’Dwyer PJ, Kingsnorth AN, Molloy RG, Small PK, Lammers B, Horeyseck G. Randomized clinical trial assessing impact of a lightweight or heavyweight mesh on chronic pain after inguinal hernia repair. Br J Surg. 2005;92:166–70.
Ferzli GS, Edwards ED, Khoury GE. Chronic pain after inguinal herniorrhaphy. J Am Coll Surg. 2007;205:333–41.
Poobalan AS, Bruce J, Smith WCS, King PM, Krukowski ZH, Chambers WA. A review of chronic pain after inguinal herniorrhaphy. Clin J Pain. 2003;19:48–54.
Kehlet H. Chronic pain after groin hernia repair. Br J Surg. 2008;95:135–6.
Aroori S, Spence RAJ. Chronic pain after hernia surgery–an informed consent issue. Ulster Med J. 2007;76:136–40.
Bay-Nielsen M, Perkins FM, Kehlet H. Danish Hernia Database. Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg. 2001;233:1–7.
Kumar S, Wilson RG, Nixon SJ, Macintyre IMC. Chronic pain after laparoscopic and open mesh repair of groin hernia. Br J Surg. 2002;89:1476–9.
Rosin D. Risk factors for chronic pain after open ventral hernia repair by underlay mesh placement. World J Surg. 2012;36:1555–6.
Gronnier C, Wattier J-M, Favre H, Piessen G, Mariette C. Risk factors for chronic pain after open ventral hernia repair by underlay mesh placement. World J Surg. 2012;36:1548–54.
Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986;3:S1–226.
Loos MJA, Roumen RMH, Scheltinga MRM. Classifying post-herniorrhaphy pain syndromes following elective inguinal hernia repair. World J Surg. 2007;31:1760–1765 (discussion 1766–1767).
Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Economic evaluation using decision analytic modelling. In: Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press; 2011. p. 227–315.
Jenkins JT, O’Dwyer PJ. Inguinal hernias. BMJ. 2008;336:269–72.
National Institute for Clinical Excellence (NICE). Guide to the methods of technology appraisal [Internet]. 2004. Available from: http://www.nice.org.uk/aboutnice/howwework/devnicetech/technologyappraisalprocessguides/guide_to_the_methods_of_technology_appraisal_reference_n0515.jsp.
Medical Research Council Laparoscopic Groin Hernia Trial Group. Cost-utility analysis of open versus laparoscopic groin hernia repair: results from a multicentre randomized clinical trial. Br J Surg. 2001;88:653–61.
McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al. Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation. Health Technol Assess. 2005;9:1–203, iii–iv.
Department of Health. Hospital and Community Health Service (HCHS) Index [Internet]. 2012 [cited 2013 Jun 18]. http://www.info.doh.gov.uk/doh/finman.nsf/Newsletters?OpenView&Start=13.1&ExpandView.
Department of Health. Payment by Results (PbR) operational guidance and tariffs. PbR 2012-13 tariff information spreadsheet [Internet]. 2012 [cited 2013 Aug 7]. https://www.gov.uk/government/publications/confirmation-of-payment-by-results-pbr-arrangements-for-2012-13.
Koch A, Bringman S, Myrelid P, Smeds S, Kald A. Randomized clinical trial of groin hernia repair with titanium-coated lightweight mesh compared with standard polypropylene mesh. Br J Surg. 2008;95:1226–31.
Bright E, Reddy VM, Wallace D, Garcea G, Dennison AR. The incidence and success of treatment for severe chronic groin pain after open, transabdominal preperitoneal, and totally extraperitoneal hernia repair. World J Surg. 2010;34:692–6.
Song D, Greilich NB, White PF, Watcha MF, Tongier WK. Recovery profiles and costs of anesthesia for outpatient unilateral inguinal herniorrhaphy. Anesth Analg. 2000;91:876–81.
NHS Electronic Drug Tariff [Internet]. National Health System (NHS) Electronic Drug Tariff. (2012). 2012. http://www.ppa.org.uk/ppa/edt_intro.htm.
NHS CKS Clinical Knowledge Summary. Depo-Medrone with Lidocaine suspension for injection 1ml vials [Internet]. 2012. http://www.cks.nhs.uk/gout/drugs_in_this_topic/scenario_acute_gout/depo_medrone_with_lidocaine_suspension_for_injection_1ml_vials.
NHS CKS Clinical Knowledge Summary. AMITRIPTYLINE HYDROCHLORIDE [Internet]. 2012. https://www.evidence.nhs.uk/formulary/bnf/current/4-central-nervous-system/43-antidepressant-drugs/431-tricyclic-and-related-antidepressant-drugs/tricyclic-antidepressants/amitriptyline-hydrochloride.
Office for National Statistics. Annual Survey of Hours and Earnings, 2012 Provisional Results [Internet]. 2012. http://www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-280149.
Schopf S, von Ahnen T, von Ahnen M, Schardey H. Chronic pain after laparoscopic transabdominal preperitoneal hernia repair: a randomized comparison of light and extralight titanized polypropylene mesh. World J Surg. 2011;35:302–10.
Courtney CA, Duffy K, Serpell MG, O’Dwyer PJ. Outcome of patients with severe chronic pain following repair of groin hernia. Br J Surg. 2002;89:1310–4.
Grant AM, Scott NW, O’Dwyer PJ, MRC Laparoscopic Groin Hernia Trial Group. Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair of groin hernia. Br J Surg. 2004;91:1570–4.
Naimark DMJ, Bott M, Krahn M. The half-cycle correction explained: two alternative pedagogical approaches. Med Decis Making. 2008;28:706–12.
Asencio F, Aguiló J, Peiró S, Carbó J, Ferri R, Caro F, et al. Open randomized clinical trial of laparoscopic versus open incisional hernia repair. Surg Endosc. 2009;23:1441–8.
Briggs AH, Claxton K, Sculpher MJ. Decision modelling for health economic evaluation. Oxford: Oxford University Press; 2006.
Briggs A, Nixon R, Dixon S, Thompson S. Parametric modelling of cost data: some simulation evidence. Health Econ. 2005;14:421–8.
Deb P, Burgess J. A Quasi-Experimental Comparison of Econometric Models for Health Care Expenditures. Hunter College Department of Economics Working Papers [Internet]. 2003;1–30. http://arrow.hunter.cuny.edu/research/papers/HunterEconWP212.pdf.
Fu L, Moncher R. Severity distributions for GLMs: Gamma or Lognormal? Evidence from Monte Carlo simulations. Casualty Actuarial Society discussion paper program. 2004;149–230.
Polsky D, Glick HA, Willke R, Schulman K. Confidence intervals for cost-effectiveness ratios: a comparison of four methods. Health Econ. 1997;6:243–52.
National Institute for Clinical Excellence (NICE). Briefing paper for the Methods Working Party on the Cost Effectiveness Threshold. [Internet]. 2007. http://www.nice.org.uk/media/4A6/41/CostEffectivenessThresholdFinalPaperTabledAtWPMeeting5Sep3907KT.pdf.
Heitjan DF, Moskowitz AJ, Whang W. Problems with interval estimates of the incremental cost-effectiveness ratio. Med Decis Making. 1999;19:9–15.
Briggs A, Fenn P. Confidence intervals or surfaces? Uncertainty on the cost-effectiveness plane. Health Econ. 1998;7:723–40.
Macintyre IMC. Best practice in groin hernia repair. Br J Surg. 2003;90:131–2.
Stinson JN, Kavanagh T, Yamada J, Gill N, Stevens B. Systematic review of the psychometric properties, interpretability and feasibility of self-report pain intensity measures for use in clinical trials in children and adolescents. Pain. 2006;125:143–57.
Kehlet H, Bay-Nielsen M, Kingsnorth A. Chronic postherniorrhaphy pain–a call for uniform assessment. Hernia. 2002;6:178–81.
Fränneby U, Gunnarsson U, Andersson M, Heuman R, Nordin P, Nyrén O, et al. Validation of an Inguinal Pain Questionnaire for assessment of chronic pain after groin hernia repair. Br J Surg. 2008;95:488–93.
Balakrishnan S, Singhal T, Samdani T, Hussain A, Shuaib S, Grandy-Smith S, et al. Laparoscopic inguinal hernia repair: over a thousand convincing reasons to go on. Hernia. 2008;12:493–8.
Wake BL, McCormack K, Fraser C, Vale L, Perez J, Grant AM. Transabdominal pre-peritoneal (TAPP) vs totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair. Cochrane Database Syst Rev. 2005;CD004703.
Taylor C, Layani L, Liew V, Ghusn M, Crampton N, White S. Laparoscopic inguinal hernia repair without mesh fixation, early results of a large randomised clinical trial. Surg Endosc. 2008;22:757–62.
Scheidbach H, Tamme C, Tannapfel A, Lippert H, Köckerling F. In vivo studies comparing the biocompatibility of various polypropylene meshes and their handling properties during endoscopic total extraperitoneal (TEP) patchplasty: an experimental study in pigs. Surg Endosc. 2004;18:211–20.
Heikkinen T, Wollert S, Osterberg J, Smedberg S, Bringman S. Early results of a randomised trial comparing Prolene and VyproII-mesh in endoscopic extraperitoneal inguinal hernia repair (TEP) of recurrent unilateral hernias. Hernia. 2006;10:34–40.
Author contributions
DA contributed to the conception and design of the study, as well as to synthesis, interpretation of the data, statistical analysis, and drafting of the manuscript. TS contributed to the statistical analysis, interpretation of the results and critical revision of the manuscript. DA takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study funding
This study has not received any funding.
Conflicts of interest
The authors declare they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Achelrod, D., Stargardt, T. Cost-Utility Analysis Comparing Heavy-Weight and Light-Weight Mesh in Laparoscopic Surgery for Unilateral Inguinal Hernias. Appl Health Econ Health Policy 12, 151–163 (2014). https://doi.org/10.1007/s40258-014-0082-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-014-0082-0