Abstract
Objective
Anecdotal evidence suggests that the training of young surgeons in Upper GI is not homogeneous across the world. This survey aimed to investigate the different training programs and the level of satisfaction of young surgeons with their surgical and scientific education pathway.
Design
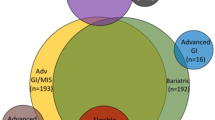
A multiple-choice and single best answer format questionnaire was sent to 36 Upper GI chairs from international referral centres and then forwarded to young surgeons (attending physician less than 40 years old). The same questionnaire containing 5 main topics (demographics, residency, fellowship, academic research and activities, manual skill improvement) was posted online on a Surveymonkey website.
Setting
San Luigi University Hospital, Orbassano (Turin), Italy; Tertiary University Hospital.
Results
Fourteen replies were received from colleagues in 36 referral centres (39% response rate) and 65 voluntary answers from the survey monkey platform. During residency training, only 43% of residents had a specific training in upper GI tract surgery, which was characterized by a small number of interventions performed both with trainer scrubbed and unscrubbed. Fellowship programmes were undertaken by 49% of participants and 64% spent this training period abroad. Operative experience was reported by nearly all respondents with only 27% performing > 10 gastrectomies and only 11% performing > 10 oesophagectomies with the trainer scrubbed. The majority attended less than 10 meetings (58%), and 70% of them published less than 5 papers.
Conclusions
The present survey reveals that the young surgeons of the twenty-first century face many hurdles during their surgical training. Overall, the surgical education settings are limited for both practical and scientific training for upper GI trainees. As a result, it is not possible to train in upper GI surgery to a level of competent independent practice.

Similar content being viewed by others
References
Begg CB, Cramer LD, Hoskins WJ, Brennan MF (1998) Impact of hospital volume on operative mortality for major cancer surgery. JAMA 280:1747–1751. https://doi.org/10.1001/jama.280.20.1747
Tol JAMG, Van Gulik TM, Busch ORC, Gouma DJ (2012) Centralization of highly complex low-volume procedures in upper gastrointestinal surgery. A summary of systematic reviews and meta-analyses. Dig Surg 29:374–383. https://doi.org/10.1159/000343929
(2011) Abstracts of the annual scientific meeting of the association of upper gastrointestinal surgeons for Great Britain and Ireland. September 15-16, 2011. Belfast, UK. Br J Surg 98 Suppl 7:1–55
Montorsi M, De Manzini N (2019) The general surgery residency program in italy: a changing scenario. Updates Surg 71:195–196
Cogbill TH, Klingensmith ME, Jones AT, et al (2015) Resident preparation for careers in general surgery: a survey of program directors. J Surg Educat Elsevier Inc, pp e251–e257
Brochu A, Aggarwal R (2018) Research during general surgery residency: a Web-based review of opportunities, structure and outputs. J Surg Res 223:149–154. https://doi.org/10.1016/j.jss.2017.10.024
General Surgery Training Program|Surgery at Johns Hopkins Medicine. https://www.hopkinsmedicine.org/surgery/education/residency/general-surgery/. Accessed 5 Dec 2020
Surgical Residency Program. https://www.massgeneral.org/surgery/education-and-training/surgical-residency-program. Accessed 5 Dec 2020
Kim J-P (2004) Surgery in Korea. Arch Surg 139:336–340. https://doi.org/10.1001/archsurg.139.3.336
Poudel S, Hirano S, Kurashima Y et al (2019) A snapshot of surgical resident training in Japan: results of a national-level needs assessment survey. Surg Today 49:870–876. https://doi.org/10.1007/s00595-019-01819-4
Wijnhoven BPL (2019) Surgical training and research in The Netherlands. Keio J Med 68:68. https://doi.org/10.2302/kjm.68-005-ABST
Greensmith M, Cho J, Hargest R (2016) Changes in surgical training opportunities in Britain and South Africa. Int J Surg 25:76–81
Goldstein AM, Blair AB, Keswani SG et al (2019) A roadmap for aspiring surgeon-scientists in today’s healthcare environment. Ann Surg 269:66–72
Qadan M, Davies AR, Polk HC et al (2018) Cancer care in the developed world: a comparison of surgical oncology training programs. Am J Surg 215:1–7. https://doi.org/10.1016/j.amjsurg.2017.05.004
Allum W, Hornby S, Khera G et al (2013) General surgery logbook survey. Bull R Coll Surg Engl 95:1–6. https://doi.org/10.1308/147363513x13500508920095
Kim CY, Nam BH, Cho GS et al (2016) Learning curve for gastric cancer surgery based on actual survival. Gastric Cancer 19:631–638. https://doi.org/10.1007/s10120-015-0477-0
Van Workum F, Stenstra MHBC, Berkelmans GHK et al (2019) Learning curve and associated morbidity of minimally invasive esophagectomy: a retrospective multicenter study. Ann Surg 269:88–94. https://doi.org/10.1097/SLA.0000000000002469
Lee GI, Lee MR (2018) Can a virtual reality surgical simulation training provide a self-driven and mentor-free skills learning? Investigation of the practical influence of the performance metrics from the virtual reality robotic surgery simulator on the skill learning and associated cognitive workloads. Surg Endosc 32:62–72. https://doi.org/10.1007/s00464-017-5634-6
O’Sullivan KE, Byrne JS, Walsh TN (2013) Basic surgical training in Ireland: the impact of operative experience, training program allocation and mentorship on trainee satisfaction. Ir J Med Sci 182:687–692. https://doi.org/10.1007/s11845-013-0956-4
Trends in Surgeon Wellness (Take a Sad Song and Make It Better): a comparison of surgical residents, fellows, and attendings—PubMed. https://pubmed-ncbi-nlm-nih-gov.bibliopass.unito.it/31267897/. Accessed 26 Jun 2020
Hikmet N, Chen SK (2003) An investigation into low mail survey response rates of information technology users in health care organizations. Int J Med Inform 72:29–34. https://doi.org/10.1016/j.ijmedinf.2003.09.002
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
The study was approved by the Ethics committee and review board of the coordinating center.
Informed consent
For this type of study informed consent is not required. By completing the questionnaire that implies proper consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Reddavid, R., Allum, W., Polom, K. et al. Upper GI training of young surgeons: a reality full of hurdles. An international survey. Updates Surg 73, 627–637 (2021). https://doi.org/10.1007/s13304-020-00955-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-020-00955-8