Abstract
Background
While it is often claimed that virtual reality (VR) training system can offer self-directed and mentor-free skill learning using the system’s performance metrics (PM), no studies have yet provided evidence-based confirmation. This experimental study investigated what extent to which trainees achieved their self-learning with a current VR simulator and whether additional mentoring improved skill learning, skill transfer and cognitive workloads in robotic surgery simulation training.
Methods
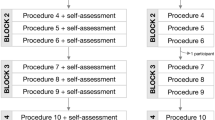
Thirty-two surgical trainees were randomly assigned to either the Control-Group (CG) or Experiment-Group (EG). While the CG participants reviewed the PM at their discretion, the EG participants had explanations about PM and instructions on how to improve scores. Each subject completed a 5-week training using four simulation tasks. Pre- and post-training data were collected using both a simulator and robot. Peri-training data were collected after each session. Skill learning, time spent on PM (TPM), and cognitive workloads were compared between groups.
Results
After the simulation training, CG showed substantially lower simulation task scores (82.9 ± 6.0) compared with EG (93.2 ± 4.8). Both groups demonstrated improved physical model tasks performance with the actual robot, but the EG had a greater improvement in two tasks. The EG exhibited lower global mental workload/distress, higher engagement, and a better understanding regarding using PM to improve performance. The EG’s TPM was initially long but substantially shortened as the group became familiar with PM.
Conclusion
Our study demonstrated that the current VR simulator offered limited self-skill learning and additional mentoring still played an important role in improving the robotic surgery simulation training.





Similar content being viewed by others
References
Ahmed K, Khan MS, Vats A, Nagpal K, Priest O, Patel V, Vecht JA, Ashrafian H, Yang GZ, Athanasiou T, Darzi A (2009) Current status of robotic assisted pelvic surgery and future developments. Int J Surg 7(5):431–440. doi:10.1016/j.ijsu.2009.08.008
Patel VR, Tully AS, Holmes R, Lindsay J (2005) Robotic radical prostatectomy in the community setting–the learning curve and beyond: initial 200 cases. J Urol 174(1):269–272. doi:10.1097/01.ju.0000162082.12962.40
Patel MN, Bhandari M, Menon M, Rogers CG (2009) Robotic-assisted partial nephrectomy. BJU Int 103(9):1296–1311. doi:10.1111/j.1464-410X.2009.08584.x
Anger JT, Mueller ER, Tarnay C, Smith B, Stroupe K, Rosenman A, Brubaker L, Bresee C, Kenton K (2014) Robotic compared with laparoscopic sacrocolpopexy: a randomized controlled trial. Obstet Gynecol 123(1):5–12. doi:10.1097/AOG.0000000000000006
Martino MA, Berger EA, McFetridge JT, Shubella J, Gosciniak G, Wejkszner T, Kainz GF, Patriarco J, Thomas MB, Boulay R (2014) A comparison of quality outcome measures in patients having a hysterectomy for benign disease: robotic vs. non-robotic approaches. J Minim Invasive Gynecol 21(3):389–393. doi:10.1016/j.jmig.2013.10.008
Ma J, Shukla PJ, Milsom JW (2011) The evolving role of robotic colorectal surgery. Dis Colon Rectum 54(3):376–377. doi:10.1007/DCR.0b013e318204a8d5
Wilson EB (2009) The evolution of robotic general surgery. Scand J Surg 98(2):125–129
You JY, Lee HY, Son GS, Lee JB, Bae JW, Kim HY (2013) Comparison of robotic adrenalectomy with traditional laparoscopic adrenalectomy with a lateral transperitoneal approach: a single-surgeon experience. Int J Med Robot Comput Assist Surg MRCAS 9(3):345–350. doi:10.1002/rcs.1497
Orady M, Hrynewych A, Nawfal AK, Wegienka G (2012) Comparison of robotic-assisted hysterectomy to other minimally invasive approaches. J Soc Laparoendosc Surg 16(4):542–548. doi:10.4293/108680812X13462882736899
Dulan G, Rege RV, Hogg DC, Gilberg-Fisher KM, Arain NA, Tesfay ST, Scott DJ (2012) Developing a comprehensive, proficiency-based training program for robotic surgery. Surgery 152(3):477–488. doi:10.1016/j.surg.2012.07.028
Rashid HH, Leung YY, Rashid MJ, Oleyourryk G, Valvo JR, Eichel L (2006) Robotic surgical education: a systematic approach to training urology residents to perform robotic-assisted laparoscopic radical prostatectomy. Urology 68(1):75–79. doi:10.1016/j.urology.2006.01.057
Antiel RM, Van Arendonk KJ, Reed DA, Terhune KP, Tarpley JL, Porterfield JR, Hall DE, Joyce DL, Wightman SC, Horvath KD, Heller SF, Farley DR (2012) Surgical training, duty-hour restrictions, and implications for meeting the Accreditation Council for Graduate Medical Education core competencies: views of surgical interns compared with program directors. Arch Surg 147(6):536–541. doi:10.1001/archsurg.2012.89
Ahmed N, Devitt KS, Keshet I, Spicer J, Imrie K, Feldman L, Cools-Lartigue J, Kayssi A, Lipsman N, Elmi M, Kulkarni AV, Parshuram C, Mainprize T, Warren RJ, Fata P, Gorman MS, Feinberg S, Rutka J (2014) A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg 259(6):1041–1053. doi:10.1097/SLA.0000000000000595
Lee JY, Mucksavage P, Sundaram CP, McDougall EM (2011) Best practices for robotic surgery training and credentialing. J Urol 185(4):1191–1197. doi:10.1016/j.juro.2010.11.067
Liu JJ, Gonzalgo ML (2011) Minimally invasive training in urologic oncology. Arch Esp Urol 64(9):865–868
Schreuder HW, Oei G, Maas M, Borleffs JC, Schijven MP (2011) Implementation of simulation in surgical practice: minimally invasive surgery has taken the lead: the Dutch experience. Med Teach 33(2):105–115. doi:10.3109/0142159X.2011.550967
Johnson E (2007) Surgical simulators and simulated surgeons: reconstituting medical practice and practitioners in simulations. Soc Stud Sci 37(4):585–608
Gallagher AG, Ritter EM, Champion H, Higgins G, Fried MP, Moses G, Smith CD, Satava RM (2005) Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg 241(2):364–372
van Empel PJ, Verdam MG, Strypet M, van Rijssen LB, Huirne JA, Scheele F, Bonjer HJ, Meijerink WJ (2012) Voluntary autonomous simulator based training in minimally invasive surgery, residents’ compliance and reflection. J Surg Educ 69(4):564–570. doi:10.1016/j.jsurg.2012.04.011
Chan B, Martel G, Poulin EC, Mamazza J, Boushey RP (2010) Resident training in minimally invasive surgery: a survey of Canadian department and division chairs. Surg Endosc 24(3):499–503. doi:10.1007/s00464-009-0611-3
Rosenthal R, Schafer J, Hoffmann H, Vitz M, Oertli D, Hahnloser D (2013) Personality traits and virtual reality performance. Surg Endosc 27(1):222–230. doi:10.1007/s00464-012-2424-z
Pitzul KB, Grantcharov TP, Okrainec A (2012) Validation of three virtual reality Fundamentals of Laparoscopic Surgery (FLS) modules. Stud Health Technol Inform 173:349–355
Brinkman WM, Buzink SN, Alevizos L, de Hingh IH, Jakimowicz JJ (2012) Criterion-based laparoscopic training reduces total training time. Surg Endosc 26(4):1095–1101. doi:10.1007/s00464-011-2005-6
Kang SG, Yang KS, Ko YH, Kang SH, Park HS, Lee JG, Kim JJ, Cheon J (2012) A study on the learning curve of the robotic virtual reality simulator. J Laparoendosc Adv Surg Tech Part A 22(5):438–442. doi:10.1089/lap.2011.0452
Lerner MA, Ayalew M, Peine WJ, Sundaram CP (2010) Does training on a virtual reality robotic simulator improve performance on the da Vinci surgical system? J Endourol 24(3):467–472. doi:10.1089/end.2009.0190
Hung AJ, Zehnder P, Patil MB, Cai J, Ng CK, Aron M, Gill IS, Desai MM (2011) Face, content and construct validity of a novel robotic surgery simulator. J Urol 186(3):1019–1024. doi:10.1016/j.juro.2011.04.064
Kenney PA, Wszolek MF, Gould JJ, Libertino JA, Moinzadeh A (2009) Face, content, and construct validity of dV-trainer, a novel virtual reality simulator for robotic surgery. Urology 73(6):1288–1292. doi:10.1016/j.urology.2008.12.044
Perrenot C, Perez M, Tran N, Jehl JP, Felblinger J, Bresler L, Hubert J (2012) The virtual reality simulator dV-Trainer((R)) is a valid assessment tool for robotic surgical skills. Surg Endosc 26(9):2587–2593. doi:10.1007/s00464-012-2237-0
Lee JY, Mucksavage P, Kerbl DC, Huynh VB, Etafy M, McDougall EM (2012) Validation study of a virtual reality robotic simulator–role as an assessment tool? J Urol 187(3):998–1002. doi:10.1016/j.juro.2011.10.160
Brinkman WM, Luursema JM, Kengen B, Schout BM, Witjes JA, Bekkers RL (2013) da Vinci skills simulator for assessing learning curve and criterion-based training of robotic basic skills. Urology 81(3):562–566. doi:10.1016/j.urology.2012.10.020
Stefanidis D, Wang F, Korndorffer JR Jr, Dunne JB, Scott DJ (2010) Robotic assistance improves intracorporeal suturing performance and safety in the operating room while decreasing operator workload. Surg Endosc 24(2):377–382. doi:10.1007/s00464-009-0578-0
Stefanidis D, Hope WW, Scott DJ (2011) Robotic suturing on the FLS model possesses construct validity, is less physically demanding, and is favored by more surgeons compared with laparoscopy. Surg Endosc 25(7):2141–2146. doi:10.1007/s00464-010-1512-1
Patel YR, Donias HW, Boyd DW, Pande RU, Amodeo JL, Karamanoukian RL, D’Ancona G, Karamanoukian HL (2003) Are you ready to become a robo-surgeon? Am Surg 69(7):599–603
Shaligram A, Meyer A, Simorov A, Pallati P, Oleynikov D (2013) Survey of minimally invasive general surgery fellows training in robotic surgery. J Robot Surg 7(2):131–136. doi:10.1007/s11701-012-0355-2
Hung AJ, Patil MB, Zehnder P, Cai J, Ng CK, Aron M, Gill IS, Desai MM (2012) Concurrent and predictive validation of a novel robotic surgery simulator: a prospective, randomized study. J Urol 187(2):630–637. doi:10.1016/j.juro.2011.09.154
Finnegan KT, Meraney AM, Staff I, Shichman SJ (2012) da Vinci Skills Simulator construct validation study: correlation of prior robotic experience with overall score and time score simulator performance. Urology 80(2):330–335. doi:10.1016/j.urology.2012.02.059
Johnston MJ, Paige JT, Aggarwal R, Stefanidis D, Tsuda S, Khajuria A, Arora S (2016) An overview of research priorities in surgical simulation: what the literature shows has been achieved during the 21st century and what remains. Am J Surg 211(1):214–225. doi:10.1016/j.amjsurg.2015.06.014
Panait L, Rafiq A, Tomulescu V, Boanca C, Popescu I, Carbonell A, Merrell RC (2006) Telementoring versus on-site mentoring in virtual reality-based surgical training. Surg Endosc 20(1):113–118. doi:10.1007/s00464-005-0113-x
Alaker M, Wynn GR, Arulampalam T (2016) Virtual reality training in laparoscopic surgery: a systematic review & meta-analysis. Int J Surg 29:85–94. doi:10.1016/j.ijsu.2016.03.034
Ahlborg L, Weurlander M, Hedman L, Nisel H, Lindqvist PG, Fellander-Tsai L, Enochsson L (2015) Individualized feedback during simulated laparoscopic training:a mixed methods study. Int J Med Educ 6:93–100. doi:10.5116/ijme.55a2.218b
Paschold M, Huber T, Zeissig SR, Lang H, Kneist W (2014) Tailored instructor feedback leads to more effective virtual-reality laparoscopic training. Surg Endosc 28(3):967–973. doi:10.1007/s00464-013-3258-z
Acknowledgements
Dr. Gyusung Lee received the Association for Surgical Education Center for Excellence in Surgical Education, Research and Training (CESERT) Grant and Intuitive Surgical Clinical Robotic Research Grant as the Principle Investigator of this study. The authors acknowledge the generous support of Dr. Michael Marohn, the Director of MISTIC, and the thoughtful and careful assistance of Karyn Rhyder in editing this manuscript.
Funding
This project was supported by the Association for Surgical Education Center for Excellence in Surgical Education, Research and Training (CESERT) Grant and Intuitive Surgical Clinical Robotic Research Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Gyusung Lee received the Association for Surgical Education Center for Excellence in Surgical Education, Research and Training (CESERT) grant and Intuitive Surgical Clinical Robotic Research Grant for this study. Dr. Mija Lee was the co-investigator in this study and is Dr. Gyusung Lee’s spouse.
Rights and permissions
About this article
Cite this article
Lee, G.I., Lee, M.R. Can a virtual reality surgical simulation training provide a self-driven and mentor-free skills learning? Investigation of the practical influence of the performance metrics from the virtual reality robotic surgery simulator on the skill learning and associated cognitive workloads. Surg Endosc 32, 62–72 (2018). https://doi.org/10.1007/s00464-017-5634-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5634-6