Abstract
Objectives
There is growing evidence that the relationship between body mass index (BMI — defined as weight in kilograms divided by height in metres squared) and patient outcomes is age-dependent; specifically, a raised BMI may have a protective effect in older adults. This has been demonstrated clearly in the community setting; less clear is the effect of age on this relationship in the inpatient setting.
Design, setting, participants and measurements
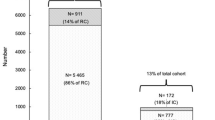
Retrospective analysis of 22,903 electronic records for patients discharged from two large public hospitals in South Australia between January 2015 and September 2018 inclusively. Records were retained if the patient’s height and weight had been recorded during the admission, BMI was between 10–99 kg/m2 and it was the patient’s first admission during that time. Patients were grouped by BMI (<18.5 kg/m2 (“underweight”), 18.5–24.9 kg/m2 (“normal weight”), 25–29.9 kg/m2 (“overweight”), >30 kg/m2 (“obese”)) and age (18–59 years, 60–79 years, > 80 years); for each group we measured the relative stay index (RSI) (actual length of stay divided by predicted length of stay), death in hospital and composite adverse outcome after discharge (unplanned readmission within 30 days and/or death within 30 days).
Results
Underweight patients across all age groups generally experienced significantly poorer outcomes compared to those not underweight. In those aged 18–59 years there were no significant differences in outcomes between the normal weight, overweight and obese groups. In those aged 60–79 years overweight patients had a significantly reduced risk of RSI > 2 compared to those of normal weight (p=0.014), and both overweight and obese patients had a significantly reduced risk of adverse outcome after discharge when compared to those of normal weight (p=0.028 & p=0.009 respectively). In those aged 80 years or older, both overweight and obese patients had a significantly reduced risk of adverse outcome after discharge when compared to those of normal weight (p=0.028 & p=0.013 respectively), and obese patients had a significantly reduced risk of inpatient mortality and RSI >2 when compared to those of normal weight (p=0.027 & p=0.037 respectively).
Conclusion
A BMI > 25 kg/m2 in older patients is associated with reduced risk of prolonged admission, inpatient mortality and adverse outcomes following discharge. This adds to growing evidence that age-specific BMI guidelines are required for adults because the healthiest BMI in the older hospital patient is seemingly not in the range 18.5–24.9 kg/m2.
Similar content being viewed by others
References
World Health Organisation, 2000. Obesity: preventing and managing the global epidemic: report of a WHO consultation. In: WHO technical report series 894. Geneva, Switzerland.
Johnson F, Cooke L, Croker H, Wardle J. Changing perceptions of weight in great britain: comparison of two population surveys. BMJ-Brit Med J 2008;337(7664):270–272. doi:https://doi.org/10.1136/bmj.a494.
Markoff B, Amsterdam A. Impact of Obesity on Hospitalized Patients. Mt Sinai J Med 2008;75(5):454–459. doi:https://doi.org/10.1002/msj.20072.
Westerly BD, Dabbagh O. Morbidity and mortality characteristics of morbidly obese patients admitted to hospital and intensive care units. J Crit Care 2011;26(2):180–185. doi:https://doi.org/10.1016/j/jcrc.2010.09.005.
Oreopoulos A, Kalantar-Zadeh K, Sharma AM, Fonarow GC. The obesity paradox in the elderly: potential mechanisms and clinical implications. Clin Geriatr Med 2009;25(4):643–659. doi:https://doi.org/10.1016/j.cger.2009.07.005.
Das SR, Alexander KP, Chen AY, Powell-Wiley TM, Diercks DB, Peterson ED, Roe MT, de Lemos JA. Impact of body weight and extreme obesity on the presentation, treatment, and in-hospital outcomes of 50,149 patients with st-segment elevation myocardial infarction. J Am Coll Cardiol 2011;58(25):2642–2650. doi:https://doi.org/10.1016/j.jacc.2011.09.030.
Hogue CW, Stearns JD, Colantuoni E, Robinson KA, Stierer T, Mitter N, Pronovost PJ, Needham DM. The impact of obesity on outcomes after critical illness: a meta-analysis. J Crit Care 2009;26(2):180–185. doi:https://doi.org/10.1016/j.jcrc.2010.09.005.
Schulman A, Abougergi MS, Thompson CC. The impact of obesity on the hospitalized patient: a nationwide analysis. Gastroenterology 2017;152(5):832.
Akinyemiju T, Meng Q, Vin-Raviv N. Association between body mass index and in-hospital outcomes: analysis of the nationwide inpatient database. Medicine 2016;95(28):4189. doi:https://doi.org/10.1097/MD.0000000000004189.
Cereda E, Klersy C, Hiesmayr M, Schindler K, Singer P, Laviano A, Caccialanza R, NutritionDay Survey Collaborators. Body mass index, age and in-hospital mortality: the NutritionDay multinational survey. Clin Nutr 2017;36(3):839–847. doi:https://doi.org/10.1016/j.clnu.2016.05.001.
Viana M, Moraes R, Fabbrin A, Santos M, Torman VB, Vieira S, Gross J, Canani L, Gerchman F, 2014. Contrasting effects of pre-existing hyperglycemia and higher body size on hospital mortality in critically ill patients: a prospective cohort study. Biomed central ltd. http://www.biomedcentral.com/1472-6823/14/50. Accessed 17 September 2018
Fusco KL, Robertson HC, Galindo H, PH Hakendorf, Thompson CH. Clinical outcomes for the obese hospital inpatient: an observational study. SAGE Open Med 2017;5:1–6. doi:https://doi.org/10.1177/2050312117700065.
Pickkers P, de Keizer N, Dusseljee J, Weerheijm D, van der Hoeven JG, Peek N. Body mass index is associated with hospital mortality in critically ill patients: an observational cohort study. Crit Care Med 2013;41(8):1878–1883. doi:https://doi.org/10.1097/CCM.0b013e31828a2aa1.
Chan T-C, Luk JKH, Chu L-W, Chan FHW. Association between body mass index and cause-specific mortality as well as hospitalization in frail chinese older adults. Geriatr Gerontol Int 2015;15(1):72–79. doi:https://doi.org/10.1111/ggi.12230.
Perotto M, Panero f, Gruden G, Fornengo P, Lorenzati B, Barutta F, Ghezzo G, Amione C, Cavallo-perin P, Bruno G. Obesity is associated with lower mortality risk in elderly diabetic subjects: the Casale Monferrato study. Acta diabetol 2013;50(4):563–568. doihttps://doi.org/10.1007/s00592-011-0338-1.
Stevens J, Cai J, Pamuk ER, Williamson DF, Thun MJ, Wood JL. The effect of age on the association between body-mass index and mortality. New Engl J Med 1998;338(1):1–7.
Jee SH, Sull JW, Park J, Lee S-Y, Ohrr H, Guallar E, Samet JM. Body-mass index and mortality in Korean men and women. New Engl J Med 2006;355(8):779–787.
Janssen I, Mark AE. Elevated body mass index and mortality risk in the elderly. Obes Rev 2007;8(1):41–59. doi:https://doi.org/10.1111/j.1467-789X.2006.00248.x
David CN, de Mello RB, Bruscato NM, Moriguchi EH. Overweight and abdominal obesity association with all-cause and cardiovascular mortality in the elderly aged 80 and over: a cohort study. J Nutr Health Aging 2017;21(5):597–603. doi:https://doi.org/10.1007/s12603-016-0812-0.
World Health Organisation, 2016. International statistical classification of diseases and related health problems 10th revision. https://icd.who.int/browse10/2016/en. Accessed 17 January 2019.
Hsieh C-H, Lai W-H, Wu S-C, Chen Y-C, Kuo P-J, Hsu S-Y, Hsieh H-Y. Trauma injury in adult underweight patients: a cross-sectional study based on the trauma registry system of a level I trauma center. Medicine 2017;96(10):e6272. doi:https://doi.org/10.1097/MD.0000000000006272.
Potter JF, Schafer DF, Bohi RL. In-hospital mortality as a function of body mass index: an age-dependent variable. J Gerontology 1988;43(3):59–63.
Finkielman JD, Gajic O, Afessa B. Underweight is independently associated with mortality in post-operative and non-operative patients admitted to the intensive care unit: a retrospective study. BMC Emerg Med 2004;4(1):1–7. doi:https://doi.org/10.1186/1471-227X-4-3.
Holme I, Tonstad S. Survival in elderly men in relation to midlife and current bmi. Age Ageing 2015;44(3):434–439. doi:https://doi.org/10.1093/ageing/afu202.
Hu H, Wang J, Han X, Li Y, Wang F, Yuan J, Miao X, Yang H, He M. Bmi, waist circumference and all-cause mortality in a middle-aged and elderly chinese population. J Nutr Health Aging 2018;22(8):975–981. doi:/https://doi.org/10.1007/s12603-018-1047-z.
Zamboni M, Mazzali G, Fantin F, Rossi A, Di Francesco V. Sarcopenic obesity: a new category of obesity in the elderly. Nutr Metab Cardiovas 2007;18(5):388–395. doi:https://doi.org/10.1016/j.numecd.2007.10.002.
Charlton K, Batterham M, Langfod K, Lateo J, Brock E, Walton K, Lyons-Wall P, Eisenhauer K, Green N, McLean C. Lean body mass associated with upper body strength in healthy older adults while higher body fat limits lower extremity performance and endurance. Nutrients 2015;7(9):7126–7142. doi:https://doi.org/10.3390/nu7095327.
Cerri AP, Bellellli G, Mazzone A, Pittella F, Landi F, Zambon A, Annoni G. Sarcopenia and malnutrition in acutely ill hospitalized elderly: prevalence and outcomes. Clin Nutr 2015;34(4):745–751. doi:https://doi.org/10.1016/j.clnu.2014.08.015.
Han P, Zhao J, Guo Q, Wang J, Zhang W, Shen S, Wang X, Dong R, Ma Y, Kang L, Fu L, Jia L, Han X, He Z, Bao Y, Wang L, Niu K. Incidence, risk factors, and the protective effect of high body mass index against sarcopenia in suburb-dwelling elderly chinese populations. J Nutr Health Aging 2016;20(10):1056–1060. doi:https://doi.org/10.1007/s12603-016-0704-3.
Sanada K, Chen R, Willcox B, Ohara T, Wen A, Takenaka C, Kamal M. Association of sarcopenic obesity predicted by anthropometric measurements and 24-y all-cause mortality in elderly men: the kuakini Honolulu heart program. Nutrition 2018;46:97–102. doi:https://doi.org/10.1016/j.nut.2017.09.003.
Deren ME, Babu J, Cohen EM, Machan J, Born CT. Increased mortality in elderly patients with sarcopenia and acetabular fractures. J Bone Joint Surg 2017;99(3):200–206. doi:https://doi.org/10.2106/JBJS.16.00734.
Woo J. Sarcopenia. Clin Geriatr Med 2017;33(3):305–314. doi:https://doi.org/10.1016/j.cger.2017.02.003.
Matsubara Y, Matsumoto T, Inoue K, Matsuda D, Yoshiga R, Yoshiya K, Furuyama T, Maehara Y. Sarcopenia is a risk factor for cardiovascular events experienced by patients with critical limb ischemia. J Vasc Surg 2015;65(5):1390–1397. doi:https://doi.org/10.1016/j.jvs.2016.09.030.
Senior HE, Henwood TR, Beller EM, Mitchell GK, Keogh JW. Prevalence and risk factors of sarcopenia among adults living in nursing homes. Maturitas 2015;82(4):418–423. doi:https://doi.org/10.1016/j.maturitas.2015.08.006.
DeAndrade J, Pedersen M, Garcia L, Nau P. Sarcopenia is a risk factor for complications and an independent predictor of hospital length of stay in trauma patients. J Surg Res 2018;221:161–166. doi:https://doi.org/10.1016/j.jss.2017.08.018.
Backx EMP, Tieland M, Borgonjen-van den Berg KJ, Claessen PR, van Loon LJC, de Groot LCPGM. Protein intake and lean body mass preservation during energy intake restriction in overweight older adults. Int J Obesity 2016;40:299–304. doi:https://doi.org/10.1038/ijo.2015.182.
Mettler S, Mitchell N, Tipton KD. Increased protein intake reduces lean body mass during weight loss in athletes. Med Sci Sport Exer 2010;42(2):326–337. doi:https://doi.org/10.1249/MSS.0b013e3181b2ef8e.
Muller MJ, Geisler C, Pourhassan M, Gluer C-C, Bosy-Westphal A. Assessment and definition of lean body mass deficiency in the elderly. Eur J Clin Nutr 2014;68(11):1220–1227. doi:https://doi.org/10.1038/ejcn.2014.169.
Fuggle N, Shaw S, Dennison E, Cooper C. Sarcopenia. Best Pract Res Cl Rh 2017;31(2):218–242. doi:https://doi.org/10.1016/j.berh.2017.11.007.
Androga L, Sharma D, Amodu A, Abramowtiz MK. Sarcopenia, obesity, and mortality in US adults with and without chronic kidney disease. Kidney Int 2017;2(2):201–211. doi:https://doi.org/10.1016/j.ekir.2016.10.008.
Kim H, Suzuki T, Kim M, Jokima N, Yoshida Y, Hirano H, Saito K, Iwasa H, Shimada H, Hosoi E, Yoshida H. Incidence and predictors of sarcopenia onset in community-dwelling elderly Japanese women: 4-year follow-up study. J Am Med Dir Assoc 2015;16(1):1–8. doi:https://doi.org/10.1016/j.jamda.2014.10.006.
Coupaye M, Bouillot J-L, Poitou C, Schutz Y, Basdevant A, Oppert J-M. Is lean body mass decreased after obesity treatment by adjustable gastric banding? Obes Surg 2007;17(4):427–433. doi:https://doi.org/10.1007/s11695-007-9072-8.
Ballor DL, Katch VL, Moorehead CP, Becque MD, Marks CR. Dietary induced weight loss results in slight leaen body mass loss even with heavy weight training. Med Sci Sport Exer 1985;17(2):243.
DeLany JP, Kelley DE, Hames KC, Jakicic JM, Goodpaster BH. Effect of physical activity on weight loss, energy expenditure, and energy intake during diet induced weight loss. Obesity 2014;22(2):363–370. doi:https://doi.org/0001981086; https://doi.org/10.1002/obt.20525.
Dudgeon WD, Kelley EP, Scheett TP. In a single-blind, matched group design: branched-chain amino acid supplementation and resistance training maintains lean body mass during a caloric restricted diet. J Int Soc Sport Nutr 2016;13(1). doi:https://doi.org/10.1186/s12970-015-0112-9.
Kulovitz MG, Kolkmeyer D, Conn CA, Cohen DA, Ferraro RT. Medical weight loss versus bariatric surgery: does method affect body composition and weight maintenance after 15% reduction in body weight? Nutrition 2014;30(1):49–54. doi:https://doi.org/10.1016/j.nut.2013.06.008.
Cava E, Yeat NC, Mittendorfer B. Preserving healthy muscle during weight loss. Adv Nutr 2017;8(3):511–519. doi:https://doi.org/10.3945/an.116.014506.
Mingrone G, Marino S, DeGaetano A, Capristo E, Heymsfield SB, Gasbarrini G, Greco AV. Different limit to the body’s ability of increasing fat-free mass. Metabolism 2001;50:1004–1007.
Lafortuna CL, Tresoldi D, Rizzo G. Influence of body adiposity on structural characteristics of skeletal muscle in men and women. Clin Phys Funct I 2014;34(1):47–55. doi:https://doi.org/10.1111/cpf.12062.
Choi SJ, Files DC, Zhang T, Wang ZM, Messi ML, Gregory H, Stone J, Lyles MF, Dhar S, Marsh AP, Nicklas BJ, Delbono O. Intramyocellular lipid and impaired myofiber contraction in normal weight and obese older adults. J Gerontol A Biol Sci Med Sci 2016;71:557–564. doihttps://doi.org/10.1111/cpf.12062.
Toft-Petersen AP, Wulff J, Harrison DA, Ostermann M, Margarson M, Rowan KM, Dawson D. Exploring the impact of using measured or estimated values for height and weight on the relationship between BMI and acute hospital mortality. J Crit Care 2018;44:196–202. doi:https://doi.org/10.1016/j.jcrc.2017.11.021.
Borg S, Persson U, Odegaard K, Berglund G, Nilsson J-A, Nilsson PM. Obesity, survival, and hospital costs — findings from a screening project in Sweden. Value Health 2005;8(5)562–571. doihttps://doi.org/10.1111/j.1524-4733.2005.00048.x.
Bo M, Massaia M, Raspo S, Bosco F.) Predictive factors of in-hospital mortality in older patients admitted to a medical intensive care unit. J Am Geriatr Soc 2003;51(4):529–533. doi:https://doi.org/10.1046/j.1532-5415.2003.51163.x.
Filardo G, Hamilton C, Hamman B, Ng HKT, Grayburn P. Categorizing bmi may lead to biased results in studies investigating in-hospital mortality after isolated cabg. J Clin Epidemiol 2007;60(11):1132–1139. doi:https://doi.org/10.1016/j.jclinepi.2007.01.008.
Hussain HG, Khan SZ, Khan MA, Graham AR, McKinsey JF. Prevalence and effects of bmi on hospital course, 30-day mortality, and morbidity in patients undergoing endovascular procedures. J Vasc Surg 2010;52(3):811–812. doi:https://doi.org/10.1016/j.jvs.2010.06.052.
Childs BR, Nahm NJ, Dolenc AJ, Vallier HA. Obesity is associated with more complications and longer hospital stays after orthopaedic trauma. J Orthop Trauma 2015;29(11):504–509. doi:https://doi.org/10.1097/BOT.0000000000000324.
Amri R, Bordeianou LG, Sylla P, Berger DL. Obesity, outcomes and quality of care: body mass index increases the risk of wound-related complications in colon cancer surgery. Am J Surg 2014;207(1). doi:https://doi.org/10.1016/j.amjsurg.2013.05.016.
Liu T, Chen JJ, Bai XJ, Zheng GS, Gao W. The effect of obesity on outcomes in trauma patients: a meta-analysis. Injury 2013;44(9):1145–1152. doi:https://doi.org/10.1016/j.injury.2012.10.038.
Lozano LM, Tio M, Rios J, Sanchez-Etayo G, Popescu D, sastre S, Basora M. Severe and morbid obesity (bmi > 35 kg/m(2)) does not increase surgical time and length of hospital stay in total knee arthroplasty surgery. Knee Surg Sport Tr A 2015;23(6):1713–1719. doi:https://doi.org/10.1007/s00167-014-3002-9.
Heneghan HM, Annaberdyev S, Attaluri V, Pitt T, Kroh M, Chalikonda S, Brethauer SA, Rosenblatt S. Obesity does not adversely affect outcomes after laparoscopic splenectomy. Am J Surg 2013;206(1):52. doi:https://doi.org/10.1016/j.amjsurg.2012.07.041.
Sing DC, Luan TF, Feeley BT, Zhang AL. Is obesity a risk factor for adverse events after knee arthroscopy? Arthroscopy 2016;32(7):1346–1353. doi:https://doi.org/10.1016/j.arthro.2016.01.017.
Husted H, Gromov K, Jorgensen CC, Kehlet H, Lundbeck Foundation Center for Fast-track Hip and Knee Replacement Collaborative Group. Does bmi influence hospital stay and morbidity after fast-track hip and knee arthroplasty? Acta Orthop 2016;87(5):466–472. doi:https://doi.org/10.1080/17453674.2016.120477.
Adogwa O, Elsasmadicy AA, Vuong VD, Mehta A, Vasquez-Castellanos RA, Cheng JS, Karikari IO, Bagley CA. Patient bmi is an independent predictor of 30-Day hospital readmission after elective spine surgery. Spine J 2016;16(10):193. doi:https://doi.org/10.1016/j.spinee.2016.07.100.
Mathus-Vliegen EM. Obesity and the elderly. J Clin Gastroenterol 2012;46(7):533–544. doi:https://doi.org/10.1097/MCG.0b013e31825692ce.
Dewan S, Wilding JPH. Obesity and type-2 diabetes in the elderly. Gerontology 2003;49(3):137–145. doi:https://doi.org/10.1159/000069176.
Lechleitner M. Obesity and the metabolic syndrome in the elderly — a mini-review. Gerontology 2008;54(5):253–259. doi:https://doi.org/10.1159/000161734.
Lechleitner M. The elderly as a target for obesity treatment. Expert Rev Endocrinol Metab 2015;10(4):375–380. doi:https://doi.org/10.1586/17446651.2015.1028530.
Porter-Starr KN, McDonald SR, Bales CW. Obesity and physical frailty in older adults: a scoping review of lifestyle intervention trials. J Am Med Dir Assoc 2014;15(4):240–250. doi:https://doi.org/10.1016/j.jamda.2013.11.008.
Rossner S. Obesity in the elderly — a future matter of concern? Obes Rev 2001;2(3):183–188. doi:https://doi.org/10.1046/j.1467-789x.2001.00034.x.
McKee A, Morley JE. Obesity in the elderly. Endotext. https://www.ncbi.nlm.nih.gov/books/NBK532533. Accessed 2 January 2019.
McGlone ER, Bond A, Reddy M, Khan OA, Wan AC. Super-obesity in the elderly: is bariatric surgery justified? Obes Surg 2015;25(9):1750–1755. doi:https://doi.org/10.1007/s11695-015-1776-6.
Qin C, Luo B, Aggarwal A, De Oliveira G, Kim JY. Advanced age as an independent predictor of perioperative risk after laparoscopic sleeve gastrectomy (lsg). Obes Surg 2015;25(3):406–412. doi:https://doi.org/10.1007/s11695-014-1462-0.
Wilson SE, Nguyen NT. Outcomes of bariatric surgery in the elderly. Am Surgeon 2006;72(10):865–869.
Gonzalez MC, Correia MITD, Heymsfield SB. A requiem for bmi in the clinical setting. Curr Opin Clin Nutr 2017;20(5):314–321. doi:https://doi.org/10.1097/MCO.0000000000000395.
Kalinkovich A, Livshits G. Sarcopenic obesity or obese sarcopenia: a cross talk between age-associated adipose tissue and skeletal muscle inflammation as a main mechanism of the pathogenesis. Ageing Res Rev 2017;35:200–221. doi:https://doi.org/10.1016/j.arr.2016.09.008.
Richman EL, Stampfer MJ. Weight loss and mortality in the elderly separating cause and effect. J Intern Med 2010;268(2):103–105. doi:https://doi.org/10.1111/j.1365-2796.2010.02227.x.
Dennis DM, Carter V, Trevenen M, Tyler J, Perrella L, Lori E, Cooper I. Do acute hospitalised patients in Australia have a different body mass index to the general Australian population a point prevalence study? Aust Health Rev 2018;42(2):121–129. doi:https://doi.org/10.1071/AH16171.
Bahat G, Tufan F, Saka B, Akin S, Ozkaya H, Yucel N, Erten N, Karan MA. Which body mass index (bmi) is better in the elderly for functional status? Arch Gerontol Geriat 2012;54(1):78–81. doi:https://doi.org/10.1016/j.archger.2011.04.019.
Kimyagarov S, Klid R, Levenkrohn S, Fleissig Y, Kopel B, Arad M, Adunsky A. Body mass index (bmi), body composition and mortality of nursing home elderly residents. Arch Gerontol Geriat 2010;51(2):227–230. doi:https://doi.org/10.1016/j.archger.2009.10.013.
Donini LM, Savina C, Gennaro E, De Felice MR, Rosano A, Pandolfo MM, Del Balzo V, Cannella C, Ritz P, Chumlea WMC. A systematic review of the literature concerning the relationship between obesity and mortality in the elderly. J Nutr Health Aging 2012;16(1):89–98. doi:https://doi.org/10.1007/s12603-011-0073-x.
Dahl AK, Fauth EB, Ernsth-Bravell M, Hassing LB, Ram N, Gerstof D. Body mass index, change in body mass index, and survival in old and very old persons. J Am Geriatr Soc 2013;61(4):512–518. doi: https://doi.org/10.1111/jgs.12158.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Woolley, C., Thompson, C., Hakendorf, P. et al. The Effect of Age upon the Interrelationship of BMI and Inpatient Health Outcomes. J Nutr Health Aging 23, 558–563 (2019). https://doi.org/10.1007/s12603-019-1206-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-019-1206-x