Abstract
Background
Optimal obesity therapy is a matter of debate. Besides weight reduction, other criteria such as safety and nutritional status are of relevance. Therefore, we compared a favored surgical intervention with the most effective conservative treatment regarding anthropometry and nutritional status.
Methods
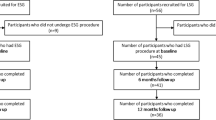
Fifty-four obese patients were included who underwent laparoscopic sleeve gastrectomy (LSG, n = 27) or a 52-week multidisciplinary intervention program (MIP, n = 27) for weight loss. Body weight, body composition assessed by bioelectrical impedance analysis, and serum protein levels were measured before and within 12 months after intervention.
Results
After 1 year of observation, excess weight loss was more pronounced following LSG (65 %) compared to MIP (38 %, p < 0.001). In both groups, body fat was clearly reduced, but a higher reduction occurred in the LSG group. However, protein status deteriorated particularly in the LSG group. Within 1 year, body cell mass declined from 37.1 to 26.9 kg in the LSG group, but only from 35.7 to 32.2 kg in the MIP group. This resulted in an increased mean extracellular mass/body cell mass ratio (1.42 versus 1.00, p < 0.001), in a decreased mean phase angle (4.4° versus 6.6°, p < 0.001), and in a lower prealbumin level in serum (p < 0.02) in the LSG group compared to the MIP group.
Conclusions
LSG, compared to MIP, was more effective regarding excess weight loss and body fat loss within 1 year, however, induced more pronounced muscle mass and protein loss, possibly requiring particular interventions such as exercise or protein supplements.


Similar content being viewed by others
References
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg. 2009;19:1605–11. PMID: 19885707.
Maggard MA, Shugarman LR, Suttorp M, et al. Meta-analysis: surgical treatment of obesity. Ann Intern Med. 2005;142:547–59.
Sjöström L, Lindroos A, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93.
Strain GW, Gagner M, Pomp A, et al. Comparison of weight loss and body composition changes with four surgical procedures. Surg Obes Relat Dis. 2009;5:582–7. PMID: 19560983.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37. PMID: 15479938.
Appel LJ, Clark JM, Yeh H, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;365:1959–68.
Ryan DH, Johnson WD, Myers VH, et al. Nonsurgical weight loss for extreme obesity in primary care settings: results of the Louisiana Obese Subjects Study. Arch Intern Med. 2010;170:146–54.
Bischoff SC, Damms-Machado A, Betz C, et al. Multicenter evaluation of an interdisciplinary 52-week weight loss program for obesity with regard to body weight, comorbidities and quality of life—a prospective study. Int J Obes (Lond). 2012;36:614–24. PMID: 21673653.
Leonetti F, Capoccia D, Coccia F, et al. Obesity, type 2 diabetes mellitus, and other comorbidities: a prospective cohort study of laparoscopic sleeve gastrectomy vs medical treatment. Arch Surg. 2012;147:694–700. PMID: 22508671.
Mingrone G, Panunzi S, de Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366:1577–85.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567–76. PMID: 22449319.
Dixon JB, O'Brien PE, Playfair J, et al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA. 2008;299:316–23. PMID: 18212316.
Batsis JA, Romero-Corral A, Collazo-Clavell ML, et al. Effect of bariatric surgery on the metabolic syndrome: a population-based, long-term controlled study. Mayo Clin Proc. 2008;83:897–907. PMID: 18674474.
Faria SL, Faria OP, Buffington C, et al. Dietary protein intake and bariatric surgery patients: a review. Obes Surg. 2011;21:1798–805. PMID: 21590346.
Damms-Machado A, Friedrich A, Kramer KM, et al. Pre- and postoperative nutritional deficiencies in obese patients undergoing laparoscopic sleeve gastrectomy. Obes Surg. 2012;22:881–9. PMID: 22403000.
Faintuch J, Matsuda M, Cruz MELF, et al. Severe protein–calorie malnutrition after bariatric procedures. Obes Surg. 2004;14:175–81. PMID: 15018745.
Bloomberg RD, Fleishman A, Nalle JE, et al. Nutritional deficiencies following bariatric surgery: what have we learned? Obes Surg. 2005;15:145–54. PMID: 15802055.
Malinowski SS. Nutritional and metabolic complications of bariatric surgery. Am J Med Sci. 2006;331:219–25. PMID: 16617238.
Bal BS, Finelli FC, Shope TR, et al. Nutritional deficiencies after bariatric surgery. Nat Rev Endocrinol. 2012;8:544–56. PMID: 22525731.
Kellum JM, Chikunguwo SM, Maher JW, et al. Long-term results of malabsorptive distal Roux-en-Y gastric bypass in superobese patients. Surg Obes Relat Dis. 2011;7:189–93. PMID: 21145293.
Kueper MA, Kramer KM, Kirschniak A, et al. Laparoscopic sleeve gastrectomy: standardized technique of a potential stand-alone bariatric procedure in morbidly obese patients. World J Surg. 2008;32:1462–5. PMID: 18368447.
Runkel N, Colombo-Benkmann M, Hüttl TP, et al. Bariatric surgery. Dtsch Arztebl Int. 2011;108:341–6. PMID: 21655459.
Dörhöfer R, Pirlich M. Das BIA Kompendium. Data Input GmbH, Germany. 2007. Available from: http://www.data-input.de/_site/_data/pdf/komp_d_all.pdf. Accessed 15 Jan 2013
Wang J, Zhang Y, Chen H, et al. Comparison of two bioelectrical impedance analysis devices with dual energy X-ray absorptiometry and magnetic resonance imaging in the estimation of body composition. J Strength Cond Res. 2013;27:236–43. PMID: 22344056.
Jiménez A, Omaña W, Flores L, et al. Prediction of whole-body and segmental body composition by bioelectrical impedance in morbidly obese subjects. Obes Surg. 2012;22:587–93. PMID: 22506280.
Thibault R, Pichard C. The evaluation of body composition: a useful tool for clinical practice. Ann Nutr Metab. 2012;60:6–16. PMID: 22179189.
Kyle UG, Genton L, Pichard C. Low phase angle determined by bioelectrical impedance analysis is associated with malnutrition and nutritional risk at hospital admission. Clin Nutr. 2012;32:294–9. PMID: 22921419.
Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129–39.
Bray GA, Smith SR, Banerji MA, Tripathy D, Clement SC, Buchanan TA, Henry RR, Kitabchi AE, Mudaliar S, Musi N, Ratner RE, Schwenke DC, Stentz FB, Reaven PD, DeFronzo RA. Effect of pioglitazone on body composition and bone density in subjects with prediabetes in the ACT NOW trial. Diabetes Obes Metab. 2013. doi:10.1111/dom.12099
Boza C, Salinas J, Salgado N, et al. Laparoscopic sleeve gastrectomy as a stand-alone procedure for morbid obesity: report of 1,000 cases and 3-year follow-up. Obes Surg. 2012;22:866–71. PMID: 22438219.
Shi X, Karmali S, Sharma AM, et al. A review of laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg. 2010;20:1171–7. PMID: 20379795.
Aggarwal S, Kini SU, Herron DM. Laparoscopic sleeve gastrectomy for morbid obesity: a review. Surg Obes Relat Dis. 2007;3:189–94. PMID: 17386400.
Nocca D, Krawczykowsky D, Bomans B, et al. A prospective multicenter study of 163 sleeve gastrectomies: results at 1 and 2 years. Obes Surg. 2008;18:560–5.
Tucker ON, Szomstein S, Rosenthal RJ. Indications for sleeve gastrectomy as a primary procedure for weight loss in the morbidly obese. J Gastrointest Surg. 2008;12:662–7. PMID: 18264685.
Du H, Feskens E. Dietary determinants of obesity. Acta Cardiol. 2010;65:377–86. PMID: 20821929.
Gardner CD, Kiazand A, Alhassan S, et al. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: the A TO Z Weight Loss Study: a randomized trial. JAMA. 2007;297:969–77. PMID: 17341711.
Vatier C, Henegar C, Ciangura C, et al. Dynamic relations between sedentary behavior, physical activity, and body composition after bariatric surgery. Obes Surg. 2012;22:1251–6. PMID: 22351039.
Andreu A, Moizé V, Rodríguez L, et al. Protein intake, body composition, and protein status following bariatric surgery. Obes Surg. 2010;20:1509–15. PMID: 20820937.
de Aquino LA, Pereira SE, de Souza Silva J, et al. Bariatric surgery: impact on body composition after Roux-en-Y gastric bypass. Obes Surg. 2012;22:195–200. PMID: 21881836.
Di Renzo L, Carbonelli MG, Bianchi A, et al. Body composition changes after laparoscopic adjustable gastric banding: what is the role of -174GC interleukin-6 promoter gene polymorphism in the therapeutic strategy? Int J Obes (Lond). 2012;36:369–78. PMID: 21730965.
Madan AK, Kuykendall S, Orth WS, et al. Does laparoscopic gastric bypass result in a healthier body composition? An affirmative answer. Obes Surg. 2006;16:465–8. PMID: 16608612.
Dixon JB, Strauss BJG, Laurie C, et al. Changes in body composition with weight loss: obese subjects randomized to surgical and medical programs. Obesity (Silver Spring). 2007;15:1187–98. PMID: 17495195.
Aarts EO, Janssen IMC, Berends FJ. The gastric sleeve: losing weight as fast as micronutrients? Obes Surg. 2011;21:207–11. PMID: 21088925.
Leivonen MK, Juuti A, Jaser N, et al. Laparoscopic sleeve gastrectomy in patients over 59 years: early recovery and 12-month follow-up. Obes Surg. 2011;21:1180–7. PMID: 21625908.
Snyder-Marlow G, Taylor D, Lenhard MJ. Nutrition care for patients undergoing laparoscopic sleeve gastrectomy for weight loss. J Am Diet Assoc. 2010;110:600–7. PMID: 20338286.
DeLegge MH, Drake LM. Nutritional assessment. Gastroenterol Clin North Am. 2007;36:1–22. PMID: 17472872.
Melissas J, Daskalakis M, Koukouraki S, et al. Sleeve gastrectomy—a “food limiting” operation. Obes Surg. 2008;18:1251–6. PMID: 18663545.
Braghetto I, Davanzo C, Korn O, et al. Scintigraphic evaluation of gastric emptying in obese patients submitted to sleeve gastrectomy compared to normal subjects. Obes Surg. 2009;19:1515–21. PMID: 19714384.
Keller U. Dietary proteins in obesity and in diabetes. Int J Vitam Nutr Res. 2011;81:125–33. PMID: 22139563.
Josse AR, Atkinson SA, Tarnopolsky MA, et al. Increased consumption of dairy foods and protein during diet- and exercise-induced weight loss promotes fat mass loss and lean mass gain in overweight and obese premenopausal women. J Nutr. 2011;141:1626–34. PMID: 21775530.
Frimel TN, Sinacore DR, Villareal DT. Exercise attenuates the weight-loss-induced reduction in muscle mass in frail obese older adults. Med Sci Sports Exerc. 2008;40:1213–9. PMID: 18580399.
Heber D, Greenway FL, Kaplan LM, et al. Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2010;95:4823–43. PMID: 21051578.
Rinaldi Schinkel E, Pettine SM, Adams E, et al. Impact of varying levels of protein intake on protein status indicators after gastric bypass in patients with multiple complications requiring nutritional support. Obes Surg. 2006;16:24–30. PMID: 16417753.
Moize V, Geliebter A, Gluck ME, et al. Obese patients have inadequate protein intake related to protein intolerance up to 1 year following Roux-en-Y gastric bypass. Obes Surg. 2003;13:23–8. PMID: 12630609.
Bavaresco M, Paganini S, Lima TP, et al. Nutritional course of patients submitted to bariatric surgery. Obes Surg. 2010;20:716–21. PMID: 18931884.
Acknowledgments
This work was supported by the “Competence Network of Obesity,” research group “Obesity and the gastrointestinal tract,” coordinated by SCB and funded by the Federal Ministry of Education and Research, Germany (No. FKZ 01GI0843).
Conflict of interest
All authors declare no conflict of interest; they are all independent from the funding institutions. The authors are part of the Competence network of obesity, which is primarily funded by a research grant of the Federal Ministry of Education and Research, Germany. Within this network, the authors are funded in part by Covidien Germany GmbH, by Johnson & Johnson, Ethicon Endo-Surgery GmbH, Germany, and by Nestlé Inc., Germany. The sponsors had no influence in study design, analysis, and interpretation of data, as well as in the writing of the manuscript. No other relationships or activities exist that could appear to have influenced the submitted work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Friedrich, A.E., Damms-Machado, A., Meile, T. et al. Laparoscopic Sleeve Gastrectomy Compared to a Multidisciplinary Weight Loss Program for Obesity—Effects on Body Composition and Protein Status. OBES SURG 23, 1957–1965 (2013). https://doi.org/10.1007/s11695-013-1036-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-013-1036-6