Abstract
Background
The aim of this study was to analyze the impact of bariatric surgery on the body composition of patients suffering from class III obesity at different postoperative time intervals.
Methods
The body composition of 114 patients undergoing Roux-en-Y gastric bypass surgery was measured prior to surgery (T0) and then 30 (T30) and 180 (T180) days following surgery. Body composition was evaluated using the following parameters: total body mass, body mass index, excess weight, percentage of excess weight loss, relative body fat (%F), lean body mass (LBM), and fat tissue mass (FTM). To determine these variables, validated formulas and equations proper to obese men and women were employed.
Results
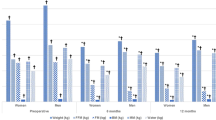
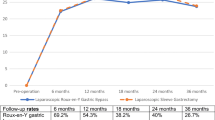
A significant reduction in %F (41.5%), LBM (20.3%), FTM (37.9%) was noted at each time interval (p ≤ 0.01).
Conclusions
Bariatric surgery proved to be effective in reducing total body mass and body fat at every time interval. However, dietary measures emphasizing adequate protein intake may be implemented in order to reduce loss of LBM and, coupled with frequent physical activity, may help curtail the impact the surgery has on morphological variables.
Similar content being viewed by others
References
Bender R, Zeeb H, et al. Causes of death in obesity: relevant increase in cardiovascular but not in all-cancer mortality. J Clin Epidemiol. 2006;59:1064–71.
Busseto L, Pisent C, Rinaldi, et al. Variation in lipid levels in morbidly obese patients operated with the Lap-Band® adjustable gastric banding system: effects of different levels of weight loss. Obes Surg. 2000;10:569–77.
Ciolac EG, Guimarães GV. Exercício físico e síndrome metabólica. Rev Bras Med Esporte. 2004;10(4):319–24.
Das SK. Body composition measurement in severe obesity. Curr Opin Clin Nutr Metab Care. 2005;8(6):602–6.
Deitel M. Overweight and obesity worldwide now estimated to involve 1.7 billion people. Obes Surg. 2003;13:329–30.
Faria OP, Pereira VA, Gangoni CMC, et al. Obesos mórbidos tratados com gastroplastia redutora com bypass gástrico em Y de Roux: análise de 160 pacientes. Brasília Méd. 2002;39(1/4):26–34.
Freedman DS, Khan LK, Serdula MK, et al. Trends and correlates of class 3 obesity in the United States from 1990 to 2000. JAMA. 2002;188:1758–61.
Halpen A. Fisiologia da Obesidade. In: Garrido Júnior AB, Ferraz EM, Barroso FL, et al., editors. Cirurgia da obesidade. São Paulo: Ed. Editora Atheneu; 2003. p. 9–12.
Hill JO, Sparling PB, Shields TW, et al. Effects of exercise and food restriction and body composition and metabolic rate in obese women. Am J Clin Nutr. 1987;46:622–30.
Instituto Brasileiro de Geografia e Estatística—IBGE. Pesquisa de Orçamentos Familiares 2008–2009: Antropometria e Estado Nutricional de Crianças, Adolescentes e Adultos no Brasil. Rio de Janeiro: Ministério do Planejamento, Orçamento e Gestão/IBGE; 2010.
Inge TH, Xanthakos SA, Zeller MH. Bariatric surgery for pediatric extreme obesity: now or later? Int J Obese (Lond). 2007;31:1–14.
Jackson AS, Stanforth PR, Gagnon J, et al. The effect of sex, age and race on estimating percentage body fat from body mass index: the heritage family study. Int J Obes. 2002;26:789–96.
Katzmarzyk PT, Mason C. Prevalence of class I, II and III obesity in Canada. CMAJ. 2006;174(2):156–7.
Karhunen L, Franssila-Kallunki A, Rissanen A, et al. Determinants of resting energy expenditure in obese non-diabetic Caucasian women. Int J Obes, London. 1997;21:197–202.
Kuhlmann HW, Falconi RA, Wolf AM. Cost-effective bariatric surgery in Germany today. Obes Surg. 2000;10:549–52.
Liou YM, Liou TH, Chang LC. Obesity among adolescents: sedentary leisure time and sleeping as determinants. Journal of Advanced Nursing. 2010;66(6):1246–56.
Loghman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Abridged edition, 1988;90
Maclean LD, Rhode BM, Shizgal HM. Gastroplasty for obesity. Surg Gynecol Obstet. 1981;153(2):200–8.
Metcalf B, Rabkin RA, Rabkin JM, et al. Weight loss composition: the effects of exercise following obesity surgery as measured by bioelectrical impedance analysis. Obes Surg. 2005;15:183–6
Mônaco DV, Merhi VAL, Aranha N, et al. Impacto da cirurgia bariátrica tipo capella modificado sobre a perda ponderal em pacientes com obesidade mórbida. Rev Ciênc Méd Campinas. 2006;15(4):289–98.
Muscelli E, Mingrone G, Camastra S, et al. Differential effect of weight loss on insulin resistance in surgically treated obese patients. Am J Med. 2005;118(1):51–7.
Nagaya T, Yoshida H, Takahashi H, et al. Body mass index (weight/height2) or percentage body fat by bioelectrical impedance analysis: which variable better reflects serum lipid profile? Int J Obes. 1999;23:771–4.
National Collaborating Centre for Primary Care. Obesity: the prevention, identification, assessment and management of overweight and obesity in adults and children. London: National Institute for Health and Clinical Excellence; 2006. p. 2590.
National Institute of Health Consensus Development Conference Statement. Gastrointestinal surgery for morbid obesity. Am J Clin Nutr. 1992;55(2):615s–9s.
Neves CE, Saboya C, Pereira SE, et al. Impact of bariatric surgery on morphological variables in the morbidly obese. FIEP Bulletin. 2007;77:692–4.
Norton K, Olds T. Antropometrica. Rosário: Biosystem Servicio Educativo; 2000.
Ogden J, Clementi C, Aylwin S, et al. Exploring the impact of obesity surgery on patients health status: a quantitative and qualitative study. Obes Surg. 2005;15(2):266–72.
Palombo JD, Maletskos CJ, Reinhold RV, et al. Composition of weight loss in morbidly obese patients after gastric bypass. J Surg Res. 1981;30(5):435–42.
Ramalle-Gómara E, Lozano DM, Hernando AB, et al. Validez de lãs medidas autodeclaradas de peso y talla en la estimación de la prevalencia de obesidad. Med Clin. 1997;716:108.
Ravussin E, Lillioja S, Knowler W, et al. Reduced rate of energy expenditure as a risk factor for body-weight gain. N Engl J Med. 1988;318:467–72.
Residori L, Garcia-Lorda P, Flancbaum L, et al. Prevalence of co-morbidities in obese patients before bariatric surgery: effect of race. Obes Surg. 2003;13:333–40.
Santos EMC, Burgos MPA, Silva SA. Perda ponderal após cirurgia bariátrica de Fobi-Capella: realidade de um hospital universitário do nordeste brasileiro. Rev Bras Nutr Clin. 2006;21(3):188–92.
Shah M, Simha V, Garg A. Review: long term impact of bariatric surgery on body weight, comorbidities, and nutritional status. J Clin Endocrinol Metabol. 2006;91(11):4223–31.
Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Skroubis G, Sakellaropoulos G, Pouggouras K, et al. Comparison of nutritional deficiencies after Roux-en-Y gastric bypass and after biliopancreatic diversion with Roux-en-y gastric bypass. Obes Surg. 2002;12:551–8.
Stiegler P, Cunliffe A. The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med. 2006;36(3):239–62.
Sugarman HJ. Bariatric surgery for severe obesity. J Assoc Acad Minor Phys. 2001;12(3):129–36.
Suter M, Giusti V. Surgical options of obesity treatment: results and complications. Rev Med Suisse. 2005;1(12):832–6.
Szego T, Mendes CJL, Bitran A. Derivaçao gastrojejunal por laparoscopia com e sem anel. In: Garrido Jr AB, editor. Cirurgia da obesidade. Sao Paulo: Atheneu; 2002. p. 189–96.
USDA (US Department of Agriculture). Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans. 2010
van Gemert WG, Westerterp KR, van Acker BA, et al. Energy, substrate and protein metabolism in morbid obesity before, during and after massive weight loss. Int J Obes Relat Metab Disord. 2000;24:711–8.
Velasco MN, Haberle TS. Tratamiento cuirúrgico de la obesidad mórbida. Rev Chil Cir. 2003;55(2):155–9.
Weltman A, Levine S, Seip R, et al. Accurate assessment of body composition in obese females. Am J Clin Nutr. 1988;48:1179–83.
Weltman A, Levine S, Seip R, et al. Practical assessment of body composition in adults males. Hum Biol. 1987;59(3):523–35.
WHO (World Health Organization). Obesity: preventing and managing the global epidemic. Report of WHO consultation on obesity. Geneva: World health organization; 1998.
Acknowledgments
We would like to thank Professor Maria das Graças Tavares do Carmo (INJC/UFRJ) for her cooperation, without which this article would not be possible. L. A. Aquino receives a grant for technical assistance from the National Council for Scientific and Technological Development (CNPq proc. 371704/2008-1).
Conflict of interest statement
LA Aquino, SE Pereira, JS Silva, CJ Saboya, and A Ramalho declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
de Aquino, L.A., Pereira, S.E., de Souza Silva, J. et al. Bariatric Surgery: Impact on Body Composition After Roux-en-Y Gastric Bypass. OBES SURG 22, 195–200 (2012). https://doi.org/10.1007/s11695-011-0500-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-011-0500-4