Abstract
Background
Laparoscopic Roux-en Y-Gastric bypass (LRYGBP) is the commonest available option for the surgical treatment of morbid obesity. Weight loss following bariatric surgery has been linked to changes of gastrointestinal peptides, shown to be implicated also in metabolic effects and appetite control. The purpose of this study was to evaluate whether gastric fundus resection in patients undergoing LRYGBP enhances the efficacy of the procedure in terms of weight loss, glucose levels, and hormonal secretion.
Methods
Twelve patients underwent LRYGBP and 12 patients LRYGBP plus gastric fundus resection (LRYGBP+FR). All patients were evaluated before and at 3, 6, and 12 months postoperatively. Blood samples were collected after an overnight fast and 30, 60, and 120 min after a standard 300-kcal mixed meal.
Results
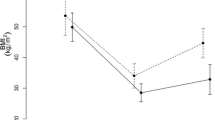
Body weight and body mass index decreased markedly and comparably after both procedures. Fasting ghrelin decreased 3 months after LRYGBP, but increased at 12 months to levels higher than baseline while after LRYGBP+FR was markedly and persistently decreased. Postprandial GLP-1, PYY, and insulin responses were enhanced more and postprandial glucose levels were lower after LRYGBP+FR compared to LRYGBP. Postoperatively, ghrelin changes correlated negatively with GLP-1 changes.
Conclusions
Resection of the gastric fundus in patients undergoing LRYGBP was associated with persistently lower fasting ghrelin levels; higher postprandial PYY, GLP-1, and insulin responses; and lower postprandial glucose levels compared to LRYGBP. These findings suggest that fundus resection in the setting of LRYGBP may be more effective than RYGBP for the management of morbid obesity and diabetes type 2.




Similar content being viewed by others
References
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357:753–61.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
Weber M, Muller MK, Bucher T, et al. Laparoscopic gastric bypass is superior to laparoscopic gastric banding for treatment of morbid obesity. Ann Surg. 2004;240:975–82.
Karra E, Batterham RL. The role of gut hormones in the regulation of body weight and energy homeostasis. Mol Cell Endocrinol. 2010;316:120–8.
Cummings DE, Weigle DS, Frayo RS, et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002;346:1623–30.
le Roux CW, Aylwin SJ, Batterham RL, et al. Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. Ann Surg. 2006;243:108–14.
Ashrafian H, le Roux CW. Metabolic surgery and gut hormones—a review of bariatric entero-humoral modulation. Physiol Behav. 2009;97:620–31.
Ashby D, Bloom SR. Recent progress in PYY research—an update report for 8th NPY meeting. Peptides. 2007;28:198–202.
Ranganath LR, Beety JM, Morgan LM, et al. Attenuated GLP-1 secretion in obesity: cause or consequence? Gut. 1996;38:916–9.
Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl. 1): S62–9.
Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27:1487–95.
Karamanakos SN, Vagenas K, Kalfarentzos F, et al. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy: a prospective, double blind study. Ann Surg. 2008;247:401–7.
Stoeckli R, Chanda R, Langer I, et al. Changes of body weight and plasma ghrelin levels after gastric banding and gastric bypass. Obes Res. 2004;12:346–50.
Faraj M, Havel PJ, Phelis S, et al. Plasma acylation-stimulating protein, adiponectin, leptin, and ghrelin before and after weight loss induced by gastric bypass surgery in morbidly obese subjects. J Clin Endocrinol Metab. 2003;88:1594–602.
Sundbom M, Holdstock C, Engstrom BE, et al. Early changes in ghrelin following Roux-en-Y gastric bypass: influence of vagal nerve functionality? Obes Surg. 2007;17:304–10.
Clements RH, Gonzalez QH, Long CI, et al. Hormonal changes after Roux-en Y gastric bypass for morbid obesity and the control of type-II diabetes mellitus. Am Surg. 2004;70:1–4.
Korner J, Bessler M, Cirilo LJ, et al. Effects of Roux-en-Y gastric bypass surgery on fasting and postprandial concentrations of plasma ghrelin, peptide YY, and insulin. J Clin Endocrinol Metab. 2005;90:359–65.
Bohdjalian A, Langer FB, Shakeri-Leidenmuhler S, et al. Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin. Obes Surg. 2010;20:535–40.
Cohen R, Uzzan B, Bihan H, et al. Ghrelin levels and sleeve gastrectomy in super-super-obesity. Obes Surg. 2005;15:1501–2.
Langer FB, Reza Hoda MA, Bohdjalian A, et al. Sleeve gastrectomy and gastric banding: effects on plasma ghrelin levels. Obes Surg. 2005;15:1024–9.
Wierup N, Bjorkqvist M, Westrom B, et al. Ghrelin and motilin are cosecreted from a prominent endocrine cell population in the small intestine. J Clin Endocrinol Metab. 2007;92:3573–81.
le Roux CW, Welbourn R, Werling M, et al. Gut hormones as mediators of appetite and weight loss after Roux-en-Y gastric bypass. Ann Surg. 2007;246:780–5.
Rodieux F, Giusti V, D’Alessio DA, et al. Effects of gastric bypass and gastric banding on glucose kinetics and gut hormone release. Obesity. 2008;16:298–305.
Vidal J, Nicolau J, Romero F, et al. Long-term effects of Roux-en-Y gastric bypass surgery on plasma glucagon-like peptide-1 and islet function in morbidly obese subjects. J Clin Endocrinol Metab. 2009;94:884–91.
Chelikani PK, Haver AC, Reidelberger RD. Ghrelin attenuates the inhibitory effects of glucagon-like peptide-1 and peptide YY(3–36) on food intake and gastric emptying in rats. Diabetes. 2006;55:3038–46.
Peterli R, Wolnerhanssen B, Peters T, et al. Improvement in glucose metabolism after bariatric surgery: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: a prospective randomized trial. Ann Surg. 2009;250:234–41.
Melissas J, Daskalakis M, Koukouraki S, et al. Sleeve gastrectomy—a “food limiting” operation. Obes Surg. 2008;18:1251–6.
Bernstine H, Tzioni-Yehoshua R, Groshar D, et al. Gastric emptying is not affected by sleeve gastrectomy—scintigraphic evaluation of gastric emptying after sleeve gastrectomy without removal of the gastric antrum. Obes Surg. 2009;19:293–8.
Ballantyne GH, Farkas D, Laker S, et al. Short-term changes in insulin resistance following weight loss surgery for morbid obesity: laparoscopic adjustable gastric banding versus laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2006;16:1189–97.
Kreymann B, Williams G, Ghatei MA, et al. Glucagon-like peptide-1 7–36: a physiological incretin in man. Lancet. 1987;2(8571):1300–4.
Meyer C. Final answer: ghrelin can suppress insulin secretion in humans, but is it clinically relevant? Diabetes. 2010;59:2726–8.
Tong J, Prigeon RL, Davis HW, et al. Ghrelin suppresses glucose-stimulated insulin secretion and deteriorates glucose tolerance in healthy humans. Diabetes. 2010;59:2145–51.
Sangiao-Alvarellos S, Cordido F. Effect of ghrelin on glucose–insulin homeostasis: therapeutic implications. Int J Pept 2010; 2010.pii. 234709. Epub 2010.
Bewick GA, Kent A, Campbell D, et al. Mice with hyperghrelinemia are hyperphagic and glucose intolerant and have reduced leptin sensitivity. Diabetes. 2009;58:840–6.
Morinigo R, Vidal J, Lacy AM, et al. Circulating peptide YY, weight loss, and glucose homeostasis after gastric bypass surgery in morbidly obese subjects. Ann Surg. 2008;247:270–5.
Callahan HS, Cummings DE, Pepe MS, et al. Postprandial suppression of plasma ghrelin level is proportional to ingested caloric load but does not predict intermeal interval in humans. J Clin Endocrinol Metab. 2004;89:1319–24.
Disclosures
Aikaterini Chronaiou declares no conflict of interest
Marina Tsoli declares no conflict of interest
Ioannis Kehagias declares no conflict of interest
Michalis Leotsinidis declares no conflict of interest
Fotis Kalfarentzos declares no conflict of interest
Theodore K. Alexandrides declares no conflict of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chronaiou, A., Tsoli, M., Kehagias, I. et al. Lower Ghrelin Levels and Exaggerated Postprandial Peptide-YY, Glucagon-Like Peptide-1, and Insulin Responses, After Gastric Fundus Resection, in Patients Undergoing Roux-en-Y Gastric Bypass: A Randomized Clinical Trial. OBES SURG 22, 1761–1770 (2012). https://doi.org/10.1007/s11695-012-0738-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-012-0738-5