Abstract
Objective
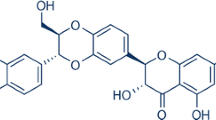
To reveal the neuroprotective effect and the underlying mechanisms of a mixture of the main components of Panax notoginseng saponins (TSPN) on cerebral ischemia-reperfusion injury and oxygen-glucose deprivation/reoxygenation (OGD/R) of cultured cortical neurons.
Methods
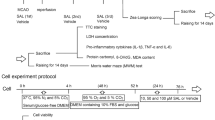
The neuroprotective effect of TSPN was evaluated by 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) assay, flow cytometry and live/dead cell assays. The morphology of dendrites was detected by immunofluorescence. Middle cerebral artery occlusion (MCAO) was developed in rats as a model of cerebral ischemia-reperfusion. The neuroprotective effect of TSPN was evaluated by neurological scoring, tail suspension test, 2,3,5-triphenyltetrazolium chloride (TTC) and Nissl stainings. Western blot analysis, immunohistochemistry and immunofluorescence were used to measure the changes in the Akt/mammalian target of rapamycin (mTOR) signaling pathway.
Results
MTT showed that TSPN (50, 25 and 12.5 µ g/mL) protected cortical neurons after OGD/R treatment (P<0.01 or P<0.05). Flow cytometry and live/dead cell assays indicated that 25 µ g/mL TSPN decreased neuronal apoptosis (P<0.05), and immunofluorescence showed that 25 µ g/mL TSPN restored the dendritic morphology of damaged neurons (P<0.05). Moreover, 12.5 µ g/mL TSPN downregulated the expression of Beclin-1, Cleaved-caspase 3 and LC3B-II/LC3B-I, and upregulated the levels of phosphorylated (p)-Akt and p-mTOR (P<0.01 or P<0.05). In the MCAO model, 50 µ g/mL TSPN improved defective neurological behavior and reduced infarct volume (P<0.05). Moreover, the expression of Beclin-1 and LC3B in cerebral ischemic penumbra was downregulated after 50 µ g/mL TSPN treatment, whereas the p-mTOR level was upregulated (P<0.05 or P<0.01).
Conclusion
TSPN promoted neuronal survival and protected dendrite integrity after OGD/R and had a potential therapeutic effect by alleviating neurological deficits and reversing neuronal loss. TSPN promoted p-mTOR and inhibited Beclin-1 to alleviate ischemic damage, which may be the mechanism that underlies the neuroprotective activity of TSPN.
Similar content being viewed by others
References
Pandian JD, Gall SL, Kate MP, Silva GS, Akinyemi RO, Ovbiagele BI, et al. Prevention of stroke: a global perspective. Lancet 2018;392:1269–1278.
Mueller M, Khamis D, Srivastava D, Exadaktylos AK, Pfortmueller CA. Understanding refugees’ health. Semin Neurol 2018;38:152–162.
Kim J, Fann DY, Seet RCS, Jo D, Mattson MP, Arumugam TV. Phytochemicals in ischemic stroke. Neuromolecular Med 2016;18:283–305.
Astrup J, Siesjo BK, Symon L. Thresholds in cerebral ischemia the ischemic penumbra. Stroke 1981;12:723–725.
Chauhan A, Sharma U, Jagannathan NR, Reeta KH, Gupta YK. Rapamycin protects against middle cerebral artery occlusion induced focal cerebral ischemia in rats. Behav Brain Res 2011;225:603–609.
Zhan L, Liu L, Li K, Wu B, Liu D, Liang D, et al. Neuroprotection of hypoxic postconditioning against global cerebral ischemia through influencing posttranslational regulations of heat shock protein 27 in adult rats. Brain Pathol 2017;27:822–838.
Li X, Li J, Qian J, Zhang D, Shen H, Li X, et al. Loss of ribosomal RACK1 (receptor for activated protein kinase C 1) induced by phosphorylation at T50 alleviates cerebral ischemia-reperfusion injury in rats. Stroke 2019;50:162–171.
Li Y, Su F, Wang L, Liu B, Shi Z, Deng J. Autophagy and hypoxic ischemic brain injuries. Acta Physiol Sin 2017;69:316–324.
Brady NR, HamacherBrady A, Yuan H, Gottlieb RA. The autophagic response to nutrient deprivation in the HL-1 cardiac myocyte is modulated by Bcl-2 and sarco/endoplasmic reticulum calcium stores. FEBS J 2007;274:3184–3197.
Kawano T, Fukunaga K, Takeuchi Y, Morioka M, Yano S, Hamada J, et al. Neuroprotective effect of sodium orthovanadate on delayed neuronal death after transient forebrain ischemia in gerbil hippocampus. J Cerebral Blood Flow Metab 2001;21:1268–1280.
Zhao H, Shimohata T, Wang J, Sun G, Schaal D, Sapolsky R, et al. Akt contributes to neuroprotection by hypothermia against cerebral ischemia in rats. J Neurosci 2005;25:9794–9806.
Hwang J, Gertner M, Pontarelli F, Court-Vazquez B, Bennett M, Ofengeim D, et al. Global ischemia induces lysosomal-mediated degradation of mTOR and activation of autophagy in hippocampal neurons destined to die. Cell Death Differ 2017;24:317–329.
Gaire B. Herbal medicine in ischemic stroke: challenges and prospective. Chin J Integr Med 2018;24:243–246.
Hu M, Zhou Z, Zhou Z, Lu H, Gao M, Liu L, et al. Effect and safety of hydroxysafflor yellow a for injection in patients with acute ischemic stroke of blood stasis syndrome: a phase II, multicenter, randomized, double-blind, multiple-dose, active-controlled clinical trial. Chin J Integr Med 2020;26:420–427.
Wang F, Wang S, Chai L, Zhang Y, Guo H, Hu L. Xueshuantong Injection (lyophilized) combined with salvianolate lyophilized injection protects against focal cerebral ischemia/reperfusion injury in rats through attenuation of oxidative stress. Acta Pharmacol Sin 2018;39:998–1011.
Sheng S, Wang J, Wang L, Liu H, Li P, Liu M, et al. Network pharmacology analyses of the antithrombotic pharmacological mechanism of Fufang Xueshuantong Capsule with experimental support using disseminated intravascular coagulation rats. J Ethnopharmacol 2014;154:735–744.
Wang L, Han L, Yu H, Sang M, Liu E, Zhang Y, et al. Analysis of the constituents in “Zhu She Yong Xue Shuan Tong” by ultra high performance liquid chromatography with quadrupole time-of-flight mass spectrometry combined with preparative high performance liquid chromatography. Molecules 2015;20:20518–20537.
Han S, Chen Y, Wang J, Zhang Q, Han B, Ge Y, et al. Anti-thrombosis effects and mechanisms by Xueshuantong Capsule under different flow conditions. Front Pharmacol 2019;10:35.
Huang Y, Guo B, Shi B, Gao Q, Zhou Q. Chinese herbal medicine Xueshuantong enhances cerebral blood flow and improves neural functions in Alzheimer’s disease mice. J Alzheimers Dis 2018;63:1089–1107.
Zhang J, Zhang B, Du M, Wang X, Li W. Chinese preparation Xuesaitong promotes the mobilization of bone marrow mesenchymal stem cells in rats with cerebral infarction. Neural Regen Res 2016;11:292–297.
Shen Q, Li J, Zhang C, Wang P, Mohammed A, Ni S, et al. Panax notoginseng saponins reduce high-risk factors for thrombosis through peroxisome proliferator-activated receptor- γ pathway. Biomed Pharmacother 2017;96:1163–1169.
Shi X, Yu W, Liu L, Liu W, Zhang X, Yang T, et al. Panax notoginseng saponins administration modulates pro-/anti-inflammatory factor expression and improves neurologic outcome following permanent MCAO in rats. Metab Brain Dis 2017;32:221–233.
Zhou J, Yang Y, Huang Z, Zou X, Liang X. Effect of Panax notoginseng saponins on cisplatin-induced kidney injury by enhancing mitochondrial autophagy via the HIF-1 α/BNIP3 pathway. Chin Pharm J 2017;52:196–200.
Shi QY, QH Z, Peng Y, Ying X, Lei W. A natural diarylheptanoid protects cortical neurons against oxygen-glucose deprivation-induced autophagy and apoptosis. J Pharm Pharmacol 2019;71:1110–1118.
Wu S, Yang T, Cen K, Zou Y, Shi X, Zhou D, et al. Panax notoginseng In vitro evaluation of the neuroprotective effect of saponins by activating the EGFR/PI3K/AKT pathway. Evid Based Complement Alternat Med 2020;2020:1403572.
Xiao HL, Zhang QH, Peng YH, Tang GY, Liao YM, Zhuang XJ, et al. 7-(4-Hydroxy-3-methoxypheny1)-1-pheny1–4E-hepten-3-one alleviates a beta 1–42 induced cytotoxicity through PI3K-mTOR pathways. Biochem Biophys Res Commun 2017;484:365–371.
Li J, Li H, Zhan D, Xiang M, Yang J, Zuo Y, et al. Niclosamide sensitizes nasopharyngeal carcinoma to radiation by downregulating Ku70/80 expression. J Cancer 2018;9:736–744.
Longa E, Weinstein P, Carlson S, Cummins R. Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke 1989;20:84–91.
Bederson J, Pitts L, Tsuji M, Nishimura M, Davis R, Bartkowski H. Rat middle cerebral artery occlusion: evaluation of the model and development of a neurologic examination. Stroke 1986;17:472–476.
Furutani R, Kibayashi K. Morphological alteration and reduction of MAP2-immunoreactivity in pyramidal neurons of cerebral cortex in a rat model of focal cortical compression. J Neurotrauma 2012;29:1266–1276.
Hendrickson ML, Ling C, Kalil RE. Degeneration of axotomized projection neurons in the rat dLGN: temporal progression of events and their mitigation by a single administration of FGF2. PLoS One 2012;7:e46918.
Li J, Chen Y, Zhang L, Xing L, Xu H, Wang Y, et al. Total saponins of panaxnotoginseng promotes lymphangiogenesis by activation VEGF-C expression of lymphatic endothelial cells. J Ethnopharmacol 2016;193:293–302.
Zhou L, Huang PP, Chen LL, Wang P. Panax notoginseng saponins ameliorate a β -mediated neurotoxicity in c. elegans through antioxidant activities. Evid Based Complement alternat Med 2019;2019:7621043.
Sun Z, Yang H, Wang Z, Pan J, Hong Z, Chen S. Erythropoietin prevents PC12 cells from beta-amyloid-induced apoptosis via PI3K/Akt pathway. Transl Neurodegener 2012;1:7.
Chen S, Liu J, Liu X, Fu Y, Zhang M, Lin Q, et al. Panax notoginseng saponins inhibit ischemia-induced apoptosis by activating PI3K/Akt pathway in cardiomyocytes. J Ethnopharmacol 2011;137:263–270.
Castaneda CA, Funes HC, Gomez HL, Ciruelos EM. The phosphatidyl inositol 3-kinase/AKT signaling pathway in breast cancer. Cancer Metast Rev 2010;29:751–759.
Yan Y, Li S, Li C, Xiong Y, Lu X, Zhou X, et al. Panax notoginsenoside saponins Rb1 regulates the expressions of Akt/mTOR/PTEN signals in the hippocampus after focal cerebral ischemia in rats. Behav Brain Res 2018;345:83–92.
He C, Klionsky DJ. Regulation mechanisms and signaling pathways of autophagy. Annu Rev Genet 2009;43:67–93.
Acknowledgement
The authors would like to thank the Key Laboratory for providing necessary facilities to ensure that the research was completed. We thank CHEN Ming and LIU Guan-ping for providing and testing the drug. We thank Dr. ZHANG Shi-qing for valuable suggestions on manuscript preparation.
Author information
Authors and Affiliations
Contributions
Li MM, Ye WC and Shi L conceived and designed the study; Wu DP and Liang HF performed the in vivo experiments and collected the data; Pan YW and Tang GY performed the in vitro experiments and collected the data; Fan CL prepared the sample and performed HPLC analysis; Wu DP, Pan YW, Liang HF, Li MM and Shi L wrote the manuscript; Li MM and Shi L revised the work for intellectual content and context; and all the authors read and approved the manuscript.
Corresponding author
Additional information
Conflict of Interest
All authors report no conflicts of interest, and no competing financial interests exist.
Supported by the National Key R&D Program of China (No. 2017YFC1703800), the Key-Area Research and Development Program of Guangdong Province (Nos. 2019B030335001 and 2020B1111110004), the Local Innovative and Research Teams Project of the Guangdong Pearl River Talents Program (No. 2017BT01Y036)
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Pan, Yw., Wu, Dp., Liang, Hf. et al. Total Saponins of Panax notoginseng Activate Akt/mTOR Pathway and Exhibit Neuroprotection in vitro and in vivo against Ischemic Damage. Chin. J. Integr. Med. 28, 410–418 (2022). https://doi.org/10.1007/s11655-021-3454-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11655-021-3454-y