Abstract
The relationships between age-related changes in circulating endogenous metabolites, inflammatory and oxidative stress markers, and arterial stiffness in 57 middle-aged (34–55 years), nonobese men were studied over the course of 3 years. Arterial stiffness was measured using brachial-ankle pulse wave velocities (ba-PWV). Plasma metabolomic profiling was performed using ultra-performance liquid chromatography and quadrupole time-of-flight mass spectrometry. After 3 years, decreased HDL cholesterol and increased malondialdehyde (MDA) and ox-LDL levels were observed. Among 15 identified lipids, lysoPCs (C16:0, C18:0, C18:2, C20:4, and C20:5) and linoleyl carnitine were the major plasma metabolites that contributed to the age-related differences. LysoPC16:0 (variable importance in the projection value, 6.2029) was found as the most important plasma metabolite for evaluating these changes. Changes in lysoPC16:0 levels positively correlated with the changes in 8-epi-PGF2α (r = 0.608), MDA (r = 0.413), high-sensitivity C-reactive protein (r = 0.509), IL-6 (r = 0.497), and ba-PWV (r = 0.283) levels. ba-PWV levels positively correlated with the changes in waist-to-hip ratios (WHR), inflammatory and oxidative stress markers. In a subgroup analysis of subjects with decreased ba-PWVs vs. increased ba-PWVs, changes in WHR and levels of lysoPC16:0, ba-PWV, IL-6, 8-epi-PGF2α, MDA, and P-selectin were significantly different. Our results suggest that age-related increases in lysoPC16:0 may contribute to lipid peroxidation, thereby activating proinflammatory phenotypes and arterial stiffness.
Similar content being viewed by others
Introduction
Aging and increased levels of circulating proinflammatory markers and oxidized LDLs (ox-LDLs) are associated with arterial stiffness (Kampus et al. 2007; Byfield et al. 2006; Brinkley et al. 2009; Scuteri et al. 2011). In particular, arterial stiffness increases with age, even in healthy individuals without clinical cardiovascular disease (CVD) (Zieman et al. 2005). Although the exact mechanism of age-related arterial stiffness is not fully understood, changes in numerous endogenous metabolites in a complex physiological aging process (Nevedomskaya et al. 2010; Yan et al. 2009) could partly result in increases of proinflammation, oxidative stress, and arterial stiffness. Particularly, lysophosphatidylcholines (lysoPCs), proinflammatory lipid mediators, are generated from phospholipase A2 (PLA2)-catalyzed hydrolysis of phosphatidylcholine. In addition, lysoPCs are reported to constitute only 1–5 % of the total PC content of non-ox-LDL; however, about 40–50 % of PC contained within LDL molecules is converted to lysoPC during LDL oxidation (Matsumoto et al. 2007). LysoPCs are also formed by the action of lecithin cholesterol acyltransferase in plasma (Kougias et al. 2006; Matsumoto et al. 2007). Recently, the inflammation induced by saturated or mono-unsaturated acyl-lysoPC in vitro has been well established. Therefore, understanding of age-related changes in these metabolites and their relationships with inflammatory and oxidative stress markers will allow better understanding of the pathological or physiological processes underlying arterial stiffness, a condition closely associated with aging.
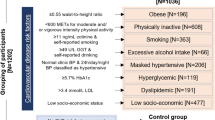
Accordingly, to study the relationship of age-related changes in the levels of endogenous metabolites and inflammatory and oxidative stress markers with arterial stiffness, we observed 57 nonobese men between the ages of 34 and 55 years, without a disease history for 3 years. To compare age-related changes between the baseline and 3-year follow-up data, we used a metabolomics approach based on the combination of ultra-performance liquid chromatography and quadrupole time-of-flight mass spectrometry (UPLC-Q-TOF MS) coupled with multivariate data analyses. Additionally, to analyze the oxidative and inflammatory status of the study subjects at baseline and after 3 years, we measured the levels of inflammatory and oxidative markers using specific immunoassays and measured arterial stiffness using brachial-ankle pulse wave velocity (ba-PWV).
Experimental
Subjects
The study protocol was approved by the Institutional Review Board of the National Health Insurance Corporation (NHIC)-sponsored Ilsan Hospital, Korea, and was conducted in accordance with the Helsinki Declaration. Fifty-seven healthy, nonobese male subjects (20 ≤ body mass index (BMI) < 30 kg/m2) between the ages of 34–55 years visiting a health promotion center at the NHIC-sponsored Ilsan Hospital in Korea between August 2007 and October 2007 were enrolled in this study. The subjects led a sedentary lifestyle and had not participated in weight reduction programs within the previous 3 years. The subjects also completed a personal health and medical history questionnaire that served as a screening tool for enrollment. Exclusion criteria included the presence of type 2 diabetes, CVD, or psychiatric problems, or the use of anti-hypertensive, lipid-lowering, anti-platelet, or anti-diabetic medications. The duration of the study was 3 years. At baseline, the usual dietary intake of the study subjects was assessed using a semiquantitative food frequency questionnaire and a 24-h recall method. The subjects were encouraged to maintain their body weight within ±3 kg and were given general oral and written information about healthy food choices and exercise at baseline and at the subsequent visit (week 4). The subjects were instructed by trained dietitians and were also asked to keep 3-day food records (2 weekdays and 1 weekend) at each visit. Nutrient intake was determined and calculated based on the 3-day food records using the Computer-Aided Nutritional Analysis Program (CAN-pro 2.0; Korean Nutrition Society, Seoul, Korea). Total energy expenditure (TEE) (kcal/day) was calculated based on the activity patterns of the study subjects, such as basal metabolic rate, 24-h physical activity, and specific dynamic actions of food.
Anthropometric parameters, blood pressure, and blood collection
Body weights and heights were measured in the morning while the study subjects were unclothed and without shoes. BMI (kg/m2) was calculated based on body weight and height. Percent body fat was analyzed using a TBF-105 body fat analyzer (Tanita Co., Tokyo, Japan). Waist circumference was measured at the umbilical level, with the subjects standing after normal expiration. Blood pressure (BP) was measured in the left arm of seated patients using an automatic blood pressure monitor (TM-2654, A&D, Tokyo, Japan) after a 20-min rest period. After a 12-h fast, venous blood specimens were collected in EDTA-treated or untreated tubes. Plasma or sera were separated and stored at −70 °C until further analysis.
Serum lipid profiles and fasting glucose levels, insulin concentrations, and homeostasis model assessment for insulin resistance
Fasting total cholesterol and triglyceride levels were measured using commercially available kits and a Hitachi 7150 autoanalyzer (Hitachi Ltd., Tokyo, Japan). After precipitation of serum chylomicrons using dextran sulfate magnesium, HDL cholesterol concentrations in the supernatants were enzymatically measured. For subjects with serum triglyceride levels <400 mg/dL, LDL cholesterol levels were estimated directly using the Friedwald formula: LDL cholesterol = total cholesterol − (HDL cholesterol + [triglycerides/5]). For subjects with serum triglyceride levels ≥400 mg/dL, LDL cholesterol levels were measured indirectly. Fasting glucose levels were measured by the glucose oxidase method using a Beckman glucose analyzer (Beckman Instruments, Irvine, CA, USA). Insulin levels were measured by radioimmunoassay using a commercial kit (Immuno Nucleo Corporation, Stillwater, MN, USA). Insulin resistance (IR) was calculated based on the homeostasis model assessment (HOMA) using the following equation: HOMA-IR = (fasting insulin [μIU/mL] × fasting glucose [mmol/L])/22.5.
Measurement of serum IL-6 levels, serum high-sensitivity C-reactive protein levels, white blood cell counts, and urinary 8-epi-PGF2α levels
Serum interleukin (IL)-6 concentrations were measured using Bio-Plex™ Reagent Kits and a Bio-Plex™ system (Bio-Rad Laboratories, Hercules, CA, USA) according to the manufacturer’s instructions. The high-sensitivity C-reactive protein (hs-CRP) levels were measured on an Express Plus™ auto-analyzer (Chiron Diagnostics Co., Walpole, MA, USA) using commercially available high-sensitivity CRP-Latex (II) X2 kits (Seiken Laboratories Ltd., Tokyo, Japan). White blood cell (WBC) counts were determined using a hematology analyzer from HORIBA ABX Diagnostic (HORIBA ABX SAS, Parc Euromedicine, France). The compound 8-epi-PGF2α was measured using an enzyme immunoassay (BIOXYTECH urinary 8-epi-PGF2αTM Assay kit, OXIS International Inc., Portland, OR, USA). Urinary creatinine levels were determined using the alkaline picrate (Jaffe) reaction.
Plasma-oxidized LDL, adiponectin, malondialdehyde, sVCAM-1, sICAM-1, and P-selectin levels
Plasma-oxidized (ox) LDL levels were measured using an enzyme immunoassay (Mercodia, Uppsala, Sweden). Plasma adiponectin concentrations were measured using an enzyme immunoassay (Human Adiponectin ELISA kit, B-Bridge International Inc., CA, USA). The absorbencies of the resulting color reactions (ox-LDLs and adiponectin) were measured at a wavelength of 450 nm using a Wallac Victor2 multilabel counter (Perkin Elmer Life Sciences, Turku, Finland). The wavelength correction was set to 540 nm. Plasma malondialdehyde (MDA) concentrations were measured based on the production of thiobarbituric acid-reactive substances (TBARS Assay Kit, Zepto-Metrix Co., Buffalo, NY, USA). Plasma vascular cell adhesion molecule (VCAM)-1, inter-cellular adhesion molecule (ICAM)-1, and P-selectin levels were measured using Bio-Plex™ Reagent Kits with a Bio-Plex™ system (Bio-Rad) according to the manufacturer’s instructions.
Brachial-ankle pulse wave velocity measurement
ba-PWVs were measured using an automatic waveform analyzer (model VP-1000; Nippon Colin Ltd., Komaki, Japan) according to a previously described method (Kim et al. 2010a, b). The average ba-PWV from both left and right sides was used for analysis (correlation between the right and left ba-PWVs: r 2 = 0.925, P < 0.001).
Plasma metabolic profiling
Plasma samples were prepared and injected into a UPLC/Q-TOF MS (Waters, Milford, MA, USA) according to previously described methods (Kim et al. 2010a, b). The Q-TOF MS was operated in positive electrospray ionization (ESI) mode. The capillary and sampling cone voltages were set at 2.78 kV and 26 V, respectively. The desolvation flow was set to 700 L/h at 300 °C, and the source temperature was set to 110 °C. The TOF MS data were collected in the range of 50–1000 m/z, with a scan time of 0.2 s and interscan delay time of 0.02 s. All analyses were performed using lock spray to ensure accuracy and reproducibility; leucine-enkephalin (556.2771 Da in the positive ESI mode) was used as the lock mass at 200 pmol and a flow rate of 3 μL/min. The lock spray frequency was set at 10 s.
For quality control, a mixture of five standard compounds (caffeine, sulfadimethoxine, terfenadine, 4-acetoaminophenol, and reserpine) was injected after every seven samples. The MS/MS spectra of the metabolites were obtained by a collision energy ramp from 10 to 30 eV. Accurate masses and compositions of the precursor and fragment ions were calculated and sequenced using MassLynx 4.1 software (Waters) incorporated in the instrument. All MS data, including retention time, m/z, and ion intensity, were extracted using the MarkerLynx 4.1 software package (Waters) incorporated in the instrument, and the resulting MS data were assembled into a data matrix.
Peaks were collected using a peak width of 5 %, a height of 1 s, a noise elimination of 6, and an intensity threshold of 120. Data were aligned with a mass tolerance of 0.04 Da and a retention time window of 0.15 min. All spectra were aligned and normalized to the total peak intensity. Assignment of metabolites contributing to the observed variance was performed using the elemental composition analysis software using calculated mass, mass tolerance (mDa and ppm), double-bond equivalent, and the i-Fit algorithm (the likelihood that the isotopic pattern of the elemental composition matches a cluster of peaks in the spectrum) implemented in the MassLynx software by the ChemSpider database (www.chemspider.com) and by the Human Metabolome Database (www.hmdb.ca). Authentic standards were used to confirm the assignments and to perform quantitative analyses.
Statistical analysis
Statistical analyses were performed using SPSS ver12.0 (Statistical Package for the Social Sciences, SPSS Inc., Chicago, IL, USA). The skewed variables were logarithmically transformed for statistical analysis. For descriptive purposes, mean values were presented using untransformed values. Results are expressed as means ± standard error (SE). A two-tailed P value of <0.05 was considered as statistically significant. Paired t-tests and Wilcoxon signed-rank tests were used to evaluate differences between baseline and 3-year follow-up levels. Differences in the clinical variables between the decreased ba-PWV and increased ba-PWV groups were tested by independent t-tests and Mann–Whitney U-tests. General linear model tests (mixed model tests) were applied to the comparison of the changes in variables over time by adjusting for confounding factors. Pearson’s and partial correlation coefficients were used to examine the relationships between variables over time.
Multivariate statistical analysis was performed using SIMCA-P+ software version 12.0 (Umetrics, Umeå, Sweden). Partial least-squares discriminant analysis (PLS-DA) was used as the classification method for modeling discrimination between the baseline and 3-year follow-up data by visualizing score plots or S-plots using the first and second PLS components. To validate the model, a sevenfold validation was applied to the PLS-DA model, and the reliabilities of the model were further rigorously validated by a permutation test (n = 200). Goodness of fit was quantified by R2Y, while the predictive ability was indicated by Q2Y. Generally, R2Y, which describes how well the data in the training set are mathematically reproduced, varies between 0 and 1, with 1 indicating a model with a perfect fit.
Results
Clinical characteristics, inflammatory markers, arterial stiffness, lipid peroxides, adhesion molecules, and nutrient intakes at baseline and at 3-year follow-up
After 3 years, the subjects showed decreased levels of HDL cholesterol (P < 0.001) and increased levels of MDA (P < 0.001) and ox-LDLs (P < 0.001) (Table 1). There were no significant differences in the levels of inflammatory markers, arterial stiffness, and adhesion molecules between the baseline and 3-year follow-up data. The estimated total calorie intake at baseline was 2,441 ± 27 kcal/day and at 3-years follow-up was 2,429 ± 23 kcal/day. There were no statistically significant differences in macronutrient intakes, especially polyunsaturated/monounsaturated/saturated (P/M/S) fat intake ratio between the baseline (1:0.96:0.72) and the 3-year follow-up (1:1.01:0.74) data. Also, there were no significant differences in total energy expenditure and the proportions of smoking and drinking between the baseline and the 3-year follow-up data (data not shown).
Multivariate statistical analysis and identification of plasma metabolites
The MS data of plasma metabolites obtained from healthy men at baseline and at 3-year follow-up were applied to a PLS-DA score plot (Fig. 1a). The first two-component PLS-DA score plots of the plasma metabolites showed distinct clustering for each group of healthy men at baseline and at 3-year follow-up. Both groups could be clearly differentiated from each other by the primary component t(1) or the secondary component t(2) based on the model with R2X (cum) and R2Y (cum) values of 0.391 and 0.990, respectively, indicating the goodness of fit of the data. The Q2Y (cum) value of 0.818 estimated the predictive ability of the model. In addition, the PLS-DA models were validated using a permutation test and indicated an R2Y intercept value of 0.0971 and a Q2Y intercept value of 0.0113. To identify the metabolites contributing to the discrimination between the baseline and the 3-year follow-up data, S-plots of p(1) and p(corr)(1) were generated using centroid scaling (Fig. 1b). The S-plots revealed that the metabolites with higher or lower p(corr) values served as the more relevant ions for discriminating between the two groups.
Among the 813 metabolites in the plasma, the metabolites that play an important role in determining age-related changes after the 3-year follow-up were selected according to their variable importance in the projection (VIP) scores. The normalized intensities of whole metabolites were statistically analyzed by a nonparametric t-test; the metabolites with significant differences between the baseline and 3-year follow-up data were included. Thus, 17 metabolites were selected based on their VIP values and independent t-tests. Finally, 15 metabolites were identified (two were unknown). The results of the UPLC-Q-TOF analysis are shown in Table 2.
Eight plasma metabolites, including l-valine, lysophosphatidyl cholines (lysoPCs) containing C16:0, C18:2, C20:4, C20:5, C22:5, and C22:6, and lysophosphatidyl ethanolamines (lysoPEs) containing C18:0 and C22:6, showed significant increases at 3-year follow-up, whereas three metabolites, including pyrroline hydroxycarboxylic acid, linoleyl carnitine, and total lysoPCs, showed decreased levels. Linoleyl carnitine and lysoPCs containing C16:0, C18:0, C18:2, C20:4, and C20:5 (with VIP values >1.0, indicating a high relevance to the difference between the sample groups) were the major plasma metabolites contributing to the discrimination between the baseline and 3-year follow-up data on the PLS-DA score plot (Table 2). In particular, lysoPC 16:0 with a VIP value of 6.2029 served as the most important plasma metabolite for evaluating the differences between the baseline and 3-year follow-up data.
Relationship between the changes in the major plasma metabolite levels
The changes in lysoPC 16:0 levels were positively correlated with the changes in lysoPC 18:0 (r = 0.624, P < 0.001), lysoPC 18:2 (r = 0.620, P < 0.001), and lysoPC 20:5 (r = 0.414, P = 0.003) levels. The changes in lysoPC 18:0 were positively correlated with the changes in lysoPC 18:2 (r = 0.773, P < 0.001) and lysoPC 20:5 (r = 0.600, P < 0.001). The changes in lysoPC 18:2 were positively correlated with the changes in lysoPC 20:4 (r = 0.325, P = 0.023) and lysoPC 20:5 (r = 0.395, P = 0.005). The changes in linoleyl carnitine were positively correlated with the changes in pyrroline hydroxycarboxylic acid (r = 0.464, P = 0.001).
Relationship between the changes in levels of lysoPC 16:0, arterial stiffness, lipid peroxides, inflammatory markers, and adhesion molecules
The changes in lysoPC 16:0 between the baseline and 3-year follow-up data were positively correlated with the changes in 8-epi-PGF2α (r = 0.608, P < 0.001) (Fig. 2), MDA (r = 0.413, P = 0.004), hs-CRP (r = 0.509, P < 0.001) (Fig. 2), IL-6 (r = 0.497, P = 0.001), and ba-PWV (r = 0.283, P = 0.049). Additionally, decreased HDL cholesterol was significantly associated with increased levels of lysoPC 20:5 (r = −0.286, P = 0.049) and lysoPC 22:6 (r = −0.422, P = 0.003) among the 15 endogenous metabolites, which were maintained after adjusting for changed values of age, BMI, LDL cholesterol, and triglyceride (r = −0.295, P = 0.052; r = −0.466, P = 0.001, respectively). The changes in ba-PWV were positively correlated with the changes in waist-to-hip ratio (WHR) (r = 0.329, P = 0.012) (Fig. 2), ox-LDLs (r = 0.312, P = 0.023), MDA (r = 0.302, P = 0.024), hs-CRP (r = 0.329, P = 0.013), IL-6 (r = 0.298, P = 0.038) (Fig. 2), and P-selectin (r = 0.345, P = 0.034). The changes in hs-CRP were positively correlated with the changes in 8-epi-PGF2α (r = 0.541, P < 0.001) (Fig. 2), ox-LDLs (r = 0.296, P = 0.033), and IL-6 (r = 0.635, P < 0.001). Additionally the changes in IL-6 were also positively correlated with the changes in WHR (r = 0.287, P = 0.046) and 8-epi-PGF2α (r = 0.311, P = 0.031). Furthermore, the ratio of total calorie intake to total calorie expenditure (TCI/TEE) was closely related with the changes in WHR (r = 0.450, P < 0.001).
Association of the levels of inflammatory markers, lipid peroxides, adhesion molecules, and metabolites with the changes in arterial stiffness
Because of the close relationship between the changes in levels of lysoPC 16:0, arterial stiffness, lipid peroxides, inflammatory markers, and adhesion molecules, we divided our subjects into two groups according to the changes in arterial stiffness from baseline to 3-year follow-up (decreased ba-PWV vs. increased ba-PWV groups). As ba-PWV was highly associated with blood pressure (systolic and diastolic), we adjusted for blood pressure when we compared the values between the groups. At baseline, men in the increased ba-PWV group (n = 30) had lower hs-CRP levels (P = 0.039) than those in the decreased ba-PWV group had. After 3 years, men in the decreased ba-PWV group (n = 27) showed a significant reduction in ba-PWVs (P < 0.001) and serum IL-6 (P = 0.038) levels and significant increases in the levels of MDA (P = 0.032) and ox-LDLs (P = 0.009) (Table 3). Men in the increased ba-PWV group showed significant increases in WHR (P = 0.025) and levels of ba-PWV (P < 0.001), MDA (P < 0.001), ox-LDLs (P = 0.002), and P-selectin (P = 0.002) after 3 years. In addition, the changes in WHR (P = 0.043), ba-PWV (P < 0.001), IL-6 (P = 0.038), 8-epi-PGF2α (P = 0.004), MDA (P = 0.027), and P-selectin (P = 0.004) levels were significantly different between the two ba-PWV groups after adjustment for changes of blood pressure (Table 3). Additionally, changes in lysoPC 16:0 levels were significantly different between the decreased and increased ba-PWV groups (−14.7 ± 50.7 vs. 106.4 ± 29.5; P = 0.049) after the adjustment. There were no significant changes in other plasma metabolite levels between the ba-PWV groups before or after adjustment for baseline values (data not shown).
Discussion
Using a metabolomics approach based on UPLC/Q-TOF MS, we identified 15 endogenous metabolites that showed age-related changes in middle-aged men. Among these metabolites, lysoPCs containing C16:0, C18:0, C18:2, C20:4, and C20:5 and linoleyl carnitine were the six major metabolites contributing to the discrimination between the baseline and 3-year follow-up. Various species of lysoPC are defined by fatty acid chain length and degree of saturation, which may translate into different physical and biological properties (Loftus et al. 2008). Although lysoPC levels obviously increase in aging rats (Fu et al. 2011), this important issue is largely unexplored in humans. In our study, among the six major metabolites identified by mass spectrometric analysis, lysoPC 16:0 was found to be the most important plasma metabolite for evaluating aging-related changes. Additionally, the changes in lysoPC 16:0 levels were strongly positively correlated with the changes in levels of 8-epi-PGF2α, a reliable marker of oxidative stress (Wolfram et al. 2005; Vassalle et al. 2004), MDA, hs-CRP, IL-6, and ba-PWVs. This result suggests that age-related changes in lysoPC 16:0 levels in middle-aged men could contribute to lipid peroxidation, the activation of a proinflammatory phenotype, and arterial stiffness. Furthermore, increases in lysoPC 16:0 levels from the baseline to the 3-year follow-up data were significantly greater in subjects with increased ba-PWVs. Pulse wave velocity is an established index of arterial stiffness (Tomiyama and Yamashina 2010), and ba-PWVs show similar characteristics to those of central aortic PWV (Tsuchikura et al. 2010).
Arterial stiffness, one of the most significant manifestations of vascular aging (Lakatta and Levy 2003; Lakatta 2003), can result in increased systolic blood pressure (Dao et al. 2005; O’Rourke and Hashimoto 2007). This is a condition that can worsen with age, even in healthy individuals without CVD. In addition, the presence of CVD risk factors such as obesity may accelerate the vascular changes that result in arterial stiffness (Zieman et al. 2005). However, in our study, we did not find significant changes overall in ba-PWV and WHR in subjects during the 3-year follow-up. When we subdivided study subjects according to the changed levels of ba-PWV, we found interesting results. Men in the subgroup of increased ba-PWVs showed significant increases in abdominal obesity, which were correlated with increases in IL-6 and the ratio of TCI/TEE (the ratio of total calorie intake to total calorie expenditure). Additionally, changes in WHR, MDA, hs-CRP, IL-6, 8-epi-PGF2α, and P-selectin levels were significantly different between subjects with decreased and increased ba-PWVs. However, the changes in MDA together with those in ox-LDL were in the same direction in both ba-PWV sub-groups (increased in both) which may need to be further studied as to whether this phenomenon occurs independent of ba-PWV change or not. Actually, the mechanisms underlying arterial stiffening remain to be elucidated, but the fact that changes in ba-PWV between the baseline and 3-year follow-up data were positively correlated with the changes in WHR, ox-LDLs, MDA, hs-CRP, and IL-6 levels suggest that changes in oxidative stress, proinflammation, or abdominal obesity could play an important role, in part, in accelerating arterial stiffness. Recently, Brinkley et al. (2009) suggested that ox-LDL levels may be related to the pathogenesis of arterial stiffness, independent of other CVD risk factors.
LysoPC constitutes only 1–5 % of the total PC content of non-ox-LDL; however, as much as 40–50 % of the PC contained within the LDL molecule is converted to lysoPC during LDL oxidation (Matsumoto et al. 2007). A saturated fatty acid or a monounsaturated fatty acid predominates in the sn-1 position of the phospholipid (Stafforini et al. 2006). The generation of free radicals as a result of oxidative stress can activate phospholipase A2 (PLA2), which hydrolyzes phosphatidylcholine (PC) to produce lysoPCs (Steinbrecher and Pritchard 1989). Production of α-palmitoyl-lysoPC (C16:0) can stimulate endothelial cells to express adhesion molecules and release cytokines (Takabe et al. 2004; Kume et al. 1992; Murohara et al. 1996; Zhu et al. 1997; Liu-Wu et al. 1998; Rong et al. 2002). In fact, IL-6 was found to be induced by α-palmitoyl-lysoPC treatment in human umbilical vein endothelial cells. In line with this result, our study showed a significant age-related increase in both ox-LDL and lysoPC 16:0 levels and a positive relationship between the changes in lysoPC 16:0 and IL-6 levels.
PLA2, including secretory PLA2 (sPLA2) and lipoprotein-associated phospholipase (Lp-PLA2), hydrolyzes PC, simultaneously generating one molecule of lysoPC and one molecule of arachidonic acid, a precursor of eicosanoids such as prostaglandins and leukotrienes (Matsumoto et al. 2007). Radical peroxidation of arachidonic acid results in a family prostaglandin F2-isomers called F2 isoprostanes (Voss and Siem 2006). One such F2-isoprostane is 8-epi-PGF2α, a sensitive marker for oxidative stress (Wolfram et al. 2005; Vassalle et al. 2004) that is probably released into biological fluids through a phospholipase-mediated pathway and consequently excreted in urine. In this study, changes in lysoPC 16:0 were closely and positively associated with changes in urinary 8-epi-PGF2α concentrations. Additionally, changes in lysoPC 16:0 and 8-epi-PGF2α were closely related with changes in CRP concentrations.
LysoPCs, representing 5–20 % of the total plasma phospholipids (Nelson 1967), are also formed by the action of lecithin cholesterol acyltransferase (LCAT) in plasma (Kougias et al. 2006). Human LCAT releases lysoPC 20:4 and 22:6 from the sn-1 position of PC (Liu et al. 1998). In plasma, up to 80 % of the lysoPC is found in the non-lipoprotein fraction, in which albumin is considered to be the main lipid-binding protein (Ojala et al. 2006). Unsaturated lysoPCs are mainly associated with albumin rather than lipoproteins (Croset et al. 2000). In our study, we observed a positive relationship between the changes in levels of lysoPC 16:0 and those of lysoPCs containing C18:0, C18:2, and C20:5, which could reflect an alternative source of lysoPC C16:0 production in addition to ox-LDLs.
In our study, a large number of metabolite markers were detected by UPLC-MS; however, most of these metabolite markers remain unidentified. Unlike gas chromatography–mass spectrometry, for which large databases exist, the use of liquid chromatography–mass spectrometry-based techniques for metabolomics research is still in its infancy, and the databases of endogenous biomolecules have not yet been constructed (Williams et al. 2006). Despite this limitation, using a UPLC-Q-TOF MS-based metabolomics strategy and multivariate data analysis, our study identified a cluster of age-associated changes in plasma metabolites that included six major metabolites: lysoPCs containing C16:0, C18:0, C18:2, C20:4, and C20:5 and linoleyl carnitine. Among these six major metabolites, lysoPC 16:0 served as the most important plasma metabolite for evaluating age-related differences between the baseline and 3-year follow-up data. Additionally, the changes in lysoPC 16:0 levels were positively correlated with the changes in levels of lipid peroxides, proinflammatory markers, and ba-PWV. These results suggest that increases in lysoPC 16:0 can be explored further as a potential marker for lipid peroxidation, the activation of a proinflammatory phenotype, and arterial stiffness related to aging.
References
Brinkley TE, Nicklas BJ, Kanaya AM, Satterfield S, Lakatta EG, Simonsick EM, Sutton-Tyrrell K, Kritchevsky SB (2009) Plasma oxidized low-density lipoprotein levels and arterial stiffness in older adults: the health, aging, and body composition study. Hypertension 53:846–852
Byfield FJ, Tikku S, Rothblat GH, Gooch KJ, Levitan I (2006) OxLDL increases endothelial stiffness, force generation, and network formation. J Lipid Res 47:715–723
Croset M, Brossard N, Polette A, Lagarde M (2000) Characterization of plasma unsaturated lysophosphatidylcholines in human and rat. Biochem J 345(Pt1):61–67
Dao HH, Essalihi R, Bouvet C, Moreau P (2005) Evolution and modulation of age-related medial elastocalcinosis: impact on large artery stiffness and isolated systolic hypertension. Cardiovasc Res 66:307–317
Fu C, Wang T, Wang Y, Chen X, Jiao J, Ma F, Zhong M, Bi K (2011) Metabonomics study of the protective effects of green tea polyphenols on aging rats induced by d-galactose. J Pharm Biomed Anal 55:1067–1074
Kampus P, Kals J, Ristimäe T, Muda P, Ulst K, Zilmer K, Salonen RM, Tuomainen TP, Teesalu R, Zilmer M (2007) Augmentation index and carotid intima-media thickness are differently related to age, C-reactive protein and oxidized low-density lipoprotein. J Hypertens 25:819–825
Kim JY, Park JY, Kim OY, Ham BM, Kim HJ, Kwon DY, Jang Y, Lee JH (2010a) Metabolic profiling of plasma in overweight/obese and lean men using ultra performance liquid chromatography and Q-TOF mass spectrometry (UPLC-Q-TOF MS). J Proteome Res 9:4368–4375
Kim OY, Yoe HY, Kim HJ, Park JY, Kim JY, Lee SH, Lee JH, Lee KP, Jang Y, Lee JH (2010b) Independent inverse relationship between serum lycopene concentration and arterial stiffness. Atherosclerosis 208:581–586
Kougias P, Chai H, Lin PH, Lumsden AB, Yao Q, Chen C (2006) Lysophosphatidylcholine and secretory phospholipase A2 in vascular disease: mediators of endothelial dysfunction and atherosclerosis. Med Sci Monit 12:RA5–RA16
Kume N, Cybulsky MI, Gimbrone MA Jr (1992) Lysophosphatidylcholine, a component of atherogenic lipoproteins, induces mononuclear leukocyte adhesion molecules in cultured human and rabbit arterial endothelial cells. J Clin Invest 90:1138–1144
Lakatta EG, Levy D (2003) Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: part I: aging arteries: a “set up” for vascular disease. Circulation 107:139–146
Lakatta EG (2003) Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: part III: cellular and molecular clues to heart and arterial aging. Circulation 107:490–497
Liu M, Subramanian VS, Subbaiah PV (1998) Modulation of the positional specificity of lecithin–cholesterol acyltransferase by the acyl group composition of its phosphatidylcholine substrate: role of the sn-1-acyl group. Biochemistry 37:13626–13633
Liu-Wu Y, Hurt-Camejo E, Wiklund O (1998) Lysophosphatidylcholine induces the production of IL-1beta by human monocytes. Atherosclerosis 137:351–357
Loftus N, Miseki K, Iida J, Gika HG, Theodoridis G, Wilson ID (2008) Profiling and biomarker identification in plasma from different Zucker rat strains via high mass accuracy multistage mass spectrometric analysis using liquid chromatography/mass spectrometry with a quadrupole ion trap-time of flight mass spectrometer. Rapid Commun Mass Spectrom 22:2547–2554
Matsumoto T, Kobayashi T, Kamata K (2007) Role of lysophosphatidylcholine (LPC) in atherosclerosis. Curr Med Chem 14:3209–3220
Murohara T, Scalia R, Lefer AM (1996) Lysophosphatidylcholine promotes P-selectin expression in platelets and endothelial cells. Possible involvement of protein kinase C activation and its inhibition by nitric oxide donors. Circ Res 78:780–789
Nelson GT (1967) The phospholipid composition of plasma in various mammalian species. Lipids 2:323–328
Nevedomskaya E, Meissner A, Goraler S, de Waard M, Ridwan Y, Zondag G, van der Pluijm I, Deelder AM, Mayboroda OA (2010) Metabolic profiling of accelerated aging ERCC1 d/- mice. J Proteome Res 9:3680–3687
Ojala PJ, Hermansson M, Tolvanen M, Polvinen K, Hirvonen T, Impola U, Jauhiainen M, Somerharju P, Parkkinen J (2006) Identification of alpha-1 acid glycoprotein as a lysophospholipid binding protein: a complementary role to albumin in the scavenging of lysophosphatidylcholine. Biochemistry 45:14021–14031
O’Rourke MF, Hashimoto J (2007) Mechanical factors in arterial aging: a clinical perspective. J Am Coll Cardiol 50:1–13
Rong JX, Berman JW, Taubman MB, Fisher EA (2002) Lysophosphatidylcholine stimulates monocyte chemoattractant protein-1 gene expression in rat aortic smooth muscle cells. Arterioscler Thromb Vasc Biol 22:1617–1623
Scuteri A, Orru M, Morrell C, Piras MG, Taub D, Schlessinger D, Uda M, Lakatta EG (2011) Independent and additive effects of cytokine patterns and the metabolic syndrome on arterial aging in the SardiNIA Study. Atherosclerosis 215:459–464
Stafforini DM, Sheller JR, Blackwell TS, Sapirstein A, Yull FE, McIntyre TM, Bonventre JV, Prescott SM, Roberts LJ 2nd (2006) Release of free F2-isoprostanes from esterified phospholipids is catalyzed by intracellular and plasma platelet-activating factor acetylhydrolases. J Biol Chem 281:4616–4623
Steinbrecher UP, Pritchard PH (1989) Hydrolysis of phosphatidylcholine during LDL oxidation is mediated by platelet-activating factor acetylhydrolase. J Lipid Res 30:305–315
Takabe W, Kanai Y, Chairoungdua A, Shibata N, Toi S, Kobayashi M, Kodama T, Noguchi N (2004) Lysophosphatidylcholine enhances cytokine production of endothelial cells via induction of l-type amino acid transporter 1 and cell surface antigen 4 F2. Arterioscler Thromb Vasc Biol 24:1640–1645
Tomiyama H, Yamashina A (2010) Non-invasive vascular function tests: their pathophysiological background and clinical application. Circ J 74:24–33
Tsuchikura S, Shoji T, Kimoto E, Shinohara K, Hatsuda S, Koyama H, Emoto M, Nishizawa Y (2010) Brachial-ankle pulse wave velocity as an index of central arterial stiffness. J Atheroscler Thromb 17:658–665
Vassalle C, Petrozzi L, Botto N, Andreassi MG, Zucchelli GC (2004) Oxidative stress and its association with coronary artery disease and different atherogenic risk factors. J intern Med 256:308–315
Voss P, Siem W (2006) Clinical oxidation parameters of aging. Free Radic Res 40:1339–1349
Williams R, Lenz EM, Wilson AJ, Granger J, Wilson ID, Major H, Stumpf C, Plumb R (2006) A multi-analytical platform approach to the metabonomic analysis of plasma from normal and Zucker (fa/fa) obese rats. Mol Biosyst 2:174–183
Wolfram R, Oguogho A, Palumbo B, Sinzinger H (2005) Enhanced oxidative stress in coronary heart disease and chronic heart failure as indicated by an increased 8-epi-PGF(2alpha). Eur J Heart Fail 7:167–172
Yan S, Wu B, Lin Z, Jin H, Huang J, Yang Y, Zhang X, Shen Z, Zhang W (2009) Metabonomic characterization of aging and investigation on the anti-aging effects of total flavones of Epimedium. Mol Biosyst 5:1204–1213
Zhu Y, Lin JH, Liao HL, Verna L, Stemerman MB (1997) Activation of ICAM-1 promoter by lysophosphatidylcholine: possible involvement of protein tyrosine kinases. Biochim Biophys Acta 1345:93–98
Zieman SJ, Melenovsky V, Kass DA (2005) Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol 25:932–943
Acknowledgments
We sincerely thank the study subjects for their participation. This study was supported by the National Research Foundation of Korea (M10642120002-06 N4212-27-00210, 2012–0005604, and 2012–0001851), Republic of Korea. All of the authors were involved in the development of the study protocol and the experimental design.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ji Young Kim and Oh Yoen Kim contributed equally to this work.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kim, J.Y., Kim, O.Y., Paik, J.K. et al. Association of age-related changes in circulating intermediary lipid metabolites, inflammatory and oxidative stress markers, and arterial stiffness in middle-aged men. AGE 35, 1507–1519 (2013). https://doi.org/10.1007/s11357-012-9454-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-012-9454-2