Abstract
A growing body of research has identified food insecurity as a barrier to antiretroviral therapy (ART) adherence. We systematically reviewed and summarized the quantitative literature on food insecurity or food assistance and ART adherence. We identified nineteen analyses from eighteen distinct studies examining food insecurity and ART adherence. Of the thirteen studies that presented an adjusted effect estimate for the relationship between food insecurity and ART adherence, nine found a statistically significant association between food insecurity and sub-optimal ART adherence. Four studies examined the association between food assistance and ART adherence, and three found that ART adherence was significantly better among food assistance recipients than non-recipients. Across diverse populations, food insecurity is an important barrier to ART adherence, and food assistance appears to be a promising intervention strategy to improve ART adherence among persons living with HIV. Additional research is needed to determine the effectiveness and cost-effectiveness of food assistance in improving ART adherence and other clinical outcomes among people living with HIV in the era of widespread and long-term treatment.



Similar content being viewed by others
References
Bangsberg DR, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15(9):1181–3.
Maggiolo F, et al. Similar adherence rates favor different virologic outcomes for patients treated with nonnucleoside analogues or protease inhibitors. Clin Infect Dis. 2005;40(1):158–63.
Sungkanuparph S, et al. Rapid CD4 decline after interruption of non-nucleoside reverse transcriptase inhibitor-based antiretroviral therapy in a resource-limited setting. AIDS Res Ther. 2007;4:26.
Kiwuwa-Muyingo S, et al. The impact of first year adherence to antiretroviral therapy on long-term clinical and immunological outcomes in the DART trial in Uganda and Zimbabwe. Trop Med Int Health. 2012;17(5):584–94.
Cohen MS, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
Mills EJ, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. JAMA. 2006;296(6):679–90.
WHO. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. Geneva: WHO; 2013.
Nagata JM, et al. Social determinants, lived experiences, and consequences of household food insecurity among persons living with HIV/AIDS on the shore of Lake Victoria, Kenya. AIDS Care. 2012;24(6):728–36.
Goudge J, Ngoma B. Exploring antiretroviral treatment adherence in an urban setting in South Africa. J Public Health Policy. 2011;32(Suppl 1):S52–64.
Weiser SD, et al. Food insecurity as a barrier to sustained antiretroviral therapy adherence in Uganda. PLoS ONE. 2010;5(4):e10340.
AO F. Rome declaration on world food security. Rome: Food and Agriculture Organization; 1996.
Frega R, et al. Food insecurity in the context of HIV/AIDS: a framework for a new era of programming. Food Nutr Bull. 2010;31(4):S292–312.
Weiser SD, et al. Food insecurity is associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francisco. J Gen Intern Med. 2009;24(1):14–20.
Wang EA, et al. Food insecurity is associated with poor virologic response among HIV-infected patients receiving antiretroviral medications. J Gen Intern Med. 2011;26(9):1012–8.
Weiser SD, et al. Longitudinal assessment of associations between food insecurity, antiretroviral adherence and HIV treatment outcomes in rural Uganda. AIDS. 2014;28(1):115–20.
Weiser SD, et al. Food insecurity and HIV clinical outcomes in a longitudinal study of homeless and marginally housed HIV-infected individuals in San Francisco. AIDS. 2013;27(18):2953–8.
McMahon JH, et al. Repeated assessments of food security predict CD4 change in the setting of antiretroviral therapy. J Acquir Immune Defic Syndr. 2011;58(1):60–3.
Normen L, et al. Food insecurity and hunger are prevalent among HIV-positive individuals in British Columbia, Canada. J Nutr. 2005;135(4):820–5.
Weiser SD, et al. Food insecurity is associated with morbidity and patterns of healthcare utilization among HIV-infected individuals in a resource-poor setting. AIDS. 2012;26(1):67–75.
Weiser SD, et al. The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr. 2009;52(3):342–9.
Weiser SD, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr. 2011;94(6):1729S–39S.
Cantrell RA, et al. A pilot study of food supplementation to improve adherence to antiretroviral therapy among food-insecure adults in Lusaka, Zambia. J Acquir Immune Defic Syndr. 2008;49(2):190–5.
Ivers LC, et al. Food assistance is associated with improved body mass index, food security and attendance at clinic in an HIV program in central Haiti: a prospective observational cohort study. AIDS Res Ther. 2010;7:33.
Sztam KA, Fawzi WW, Duggan C. Macronutrient supplementation and food prices in HIV treatment. J Nutr. 2010;140(1):213S–23S.
Anema A, et al. Availability of nutritional support services in HIV care and treatment sites in sub-Saharan African countries. Public Health Nutr. 2012;15(5):938–47.
Lamb MR, et al. Association of adherence support and outreach services with total attrition, loss to follow-up, and death among ART patients in sub-Saharan Africa. PLoS ONE. 2012;7(6):e38443.
Forrester JE, Sztam KA. Micronutrients in HIV/AIDS: is there evidence to change the WHO 2003 recommendations? Am J Clin Nutr. 2011;94(6):1683S–9S.
Ndekha M, et al. Nutritional status of Malawian adults on antiretroviral therapy 1 year after supplementary feeding in the first 3 months of therapy. Trop Med Int Health. 2009;14(9):1059–63.
Ndekha MJ, et al. Supplementary feeding with either ready-to-use fortified spread or corn-soy blend in wasted adults starting antiretroviral therapy in Malawi: randomised, investigator blinded, controlled trial. BMJ. 2009;338:b1867.
Kabore I, et al. The effect of community-based support services on clinical efficacy and health-related quality of life in HIV/AIDS patients in resource-limited settings in sub-Saharan Africa. AIDS Patient Care STDS. 2010;24(9):581–94.
Franke MF, et al. Improved Retention Associated With Community-Based Accompaniment for Antiretroviral Therapy Delivery in Rural Rwanda. Clin Infect Dis. 2013;56(9):1319–26.
Nyamathi A, et al. Impact of a rural village women (Asha) intervention on adherence to antiretroviral therapy in southern India. Nurs Res. 2012;61(5):353–62.
Talisuna-Alamo S, et al. Socioeconomic support reduces nonretention in a comprehensive, community-based antiretroviral therapy program in Uganda. J Acquir Immune Defic Syndr. 2012;59(4):e52–9.
Biadgilign S, et al. Adherence to highly active antiretroviral therapy and its correlates among HIV infected pediatric patients in Ethiopia. BMC Pediatr. 2008;8:53.
Stroup DF, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
StataCorp. Stata statistical software: Release 12, 2011, StataCorp LP: College Station, TX.
Anema A, et al. High prevalence of food insecurity among HIV-infected individuals receiving HAART in a resource-rich setting. AIDS Care. 2011;23(2):221–30.
Peretti-Watel P, et al. Vulnerability, unsafe sex and non-adherence to HAART: evidence from a large sample of French HIV/AIDS outpatients. Soc Sci Med. 2006;62(10):2420–33.
Young S, et al. A review of the role of food insecurity in adherence to care and treatment among adult and pediatric populations living with HIV and AIDS. AIDS Behav. 2013. doi:10.1007/s10461-013-0547-4.
Kalichman SC, et al. Health and treatment implications of food insufficiency among people living with HIV/AIDS, Atlanta, Georgia. J Urban Health. 2010;87(4):631–41.
Kalichman SC, et al. Food insufficiency and medication adherence among people living with HIV/AIDS in urban and peri-urban settings. Prev Sci. 2011;12(3):324–32.
Boyer S, et al. Non-adherence to antiretroviral treatment and unplanned treatment interruption among people living with HIV/AIDS in Cameroon: individual and healthcare supply-related factors. Soc Sci Med. 2011;72(8):1383–92.
Marcellin F, et al. Determinants of unplanned antiretroviral treatment interruptions among people living with HIV in Yaounde, Cameroon (EVAL survey, ANRS 12-116). Trop Med Int Health. 2008;13(12):1470–8.
Posse M, et al. The effect of food assistance on adherence to antiretroviral therapy among HIV/AIDS patients in Sofala Province, in Mozambique: a retrospective study. J AIDS Clin Res. 2013;4(3):1000198. doi:10.4172/2155-6113.1000198.
Gebo KA, Keruly J, Moore RD. Association of social stress, illicit drug use, and health beliefs with nonadherence to antiretroviral therapy. J Gen Intern Med. 2003;18(2):104–11.
Kalichman SC, Grebler T. Stress and poverty predictors of treatment adherence among people with low-literacy living with HIV/AIDS. Psychosom Med. 2010;72(8):810–6.
Anema A, et al. Relationship between food insecurity and mortality among HIV-positive injection drug users receiving antiretroviral therapy in British Columbia, Canada. PLoS ONE. 2013;8(5):e61277.
Kelly A, et al. Moresby food isn’t good: food security, nutritional information and adherence to antiretroviral therapy in Papua New Guinea. P N G Med J. 2011;54(1–2):23–34.
Van Dyk AC. Treatment adherence following national antiretroviral rollout in South Africa. Ajar-Afr J Aids Res. 2010;9(3):235–47.
Birbeck GL, et al. Neuropsychiatric and socioeconomic status impact antiretroviral adherence and mortality in rural Zambia. Am J Trop Med Hyg. 2011;85(4):782–9.
Franke MF, et al. Food insufficiency is a risk factor for suboptimal antiretroviral therapy adherence among HIV-infected adults in urban Peru. AIDS Behav. 2011;15(7):1483–9.
Sasaki Y, et al. Adherence to antiretroviral therapy (ART) during the early months of treatment in rural Zambia: influence of demographic characteristics and social surroundings of patients. Ann Clin Microbiol Antimicrob. 2012;11:34.
Parashar S, et al. Sticking to it: the effect of maximally assisted therapy on antiretroviral treatment adherence among individuals living with HIV who are unstably housed. AIDS Behav. 2011;15(8):1612–22.
Berhe N, Tegabu D, Alemayehu M. Effect of nutritional factors on adherence to antiretroviral therapy among HIV-infected adults: a case control study in Northern Ethiopia. BMC Infect Dis. 2013;13:233.
Sterne JAC, Harbord RM. Funnel plots in meta-analysis. Stata J. 2004;4(2):127–41.
Tirivayi N, Koethe JR, Groot W. Clinic-based food assistance is associated with increased medication adherence among HIV-infected adults on long-term antiretroviral therapy in Zambia. J AIDS Clin Res. 2012;3(7):171.
Serrano C, et al. Family nutritional support improves survival, immune restoration and adherence in HIV patients receiving ART in developing country. Asia Pac J Clin Nutr. 2010;19(1):68–75.
Chesney MA. Factors affecting adherence to antiretroviral therapy. Clin Infect Dis. 2000;30(Suppl 2):S171–6.
Spire B, et al. Adherence to highly active antiretroviral therapies (HAART) in HIV-infected patients: from a predictive to a dynamic approach. Soc Sci Med. 2002;54(10):1481–96.
Gutierrez EB, et al. Measuring adherence to antiretroviral treatment: the role of pharmacy records of drug withdrawals. AIDS Behav. 2012;16(6):1482–90.
Palar K, et al. Role of antiretroviral therapy in improving food security among patients initiating HIV treatment and care. AIDS. 2012;26(18):2375–81.
Weiser SD, et al. Changes in food insecurity, nutritional status, and physical health status after antiretroviral therapy initiation in rural Uganda. J Acquir Immune Defic Syndr. 2012;61(2):179–86.
McCoy SI, et al. Food insecurity, socioeconomic status, and HIV-related risk behavior among women in farming households in Tanzania. AIDS Behav. 2014;18(7):1224–36.
Riley ED, et al. Basic subsistence needs and overall health among human immunodeficiency virus-infected homeless and unstably housed women. Am J Epidemiol. 2011;174(5):515–22.
Mugavero MJ, Norton WE, Saag MS. Health care system and policy factors influencing engagement in HIV medical care: piecing together the fragments of a fractured health care delivery system. Clin Infect Dis. 2011;52(Suppl 2):S238–46.
McNairy ML, El-Sadr WM. The HIV care continuum: no partial credit given. AIDS. 2012;26(14):1735–8.
de Pee S, et al. Antiretroviral therapy requires life-long adherence. Lancet Infect Dis. 2012; 12(9):661–662; author reply 662.
Galarraga O, et al. Conditional economic incentives to improve HIV treatment adherence: literature review and theoretical considerations. AIDS Behav. 2013;17(7):2283–92.
McCoy SI. Comparing food and cash assistance for HIV-positive men and women on antiretroviral therapy in Tanzania. 2013 [cited 2014 06/07/2014].
Barnighausen T, et al. Interventions to increase antiretroviral adherence in sub-Saharan Africa: a systematic review of evaluation studies. Lancet Infect Dis. 2011;11(12):942–51.
Grobler L, et al. Nutritional interventions for reducing morbidity and mortality in people with HIV. Cochrane Database Syst Rev. 2013;2:CD004536.
Tirivayi N, Groot W. Health and welfare effects of integrating AIDS treatment with food assistance in resource constrained settings: a systematic review of theory and evidence. Soc Sci Med. 2011;73(5):685–92.
Koethe JR, et al. Macronutrient supplementation for malnourished HIV-infected adults: a review of the evidence in resource-adequate and resource-constrained settings. Clin Infect Dis. 2009;49(5):787–98.
Acknowledgments
Ms. Singer acknowledges support from NIEHS R01 ES09137. Dr. McCoy is supported by Award Number K01MH094246 from the National Institute of Mental Health. Dr. Weiser acknowledges support from the Burke Global Health Family Foundation, and NIMH K23 MH079713. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health, the National Institute of Environmental Health Sciences, or the National Institutes of Health. The funding bodies had no role in the study. We thank Dr. Nancy Padian for helpful comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
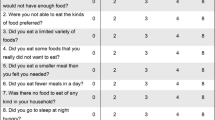
Appendix
Appendix
Full PubMed Search strategy: (“Antiretroviral Therapy, Highly Active”[Mesh] OR “HIV Infections/drug therapy”[Mesh] OR “Anti-HIV Agents/therapeutic use”[Mesh] OR “Acquired Immunodeficiency Syndrome/drug therapy”[Mesh] OR antiretroviral OR HAART OR ART) AND (“Patient Compliance”[Mesh] OR “Medication adherence”[Mesh] OR adherence OR nonadherence OR non-adherence) AND (“Food Supply”[Mesh] OR food OR hunger OR “Socioeconomic factors”[Mesh] OR “risk factors” OR poverty OR barrier OR nutrition OR malnutrition).
Rights and permissions
About this article
Cite this article
Singer, A.W., Weiser, S.D. & McCoy, S.I. Does Food Insecurity Undermine Adherence to Antiretroviral Therapy? A Systematic Review. AIDS Behav 19, 1510–1526 (2015). https://doi.org/10.1007/s10461-014-0873-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-014-0873-1