Abstract
Food insecurity disproportionately affects people with HIV and women in the United States (US). More evidence is needed to understand the interplay between levels of food insecurity and levels of antiretroviral therapy (ART) adherence over time, as well as how food insecurity relates to engagement in HIV care. We used random effects models with longitudinal data from the US Women’s Interagency HIV Study to estimate the (1) adjusted associations of current and 6-month lagged food security with ART adherence categories (n = 1646), and (2) adjusted associations of food security with engagement-in-care (n = 1733). Very low food security was associated with a higher relative risk of ART non-adherence at prior and current visits compared with food security, and this association increased across non-adherence categories. Very low food security was associated with lower odds of receiving HIV care and higher odds of a missed visit. Food insecurity among US women with HIV is associated with poorer engagement in care and degree of ART non-adherence over time.
Similar content being viewed by others
Data availability
Access to individual-level data from the MACS/WIHS Combined Cohort Study Data (MWCCS) may be obtained upon review and approval of a MWCCS concept sheet. Links and instructions for online concept sheet submission are on the study website: https://statepi.jhsph.edu/mwccs/work-with-us/
Code Availability
Stata 14 (Stata Corp., College Station, TX, USA) was used for all analyses. Study code has been shared with the main MACS/WIHS Combined Cohort Study Data Center. We are willing to share our study code upon request.
References
Giordano TP, Gifford AL, White AC Jr, Suarez-Almazor ME, Rabeneck L, Hartman C, et al. Retention in care: a challenge to survival with HIV infection. Clin Infect Dis. 2007;44(11):1493–9.
Press N, Tyndall MW, Wood E, Hogg RS, Montaner JS. Virologic and immunologic response, clinical progression, and highly active antiretroviral therapy adherence. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S112–7.
Bangsberg D, Perry S, Charlebois E, Clark R, Roberston M, Zolopa A, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15(9):1181.
Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372(9635):293–9.
Walensky RP, Paltiel AD, Losina E, Mercincavage LM, Schackman BR, Sax PE, et al. The survival benefits of AIDS treatment in the United States. J Infect Dis. 2006;194(1):11–9.
Anglemyer A, Rutherford GW, Horvath T, Baggaley RC, Egger M, Siegfried N. Antiretroviral therapy for prevention of HIV transmission in HIV-discordant couples. Cochrane Database Syst Rev. 2013;4:9153.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
Cunningham W, Mosen DM, Morales LS, Andersen RM, Shapiro MF, Hays RD. Ethnic and racial differences in long-term survival from hospitalization for HIV infection. J Health Care Poor Underserved. 2000;11(2):163–78.
Cunningham W. HIV racial disparities: time to close the gaps. Arch Intern Med. 2012;172(20):1599–600.
Simard EP, Fransua M, Naishadham D, Jemal A. The influence of sex, race/ethnicity, and educational attainment on human immunodeficiency virus death rates among adults, 1993–2007. Arch Intern Med. 2012;172(20):1591–8.
Life Sciences Research Office (LSRO), Anderson Se. Core indicators of nutritional state for difficult-to-sample populations. J Nutr. 1990;120(Suppl 11):1559–600.
Marcellin F, Boyer S, Protopopescu C, Dia A, Ongolo-Zogo P, Koulla-Shiro S, et al. Determinants of unplanned antiretroviral treatment interruptions among people living with HIV in Yaounde, Cameroon (EVAL survey, ANRS 12–116). Trop Med Int Health. 2008;13(12):1470–8.
Weiser S, Tsai AC, Gupta R, Frongillo EA, Kawuma A, Senkugu J, et al. Food insecurity is associated with morbidity and patterns of healthcare utilization among HIV-infected individuals in rural Uganda. AIDS (London, England). 2012;26(1):67–75.
Franke MF, Murray MB, Munoz M, Hernandez-Diaz S, Sebastian JL, Atwood S, et al. Food insufficiency is a risk factor for suboptimal antiretroviral therapy adherence among HIV-infected adults in urban Peru. AIDS Behav. 2011;15(7):1483–9.
Weiser SD, Tuller DM, Frongillo EA, Senkungu J, Mukiibi N, Bangsberg DR. Food insecurity as a barrier to sustained antiretroviral therapy adherence in Uganda. PLoS ONE. 2010;5(4): e10340.
Coleman-Jensen A, Rabbitt M, Gregory C, Singh A. Household food security in the United States in 2016. ERR 237. United States Department of Agriculture, Economic Research Service; 2017.
Kalichman SC, Cherry C, Amaral C, White D, Kalichman MO, Pope H, et al. Health and treatment implications of food insufficiency among people living with HIV/AIDS, Atlanta, Georgia. J Urban Health. 2010;87(4):631–41.
Normen L, Chan K, Braitstein P, Anema A, Bondy G, Montaner JS, et al. Food insecurity and hunger are prevalent among HIV-positive individuals in British Columbia, Canada. J Nutr. 2005;135(4):820–5.
Pellowski JA, Kalichman SC, Cherry S, Conway-Washington C, Cherry C, Grebler T, et al. The daily relationship between aspects of food insecurity and medication adherence among people living with HIV with recent experiences of hunger. Ann Behav Med. 2016;50(6):844–53.
Chen Y, Kalichman SC. Synergistic effects of food insecurity and drug use on medication adherence among people living with HIV infection. J Behav Med. 2015;38(3):397–406.
Peretti-Watel P, Spire B, Schiltz MA, Bouhnik AD, Heard I, Lert F, et al. Vulnerability, unsafe sex and non-adherence to HAART: evidence from a large sample of French HIV/AIDS outpatients. Soc Sci Med. 2006;62(10):2420–33.
Gebo KA, Keruly J, Moore RD. Association of social stress, illicit drug use, and health beliefs with nonadherence to antiretroviral therapy. J Gen Intern Med. 2003;18(2):104–11.
Weiser SD, Yuan C, Guzman D, Frongillo EA, Riley ED, Bangsberg DR, et al. Food insecurity and HIV clinical outcomes in a longitudinal study of homeless and marginally housed HIV-infected individuals in San Francisco. AIDS. 2013;27(18):2953–8.
Summers NA, Colasanti JA, Feaster DJ, Armstrong WS, Rodriguez A, Jain MK, et al. Predictors for poor linkage to care among hospitalized persons living with HIV and co-occurring substance use disorder. AIDS Res Hum Retroviruses. 2020;36(5):406–14.
Colasanti J, Stahl N, Farber EW, Del Rio C, Armstrong WS. An exploratory study to assess individual and structural level barriers associated with poor retention and re-engagement in care among persons living With HIV/AIDS. J Acquir Immune Defic Syndr. 2017;74:S113–20.
Wawrzyniak AJ, Rodríguez AE, Falcon AE, Chakrabarti A, Parra A, Park J, et al. Association of individual and systemic barriers to optimal medical care in people living with HIV/AIDS in Miami-Dade County. J Acquir Immune Defic Syndr. 2015;69:S63-72.
Boyer S, Clerc I, Bonono CR, Marcellin F, Bile PC, Ventelou B. Non-adherence to antiretroviral treatment and unplanned treatment interruption among people living with HIV/AIDS in Cameroon: individual and healthcare supply-related factors. Soc Sci Med. 2011;72(8):1383–92.
Sasaki Y, Kakimoto K, Dube C, Sikazwe I, Moyo C, Syakantu G, et al. Adherence to antiretroviral therapy (ART) during the early months of treatment in rural Zambia: influence of demographic characteristics and social surroundings of patients. Ann Clin Microbiol Antimicrob. 2012;11:34.
Weiser SD, Palar K, Frongillo EA, Tsai AC, Kumbakumba E, Depee S, et al. Longitudinal assessment of associations between food insecurity, antiretroviral adherence and HIV treatment outcomes in rural Uganda. AIDS. 2014;28(1):115–20.
Benzekri NA, Sambou JF, Ndong S, Diallo MB, Tamba IT, Faye D, et al. Food insecurity predicts loss to follow-up among people living with HIV in Senegal, West Africa. AIDS Care. 2022;34(7):878–86.
Benzekri NA, Sambou JF, Ndong S, Diallo MB, Tamba IT, Faye D, et al. The impact of food insecurity on HIV outcomes in Senegal, West Africa: a prospective longitudinal study. BMC Public Health. 2021;21(1):451.
Weiser SD, Tsai AC, Gupta R, Frongillo EA, Kawuma A, Senkungu J, et al. Food insecurity is associated with morbidity and patterns of healthcare utilization among HIV-infected individuals in a resource-poor setting. AIDS. 2012;26(1):67–75.
Young S, Wheeler AC, McCoy SI, Weiser SD. A review of the role of food insecurity in adherence to care and treatment among adult and pediatric populations living with HIV and AIDS. AIDS Behav. 2014;18:S505–15.
Weiser S, Hatcher A, Frongillo EA, Guzman D, Riley ED, Bangsberg DR, et al. Food insecurity is associated with greater acute care utilization among HIV-infected homeless and marginally housed individuals in San Francisco. J Gen Intern Med. 2012;28(1):91–8.
Dandachi D, May SB, Davila JA, Cully J, Amico KR, Kallen MA, et al. The association of unmet needs with subsequent retention in care and HIV suppression among hospitalized patients with HIV who are out of care. J Acquir Immune Defic Syndr. 2019;80(1):64–72.
D’Souza G, Bhondoekhan F, Benning L, Margolick JB, Adedimeji AA, Adimora AA, et al. Characteristics of the MACS/WIHS combined cohort study: opportunities for research on aging with HIV in the longest US observational study of HIV. Am J Epidemiol. 2021;190(8):1457–75.
Barkan SE, Melnick SL, Preston-Martin S, Weber K, Kalish LA, Miotti P, et al. The women’s interagency HIV study WIHS Collaborative Study Group. Epidemiology. 1998;9(2):117–25.
Adimora AA, Ramirez C, Benning L, Greenblatt RM, Kempf M-C, Tien PC, et al. Cohort profile: the Women’s Interagency HIV Study (WIHS). Int J Epidemiol. 2018;47(2):393–4.
Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, Frick PA. Self-report measures of antiretroviral therapy adherence: a review with recommendations for HIV research and clinical management. AIDS Behav. 2006;10(3):227–45.
Feldman BJ, Fredericksen RJ, Crane PK, Safren SA, Mugavero MJ, Willig JH, et al. Evaluation of the single-item self-rating adherence scale for use in routine clinical care of people living with HIV. AIDS Behav. 2013;17(1):307–18.
Genberg BL, Wilson IB, Bangsberg DR, Arnsten J, Goggin K, Remien RH, et al. Patterns of antiretroviral therapy adherence and impact on HIV RNA among patients in North America. AIDS. 2012;26(11):1415–23.
Gifford AL, Groessl EJ. Chronic disease self-management and adherence to HIV medications. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S163–6.
Marshall R, Beach MC, Saha S, Mori T, Loveless MO, Hibbard JH, et al. Patient activation and improved outcomes in HIV-infected patients. J Gen Intern Med. 2013;28(5):668–74.
Gifford AL, Groessl EJ. Chronic disease self-management and adherence to HIV medications. J Acquir Immune Defic Syndr. 1999;2002(31):S163–6.
Frongillo EA Jr. Validation of measures of food insecurity and hunger. J Nutr. 1999;129(2S Suppl):506S-S509.
Radimer KL, Olson CM, Greene JC, Campbell CC, Habicht JP. Understanding hunger and developing indicators to assess it in women and children. J Nutr Educ. 1992;24(1 suppl.):36S-44S.
Hamelin AM, Beaudry M, Habicht JP. Characterization of household food insecurity in Quebec: food and feelings. Soc Sci Med. 2002;54(1):119–32.
Ganann R, Fitzpatrick-Lewis D, Ciliska D, Peirson LJ, Warren RL, Fieldhouse P, et al. Enhancing nutritional environments through access to fruit and vegetables in schools and homes among children and youth: a systematic review. BMC Res Notes. 2014;7:422.
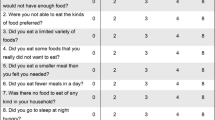
Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to measuring household food security, revised 2000. Alexandria, VA: Food and Nutrition Service, U.S. Department of Agriculture; 2000.
National Institute on Alcohol Abuse Alcoholism. The physicians’ guide to helping patients with alcohol problems: US Department of Health and Human Services. National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism: Public Health Service; 1995.
Abuse NIoA, Alcoholism. The physicians' guide to helping patients with alcohol problems: US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism; 1995.
UCLA: Statistical Consulting Group. Multinomial logistic regression. Stata annotated output. (accessed January 31, 2023) https://stats.oarc.ucla.edu/stata/output/multinomial-logistic-regression/.
Vittinghoff E, Glidden DV, Shiboski SC, McCulloch CE. Regression methods in biostatistics: linear, logistic, survival, and repeated measures models. 2nd ed. New York: Springer; 2006.
Ender P. Applied Categorical & Nonnormal Data Analysis: Multinomial Logistic Regression Models). http://www.philender.com/courses/categorical/notes3/mlogit1.html. accessed 31 Jan 2023
Tan JY, Sheira LA, Frongillo EA, Gustafson D, Sharma A, Merenstein D, et al. Food insecurity and frailty among women with and without HIV in the United States: a cross-sectional analysis. J Int AIDS Soc. 2021;24(6): e25751.
Whittle HJ, Palar K, Seligman HK, Napoles T, Frongillo EA, Weiser SD. How food insecurity contributes to poor HIV health outcomes: Qualitative evidence from the San Francisco Bay Area. Soc Sci Med. 2016;170:228–36.
Weiser S, Tuller D, Frongillo E, Senkungu J, Mukiibi N, Bangsberg D, et al. Food Insecurity as a barrier to sustained antiretroviral therapy adherence in Uganda. PLoS ONE. 2010;5(4):357–66.
Cunningham W, Andersen RM, Katz MH, Stein MD, Turner BJ, Crystal S, et al. The impact of competing subsistence needs and barriers on access to medical care for persons with human immunodeficiency virus receiving care in the United States. Med Care. 1999;37(12):1270–81.
Whitaker RC, Phillips SM, Orzol SM. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. 2006;118(3):e859–68.
Palar K, Kushel M, Frongillo EA, Riley ED, Grede N, Bangsberg D, et al. Food insecurity is longitudinally associated with depressive symptoms among homeless and marginally-housed individuals living with HIV. AIDS Behav. 2015;19(8):1527–34.
Montgomery BE, Rompalo A, Hughes J, Wang J, Haley D, Soto-Torres L, et al. Violence against women in selected areas of the United States. Am J Public Health. 2015;105(10):2156–66.
Gonzalez JS, Batchelder AW, Psaros C, Safren SA. Depression and HIV/AIDS treatment nonadherence: a review and meta-analysis. J Acquir Immune Defic Syndr. 2011;58(2):181–7.
Weiser SD, Frongillo EA, Ragland K, Hogg RS, Riley ED, Bangsberg DR. Food insecurity is associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francisco. J Gen Intern Med. 2009;24(1):14–20.
Kalichman SC, Grebler T. Stress and poverty predictors of treatment adherence among people with low-literacy living with HIV/AIDS. Psychosom Med. 2010;72(8):810.
Genberg BL, Wilson IB, Bangsberg DR, Arnsten J, Goggin K, Remien RH, et al. Patterns of antiretroviral therapy adherence and impact on HIV RNA among patients in North America. AIDS (London, England). 2012;26(11):1415.
Kalichman SC, Kalichman MO, Cherry C. Forget about forgetting: structural barriers and severe non-adherence to antiretroviral therapy. AIDS Care. 2017;29(4):418–22.
Kobin AB, Sheth NU. Levels of adherence required for virologic suppression among newer antiretroviral medications. Ann Pharmacother. 2011;45(3):372–9.
Feldman MB, Alexy ER, Thomas JA, Gambone GF, Irvine MK. The association between food insufficiency and HIV treatment outcomes in a longitudinal analysis of HIV-infected individuals in New York City. J Acquir Immune Defic Syndr. 2015;69(3):329–37.
Palar K, Napoles T, Hufstedler LL, Seligman H, Hecht FM, Madsen K, et al. Comprehensive and medically appropriate food support is associated with improved HIV and diabetes health. J Urban Health. 2017;94(1):87–99.
McKay FH, Lippi K, Dunn M. Investigating responses to food insecurity among HIV positive people in resource rich settings: a systematic review. J Commun Health. 2017;42(5):1062–8.
Acknowledgements
The authors gratefully acknowledge the contributions of the study participants and dedication of the staff at the MWCCS sites.
Funding
Data in this manuscript were collected by the Women’s Interagency HIV Study (WIHS), now the MACS/WIHS Combined Cohort Study (MWCCS), and funded by a grant from the National Institute of Mental Health, R01MH095683 (Weiser). Additional salary support was provided by K01DK107335 (Palar). The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH). MWCCS (Principal Investigators): Atlanta CRS (Ighovwerha Ofotokun, Anandi Sheth, and Gina Wingood), U01-HL146241; Baltimore CRS (Todd Brown and Joseph Margolick), U01-HL146201; Bronx CRS (Kathryn Anastos, David Hanna, and Anjali Sharma), U01-HL146204; Brooklyn CRS (Deborah Gustafson and Tracey Wilson), U01-HL146202; Data Analysis and Coordination Center (Gypsyamber D’Souza, Stephen Gange and Elizabeth Topper), U01-HL146193; Chicago-Cook County CRS (Mardge Cohen and Audrey French), U01-HL146245; Chicago-Northwestern CRS (Steven Wolinsky), U01-HL146240; Northern California CRS (Bradley Aouizerat, Jennifer Price, and Phyllis Tien), U01-HL146242; Los Angeles CRS (Roger Detels and Matthew Mimiaga), U01-HL146333; Metropolitan Washington CRS (Seble Kassaye and Daniel Merenstein), U01-HL146205; Miami CRS (Maria Alcaide, Margaret Fischl, and Deborah Jones), U01-HL146203; Pittsburgh CRS (Jeremy Martinson and Charles Rinaldo), U01-HL146208; UAB-MS CRS (Mirjam-Colette Kempf, Jodie Dionne-Odom, and Deborah Konkle-Parker), U01-HL146192; UNC CRS (Adaora Adimora and Michelle Floris-Moore), U01-HL146194. The MWCCS is funded primarily by the National Heart, Lung, and Blood Institute (NHLBI), with additional co-funding from the Eunice Kennedy Shriver National Institute Of Child Health & Human Development (NICHD), National Institute On Aging (NIA), National Institute Of Dental & Craniofacial Research (NIDCR), National Institute Of Allergy And Infectious Diseases (NIAID), National Institute Of Neurological Disorders And Stroke (NINDS), National Institute Of Mental Health (NIMH), National Institute On Drug Abuse (NIDA), National Institute Of Nursing Research (NINR), National Cancer Institute (NCI), National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Institute on Deafness and Other Communication Disorders (NIDCD), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute on Minority Health and Health Disparities (NIMHD), and in coordination and alignment with the research priorities of the National Institutes of Health, Office of AIDS Research (OAR). MWCCS data collection is also supported by UL1-TR000004 (UCSF CTSA), UL1-TR003098 (JHU ICTR), UL1-TR001881 (UCLA CTSI), P30-AI-050409 (Atlanta CFAR), P30-AI-073961 (Miami CFAR), P30-AI-050410 (UNC CFAR), P30-AI-027767 (UAB CFAR), P30-MH-116867 (Miami CHARM), UL1-TR001409 (DC CTSA), KL2-TR001432 (DC CTSA), and TL1-TR001431 (DC CTSA).
Author information
Authors and Affiliations
Contributions
SDW, KP, PT, MK and EAF conceived of the work. SDW, KP, EAF, LS and KP designed the work. KP wrote the manuscript. TEW, AC, AA, DM, MHC, ELW, AAA, IO, LM, JMT, and PCT contributed to acquisition of the data. LAS and EAF performed statistical analyses. SDW, LAS, EAF, TEW, AC, AA, DM, MHC, ELW, AAA, IO, LM, JMT, and PCT contributed to the interpretation of data for the work and made critical revisions to the work for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical Approval
This study was approved by the Institutional Review Board at each study site’s institution and by the WIHS Executive Committee.
Consent to Participate
Written informed consent was obtained for all participants in the study.
Consent for Publication
Written informed consent obtained for the study included publication of the results, with the assurance that no individually identifiable data would be included in publications.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Palar, K., Sheira, L.A., Frongillo, E.A. et al. Longitudinal Relationship Between Food Insecurity, Engagement in Care, and ART Adherence Among US Women Living with HIV. AIDS Behav 27, 3345–3355 (2023). https://doi.org/10.1007/s10461-023-04053-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-023-04053-9