Abstract
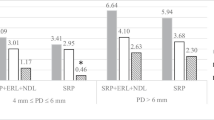
The purpose of this study was to evaluate the influence of an erbium, chromium:yttrium–scandium–gallium–garnet (Er,Cr:YSGG) laser in the absence or presence of manual scaling and root planning (SRP) for the treatment of induced periodontitis in rats. Ligatures were placed in the subgingival region of the maxillary first molar. After a 7-day period, the ligatures were removed, and 40 rats were randomly divided into four groups (G), as follows: (GI) no treatment, (GII) scaling and root planning (SRP) with curettes, (GIII) Er,Cr:YSGG laser irradiation and (GIV) SRP with curettes followed by Er,Cr:YSGG laser irradiation. Seven and 30 days after the treatment, the animals were sacrificed and histologic, histometric and immunohistochemistry analyses were performed. All groups showed similar histopathological characteristics during the evaluation period. The histometric analysis was confirmed using Bonferroni and paired t tests. At 7 and 30 days, groups II, III and IV exhibited greater bone formation in the furcation area when compared to group I (p < 0.0001; p < 0.05). During the 7-day period, the groups irradiated with the laser (III and IV) showed a statistically larger new bone area than the group treated with SRP (II) (p < 0.01). Immunohistochemistry analysis revealed that the control group exhibited a higher expression of tartrate-resistant acid phosphatase (TRAP) and the receptor activator of nuclear factor κΒ ligand (RANKL) when compared to groups II, III and IV (p < 0.05). All treatments were able to reduce the inflammatory processes, consequently enabling the repair of periodontal tissues. The results achieved with the application of the Er,Cr:YSGG laser suggest that this laser can stimulate greater bone formation, especially over a shorter period of time.


Similar content being viewed by others
References
Tatakis D, Kumar P (2005) Etiology and pathogenesis of periodontal diseases. Dent Clin N Am 49:491–516
Flemmig TF, Beikler T (2011) Control of oral biofilms. Periodontol 55:9–15
Fernandes LA, de Almeida JM, Theodoro LH et al (2009) Treatment of experimental periodontal disease by photodynamic therapy in immunosuppressed rats. J Clin Periodontol 36:219–228
Eberhard J, Ehlers H, Falk W, Acil Y, Albers HK, Jepsen S (2003) Efficacy of subgingival calculus removal with Er:YAG laser compared to mechanical debridement: an in situ study. J Clin Periodontol 30:511–518
van As G (2004) Erbium lasers in dentistry. Dent Clin N Am 48:1017–1059
Hakki SS, Berk G, Dundar N, Saglam M, Berk N (2010) Effects of root planing procedures with hand instrument or erbium, chromium: yttrium–scandium–gallium–garnet laser irradiation on the root surfaces: a comparative scanning electron microscopy study. Lasers Med Sci 25:345–353
Eversole LR, Rizoiu IM (1995) Preliminary investigations on the utility of an erbium, chromium YSGG laser. J Calif Dent Assoc 23:41–47
Tachibana A, Marques MM, Soler JM, Matos AB (2008) Erbium, chromium:yttrium scandium gallium garnet laser for caries removal: influence on bonding of a self-etching adhesive system. Lasers Med Sci 23:435–441
De Freitas PM, Rapozo-Hillo M, Eduardo CDP, Featherstone JDB (2008) In vitro evaluation of erbium, chromium: yttrium–scandium–gallium–garnet laser-treated enamel demineralization. Lasers Med Sci 23:1–6
Gholami GA, Fekrazad R, Esmaiel-Nejad A, Kalhori KAM (2011) An evaluation of the occluding effects of Er,Cr:YSGG, Nd:YAG, CO2 and diode lasers on dentinal tubules: a scanning electron microscope in vitro study. Photomed Laser Surg 29:115–121
Perussi LR, Pavone C, de Oliveira GJPL, Cerri PS, Marcantonio RAC (2012) Effects of the Er,Cr:YSGG laser on bone and soft tissue in a rat model. Lasers Med Sci 27:95–102
Cesar-Neto JB, Benatti BB, Sallum EA, Casati MZ, Nociti FH Jr (2006) The influence of cigarette smoke inhalation and its cessation on the tooth-supporting alveolar bone: a histometric study in rats. J Periodontol Res 41:118–123
Cerri PS, Pereira-Junior JA, Biselli NB, Sasso-Cerri E (2010) Mast cells and MMP-9 in the lamina propria during eruption of rat molars: quantitative and immunohistochemical evaluation. J Anat 217:116–125
Mizutani K, Aoki A, Takasaki AA et al (2006) Periodontal tissue healing following flap surgery using an Er: YAG laser in dogs. Lasers Surg Med 38:314–324
Pourzarandian A, Watanabe H, Aoki A, Ichinose S, Sasaki KM, Nitta H, Ishikawa I (2004) Histological and TEM examination of early stages of bone healing after Er: YAG laser irradiation. Photomed Laser Surg 22:342–350
Ozawa Y, Shimizu N, Kariya G, Abiko Y (1998) Low-energy laser irradiation stimulates bone nodule formation at early stages of cell in rat calvarial cells. Bone 22:347–354
Lee HJ, Heo JS, Koak YJ, Kim KS, Lee JS, Lee HS (2008) Cellular response on anodized titanium discs after laser irradiation. Lasers Surg Med 40:738–742
Harashima T, Kinoshita J, Kimura Y et al (2005) Morphological comparative study on ablation of dental hard tissues at cavity preparation by Er:YAG and Er,Cr:YSGG lasers. Photomed Laser Surg 23:52–55
Hossain M, Nakamura Y, Yamada Y, Suzuki N, Murakami Y, Matsumoto K (2001) Analysis of surface roughness of enamel and dentin after Er,Cr:YSGG laser irradiation. J Clin Laser Med Surg 19:297–303
Yu G, Kimura Y, Kinoshita J, Matsumoto K (2000) Morphological and atomic analytical studies on enamel and dentin irradiated by an erbium, chromium: YSGG laser. J Clin Laser Med Surg 18:139–143
Hakki SS, Korkusuz P, Berk G et al (2010) Comparison of Er,Cr:YSGG laser and hand instrumentation on the attachment of periodontal ligament fibroblasts to periodontally diseased root surfaces: an in vitro study. J Periodontol 81:1216–1225
Oliveira GJLP, Pavone C, Sampaio JEC, Marcantonio RAC (2010) Influence of the angle of irradiation of the Er,Cr:YSGG laser on the morphology, attachment of blood components, roughness and root wear: in vitro study. Lasers Surg Med 42:683–691
Ting CC, Fukuda M, Watanabe T, Aoki T, Sanaoka A, Noguchi T (2007) Effects of Er,Cr:YSGG laser irradiation on the root surface: morphologic analysis and efficiency of calculus removal. J Periodontol 78:2156–2164
Ekworapoj P, Sidhu SK, McCabe JF (2007) Effect of different power parameters of Er–Cr:YSGG on human dentine (2007). Lasers Med Sci 22:175–182
Sperandio FF, Meneguzzo DT, Ferreira LS, Ana PA, Azevedo LH, Sousa S (2011) Different air-water spray regulations affect the healing of Er,Cr:YSGG laser incisions. Lasers Med Sci 26:257–265
Olivi G, Angiero F, Benedicenti S, Iaria G, Signore A, Kaitsas V (2010) Use of the erbium, chromium:yttrium–scandium–gallium–garnet laser on human enamel tissues. Influence of air–water spray on the laser–tissue interaction: scanning electron microscope evaluations. Lasers Med Sci 25:793–797
Meister J, Franzen R, Forner K, Grebe H (2006) Influence of the water content in dental enamel and dentin on ablation with erbium YAG and erbium YSGG lasers. J Biomed Opt 11:34030
Arnabat J, Escribano C, Fenosa A et al (2010) Bactericidal activity of erbium chromium: yttrium scandium gallium–garnet laser in root canals. Lasers Med Sci 25:805–810
Franzen R, Oliveira ME, Meister J et al (2009) Decontamination of deep dentin by means of erbium, chromium: yttrium–scandium–gallium–garnet laser irradiation. Lasers Med Sci 24:75–80
Yavari HR, Rahimi S, Shani S et al (2010) Effect of Er,Cr:YSGG laser irradiation on Enterococcus faecalis in infected root canals. Photomed Laser Surg 28:91–96
Fontana CR, Kurachi C, Mendonca CR, Bagnato VS (2004) Microbial reduction in periodontal pockets under exposition of a medium power diode laser: an experimental study in rats. Lasers Surg Med 35:263–268
Akiyama F, Aoki A, Uchiyama MM et al (2011) In vitro studies of the ablation mechanism on periodontopathic bacteria and decontamination effect on periodontally diseased root surfaces by erbium:yttrium–aluminum–garnet laser. Lasers Med Sci 26:193–204
Xu M, Deng T, Mo F et al (2009) Low-intensity pulsed laser irradiation affects RANKL and OPG mRNA expression in rat calvarial cells. Photomed Laser Surg 27:309–315
Kimura R, Anan H, Matsumoto A, Noda D, Maeda K (2003) Dental root resorption and repair: histology and histometry during physiological drift of rat molars. J Periodontal Res 38:525–532
Ninomiya T, Hosoya A, Nakamura H, Sano K, Nishisaka T, Ozawa H (2007) Increase of bone volume by a nanosecond pulsed laser irradiation is caused by a decreased osteoclast number and an activated osteoblasts. Bone 40:140–148
Kelbauskiene S, Baseviciene N, Goharkhay K, Moritz A, Machiulskiene V (2011) One-year clinical results of Er,Cr:YSGG laser application in addition to scaling and root planning in patients with early to moderate periodontitis. Lasers Med Sci 26:445–452
Qadri T, Javed F, Poddani P, Tuner J, Gustafsson A (2011) Long-term effects of a single application of water-cooling pulsed Nd:YAG laser in supplement to scaling and root planning in patients with periodontal inflammation. Lasers Med Sci 26:763–766
Euzebio VTA, de Andrade AK, Toaliar JM et al (2013) Clinical and microbiologial evaluation of high intensity diode laser adjutant to non-surgical periodontal treatment: a 6-month clinical trial. Clin Oral Investig 17:87–95
Rotundo R, Nieri M, Cairo F et al (2010) Lack of adjunctive benefit of Er:YAG laser in non-surgical treatment: a randomized split mouth clinical trial. J Clin Periodontol 37:526–533
Acknowledgement
This study was financially supported by the São Paulo Research Foundation (FAPESP—process number 2009/00479-9, São Paulo, Brazil), the Coordination for the Improvement of Higher Educated Personnel (CAPES, Brasilia, DF, Brazil) and the National Council for Scientific and Technological Development (CNPq, Brasilia, DF, Brazil).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pavone, C., Perussi, L.R., de Oliveira, G.J.P.L. et al. Effect of Er,Cr:YSGG laser application in the treatment of experimental periodontitis. Lasers Med Sci 30, 993–999 (2015). https://doi.org/10.1007/s10103-014-1526-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-014-1526-3