Abstract
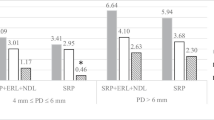
In 30 patients with periodontitis, a total of 278 teeth exhibiting bleeding on probing, subgingival calculus, and a probing depth between 3–6 mm were examined. For each participant, two treatment types were alternatively applied on the contralateral quadrants: scaling and root planing (SRP) as control, and SRP followed by Er,Cr:YSGG laser application (SRP+laser), as a test method. Five clinical parameters: plaque level, bleeding on probing, probing depth, gingival recession and clinical attachment level were examined at baseline and at 2, 3, 6, 12 months after treatment. Of the total of 1,668 sites examined in all patients, 1,088 sites were found with a probing depth of 3–6 mm. In these sites, differences in clinical parameters between SRP and SRP+laser-treated quadrants were analyzed, assuming the level of p < 0.05 as significant. After 2 months from baseline, the mean probing depth reduction and the clinical attachment level gain were significantly greater in SRP+laser than in SRP quadrants, and remained so throughout the study (p < 0.001). A marked reduction of the bleeding scores occurred in all examined sites, irrespective of the treatment method. However, after 12 months, significantly less teeth exhibited bleeding on probing in SRP+laser quadrants than in SRP quadrants (p < 0.001). The mean plaque and gingival recession levels did not differ between the SRP and SRP+laser quadrants neither before nor after the treatment. The periodontal procedures either using Er,Cr:YSGG laser after SRP or SRP alone, lead to significant improvements in all clinical parameters investigated. However, laser application, as an adjunct to SRP, appeared to be more advantageous.




Similar content being viewed by others
References
O’Leary TJ (1986) The impact of research on scaling and root planing. J Periodontol 57(2):69–75
Kepic TJ, O’Leary TJ, Kafrawy AH (1986) Total calculus removal: an attainable objective? J Periodontol 57:69–75
Nyman S, Lindhe J, Karring T (1992) Reattachment–New attachment. In: Lindhe J (ed) Textbook of clinical periodontology. Munksgaard, Copenhagen
Adrians PA, Edwards CA, De Boever IA et al (1988) Ultrastructural observations on bacterial invasion in cementum and radicular dentin of periodontally diseased human teeth. J Periodontol 59:493–503
Yukna RA, Scott JB, Aichelmann-Reidy ME et al (1997) Clinical evaluation of the speed and effectiveness of subgingival calculus removal on single-rooted teeth with diamond-coated ultrasonic tips. J Periodontol 68(5):436–442
Polson AM, Frederic GT, Ladenheim S et al (1984) The production of a root surface smear layer by instrumentation and its removal by citric acid. J Periodontol 55:443–446
Moritz A, Schoop U, Goharkhay K et al (1998) Treatment of periodontal pockets with a diode laser. Lasers Surg Med 22:302–311
Rossman JA, Cobb M (1995) Lasers in periodontal therapy. Periodontol 2000(9):150–164
Watanabe H, Ishikawa I, Suzuki M (1996) Clinical assessments of the erbium:YAG laser for soft tissue surgery and scaling. J Clin Laser Med Surg 14(2):67–75
Folwaczny M, Mehl A, Haffner C et al (2003) Root substance removal with Er:YAG laser radiation at different parameters using a new delivery system. J Periodontol 74(2):147–155
Ando Y, Aoki A, Watanabe H et al (1996) Bactericidal effect of erbium YAG laser on periodontopathic bacteria. Lasers Surg Med 19:190–200
Folwaczny M, Mehl A, Aggstaller H et al (2002) Antimicrobial effects of 2.94 micron Er:YAG laser radiation on root surfaces: an in vitro study. J Clin Periodontol 29:73–78
Yamaguchi H, Kobayashi K, Osada R et al (1997) Effects of irradiation of an erbium:YAG laser radiation on root surfaces. J Periodontol 68:1151–1155
Theodoro LH, Haaypek P, Bachmann L et al (2003) Effect of Er:YAG and diode laser irradiation on the root surfaces: morphological and thermal analysis. J Periodontol 74:838–843
Caton J, Zander HA (1976) Osseous repair of an intrabony pocket without new attachment of connective tissue. J Clin Periodontol 3:54–58
Listgarten MA, Rosenberg MM (1979) Histological study of repair following new attachment procedures in human periodontal lesions. J Periodontol 50:333–344
Centry IG, Blank LW, Levy BA et al (1997) Carbon dioxide laser for de-epithelization of periodontal flaps. J Periodontol 68(8):763–768
Israel M, Rossmann JA, Froum SJ (1995) Use of the carbon dioxide laser in retarding epithelial migration: a pilot histological study utilizing case reports. J Periodontol 66:197–203
Kelbauskiene S, Maciulskiene V (2007) A pilot study of Er,Cr:YSGG laser therapy used as an adjunct to scaling and root planing in patients with early and moderate periodontitis. Stomatologija 9(1):21–26
Nyman S, Gottlow J, Karring T et al (1982) The regenerative potential of the periodontal ligament: an experimental study in monkeys. J Clin Periodontol 9:257
Nyman S, Lindhe J, Karring T et al (1982) New attachment following surgical treatment of human periodontal disease. J Clin Periodontol 9:290
Loe H, Silness J (1963) Periodontal disease in pregnancy. Prevalence and severity. Acta Odontol Scand 21:553–551
Melcher AH (1976) On the repair potential of periodontal tissues. J Periodontol 47(5):256–260
Melcher AH, Mcculloch CAG, Cheong T et al (1987) Cells from bone synthesize cementum-like and bone-like tissue in vitro and may migrate into periodontal ligament in vivo. J Periodontal Res 22:246–247
Shulean A, Schwarz F, Berakdar M et al (2004) Periodontal treatment with an Er:YAG laser compared to ultrasonic instrumentation: a pilot study. J Periodontol 75:966–973
Schwarrz F, Berakdar M, Georg T et al (2003) Clinical evaluation of an Er:YAG laser combined with scaling and root planing for non-surgical periodontal treatment. J Clin Periodontol 30:26–34
Crespi R, Cappare P, Toscanelli I, Gherlone E et al (2007) Effects of Er:YAG laser compared to ultrasonic scaler in periodontal treatment: a 2-year follow-up split mouth clinical study. J Periodontol 78:1195–1200
Schwarz F, Berakdar M, Georg T, Reich E et al (2003) Clinical evaluation of an Er:YAG laser combined with scaling and root planing for non-surgical periodontal treatment. J Clin Periodontol 30:26–34
Blomlof JP, Blomlof LB, Lindskog SF (1996) Smear removal and collagen exposure after non-surgical root planing followed by etching with an EDTA gel preparation. J Periodontol 67(9):841–845
Polson AM, Frederich GT, Ladenheim S, Hanes PJ (1984) The production of a root surface smear layer by instrumentation and its removal by citric acid. J Periodontol 55:443–446
Crespi R, Romanos GE, Cassinelli C, Gherlone E (2006) Effects of Er:YAG laser and ultrasonic system on fibroblast attachment to root surfaces: in vitro study. J Periodontol 77:1217–1222
Schwarz F, Shulean A, Georg T, Reich E (2001) Periodontal treatment with an Er:YAG laser compared to scaling and root planing. A controlled clinical study. J Periodontol 72:361–368
Folwaczny M, Aggsataller H, Mehl A, Hickel R (2003) Removal of bacterial endotoxin from root surface with Er:YAG laser. Am J Dent 16:3–5
Renvert S, Wikstrom M, Dahlen G, Slots J et al (1990) Effect of root debridement on the elimination of Actinobacillus actinomycetemcomitans. J Clin Periodontol 17:345–350
Takamatsu N, Yano K, He T, Umeda M et al (1999) Effect of initial periodontal therapy on the frequency of detecting Bacteroides forsythus, Porphyromonas gingivalis and Actinobacillus actinomycetemcomitans. J Periodontol 70:574–580
Centty I, Blank L, Levy B et al (1997) Carbon dioxide laser for de-epithelization of periodontal flaps. J Periodontol 763–768
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kelbauskiene, S., Baseviciene, N., Goharkhay, K. et al. One-year clinical results of Er,Cr:YSGG laser application in addition to scaling and root planing in patients with early to moderate periodontitis. Lasers Med Sci 26, 445–452 (2011). https://doi.org/10.1007/s10103-010-0799-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-010-0799-4