Abstract
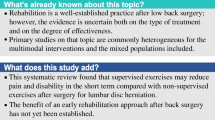
Purpose
To evaluate the effectiveness of rehabilitation strategies on disability, pain, pain-related fear, and return-to-work in patients undergoing lumbar fusion surgery for degenerative conditions or adult isthmic spondylolisthesis.
Methods
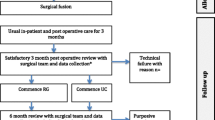
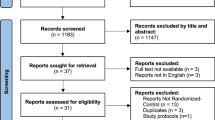
Six electronic databases were systematically searched for randomized controlled trials (RCTs) evaluating the effect of rehabilitation (unimodal or multimodal). The estimated effect size was calculated for interventions with homogeneous content using a random-effects model. Certainty of evidence was assessed by GRADE.
Results
In total, 18 RCTs, including 1402 unique patients, compared specific rehabilitation to other rehabilitation strategies or usual care. Most described indications were degenerative disc disease and spondylolisthesis. All rehabilitation interventions were delivered in the postoperative period, and six of them also included a preoperative component. Intervention dose and intensity varied between studies (ranging from one session to daily sessions for one month). Usual care consisted mostly of information and postoperative mobilization. At short term, low quality of evidence shows that exercise therapy was more effective for reducing disability and pain than usual care (standardized mean difference [95% CI]: −0.41 [−0.71; −0.10] and −0.36 [−0.65; −0.08], four and five studies, respectively). Multimodal rehabilitation consisted mostly of exercise therapy combined with cognitive behavioral training, and was more effective in reducing disability and pain-related fear than exercise therapy alone (−0.31 [−0.49; −0.13] and −0.64 [−1.11; −0.17], six and four studies, respectively). Effects disappeared beyond one year. Rehabilitation showed a positive tendency towards a higher return-to-work rate (pooled relative risk [95% CI]: 1.30 [0.99; 1.69], four studies).
Conclusion
There is low-quality evidence showing that both exercise therapy and multimodal rehabilitation are effective for improving outcomes up to six months after lumbar fusion, with multimodal rehabilitation providing additional benefits over exercise alone in reducing disability and pain-related fear. Additional high-quality studies are needed to demonstrate the effectiveness of rehabilitation strategies in the long term and for work-related outcomes.







Similar content being viewed by others
References
Rajaee SS, Bae HW, Kanim LE, Delamarter RB (2012) Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976) 37:67–76. https://doi.org/10.1097/BRS.0b013e31820cccfb
Al Jammal OM, Delavar A, Maguire KR, Hirshman BR, Wali AR, Kazzaz M et al (2019) National trends in the surgical management of lumbar spinal stenosis in adult spinal deformity patients. Spine (Phila Pa 1976) 44:E1369–E1378. https://doi.org/10.1097/brs.0000000000003155
Van Grinsven V (2018) Lumbar fusion surgery: are fusion success and clinical outcome associated? https://www.scriptiebank.be/scriptie/2018/lumbar-fusion-surgery-are-fusion-success-and-clinical-outcome-associated. Accessed 28 Apr 2021
Reisener M-J, Pumberger M, Shue J, Girardi FP, Hughes AP (2020) Trends in lumbar spinal fusion-a literature review. J Spine Surg 6:752–761. https://doi.org/10.21037/jss-20-492
Khor S, Lavallee DC, Cizik AM, Bellabarba C, Dagal A, Hart RA et al (2020) Hospital and surgeon variation in patient-reported functional outcomes after lumbar spine fusion: a statewide evaluation. Spine (Phila Pa 1976) 45:465–472. https://doi.org/10.1097/BRS.0000000000003299
Strömqvist B, Fritzell P, Hägg O, Jönsson B, Sandén B (2013) Swespine: the Swedish spine register: the 2012 report. Eur Spine J 22:953–974. https://doi.org/10.1007/s00586-013-2758-9
Hedlund R, Johansson C, Hägg O, Fritzell P, Tullberg T (2016) The long-term outcome of lumbar fusion in the Swedish lumbar spine study. Spine J 16:579–587. https://doi.org/10.1016/j.spinee.2015.08.065
Mannion AF, Brox JI, Fairbank JC (2013) Comparison of spinal fusion and nonoperative treatment in patients with chronic low back pain: long-term follow-up of three randomized controlled trials. Spine J 13:1438–1448
Greenwood J, McGregor A, Jones F, Mullane J, Hurley M (2016) Rehabilitation following lumbar fusion surgery: a systematic review and meta-analysis. Spine (Phila Pa 1976) 41:E28–E36. https://doi.org/10.1097/brs.0000000000001132
Madera M, Brady J, Deily S, McGinty T, Moroz L, Singh D et al (2017) The role of physical therapy and rehabilitation after lumbar fusion surgery for degenerative disease: a systematic review. J Neurosurg Spine 26:694–704. https://doi.org/10.3171/2016.10.Spine16627
van Erp RMA, Jelsma J, Huijnen IPJ, Lundberg M, Willems PC, Smeets R (2018) Spinal surgeons’ opinions on pre- and postoperative rehabilitation in patients undergoing lumbar spinal fusion surgery: a survey-based study in the Netherlands and Sweden. Spine (Phila Pa 1976) 43:713–719. https://doi.org/10.1097/brs.0000000000002406
Gilmore SJ, McClelland JA, Davidson M (2016) Physiotherapy management of patients undergoing lumbar spinal surgery: a survey of Australian physiotherapists. N Z J Physiother 44:105–112
Rushton A, Wright C, Heap A, White L, Eveleigh G, Heneghan N (2014) Survey of current physiotherapy practice for patients undergoing lumbar spinal fusion in the United Kingdom. Spine (Phila Pa 1976) 39:E1380–E1387. https://doi.org/10.1097/brs.0000000000000573
Rushton A, Eveleigh G, Petherick EJ, Heneghan N, Bennett R, James G et al (2012) Physiotherapy rehabilitation following lumbar spinal fusion: a systematic review and meta-analysis of randomised controlled trials. BMJ Open. https://doi.org/10.1136/bmjopen-2012-000829
Janssen ERC, Punt IM, Clemens MJ, Staal JB, Hoogeboom TJ, Willems PC (2021) Current prehabilitation programs do not improve the postoperative outcomes of patients scheduled for lumbar spine surgery: a systematic review with meta-analysis. J Orthop Sports Phys Ther 51:103–114. https://doi.org/10.2519/jospt.2021.9748
HHiggins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2022) Cochrane handbook for systematic reviews of interventions version 6.3. https://www.training.cochrane.org/handbook
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Jane F (2018) Removing duplicates from an EndNote library. https://blogs.lshtm.ac.uk/library/2018/12/07/removing-duplicates-from-an-endnote-library/. Accessed 28 Apr 2021
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan—a web and mobile app for systematic reviews. Syst Rev 5:210. https://doi.org/10.1186/s13643-016-0384-4
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Cochrane Training (2021) RoB 2: learning live webinar series. https://training.cochrane.org/rob-2-learning-live-webinar-series
Hanel J, Owen PJ, Held S, Tagliaferri SD, Miller CT, Donath L et al (2020) Effects of exercise training on fear-avoidance in pain and pain-free populations: systematic review and meta-analysis. Sports Med 50:2193–2207. https://doi.org/10.1007/s40279-020-01345-1
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D et al (2014) Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 348:g1687. https://doi.org/10.1136/bmj.g1687
Balduzzi S, Schwarzer G (2019) How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 22:153–160
Harrer M, Cuijpers P, Furukawa TA, Ebert DD (2019) Doing meta-analysis in R: a hands-on guide. PROTECT Lab, Erlangen
R Core Team (2020) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Australia
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926. https://doi.org/10.1136/bmj.39489.470347.AD
Rolving N, Nielsen CV, Christensen FB, Holm R, Bünger CE, Oestergaard LG (2015) Does a preoperative cognitive-behavioral intervention affect disability, pain behavior, pain, and return to work the first year after lumbar spinal fusion surgery? Spine (Phila Pa 1976) 40:593–600. https://doi.org/10.1097/brs.0000000000000843
Abbott AD, Tyni-Lenné R, Hedlund R (2010) Early rehabilitation targeting cognition, behavior, and motor function after lumbar fusion: a randomized controlled trial. Spine (Phila Pa 1976) 35:848–857. https://doi.org/10.1097/BRS.0b013e3181d1049f
Ilves O, Häkkinen A, Dekker J, Wahlman M, Tarnanen S, Pekkanen L et al (2017) Effectiveness of postoperative home-exercise compared with usual care on kinesiophobia and physical activity in spondylolisthesis: a randomized controlled trial. J Rehabil Med 49:751–757. https://doi.org/10.2340/16501977-2268
Greenwood J, McGregor A, Jones F, Hurley M (2019) Rehabilitation following lumbar fusion surgery (REFS) a randomised controlled feasibility study. Eur Spine J 28:735–744. https://doi.org/10.1007/s00586-019-05913-6
Monticone M, Ferrante S, Teli M, Rocca B, Foti C, Lovi A et al (2014) Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomised controlled trial. Eur Spine J 23:87–95. https://doi.org/10.1007/s00586-013-2889-z
Lotzke H, Brisby H, Gutke A, Hägg O, Jakobsson M, Smeets R et al (2019) A person-centered prehabilitation program based on cognitive-behavioral physical therapy for patients scheduled for lumbar fusion surgery: a randomized controlled trial. Phys Ther 99:1069–1088. https://doi.org/10.1093/ptj/pzz020
Strøm J, Nielsen CV, Jørgensen LB, Andersen NT, Laursen M (2019) A web-based platform to accommodate symptoms of anxiety and depression by featuring social interaction and animated information in patients undergoing lumbar spine fusion: a randomized clinical trial. Spine J 19:827–839. https://doi.org/10.1016/j.spinee.2018.11.011
Oestergaard LG, Christensen FB, Bünger CE, Søgaard R, Holm R, Helmig P et al (2020) Does adding case management to standard rehabilitation affect functional ability, pain, or the rate of return to work after lumbar spinal fusion? A randomized controlled trial with two-year follow-up. Clin Rehabil 34:357–368. https://doi.org/10.1177/0269215519897106
Oestergaard LG, Nielsen CV, Bünger CE, Sogaard R, Fruensgaard S, Helmig P et al (2012) The effect of early initiation of rehabilitation after lumbar spinal fusion: a randomized clinical study. Spine (Phila Pa 1976) 37:1803–1809. https://doi.org/10.1097/BRS.0b013e31825a17ab
Christensen FB, Laurberg I, Bünger CE (2003) Importance of the back-café concept to rehabilitation after lumbar spinal fusion: a randomized clinical study with a 2-year follow-up. Spine (Phila Pa 1976) 28:2561–2569. https://doi.org/10.1097/01.Brs.0000097890.96524.A1
Kang H, Cho K, Shim S, Yu J, Jung J (2012) Effects of exercise rehabilitation on pain, disability, and muscle strength after posterior lumbar interbody fusion surgery: a randomized controlled trial. J Phys Ther Sci 24:1037–1040. https://doi.org/10.1589/jpts.24.1037
Nielsen PR, Jørgensen LD, Dahl B, Pedersen T, Tønnesen H (2010) Prehabilitation and early rehabilitation after spinal surgery: randomized clinical trial. Clin Rehabil 24:137–148. https://doi.org/10.1177/0269215509347432
Kernc D, Strojnik V, Vengust R (2018) Early initiation of a strength training based rehabilitation after lumbar spine fusion improves core muscle strength: a randomized controlled trial. J Orthop Surg Res 13:151. https://doi.org/10.1186/s13018-018-0853-7
Salik Sengul Y, Kaya N, Yalcinkaya G, Kirmizi M, Kalemci O (2020) The effects of the addition of motor imagery to home exercises on pain, disability and psychosocial parameters in patients undergoing lumbar spinal surgery: a randomized controlled trial. Explore (NY). https://doi.org/10.1016/j.explore.2020.02.001
Elsayyad MM, Abdel-Aal NM, Helal ME (2021) Effect of adding neural mobilization versus myofascial release to stabilization exercises after lumbar spine fusion: a randomized controlled trial. Arch Phys Med Rehabil 102:251–260. https://doi.org/10.1016/j.apmr.2020.07.009
Zhao BX, Wang KZ, Zhao JX, Wang CS, Huang XH, Shu-qiang M et al (2008) Clinical effects of acupuncture after surgical operation in patients with prolapse of the lumbar intervertebral disc. J Tradit Chin Med 28:250–254. https://doi.org/10.1016/s0254-6272(09)60003-0
Oestergaard LG, Maribo T, Bünger CE, Christensen FB (2012) The Canadian Occupational Performance Measure’s semi-structured interview: its applicability to lumbar spinal fusion patients. A prospective randomized clinical study. Eur Spine J 21:115–121. https://doi.org/10.1007/s00586-011-1957-5
Reichart R, Vogel I, Weiss T, Hennig S, Walter J, Kalff R (2011) Short Psychological intervention as a perioperative pain reduction treatment in spinal neurosurgery. J Neurol Surg A Cent Eur Neurosurg 73:387–396. https://doi.org/10.1055/s-0032-1313642
Wewege MA, Jones MD (2021) Exercise-induced hypoalgesia in healthy individuals and people with chronic musculoskeletal pain: a systematic review and meta-analysis. J Pain 22:21–31. https://doi.org/10.1016/j.jpain.2020.04.003
Kemani MK, Hägg O, Jakobsson M, Lundberg M (2020) Fear of movement is related to low back disability during a two-year period in patients who have undergone elective lumbar spine surgery. World Neurosurg 137:e416–e424. https://doi.org/10.1016/j.wneu.2020.01.218
Johansson A-C, Linton SJ, Rosenblad A, Bergkvist L, Nilsson O (2010) A prospective study of cognitive behavioural factors as predictors of pain, disability and quality of life one year after lumbar disc surgery. Disabil Rehabil 32:521–529. https://doi.org/10.3109/09638280903177243
Abbott AD, Tyni-Lenné R, Hedlund R (2011) Leg pain and psychological variables predict outcome 2–3 years after lumbar fusion surgery. Eur Spine J 20:1626–1634. https://doi.org/10.1007/s00586-011-1709-6
Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW (2007) The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med 30:77–94. https://doi.org/10.1007/s10865-006-9085-0
Bränström H, Fahlström M (2008) Kinesiophobia in patients with chronic musculoskeletal pain: differences between men and women. J Rehabil Med 40:375–380. https://doi.org/10.2340/16501977-0186
Vlaeyen JWS, Linton SJ (2000) Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain 85:317–332. https://doi.org/10.1016/s0304-3959(99)00242-0
Boutevillain L, Dupeyron A, Rouch C, Richard E, Coudeyre E (2017) Facilitators and barriers to physical activity in people with chronic low back pain: a qualitative study. PLoS ONE 12:e0179826. https://doi.org/10.1371/journal.pone.0179826
Slade SC, Dionne CE, Underwood M, Buchbinder R (2016) Consensus on exercise reporting template (CERT): explanation and elaboration statement. Br J Sports Med 50:1428–1437. https://doi.org/10.1136/bjsports-2016-096651
Whyte J, Dijkers MP, Fasoli SE, Ferraro M, Katz LW, Norton S et al (2021) Recommendations for reporting on rehabilitation interventions. Am J Phys Med Rehabil 100:5–16. https://doi.org/10.1097/phm.0000000000001581
Acknowledgements
The authors wish to thank Thomas Vandendriessche, Kristel Paque and Krizia Tuand, the biomedical reference librarians of the KU Leuven Libraries, 2Bergen Learning Centre Désiré Collen (Leuven, Belgium), for their help in conducting the systematic literature search.
Funding
This work was supported by the Research Foundation—Flanders (FWO, grant 1181521N) and Competence Centre Physiotherapy UZ/KU Leuven.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The articles screening and selection was performed by LB and TT. Studies' quality assessment and data extraction was performed by LB, TT and CA. Analysis and interpretation of results was performed by LB, LJ and TWS. The first draft of the manuscript was written by LB and all authors revised it critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Availability of data and material
NA.
Code availability
NA.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Thijs Willem Swinnen and Lotte Janssens are shared last authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bogaert, L., Thys, T., Depreitere, B. et al. Rehabilitation to improve outcomes of lumbar fusion surgery: a systematic review with meta-analysis. Eur Spine J 31, 1525–1545 (2022). https://doi.org/10.1007/s00586-022-07158-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07158-2