Abstract
Background
The role of rehabilitation after surgery in patients with low back pain is well recognized. The aim of this systematic review is to summarize and update the existing evidence according to the type of clinical condition and rehabilitation approach.
Methods
This systematic review included RCTs on the effectiveness of rehabilitation after surgery for lumbar disc herniation, spinal stenosis, and spondylolisthesis. We searched the literature for randomized controlled trials indexed in MEDLINE, Embase, CINHAL, CENTRAL, Scopus, PEDro, and Web of Science databases, up to April 15, 2023. We used Cochrane Risk of Bias 2.0 tool to assess each study. We conducted a quantitative synthesis when population, intervention, control, and outcome were sufficiently homogeneous; otherwise, we conducted a qualitative analysis.
Results
Forty-five studies (3.036 subjects) were included and analyzed according to the population considered: lumbar stenosis (1 trial), spondylolisthesis (3 trials), and disc herniation (41 trials). Regarding lumbar stenosis, a supervised active exercise program appears to improve outcomes related to pain, disability, and quality of life both in the short- and mid-term (1 study, n = 60). Concerning spondylolisthesis, kinesiophobia is reduced in the home exercises group compared to usual care, at 3-months follow-up (3 studies, n = 98). For disk herniation, supervised exercises are better than non-supervised exercises to reduce pain (MD -1.14; 95% CIs -1.65, -0.62; 5 trials, n = 250) and disability (SMD -0.70; 95% CIs -1.14, -0.26; 4 trials, n = 175). Supervised exercises are better than advice in reducing pain (SMD -0.91; 95% CIs -1.61, -0.21; 5 trials, n = 341) and disability (SMD -0.80; 95% CIs -1.59, -0.01; 4 trials, n = 261), in the short-term. Supervised exercises are equal to no treatment in reducing pain and disability, at 3 and 6 months after intervention (2 trials, n = 166). These results are supported by a very low to low quality of evidence.
Conclusions
Our research suggests that supervised exercise may be effective in improving patient’s pain and disability after lumbar surgery, but RCTs regarding lumbar spinal stenosis and lumbar spondylolisthesis are still scarce, with significant heterogeneity of proposed interventions.
Similar content being viewed by others

Background
Pain and disability caused by lumbar disc herniation, spondylolisthesis, and stenosis are the most frequent reasons for lumbar surgery referral [1]. Nevertheless, surgical treatment itself may provoke muscle atrophy and weakness [2], stiffness [3], fear of movement, and consequent disability [4] in activities of daily living [5]. Therefore, postoperative physical and mental health may be affected over than expected [6]. For this reason, different rehabilitation programs have been proposed, with the aim to accelerate the resolution of symptoms, especially pain, promoting functional recovery and return to work, reassuring patients, and finally preventing chronic pain, complications, and relapses [7].
The effectiveness of rehabilitation after lumbar surgery has been investigated by several studies. A Cochrane review on lumbar disc herniation surgery [8] found no differences between supervised and home exercises for pain, disability, or perceived overall effect. Moreover, none of the included studies reported an increase in the reoperation rate after the first lumbar surgery.
Another systematic review by Santana-Ríos and colleagues [9] concluded that an early rehabilitation program is recommended for patients undergoing first microdiscectomy, due to the excellent results and the absence of adverse effects. More specifically, positive reinforcement / cognitive intervention along with exercise was considered an effective treatment, potentially an alternative to spinal fusion in patients with symptom recurrence, after the first surgery.
Another Cochrane review on the effectiveness of rehabilitation after lumbar spinal stenosis surgery [10] suggested that active rehabilitation is more effective than usual care in improving back-related functional status, in the short- and long-term. Similar results emerged for secondary outcomes, including short-term improvement in low back pain (LBP) and long-term improvement in both LBP and leg pain, although limited impact was observed for the overall health improvement. The clinical relevance of these effects was reported as medium to small. These conclusions were limited by the few number (# 3) of relevant studies identified. More recently, the Danish Guidelines published in 2019 [11] recommended the use of supervised exercise after surgery for lumbar stenosis, due to its effectiveness on overall health, although no evidence of effects on neurogenic pain was found. These Guidelines did not recommend manual therapy.
With regard to the effectiveness of rehabilitation after surgery for lumbar spondylolisthesis, the North American Spine Society (NASS) Evidence-based Clinical Guidelines [12] concluded that post-surgical rehabilitation (including physical exercise, spinal mobilization/ manipulation, or psychosocial interventions) in degenerative lumbar spondylolisthesis is unresponsive due to the paucity of evidence. These guidelines stated that no systematic review concerning rehabilitation after surgery for isthmic spondylolisthesis is available at present.
All the cited reviews and Guidelines pointed out the need for further, high-quality randomized controlled trials (RCTs), to make their conclusions stronger.
The objective of this review is to estimate the effectiveness of various post-surgical rehabilitation interventions on pain, function, disability, and health in adults after a first surgery for lumbar disc herniation, lumbar spinal stenosis, or lumbar spondylolisthesis. In addition, we aimed to collect the occurrence and severity of adverse events or complications related to post-surgical rehabilitation.
Methods
This systematic review protocol was registered on the PROSPERO database (code ___________CRD42021278556).
Inclusion criteria
Types of studies
We included only RCTs.
Types of participants
We included studies on adults (e.g. people older than 18 years) who underwent first lumbar surgery for lumbar disc herniation, lumbar spinal stenosis, or lumbar spondylolisthesis.
Setting
We considered all settings in which post-surgical rehabilitation can be carried out, such as Hospital Departments of Physical and Rehabilitation Medicine, Physiotherapy and Rehabilitation Outpatient Clinics, Physiotherapy and Rehabilitation Professional Practices, both public and private, as well as home settings in case of self-treatment.
Publication date
We considered all articles published from inception to the search date.
Language
We included all articles without language limitations. Collaborating translators, in case of needs, offered assistance.
State of publication
We included all published RCTs.
Types of interventions
According to the World Health Organization (WHO) [13], rehabilitation is defined as “a set of interventions aimed at optimizing functioning and reducing disability in subjects with health conditions interacting with their environment”. Rehabilitation includes passive/manual techniques and active exercise, with or without the use of physical/mechanical agents, splinting or bracing, education, and strategies for improving self-efficacy. Categorization of rehabilitation interventions is neither simple nor exhaustive, so the authors included in the search strategy all the terms that could includeprocedures used by this discipline.
Comparison
Comparisons can be among different physiotherapy or pharmacological interventions, wait-and-see strategies, placebo, sham, or no intervention.
Types of outcome measures
Primary outcomes were pain measured through the Visual Analogue Scale (VAS) or the Numeric Rating Scale (NRS), and physical function (e.g. the range of motion, measured with a manual or digital goniometer). Secondary outcomes were disability, measured with the Roland and Morris Disability Questionnaire or the Oswestry Disability Index (ODI), and the perceived health status measured through the Short Form-36 (SF-36), or the EuroQol-5 Dimension (EQ-5D).
In addition, we collected adverse events, defined as any adverse symptoms, signs, or temporary illness associated with treatment. Indirect harms were also considered, where an intervention delayed a diagnosis or treatment, and that delay represented potential harm. The need for additional surgery was also considered.
Search strategy for identification of studies
We searched MEDLINE, Embase, CINHAL, CENTRAL, Scopus, PEDro, and Web of Science databases. Different search strategies were used for each database; these included a combination of specific terms (e.g., MeSH in MEDLINE) and free text words to capture key concepts in titles and abstracts (Additional file 1).
We uploaded records into Endnote Web Reference Management software (Clarivate Analytics, Philadelphia, Pennsylvania, USA) to manage articles and remove duplicates. Two independent reviewers screened the articles based by titles and abstracts using RAYYAN.AI website tool, then by full texts according to inclusion and exclusion criteria. Any disagreements were resolved by a third reviewer. We completed this process by also looking through the reference lists of included studies. Review members met before starting the screening process to ensure agreement on the application of pre-defined inclusion criteria. In addition, bimonthly meetings were held to discuss the screening process and any unforeseen challenge.
Data extraction
Two independent reviewers extracted the following data from all the included studies:
-
• populations: socio-demographic information (e.g. age, sex, education, occupation, culture), health status (e.g. comorbidities, previous surgery), geographic region, type of pre-surgical pathology (e.g. lumbar disc herniation, spondylolisthesis, or spinal stenosis), surgical procedure (e.g. microdiscectomy, decompressive laminectomy/laminotomy/foraminotomy, spinal fusion);
-
• interventions: type (e.g. endurance exercise, manual therapy, physical agents), context (e.g. hospital, outpatient clinic), start time (weeks or months after surgery), type of clinician providing the surgery, duration (weeks or months), dosage (times per week);
-
• comparisons: wait and see, placebo, no treatment, other rehabilitation treatments, drugs;
-
• outcomes of interest;
-
• adverse events and further surgery;
-
• key findings stratified by patient characteristics, pre-surgical pathology, type of surgery, and specific type of post-surgical rehabilitation or care programs, where possible.
In case there is more than one outcome measure to evaluate the same construct, different analyses were performed. Any disagreements between the reviewers were resolved through discussion or with the help of a third expert reviewer. Studies’ authors were contacted if there were missing data.
Data synthesis
Reviewers considered pooling studies in a meta-analysis when there was a clinical and methodological homogeneity with respect to the PICO models.
We performed statistical analyses with the REVMAN 5.4 software (produced by the Cochrane Collaboration), using post-treatment data at different endpoints; we categorized short-term (up to 6 months) and long-term (at least 1 year). Endpoints for all studies are given in Additional file 2.
When outcomes were continuous, we calculated the mean difference (MD) if the outcome in all studies was measured with the same scale; otherwise, a standardized mean difference (SMD) was used. We set a 95% confidence interval.
When the PICOs of the included trials implied a common effect between the studies, a fixed effect was chosen; otherwise, a random effect analysis was performed.
In two studies [14, 15] only change-from-baseline scores were reported and we pooled them with other trials’ post-treatment data, backed up by sensitivity analysis (Cochrane, 7.7.3.1; da Costa, 2013).
In case of missing data, first, the reviewers contacted the authors to obtain the missing information; in the absence of any response, the data were extracted when presented only in the form of graphs by using the Web Plot Digitizer ver. 4.5 software (produced by WebPlotDigitizer, 2020). A study [16] reported only median and interquartile range; the mean and standard deviation were imputed considering the sample size as recommended by Hozo et al. [17].
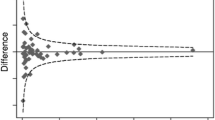
Statistical heterogeneity was calculated by the I2 test and visual analysis of confidence intervals’ overlap. When the reviewers found a moderate to substantial level of heterogeneity (I2 > 50%), subgroup and sensitivity analyses were performed to investigate the source of heterogeneity.
When clinical heterogeneity was relevant, we did not perform meta-analysis instead, we did a qualitative synthesis.
Assessment of risk of bias and quality of evidence
To assess the risk of bias we used the RoB 2.0 Cochrane tool, which contains five domains (Randomization process, Deviations from the intended interventions, Missing outcome data, Measurement of the outcome, Selection of the reported result). If the details reported in a study were insufficient, the reviewers contacted the authors of the original study to obtain more information before conducting the risk of bias assessment. This process was carried out by two independent reviewers; if there was disagreement, a third reviewer intervened to discuss and resolve the debate. At the end of this process, a summary table was created.
The reviewers judged the quality of evidence for all findings through the GRADE (Grading of Recommendations, Assessment, Development and Evaluations) tool and created SoF (Summary of Findings) tables accordingly.
Results
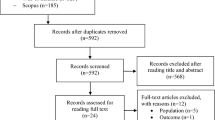
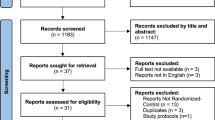
The search was performed from June to October 2021 and updated on April 15, 2023. 14,826 studies were identified and 2 more studies were added by checking the references of the included studies. After removal of duplicates and screening process, 45 studies were included and grouped according to the population considered: lumbar stenosis (1 article), spondylolisthesis (3 articles), and disc herniation (41 articles). Of the latter 41 articles, 11 studies were considered for quantitative analysis, while all other studies were analyzed only qualitatively, due to the high heterogeneity of the intervention, comparison, and outcomes (see Fig. 1).
Description of studies and results
A complete description of the included studies is available in Additional file 2, while the risk of bias assessment is presented in Table 1 and GRADE assessment in Tables 2, 3 and 4.
Lumbar spinal stenosis
Comparison: education plus exercises vs usual care
One RCT on 60 participants was included in this review [18]. Patients were randomly allocated in a peri-operative group and a control group. The peri-operative group received preoperatively and early postoperative education, postural awareness, mobilization strategies, core stability exercises, muscle strengthening exercises, deep breathing exercises, and exercises oriented to the activities of daily living, for 30 min a day during hospitalization. The control group only received instructions on post-operative care (usual care protocol).
Compared with the control group, the peri-operative group demonstrated a significant decrease in pain and higher quality of life (mental health), at 1-month follow-up. On the other hand, the control group demonstrated better scores for both domains of quality of life from 1-month follow-up onwards. The average level of disability improved significantly in both groups at 6-month follow-up. All patients changed their functional capacity. The main improvement was demonstrated in the five repeated sit-to-stands exercises, with no difference between the peri-operative and control group. This study is considered to have a moderate risk of bias, due to the randomization process (unclear) and missing data in the results.
Lumbar spondylolisthesis
Comparison: home exercises versus usual care
The three articles included on rehabilitation after spondylolisthesis surgery [19,20,21] were considered as one study, because they were conducted on the same sample, but on different outcomes. This sample included 98 patients with isthmic (31 patients) or degenerative (67 patients) spondylolisthesis. The aim of the study was to investigate the effectiveness of postoperative 12-month home exercises compared with usual care on pain, disability, quality of life, and kinesiophobia
During the three months after surgery, before the start of physiotherapy intervention, low back and leg pain intensity decreased in both samples. During the 12 months of physiotherapy intervention, no changes in low back or leg pain were observed within the groups. Disability, measured with the ODI scale, decreased in both groups; no differences in quality of life were found at any time point between groups. At 3-month follow-up there was a reduction in kinesiophobia in the home exercise group compared with the usual care group. This study was assessed as affected by a low risk of bias.
Lumbar disc herniation
Forty-one RCTs were included in this systematic review [14,15,16, 22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60], with a total of 3036 participants. Twenty-five studies evaluated the effectiveness of rehabilitation in an early phase after surgery, sixteen RCTs analyzed the interventions within one year and only one RCT studied physiotherapy delivered one year after surgery. The rehabilitation programs were heterogeneous; most studies focused on comparing supervised exercise programs with home-based exercise programs. In addition, education programs were investigated, with a particular attention on the effectiveness of cognitive behavioral therapy.
Quantitative analysis
We pooled 13 trials for three different comparisons: supervised exercises vs non-supervised exercises (6 trials), supervised exercises vs advice (5 trials), and supervised exercises vs no treatment (2 trials). Data included in the meta-analyses were collected at 3 and 6 months after surgery.
Comparison: supervised vs non-supervised exercises
Six trials reported results on short-term effects of supervised exercises vs non-supervised exercises; in one trial [18] the treatment started early after surgery and it was therefore clinically heterogeneous. We pooled the effect from the five remaining trials [14, 22,23,24,25] with a similar delayed approach (mean ± SD = 4.4 ± 0.8 weeks post-surgery).
There is low quality evidence that supervised exercises reduce pain in the short-term (MD -1.14; 95% CIs -1.65, -0.62; I2 = 33%; 5 trials, n = 250) (Fig. 2a). This finding is statistically significant although the clinical impact may be minimal.
There is low quality evidence that supervised exercises reduce disability in the short-term (SMD -0.70; 95% CIs -1.14, -0.26; I2 = 48%; 4 trials, n = 175) (Fig. 2b). This finding is statistically significant with a moderate-large effect.
There is low quality evidence that supervised exercises are not better than non-supervised exercises in improving lumbar range of motion in the short-term (MD -0.27; 95% Cis -0.70, 0.16; I2 = 31%; 2 trials, n = 68) (Fig. 2c).
Comparison: supervised exercises vs advice
Five trials [22, 24, 32,33,34] reported results on the effect of supervised exercises vs clinical advice. The reviewers decided to use the term advice to collect interventions like guidebook, booklet or electronic file containing advice on exercises and movements to do or to avoid.
A high statistical heterogeneity emerged, partially reduced with subgroup analysis: in three trials [32,33,34] the treatment started early after surgery, while in two trials [22, 24] a delayed rehabilitation approach was delivered.
There is very low quality evidence that supervised exercises are better than advice in reducing pain (SMD -0.91; 95% CIs -1.61, -0.21; I2 = 87%; 5 trials, n = 341) (Fig. 2d) and disability (SMD -0.80; 95% CIs -1.59, -0.01; I2 = 84%, 4 trials, n = 261) in the short-term (Fig. 2e). After the subgroup analyses, only the delayed approach confirmed these findings for both outcomes, while no significant differences emerged in the early approach.
Comparison: supervised exercises vs no treatment
Two trials [15, 29] reported results on the effect of supervised exercises vs no treatment with a late rehabilitation approach. A medium to low statistical heterogeneity was found.
There is very low-quality evidence supporting that supervised exercises are better than treatment in reducing pain (MD -0.34; 95% CIs -7.32, 6.63; I2 = 5%; 2 trials, n = 166) (Fig. 2f) and disability (SMD -0.13; 95% CIs -0.5, 0.24; I2 = 11%; 2 trials, n = 166) (Fig. 2g) at 3 months after intervention.
There is very low-quality evidence that no treatment is better than supervised exercises in reducing pain (MD 9.28; 95% CIs 2.78, 15.77; I2 = 9%; 2 trials, n = 166) (Fig. 2h) and no better than supervised exercises for disability (SMD -0.06; 95% CIs -0.71, 0.59; I2 = 53%; 2 trials, n = 166) (Fig. 2i) at 6 months after surgery.
Qualitative analysis
A complete description of the qualitative analysis of the lumbar disc herniation studies is reported in Additional file 3.
Adverse events
No relevant adverse events or further surgery related to the post-surgical rehabilitation emerged.
Assessment of risk of bias: overview
Only 8 included studies had low risk of bias [19, 20, 22, 23, 25, 34, 35, 37, 43], whereas 14 studies had moderate risk of bias [14, 18, 28, 31, 33, 38, 39, 41, 47, 53,54,55, 58, 59], and 21 studies had high risk of bias [15, 16, 24, 26, 27, 29, 30, 32, 36, 40, 42, 44,45,46, 48,49,50,51,52, 56, 57] (see Table 2).
The randomization procedure and allocation concealment were not adequately described in 13 RCTs with a high risk of bias and in 8 articles with a moderate risk of bias.
Deviations from the interventions occurred in 27 studies, mainly due to the inability to blind patients and caregivers to the interventions. 10 articles did not report all data, so results were probably biased by missing information.
In 13 RCTs with a high risk of bias and 5 RCTs with a moderate risk of bias, the authors used an inadequate method to detect outcomes between groups. For example Beneck et al. [50] used a patient-reported outcome measure, but only patients in the intervention group had a constant confrontation with the therapist, and this may have influenced the final questionnaire score. Finally, only 2 RCTs presented problems in the selection of the reported result; for example one RCT [49] did not report secondary outcome scores related to disability and pain.
Discussion
The aim of this systematic review was to investigate the effectiveness of postoperative physiotherapy, in patients after surgery for lumbar stenosis, spondylolisthesis, or disc herniation. Due to the scarcity and heterogeneity of data collected, quantitative analysis was conducted only for the population with lumbar disc herniation. In fact, not enough articles were found on stenosis and spondylolisthesis populations, and most of them considered mixed samples without stratification by pathology. Finally, the outcomes and endpoints were often heterogeneous and not comparable.
Concerning lumbar stenosis, the article by Chen et al. [18] showed that a supervised active exercise program brings some improvements in pain, disability, and quality of life (mental health) in both the short and medium term, while no significant improvements were observed in functional testing. The results of this study are consistent with a Cochrane review [10], reporting the effectiveness of active exercise, in patients operated for lumbar stenosis.
Only one study on lumbar stenosis could be included in this review, while three were included in the Cochrane review [10], where a meta-analysis was performed. One reason for this difference is related to our inclusion criteria, which were more stringent. In particular, the study by Mannion et al. [1], included in the Cochrane review, was excluded from our work because it considered patients who had previously undergone lumbar surgery; the study by Aalto et al. [61] was excluded due to the lack of a true randomization. In addition, Cochrane authors [10] included in their meta-analysis two studies on heterogeneous populations, which did not meet specific diagnostic criteria for lumbar spinal stenosis. Indeed, both studies by Mannion et al. [1] and McGregor et al. [31] also included also patients operated for herniated discs.
The three articles on spondylolisthesis included in our review [19,20,21] were considered as one study. In the first publication [19], there was no significant difference on disability between the home exercises and the usual care group; the first ODI assessment was performed three months after surgery, when the exercise intervention started. This is the reason why it was not possible to measure the change in disability during the early three months after surgery, as in the study by Abbott et al. [60] where this outcome significantly improved. However, Abbott studied a mixed population of patients operated for spondylolisthesis, herniated disc, and stenosis. Information and education strategies provided only to the exercise group did not seem to have the same effect as in the study by Monticone et al. [62] on a mixed population (patients operated for spondylolisthesis and stenosis), in which cognitive and behavioral treatment in addition to exercise was more effective than exercise alone.
Kinesiophobia and activity levels assessed by Ilves et al. [20] did not significantly change between the two groups, despite the presence of educational sessions in the intervention group compared to the control one. Like disability, the greatest improvement of kinesiophobia seems to occur in the first months after surgery.
These results could suggest to investigate the best timing of rehabilitation program, as Oestergaard et al. [63, 64] found that early rehabilitation had no significant ineffective on pain, disability, and quality of life, and it was more expensive. There is currently no consensus in the literature on the most effective rehabilitation program after surgery for lumbar spondylolisthesis.
Concerning physiotherapy after surgery for lumbar herniation, our findings support the Cochrane review by Oosterhuis et al. [8], which suggested that therapeutic programs should be started between week 4 and 6 after surgery and that the methodological quality of future RCT studies should be improved. However, there are differences in the inclusion criteria between the present study and the Cochrane review. In fact, we excluded the studies by Alaranta et al. [65], Kjellby-Wendt et al. [66] and Donaldson et al. [67] because they included patients younger than 18 years old; the study of Scrimshaw et al. [68] due to a mixed population considering patients with herniated disc, stenosis, and spondylolisthesis; and finally, the study by Timm et al. [69] which was performed on a sample that was not representative of the general population, as all subjects worked in the same place.
We found a relevant heterogeneity in terms of type, duration, frequency, and intensity of rehabilitation interventions. However, it was noted that in 28 studies [14, 22,23,24,25,26, 28, 32,33,34,35,36,37,38,39, 42,43,44, 46, 48, 49, 51,52,53,54,55, 57, 59], rehabilitation started within four weeks after surgery, while in 12 studies [15, 16, 22, 26, 29, 31, 41, 45, 47, 50, 56, 58], physiotherapy began after the fourth postoperative week. Only one study [39] considered a treatment starting one year after surgery.
Compared to the systematic review by Atsidakou et al. [70] which support with moderate evidence the effectiveness of an early rehabilitation in patients operated for lumbar disc herniation, the results of our systematic review argues for greater caution. This different conclusion is probably related to the fact that Atsidakou et al. [70] included only seven RCTs, excluding all studies on patients performing supervised exercise as a control group or studies in which the intervention group carried out any other treatment, besides supervised exercise.
Regarding the type of intervention, most of the supervised exercises were described, although the programs were very heterogeneous. It should be noted that in some studies [14, 16, 22,23,24, 26,27,28,29, 31, 32, 34,35,36,37,38,39, 42, 44, 46, 51, 55, 57,58,59] the authors described the details and dosage of each exercise, while others did not reported them [15, 21, 22, 25, 31, 40, 41, 43, 45, 47,48,49, 52,53,54]. Extracting and categorizing treatments for both intervention and control groups was very difficult because of the reporting of the articles and the high heterogeneity of interventions’ types and definitions (e.g. “usual care”, “no treatment”, “advice”, etc.). We strongly expect that future RCTs follow the TIDieR Checklist and the World Physiotherapy glossary for defining and reporting interventions [71].
After performing the meta-analyses, a clear direction of effect can be confirmed toward a face-to-face physiotherapy intervention versus non-supervised exercises or post-surgical pain and disability counseling for the delayed approach. However, an early approach should not be discouraged a priori, but more primary studies investigating the immediate post-surgery rehabilitation are needed.
In a different way from the Cochrane Review by Oosterhuis et al. [8], our findings suggest a significant improvement in disability for patients undergoing supervised exercise programs compared with those involved in non-supervised exercise programs; this discordance is mostly due to the inclusion of two RCTs [16, 28] published after the last search by the Cochrane group.
Education as an intervention has been studied in many articles. According to Ostelo et al. [47], different educational interventions (cognitive-behavioral therapy and standard education) produce similar effects, while the combination of supervised exercises with education can produce superior results, compared to instruction alone [30, 50, 51].
A limitation in this review may be the exclusion of grey literature consistently with our protocol.
Conclusions
In this review only studies concerning rehabilitation after surgery for lumbar disc herniation could be pooled in a quantitative analysis. These meta-analyses showed with low quality evidence that supervised exercises can reduce short-term pain and disability compared with non-supervised exercises, but do not significantly improve lumbar range of motion. In addition, supervised exercises were found to be better than advice in reducing short-term pain and disability, with a low quality evidence.
Suggestions concerning rehabilitation after lumbar spinal stenosis and spondylolisthesis surgery arise only from qualitative analyses. In lumbar spinal stenosis surgery, education and exercises in the peri-surgical period seems to induce similar results when compared to usual care. In lumbar spondylolisthesis surgery, home exercises significantly reduce kinesiophobia in the short-term, but do not improve pain or disability in the long-term follow-ups, compared with usual care.
This research suggests that multimodal rehabilitation protocols after lumbar surgery may be used to improve outcomes such as pain, disability, and physical function, but reveals a scarcity of RCTs regarding rehabilitation after surgery for lumbar spinal stenosis and lumbar spondylolisthesis and relevant heterogeneity of proposed interventions.
Further research should be conducted on the effectiveness of combined pre-operative and post-operative rehabilitation programs, the best time to start physiotherapy after interventions, and the long-term effects. There is a need to improve the overall quality of the studies on this topic.
Availability of data and materials
The datasets analysed during the current review and the metanalisis are available from the correspondent author on reasonable request.
Abbreviations
- CIs:
-
Confidence Intervals
- EQ-5D:
-
EuroQol-5 Dimension
- GRADE:
-
Granding of recommendation, Assessment, development and Evaluation
- LBP:
-
Low Back Pain
- MD:
-
Mean Difference
- NASS:
-
North American Spine Society
- NRS:
-
Numeric rating Scale
- ODI:
-
Oswestry Disability Index
- PICO:
-
Patient, Intervention/Treatment, Control, Outcome
- RCT:
-
Randomized Clinical Trial
- RoB:
-
Risk of Bias
- SF-36:
-
Short-Form 36
- SMD:
-
Standardized Mean Difference
- SoF:
-
Summary of Findings
- TIDieR:
-
Template for Intervention Description and Replication
- VAS:
-
Visual Analogue Scale
- WHO:
-
World Health Organization
References
Mannion AF, Impellizzeri FM, Luenig M, Jeszenszy D, Becker HJ, Haschtmann D, Preiss S, Fehete TF. Time to remove our rose-tinted spectacles: a candid appraisal of the relative success of surgery in over 4500 patients with degenerative disorders of the lumbar spine, hip or knee. Eur Spine J. 2018;27(4):778–88.
Pourtaheri S, Issa K, Lord E, Ajiboye R, Drysch A, Hwang K, Faloon M, Sinha K, Emami A. Paraspinal muscle atrophy after lumbar spine surgery. Orthopedics. 2016;39(2):e209–14.
Hakkinen A, Kuukkanen T, Tarvainen U, Ylinen J. Trunk muscle strength in flexion, extension, and axial rotation in patients managed with lumbar disc herniation surgery and in healthy control subjects. Spine (Phila Pa 1976). 2003;28(10):1068–73.
Choi JH, Jang JS, Yoo KS, Shin JM, Jang IT. Functional limitations due to stiffness after long-level spinal instrumented fusion surgery to correct lumbar degenerative flat back. Spine. 2018;43(15):1044–51.
Kimura H, Fujibayashi S, Otsuki B, Takahashi Y, Nakayama T, Matsuda S. Effects of lumbar stiffness after lumbar fusion surgery on activities of daily living. Spine. 2016;41(8):719–27.
Ravishankar P, Winkleman R, Rabah N, Steinmetz M, Mroz T. Analysis of patient-reported outcomes measures used in lumbar fusion surgery research for degenerative spondylolisthesis. Clin Spine Surg. 2022;35(6):287–94.
Rushton A, Wright C, Goodwin P, Calvert M, Freemantle N. Physiotherapy rehabilitation post first lumbar discectomy: a systematic review and meta-analysis of randomized controlled trials. Spine. 2011;36(14):E961–72.
Oosterhuis T, Costa LO, Maher CG, de Vet HC, van Tulder MW, Ostelo RW. Rehabilitation after lumbar disc surgery. Cochrane Database Syst Rev. 2014;2014(3):CD003007.
Santana-Ríos JS, Chívez-Arias DD, Coronado-Zarco R, Cruz-Medina E, Nava-Bringas T. Tratamiento postquirúrgico de hernia discal lumbar en rehabilitación. Revisión sistemática [Postoperative treatment for lumbar disc herniation during rehabilitation. Systematic review]. Acta Ortop Mex. 2014;28(2):113–24 Spanish.
McGregor AH , Probyn K, Cro S, Doré CJ, Burton AK, Balagué F, et al. Rehabilitation following surgery for lumbar spinal stenosis. A Cochrane Review. Spine. 2014;39(13):1044–54.
Rousing R, Jensen RK, Fruensgaard S, Strøm J, Brøgger HA, Degn JDM, Andersen MØ. Danish national clinical guidelines for surgical and nonsurgical treatment of patients with lumbar spinal stenosis. Eur Spine J. 2019;28(6):1386–96.
Matz PG, Meagher RJ, Lamer T, Tontz WL Jr, Annaswamy TM, Cassidy RC, Cho CH, Dougherty P, Easa JE, Enix DE, Gunnoe BA, Jallo J, Julien TD, Maserati MB, Nucci RC, O’Toole JE, Rosolowski K, Sembrano JN, Villavicencio AT, Witt JP. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J. 2016;16(3):439–48.
Rehabilitation. November 2021, Accessible on https://www.who.int/news-room/fact-sheets/detail/rehabilitation.
Lu Z, Bai JZ. A prospective study on the application of staged lumbar motion chain in rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy. Chin J T issue Eng Res. 2021;25(9):1398–403.
Paulsen RT, Carreon LY, Andersen MØ. Patient-reported outcomes after surgery for lumbar disc herniation, a randomized controlled trial comparing the effects of referral to municipal physical rehabilitation versus no referral. Spine (Phila Pa 1976). 2020;45(1):3–9.
Demir S, Dulgeroglu D, Cakci A. Effects of dynamic lumbar stabilization exercises following lumbar microdiscectomy on pain, mobility and return to work. randomized controlled trial. Eur J Phys Rehabil Med. 2014;50(6):627–40.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;20(5):13.
Chen CY, Chang CW, Lee ST, Chen YC, Tang SF, Cheng CH, Lin YH. Is rehabilitation intervention during hospitalization enough for functional improvements in patients undergoing lumbar decompression surgery? a prospective randomized controlled study. Clin Neurol Neurosurg. 2015;129(Suppl 1):S41–6.
Ilves O, Häkkinen A, Dekker J, Pekkanen L, Piitulainen K, Järvenpää S, Marttinen I, Vihtonen K, Neva MH. Quality of life and disability: can they be improved by active postoperative rehabilitation after spinal fusion surgery in patients with spondylolisthesis? a randomised controlled trial with 12-month follow-up. Eur Spine J. 2017;26(3):777–84.
Ilves O, Häkkinen A, Dekker J, Wahlman M, Tarnanen S, Pekkanen L, Ylinen J, Kautiainen H, Neva M. Effectiveness of postoperative home- exercise compared with usual care on kinesiophobia and physical activity in spondylolisthesis: a randomized controlled trial. J Rehabil Med. 2017;49(9):751–7.
Ilves O, Neva MH, Häkkinen K, Dekker J, Järvenpää S, Kyrölä K, Häkkinen A. Effectiveness of a 12-month home-based exercise program on trunk muscle strength and spine function after lumbar spine fusion surgery: a randomized controlled trial. Disabil Rehabil. 2022;44(4):549–57.
Johansson AC, Linton SJ, Bergkvist L, Nilsson O, Cornefjord M. Clinic-based training in comparison to home-based training after first-time lumbar disc surgery: a randomised controlled trial. Eur Spine J. 2009;18(3):398–409.
Hebert JJ, Fritz JM, Thackeray A, Koppenhaver SL, Teyhen D. Early multimodal rehabilitation following lumbar disc surgery: a randomised clinical trial comparing the effects of two exercise programmes on clinical outcome and lumbar multifidus muscle function. Br J Sports Med. 2015;49(2):100–6.
Zhang R, Zhang SJ, Wang XJ. Postoperative functional exercise for patients who underwent percutaneous transforaminal endoscopic discectomy for lumbar disc herniation. Eur Rev Med Pharmacol Sci. 2018;22(1 Suppl):15–22.
Danielsen JM, Johnsen R, Kibsgaard SK, Hellevik E. Early aggressive exercise for postoperative rehabilitation after discectomy. Spine (Phila Pa 1976). 2000;25(8):1015–20.
Yílmaz F, Yílmaz A, Merdol F, Parlar D, Sahin F, Kuran B. Efficacy of dynamic lumbar stabilization exercise in lumbar microdiscectomy. J Rehabil Med. 2003;35(4):163–7.
Choi G, Raiturker PP, Kim MJ, Chung DJ, Chae YS, Lee SH. The effect of early isolated lumbar extension exercise program for patients with herniated disc undergoing lumbar discectomy. Neurosurgery. 2005;57(4):764–72.
Filiz M, Cakmak A, Ozcan E. The effectiveness of exercise programmes after lumbar disc surgery: a randomized controlled study. Clin Rehabil. 2005;19(1):4–11.
Dolan P, Greenfield K, Nelson RJ, Nelson IW. Can exercise therapy improve the outcome of microdiscectomy? Spine (Phila Pa 1976). 2000;25(12):1523–32.
Kulig K, Beneck GJ, Selkowitz DM, Popovich JM Jr, Ge TT, Flanagan SP, Poppert EM, Yamada KA, Powers CM, Azen S, Winstein CJ, Gordon J, Samudrala S, Chen TC, Shamie AN, Khoo LT, Spoonamore MJ, Wang JC. Physical Therapy Clinical Research Network (PTClinResNet). an intensive, progressive exercise program reduces disability and improves functional performance in patients after single-level lumbar microdiskectomy. Phys Ther. 2009;89(11):1145–57.
McGregor AH, Doré CJ, Morris TP, Morris S, Jamrozik K. ISSLS prize winner: Function After Spinal Treatment, Exercise, and Rehabilitation (FASTER): a factorial randomized trial to determine whether the functional outcome of spinal surgery can be improved. Spine (Phila Pa 1976). 2011;36(21):1711–20.
Oosterhuis T, Ostelo RW, van Dongen JM, Peul WC, de Boer MR, Bosmans JE, Vleggeert-Lankamp CL, Arts MP, van Tulder MW. Early rehabilitation after lumbar disc surgery is not effective or cost-effective compared to no referral: a randomised trial and economic evaluation. J Physiother. 2017;63(3):144–53.
Janssens L, Brumagne S, Claeys K, Pijnenburg M, Goossens N, Rummens S, Depreitere B. Proprioceptive use and sit-to-stand-to-sit after lumbar microdiscectomy: The effect of surgical approach and early physiotherapy. Clin Biomech (Bristol, Avon). 2016;32:40–8.
Erdogmus CB, Resch KL, Sabitzer R, Müller H, Nuhr M, Schöggl A, Posch M, Osterode W, Ungersböck K, Ebenbichler GR. Physiotherapy-based rehabilitation following disc herniation operation: results of a randomized clinical trial. Spine (Phila Pa 1976). 2007;32(19):2041–9.
Ebenbichler GR, Inschlag S, Pflüger V, Stemberger R, Wiesinger G, Novak K, Christoph K, Resch KL. Twelve-year follow-up of a randomized controlled trial of comprehensive physiotherapy following disc herniation operation. Clin Rehabil. 2015;29(6):548–60.
Ju S, Park G, Kim E. Effects of an exercise treatment program on lumbar extensor muscle strength and pain of rehabilitation patients recovering from lumbar disc herniation surgery. J Phys Ther Sci. 2012;24(6):515–8.
Kim BHJ, Ahn JH, Cho HC, Kim DY, Kim TY, Yoon BC. Rehabilitation with osteopathic manipulative treatment after lumbar disc surgery: a randomised, controlled pilot study. Int J Osteopath Med. 2015;18(3):181–8.
Kim BJ, Ahn J, Cho H, Kim D, Kim T, Yoon B. Early individualised manipulative rehabilitation following lumbar open laser microdiscectomy improves early post-operative functional disability: A randomized, controlled pilot study. J Back Musculoskelet Rehabil. 2016;29(1):23–9.
Häkkinen A, Ylinen J, Kautiainen H, Tarvainen U, Kiviranta I. Effects of home strength training and stretching versus stretching alone after lumbar disk surgery: a randomized study with a 1-year follow-up. Arch Phys Med Rehabil. 2005;86(5):865–70.
Manniche C, Asmussen K, Lauritsen B, Vinterberg H, Karbo H, Abildstrup S, Fischer-Nielsen K, Krebs R, Ibsen K. Intensive dynamic back exercises with or without hyperextension in chronic back pain after surgery for lumbar disc protrusion. A clinical trial. Spine (Phila Pa 1976). 1993;18(5):560–7.
Zoia C, Bongetta D, Alicino C, Chimenti M, Pugliese R, Gaetani P. Usefulness of corset adoption after single-level lumbar discectomy: a randomized controlled trial. J Neurosurg Spine. 2018;28(5):481–5.
Kara B, Baskurt F, Acar S, Karadibak D, Ciftci L, Erbayraktar S, Gokmen AN. The effect of TENS on pain, function, depression, and analgesic consumption in the early postoperative period with spinal surgery patients. Turk Neurosurg. 2011;21(4):618–24.
Bono CM, Leonard DA, Cha TD, Schwab JH, Wood KB, Harris MB, Schoenfeld AJ. The effect of short (2-weeks) versus long (6-weeks) post-operative restrictions following lumbar discectomy: a prospective randomized control trial. Eur Spine J. 2017;26(3):905–12.
Aldemir K, Gürkan A. The effect of pedometer-supported walking and telemonitoring after disc hernia surgery on pain and disability levels and quality of life. Int J Nurs Pract. 2021;27(2): e12917.
Rothhaupt D, Laser T, Ziegler H, Liebig K. Die Orthopädische Hippotherapie in der postoperativen Rehabilitation von lumbalen Bandscheibenpatienten. Eine prospektive, randomisierte Therapiestudie [Orthopedic hippotherapy in postoperative rehabilitation of lumbar intervertebral disk patients. A prospective, randomized therapy study]. Sportverletz Sportschaden. 1997;11(2):63–9 German.
Reyes A, Aguilera MP, Torres P, Reyes-Ferrada W, Peñailillo L. Effects of neural mobilization in patients after lumbar microdiscectomy due to intervertebral disc lesion. J Bodyw Mov Ther. 2021;25:100–7.
Ostelo RW, de Vet HC, Berfelo MW, Kerckhoffs MR, Vlaeyen JW, Wolters PM, van den Brandt PA. Effectiveness of behavioral graded activity after first-time lumbar disc surgery: short term results of a randomized controlled trial. Eur Spine J. 2003;12(6):637–44.
Kacar S, Alptekin K, Atilla Alkan ŞN, Öncü J. Comparison of daily living return efficiency of patients with pressure biofeedback and normal exercise program after lumbar disc herniation surgery. Gazz Med Ital - Arch Sci Med. 2020;179(9):512–9.
Newsome RJ, May S, Chiverton N, Cole AA. A prospective, randomised trial of immediate exercise following lumbar microdiscectomy: a preliminary study. Physiotherapy. 2009;95(4):273–9.
Beneck GJ, Popovich JM Jr, Selkowitz DM, Azen S, Kulig K. Physical Therapy Clinical Research Network (PTClinResNet). Intensive, progressive exercise improves quality of life following lumbar microdiskectomy: a randomized controlled trial. Clin Rehabil. 2014;28(9):892–901.
Jentoft ES, Kvåle A, Assmus J, Moen VP. Effect of information and exercise programmes after lumbar disc surgery: a randomized controlled trial. Physiother Res Int. 2020;25(4): e1864.
Zhao BX, Wang KZ, Zhao JX, Wang CS, Huang XH, Shu-qiang M, Qiang H. Clinical effects of acupuncture after surgical operation in patients with prolapse of the lumbar intervertebral disc. J Tradit Chin Med. 2008;28(4):250–4.
Ostelo RW, Goossens ME, de Vet HC, van den Brandt PA. Economic evaluation of a behavioral-graded activity program compared to physical therapy for patients following lumbar disc surgery. Spine (Phila Pa 1976). 2004;29(6):615–22.
Erdogan Z, Bulut H. Effectiveness of computer assisted training of patients undergoing lumbar disc herniation surgery. Turk Neurosurg. 2020;30(1):69–77.
Ozkara GO, Ozgen M, Ozkara E, Armagan O, Arslantas A, Atasoy MA. Effectiveness of physical therapy and rehabilitation programs starting immediately after lumbar disc surgery. Turk Neurosurg. 2015;25(3):372–9.
Manniche C, Skall HF, Braendholt L, Christensen BH, Christophersen L, Ellegaard B, Heilbuth A, Ingerslev M, Jørgensen OE, Larsen E, et al. Clinical trial of postoperative dynamic back exercises after first lumbar discectomy. Spine (Phila Pa 1976). 1993;18(1):92–7.
Kim BJ, Kim T, Ahn J, Cho H, Kim D, Yoon B. Manipulative rehabilitation applied soon after lumbar disc surgery improves late post-operative functional disability: a preliminary 2-year follow-up study. J Back Musculoskelet Rehabil. 2017;30(5):999–1004.
Abdi A, Bagheri SR, Shekarbeigi Z, Usefvand S, Alimohammadi E. The effect or repeated flexion-based versus extension-based exercises on the clinic outcome of patients with lumbar disk herniation surgery: a randomized clinical trial. Neurol Res. 2023;45(1):28–40.
Wang S, Yu HL, Zheng L, Ma JX, Wang H, Xiang LB, Chen Y. Randomized controlled trial of overall functional exercise process in perioperative of percutaneous transforaminal endoscopic discectomy. Medicine. 2022;101:52.
Abbott AD, Tyni-Lenné R, Hedlund R. Early rehabilitation targeting cognition, behavior, and motor function after lumbar fusion: a randomized controlled trial. Spine (Phila Pa 1976). 2010;35(8):848–57.
Aalto TJ, Leinonen V, Herno A, et al. Postoperative rehabilitation does not improve functional outcome in lumbar spinal stenosis: a prospective study with 2-year postoperative follow-up. Eur Spine J. 2011;20(8):1331–40.
Monticone M, Ferrante S, Teli M, et al. Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomised controlled trial. Eur Spine J. 2014;23(1):87–95.
Oestergaard LG, Nielsen CV, Bünger CE, et al. The effect of early initiation of rehabilitation after lumbar spinal fusion: a randomized clinical study. Spine (Phila Pa 1976). 2012;37(21):1803–9.
Oestergaard LG, Christensen FB, Nielsen CV, Bünger CE, Fruensgaard S, Sogaard R. Early versus late initiation of rehabilitation after lumbar spinal fusion: economic evaluation alongside a randomized controlled trial. Spine (Phila Pa 1976). 2013;38(23):1979–85.
Alaranta H, Hurme M, Einola S, Kallio V, Knuts LR, Torma T. Rehabilitation after surgery for lumbar disc herniation: results of a randomized clinical trial. Int J Rehabil Res. 1986;9(3):247–57.
Kjellby-Wendt G, Styf J, Carlsson SG. Early active rehabilitation after surgery for lumbar disc herniation: a prospective, randomized study of psychometric assessment in 50 patients. Acta Orthop Scand. 2001;72(5):518–24.
Donaldson BL, Shipton EA, Inglis G, Rivett D, Frampton C. Comparison of usual surgical advice versus a nonaggravating six-month gym-based exercise rehabilitation program post-lumbar discectomy: results at one-year follow-up. Spine J. 2006;6(4):357–63.
Scrimshaw SV, Maher CG. Randomized controlled trial of neural mobilization after spinal surgery. Spine (Phila Pa 1976). 2001;26(24):2647–52.
Timm KE. A randomized-control study of active and passive treatments for chronic low back pain following L5 laminectomy. J Orthop Sports Phys Ther. 1994;20(6):276–86.
Atsidakou N, Matsi AE, Cristakaou A. The effectiveness of exercise program after lumbar discectomy surgery. J Clin Orthop Trauma. 2021;16:99–105.
Description of Physical Therapy. Policy statement. May 2019. Accessible on https://world.physio/policy/ps-descriptionPT.
Acknowledgements
Not applicable.
Funding
None of the authors have any fundings interests.
Author information
Authors and Affiliations
Contributions
CV,SF and PP were the main supervisors on location and overlooked every step of the process. SF and CV conceived the study and were responsible for drafting the manuscript. All authors were responsible for the study design. TM, NF, CG, IS, IC performed the data collection, undertook the analyses and composed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
None of the authors have any competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Manni, T., Ferri, N., Vanti, C. et al. Rehabilitation after lumbar spine surgery in adults: a systematic review with meta-analysis. Arch Physiother 13, 21 (2023). https://doi.org/10.1186/s40945-023-00175-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40945-023-00175-4