Abstract
Background
Fear of pain and movement is an important factor in the development of hypervigilance and avoidance behaviours.
Objective
We examined the effectiveness of exercise training on improving fear-avoidance beliefs.
Methods
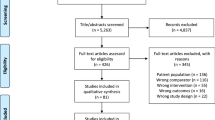
A systematic review (data sources: MEDLINE, CINAHL, SPORTDiscus, EMBASE, CENTRAL) and metaanalysis of randomised controlled/clinical trials of exercise training in adults versus relevant nonexercise comparators that quantified fear-avoidance was conducted.
Results
After screening 4603 identified records, 17 (2014 participants) and 13 (1152 participants) studies were eligible for qualitative and quantitative synthesis, respectively. Pairwise meta-analysis showed exercise training was more effective than all non-exercise comparators (standardised mean difference (SMD) [95% CI] − 0.378 [− 0.623, − 0.133], P = 0.002, Grading of Recommendations Assessment, Development and Evaluation [GRADE]: very low) for reducing fear-avoidance. Exercise training was more effective than true control for reducing fear avoidance (− 0.407 [− 0.750, − 0.065], P = 0.020, GRADE: very low), however it was not more effective than other interventions (− 0.243 [− 0.614, 0.128], P = 0.199, GRADE: very low). In people with low back pain, exercise training was more effective than non-exercise comparator groups for reducing fear-avoidance (− 0.530 [− 0.755, − 0.304], P < 0.001, GRADE: very low). For individuals with neck pain, exercise training was not more effective than non-exercise comparator groups for reducing fear-avoidance (0.061 [− 0.360, 0.482], P = 0.777, GRADE: very low).
Conclusion
There is very low to low-quality evidence that exercise training is effective for reducing fear-avoidance, including in people with low back pain. Exercise training may be more effective than no intervention for reducing fear avoidance, but there is very low-quality evidence that non-exercise interventions are as effective as exercise for fear avoidance. Few studies with low risk of bias is a limitation.
Trail Registration
PROSPERO Registration Number: CRD42019139678.




Similar content being viewed by others
References
Vlaeyen JW, Linton SJ. Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain. 2012;153(6):1144–7.
Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317–32. https://doi.org/10.1016/S0304-3959(99)00242-0.
Lethem J, Slade P, Troup J, Bentley G. Outline of a fear-avoidance model of exaggerated pain perception—I. Behav Res Ther. 1983;21(4):401–8.
Crombez G, Eccleston C, Van Damme S, Vlaeyen JWS, Karoly P. Fear-avoidance model of chronic pain: the next generation. Clin J Pain. 2012;28(6):475–83. https://doi.org/10.1097/AJP.0b013e3182385392.
Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30(1):77–94.
Kori S. Kinesiophobia: a new view of chronic pain behavior. Pain Manag. 1990;35–43.
Vlaeyen JW, Kole-Snijders AM, Boeren RG, Van Eek H. Fear of movement/(re) injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62(3):363–72.
Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–68.
Pfingsten M, Kröner-Herwig B, Leibing E, Kronshage U. Validation of the German version of the fear-avoidance beliefs questionnaire (FABQ). Eur J Pain. 2000;4(3):259–66.
Lee K-C, Chiu TT, Lam T-H. Psychometric properties of the Fear-Avoidance Beliefs Questionnaire in patients with neck pain. Clin Rehabil. 2006;20(10):909–20.
Bränström H, Fahlström M. Kinesiophobia in patients with chronic musculoskeletal pain: differences between men and women. J Rehabil Med. 2008;40(5):375–80.
Luque-Suarez A, Martinez-Calderon J, Falla D. Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: a systematic review. Br J Sports Med. 2019;53(9):554–9.
Picavet HSJ, Vlaeyen JWS, Schouten JSAG. Pain catastrophizing and kinesiophobia: predictors of chronic low back pain. Am J Epidemiol. 2002;156(11):1028–34. https://doi.org/10.1093/aje/kwf136.
Owen PJ, Miller CT, Mundell NL, Verswijveren SJ, Tagliaferri SD, Brisby H et al. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. 2019.
Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389(10070):736–47.
Kernan T, Rainville J. Observed outcomes associated with a quota-based exercise approach on measures of kinesiophobia in patients with chronic low back pain. J Orthop Sports Phys Ther. 2007;37(11):679–87.
Booth J, Moseley GL, Schiltenwolf M, Cashin A, Davies M, Hübscher M. Exercise for chronic musculoskeletal pain: a biopsychosocial approach. Musculoskelet Care. 2017;15(4):413–21.
Martinez-Calderon J, Flores-Cortés M, Morales-Asencio JM, Luque-Suarez A. Conservative interventions reduce fear in individuals with chronic low back pain: a systematic review. Arch Phys Med Rehabil. 2019;101:329.
Moher D, Liberati A, Tetzlaff J, Altman D, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Vincent HK, George SZ, Seay AN, Vincent KR, Hurley RW. Resistance exercise, disability, and pain catastrophizing in obese adults with back pain. Med Sci Sports Exerc. 2014;46(9):1693.
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.0 Cochrane. 2019. https://www.training.cochrane.org/handbook.
Tagliaferri SD, Miller CT, Owen PJ, Mitchell UH, Brisby H, Fitzgibbon B, et al. Domains of chronic low back pain and assessing treatment effectiveness: a clinical perspective. Pain Pract. 2020;2:211. https://doi.org/10.1111/papr.12846.
Bernard P, Ninot G, Bernard P, Picot M, Jaussent A, Tallon G, et al. Effects of a 6-month walking intervention on depression in inactive post-menopausal women: a randomized controlled trial. Aging Ment Health. 2015;19(6):485–92.
Keane LG. Comparing AquaStretch with supervised land based stretching for chronic lower back pain. J Bodyw Move Ther. 2017;21(2):297–305.
Klaber Moffett J, Jackson DA, Gardiner E, Torgerson DJ, Coulton S, Eaton S, et al. Randomized trial of two physiotherapy interventions for primary care neck and back pain patients: ‘McKenzie’ vs brief physiotherapy pain management. Rheumatology. 2006;45(12):1514–21.
Klaber Moffett JA, Torgerson D, Bell-Syer S, Jackson D, Llewlyn-Phillips H, Farrin A, et al. Randomised controlled trial of exercise for low back pain: clinical outcomes, costs, and preferences. BMJ. 1999;319(7205):279–83.
Oksuz S, Unal E. The effect of the clinical pilates exercises on kinesiophobia and other symptoms related to osteoporosis: randomised controlled trial. Complement Ther Clin Pract. 2017;26:68–72.
Smeets RJ, Vlaeyen JW, Hidding A, Kester AD, van der Heijden GJ, van Geel AC, et al. Active rehabilitation for chronic low back pain: cognitive-behavioral, physical, or both? First direct post-treatment results from a randomized controlled trial [ISRCTN22714229]. BMC Musculoskelet Disord. 2006;7(1):5.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
Zadro JR, Shirley D, Simic M, Mousavi SJ, Ceprnja D, Maka K, et al. Video-game–based exercises for older people with chronic low back pain: a randomized controlled table trial (GAMEBACK). Phys Ther. 2018;99(1):14–27.
Bahat HS, Croft K, Carter C, Hoddinott A, Sprecher E, Treleaven J. Remote kinematic training for patients with chronic neck pain: a randomised controlled trial. Eur Spine J. 2018;27(6):1309–23.
Cruz-Díaz D, Bergamin M, Gobbo S, Martínez-Amat A, Hita-Contreras F. Comparative effects of 12 weeks of equipment based and mat Pilates in patients with chronic low back pain on pain, function and transversus abdominis activation. A randomized controlled trial. Complement Ther Med. 2017;33:72–7.
Cruz-Díaz D, Romeu M, Velasco-González C, Martínez-Amat A, Hita-Contreras F. The effectiveness of 12 weeks of Pilates intervention on disability, pain and kinesiophobia in patients with chronic low back pain: a randomized controlled trial. Clin Rehabil. 2018;32(9):1249–57.
Harts CC, Helmhout PH, de Bie RA, Staal JB. A high-intensity lumbar extensor strengthening program is little better than a low-intensity program or a waiting list control group for chronic low back pain: a randomised clinical trial. Aust J Physiother. 2008;54(1):23–31.
Jørgensen MB, Ektor-Andersen J, Sjøgaard G, Holtermann A, Søgaard K. A randomised controlled trial among cleaners-effects on strength, balance and kinesiophobia. BMC Public Health. 2011;11(1):776.
Karahan AY, Sahin N, Baskent A. Comparison of effectiveness of different exercise programs in treatment of failed back surgery syndrome: a randomized controlled trial. J Back Musculoskelet Rehabil. 2017;30(1):109–20.
Lee J, Lee M, Lim T, Kim T, Kim S, Suh D, et al. Effectiveness of an application-based neck exercise as a pain management tool for office workers with chronic neck pain and functional disability: a pilot randomized trial. Eur J Integr Med. 2017;12:87–92.
Klaber Moffett JA, Carr J, Howarth E. High fear-avoiders of physical activity benefit from an exercise program for patients with back pain. Spine J. 2004;29(11):1167–72.
Storheim K, Brox JI, Holm I, Koller AK, Bo K. Intensive group training versus cognitive intervention in sub-acute low back pain: short-term results of a single-blind randomized controlled trial. J Rehabil Med. 2003;35(3):132–40.
Boutevillain L, Dupeyron A, Rouch C, Richard E, Coudeyre E. Facilitators and barriers to physical activity in people with chronic low back pain: a qualitative study. PLoS ONE. 2017;12(7):e0179826.
Nijs J, Girbés EL, Lundberg M, Malfliet A, Sterling M. Exercise therapy for chronic musculoskeletal pain: innovation by altering pain memories. Man Ther. 2015;20(1):216–20.
Zusman M. Mechanisms of musculoskeletal physiotherapy. Phys Ther Rev. 2004;9(1):39–49.
Tucker K, Larsson A-K, Oknelid S, Hodges P. Similar alteration of motor unit recruitment strategies during the anticipation and experience of pain. Pain. 2012;153(3):636–43.
Smith BE, Hendrick P, Bateman M, Holden S, Littlewood C, Smith TO, et al. Musculoskeletal pain and exercise—challenging existing paradigms and introducing new. Br J Sports Med. 2019;53(14):907–12.
Tagliaferri SD, Miller CT, Ford JJ, Hahne AJ, Main LC, Rantalainen T, et al. Randomized trial of general strength and conditioning versus motor control and manual therapy for chronic low back pain on physical and self-report outcomes. J Clin Med. 2020;9(6):1726.
Tryon WW. Possible mechanisms for why desensitization and exposure therapy work. Clin Psychol Rev. 2005;25(1):67–95.
Petruzzello SJ, Landers DM, Hatfield BD, Kubitz KA, Salazar W. A meta-analysis on the anxiety-reducing effects of acute and chronic exercise. Sports Med. 1991;11(3):143–82.
Chen Y-C, Chen C, Martínez RM, Etnier JL, Cheng Y. Habitual physical activity mediates the acute exercise-induced modulation of anxiety-related amygdala functional connectivity. Sci Rep. 2019;9(1):1–12.
Linton SJ, Buer N, Vlaeyen J, Hellsing A-L. Are fear-avoidance beliefs related to the inception of an episode of back pain? A prospective study. Psychol Health. 2000;14(6):1051–9. https://doi.org/10.1080/08870440008407366.
Lüning Bergsten C, Lundberg M, Lindberg P, Elfving B. Change in kinesiophobia and its relation to activity limitation after multidisciplinary rehabilitation in patients with chronic back pain. Disabil Rehabil. 2012;34(10):852–8. https://doi.org/10.3109/09638288.2011.624247.
Acknowledgements
The authors thank Josh Defazio for his assistance in the project in screening of the titles/abstracts and full-texts. Scott Tagliaferri is supported by an Australian Government Research Training Program (RTP) Scholarship.
Author information
Authors and Affiliations
Contributions
Secured funding: NA; Study conception: Belavy, Donath, Owen, Miller; Screening: Held, Defazio; Extraction: Hanel, Held; Statistical analyses: Hanel, Owen, Tagliaferri; Drafted manuscript: Hanel; Revised manuscript for intellectually important content: Owen, Held, Tagliaferri, Miller, Donath, Belavy; Approved final manuscript: All.
Corresponding author
Ethics declarations
Funding
No funding was received for the performance of this work.
Conflict of interest
The authors declare no conflicts of interest.
Availability of Data and Material
The data extracted as part of this systematic review and used in subsequent analysis is made available in Table 1.
Code Availability (Software Application or Custom Code)
Not applicable.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hanel, J., Owen, P.J., Held, S. et al. Effects of Exercise Training on Fear-Avoidance in Pain and Pain-Free Populations: Systematic Review and Meta-analysis. Sports Med 50, 2193–2207 (2020). https://doi.org/10.1007/s40279-020-01345-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-020-01345-1