Abstract
Background
Evidence-based data are required to provide insightful information on the timing of rehabilitation after lumbar spine surgery (LSS).
Objectives
The aim of this study is to systematically review the outcomes of early rehabilitation interventions and conduct its meta-analysis in patients after LSS.
Patients and methods
A total of 1183 articles were retrieved through PubMed (n = 793), Web of Science (n = 721), Scopus (n = 335), and ScienceDirect (n = 83) databases. Fourteen studies were included in the systematic review. The quality analysis and risk of bias assessment of the trials included in the systematic review were performed using the Physiotherapy Evidence Database (PEDro) scoring and classification system. Narrative synthesis and standardized mean difference based pooling results were given for the systematic review and meta-analysis, respectively.
Results
The additional benefit of early rehabilitation on physical function was moderately effective (ES: − 0.62, 95% CI − 1.00; − 0.25) at the 1-month follow-up. In terms of pain, early rehabilitation provided additional improvement at 1 month (ES: 0.34, 95% CI − 0.03; 0.71), 3 months (ES: − 0.14, 95% CI − 0.37; 0.10), 6 months (ES: 0.35, 95% CI 0.04; 0.65) and 1 year (ES: 0.21, 95% CI − 0.09; 0.52) follow-up at a low level of evidence.
Conclusions
This systematic review demonstrated that early rehabilitation mainly improved disability in the early period (1-month follow-up). Regarding pain, short-term (1 month) and mid-term (6 months) follow-ups showed the most significant additional benefit. The positive effects of starting rehabilitation early after surgery on pain may have positively affected disability, specifically in the early period (1 month).
Similar content being viewed by others
Background
The diagnosis of degenerative lumbar spinal stenosis and back pain has increased over time due to longer life expectancies, the desire for a higher quality of life, awareness of the condition, and the availability of cutting-edge imaging tools. Patients with severe lower back pain who do not respond to nonsurgical treatments for 3–6 months frequently have lumbar spine surgery (LSS) [1]. LSS is widespread in the older population and is becoming more common as the average lifespan rises [2]. Lumbar spinal fusion has emerged as the most widely utilized surgical procedure, with a rate of 13.8% for degenerative disk disease due to its superiority in terms of effectiveness [3, 4].
The typical success rate for lumbar spine procedures regarding capacity to work, neurological symptoms, and leg/back diskomfort is between 45 and 72% and reported satisfactory clinical outcomes to range from 16 to 95% [5, 6]. Questionnaires on patients’ expectations after LSS demonstrated that pain reduction and better mobility are the most expected results [7]. Numerous studies have demonstrated the efficacy of rehabilitation as the primary treatment for low back pain. However, research has demonstrated that rehabilitation after LSS is preferable to only rehabilitation including non-operative treatment but remains unclear, whereas a recent systematic review concluded that surgery might be more efficacious than unstructured care but may not be more efficacious than structured cognitive-behavioral therapy [8].
A recent meta-analysis demonstrated that standard treatment after lumbar fusion surgery does not significantly reduce disability and pain at 6 months compared to rehabilitation that combines an exercise program with cognitive behavioral therapy. Additionally, multimodal rehabilitation, which incorporates exercise therapy and cognitive behavioral training, is more effective than exercise therapy alone at reducing disability and pain-related fear [9, 10]. The most common specialized exercises are the Williams and McKenzie exercise regimens, floor exercises with the exercise ball or band, co-contraction for the transversus abdominus/multifidus muscles, and lumbopelvic stabilization. These exercise routines have been found to be both short- and long-term beneficial concerning low back issues such as persistent pain, lumbar spinal stenosis, and lumbar disk degeneration [11, 12]. According to a recent systematic review and meta-analysis, rehabilitation that includes cognitive therapy or counseling while the patient participates in an activity program has better results than exercise-only rehabilitation for lumbar fusion surgery [13].
The timing of the rehabilitation therapy is a crucial consideration. A study showed that ambulation within 8 h after elective cervical and LSS improved outcomes such as less complication rate, shorter hospital stays, lower 90-day readmission, and lower urinary retention rate compared to the patients who ambulated between 8 and 24 h [14]. Systematic reviews have demonstrated the significance of the timing of rehabilitation following procedures other than LSS. For instance, early rehabilitation following spinal cord injury was related to better functional outcomes and shorter hospital stays, according to a recent review [15]. Additionally, Greenwood et al.'s comprehensive review and meta-analysis showed that rehabilitation reduces short- and long-term impairment and fear avoidance behavior after lumbar fusion surgery. However, the effect of early rehabilitation after LSS has not been thoroughly evaluated [16].
More evidence-based data for better patient outcomes in rehabilitation practice would emerge from a systematic review and meta-analysis that provides insightful information on the timing of rehabilitation after lumbar spine surgery (LSS). To date, no systematic review has focused on the effectiveness of early rehabilitation after LSS. Additionally, a more thorough evaluation is required to highlight existing exercise alternatives and rehabilitation strategies that do not involve exercises that can be performed throughout the postoperative period of lumbar surgeries.
Aim of the work
The aim of this study is to systematically review the outcomes of early rehabilitation interventions and conduct its meta-analysis in patients after LSS.
Patients and methods
Search strategy
"Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA)" and "Cochrane Handbook for Systematic Reviews of Interventions" guidelines were considered for the methodological design of the review [17, 18]. Between November 2022 and January 2023, the literature search was performed through PubMed, Web of Science, Scopus and ScienceDirect databases with the specific keywords presented in “Appendix”. The "Medical Subject Headings (MeSH)" database was used to identify keywords. The terms "Lumbar surgery", "Early rehabilitation", "Enhanced rehabilitation", "Accelerated rehabilitation", and "Fast-track rehabilitation" were combined with Boolean operators to focus on studies concentrating on early rehabilitation after LSS. The search was performed independently by two separate researchers of the study.
Eligibility criteria
Before the screening procedures, the study's investigators determined the inclusion and exclusion criteria to ensure that the studies included in the systematic review had a more homogeneous sample and methodology. Inclusion criteria for the review were: (1) studies focusing on the effectiveness of early rehabilitation after LSS, (2) studies with a randomized controlled design. Exclusion criteria for the review: (1) studies focusing on the efficacy of rehabilitation before LSS, (2) studies with other non-randomized controlled research designs and designs, (3) articles published in a language other than English, (4) duplicate publications, (5) publications for which the full text was not available, (6) studies focusing on the efficacy of medical interventions other than rehabilitation after surgery.
Study selection and data extraction
The datasets containing the independent searches of two researchers were imported into Rayyan (QCRI, Qatar) software. Rayyan is a practical and automated article management tool for systematic reviews. Owing to this software, duplicate records can be detected automatically [19]. On the other hand, it is possible to manually mark the inclusion of trials in the review with "yes", "no", and "maybe" commands on the title/summary.
The two investigators who performed the screening evaluated the trials' eligibility by considering the study's inclusion/exclusion criteria through the Rayyan software. When two investigators disagreed on trial selection, a consensus was reached by considering the opinion of an experienced investigator who is an expert in the field of neurosurgical rehabilitation and knowledgeable about the systematic review methodology. The CONSORT flowchart of the systematic review is presented in Fig. 1. "Author, purpose, gender, sample, sample size, intervention, assessment and outcomes sections of the included studies were recorded (Table 1).
Quality and risk of bias assessment
The quality analysis and risk of bias assessment of the trials included in the systematic review were performed using the Physiotherapy Evidence Database (PEDro) scoring and classification system. The primary purpose of selecting the PEDro tool was to include specific items to audit the design of trials, including rehabilitation interventions. PEDro scoring was performed independently by the two investigators of the study. In case of disagreement, a consensus was achieved by obtaining the opinion of a third expert academic. PEDro addresses the level of evidence of the trials with 11 items, including eligibility criteria, random allocation, concealed allocation, baseline comparability, blind subjects, blind therapists, blind assessors, adequate follow-up, intention-to-treat analysis, between-group comparisons, point estimates and variability. Both items are scored with "Yes" (1-point) or "No" (0-point). The first question (eligibility criteria) is not included in the scoring. PEDro scores are classified as "excellent (9–10 points)", "good (6–8 points)", "moderate (4–5 points)", and "poor (0–3 points)". The validity and reliability of PEDro have been demonstrated [20].
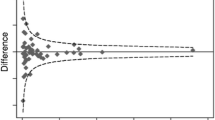
Evidence synthesis and meta-analysis
The review results were presented, considering the principles of narrative synthesis when pooling was not possible. The procedures of "developing a preliminary synthesis, exploring relationships within and between studies, and determining the synthesis's robustness" were regarded during the synthesis. Then, the results were shown, considering the qualitative and quantitative characteristics of the trials. In the meta-analysis section, numerical data on pooling were presented. Meta-Mar software (Philipps-Universität Marburg, Germany) calculated effect size and associated statistics [28]. The "Standardized Mean Difference (SMD)" was calculated regarding the "mean, standard, and sample size" of the relevant pooled parameter. Unknown standard deviation and confidence interval values were calculated according to the "Cochrane Handbook" guidelines [17]. "SMD, CI, weighted average effect size and p-value" values were given for each parameter pooled for meta-analysis. The heterogeneity of the measurements was analyzed with "I2, Tau2, and Chi2". Meta-analysis results were schematized with Forest plots.
Results
A total of 1183 articles were retrieved through PubMed (n = 793), Web of Science (n = 721), Scopus (n = 335), and ScienceDirect (n = 83) databases. Fourteen studies were included in the systematic review. After excluding duplicate and irrelevant studies for systematic review, 37 articles were analyzed according to the eligibility criteria. We excluded 24 studies that did not meet the eligibility criteria. Finally, 13 studies were included in the systematic review (Fig. 1).
Quality analysis and risk of bias results
The median score calculated for the PEDro total score of the 13 studies included in the systematic review was 5 (range = 3–8) [22,23,24,25, 29,30,31,32,33,34,35,36,37]. According to the PEDro classification, there were 5 "good" [24, 25, 29, 31, 34], 6 "moderate" [22, 23, 30, 33, 35, 37], and 2 "poor" [32, 36] evidence-level studies. All studies provided details on eligibility criteria and random allocation [22,23,24,25, 29,30,31,32,33,34,35,36,37]. Seven studies stated that allocations were concealed [23,24,25, 29, 31, 33, 34]. Most studies (nine) provided information on the homogeneity of the groups in terms of baseline comparability for assessment parameters [23,24,25, 29,30,31, 34,35,36]. None of the studies mentioned the identity of "therapists and subjects". Only three studies reported that the assessors were blind [24, 31, 35]. Nine studies reported appropriate monitoring procedures [22, 25, 29,30,31,32, 34, 36, 37]. Two studies calculated the intention-to-treat analysis [25, 29]. Only one study did not provide data on between-group comparison [36], point estimates and variability (e.g., intergroup comparison, SD, CI) [32]. Regarding items, the median value for total scores calculated from the scores of 14 studies was 9. Accordingly, items 3, 5, 6, 7, and 9 were below the median value (Table 2).
Study characteristics
A total of 1658 patients were available in 13 studies included in the systematic review [22,23,24,25, 29,30,31,32,33,34,35,36,37]. Four studies included Lumbar Microdiskectomy [22, 24, 35, 36], 3 Lumbar Fusion Surgeries [23, 29, 34], 2 Lumbar disk Herniation Surgeries [25, 32], one Microsurgical Lumbar disk Herniation [31], one study included "Lumbar Microdiskectomy or Percutaneous Endoscopic diskectomy", one "Percutaneous Transforaminal Endoscopic diskectomy [30] and one Robot-Assisted Minimally Invasive" and "Minimally Invasive Internal Lumbar Spine Fixation" [33]. All the studies focused on the effectiveness of early rehabilitation. Ten ODI, 9 VAS, 3 SF-36, 2 BDI, EQ-5D, 2 FABQ, two muscle strength and one each 50 Foot Walking Test, 6MWT, BBQ, BI, Complication Rates, Reliability/Expectation Questionnaire, Multifidus and Longissimus Muscle Cross Sectional Area (mm2), CSQ, CST, Early Retirement, EQ-5D-3L, Global Perceived Impact Scale, Health Care and Productivity Costs (euros), Intraabdominal Pre-Activation Pattern (seconds) Long Term Curative Effects (Excellent/Good/Bad), Lordosis index (MRI), Lumbar curvature (MRI), Lumbar Function Scale, Orebro Musculoskeletal Pain Screening Questionnaire, Pain Coping Inventory, Patients' 1st and 4th and 4. Days (Complete/Partial/Non-Compliant), Postoperative Conditions (Drainage Time, Time from Placement to Removal of Surgical Plasma Drainage Tube, Time to Lying on the Floor for the First Time After Surgery, Time from Completion of Surgery to Return to the Ward, Time to Get Out of Bed and Standing on Lumbar Support; Time of Postoperative Hospitalization, Time from Completion of Surgery to diskharge.), PSFS, QALY, Questionnaire (Remaining Sciatica, Sick Leave Days, Questionnaire (Working Status, Sick Leave, External Healthcare Use, Analgesic Use, Treatment Satisfaction, Frequency of Education and Reoperation Rates), Percentage Return to Work Questionnaire (%), Return to Work Rate, Return to Work (weeks), Roland's Disability Questionnaire, Sacral Tilt Angle (MRI), Satisfaction with Procedure), SES, Short Form McGill Pain Questionnaire, Less than 12, Short-Term Curative Effects (Excellent/Good/Bad), Spinal Stability (Lateral X-Ray), SRH (Table 1) [22,23,24,25, 29,30,31,32,33,34,35,36,37].
Quantitative synthesis results
Regarding pain parameters evaluated by VAS, the advantage of early rehabilitation (min 3 months, max 1 year) was emphasized in 5 of 9 studies [24, 29,30,31, 34]. Four studies emphasized that early rehabilitation did not contribute more to pain (min 1 month, max 7 years) [22, 33, 35, 36]. Four of the nine studies that evaluated ODI-based physical function reported that early rehabilitation (min 3 months, maximum 1 year) provided significantly more improvement [23, 24, 29, 34]. Five studies reported no additional benefit from early initiation of rehabilitation (min 1 week, max 3 years) [22, 25, 30, 33, 36]. Most of the studies (four) reported that early rehabilitation had no additional positive effect on quality of life. Two studies showed that early rehabilitation did not positively affect depression and fear avoidance beliefs [29, 35, 36]. Detailed results of the studies are presented in Table 1.
Meta-analysis results
Of the seven homogeneous studies, five evaluated pain evaluated by VAS [25, 29, 31, 33, 36], six assessed function by ODI [23,24,25, 29, 33, 36], and 3 included quality of life measurement by EQ-5D and SF-36 [23, 24, 29]. The additional benefit of early rehabilitation on physical function was moderately effective (ES: − 0.62, 95% CI − 1.00; − 0.25) at the 1-month follow-up. However, at 3 months (ES: 0.06, 95% CI − 0.17; 0.29), 6 months (ES: 0.09, 95% CI − 0.15; 0.33) and 1 year (ES: 0.08, 95% CI − 0.21; 0.37) follow-up, the contribution of early rehabilitation to physical function was at a low level of evidence. In terms of pain, early rehabilitation provided additional improvement at 1 month (ES: 0.34, 95% CI − 0.03; 0.71), 3 months (ES: − 0.14, 95% CI − 0.37; 0.10), 6 months (ES: 0.35, 95% CI 0.04; 0.65) and 1 year (ES: 0.21, 95% CI − 0.09; 0.52) follow-up at a low level of evidence. Finally, early rehabilitation was found to have a small effect size at 3 months (mental component) (ES: 0.13, 95% CI − 0.20; 0.47) and 1 year (general quality of life) (ES: − 0.04, 95% CI − 0.33; 0.25) follow-up (Figs. 2, 3, 4).
Discussion
This systematic review demonstrated that early rehabilitation mainly improved disability in the early period (1-month follow-up). Regarding pain, short-term (1 month) and mid-term (6 months) follow-ups showed the most significant additional benefit. There is insufficient evidence for the effectiveness of early rehabilitation in terms of quality of life and psychosocial status. The positive effects of starting rehabilitation early after surgery on pain may have positively affected disability, specifically in the early period (1 month). Future trials should elaborate on which types of exercises may be more effective in early rehabilitation.
In the early period, muscle strength, activities of daily living training, core stabilization, balance and gait training can provide more gains in the physical functions of individuals after lumbar surgery [13, 26]. In addition, earlier progress in joint range of motion may lead to less disability. Rehabilitation practices aimed at reducing pain after lumbar spine surgery may contribute more to improving function [16]. However, excessive training on the range of motion in the early period may cause an increase in the pain level of individuals. On the other hand, it is also comprehended that individuals have few gains in disability levels due to avoidance of functionality, fear of movement, and increased fear-avoidance beliefs to avoid pain [38, 39]. In this respect, our meta-analysis is unique to emphasize the gains in pain and function more clearly. In particular, we interpreted that improvement in early disability may be due to improvement in early and mid-term pain because the effect size in individuals' mid- and long-term functional improvements was low. However, since psychological and social multidimensional parameters (kinesiophobia, fear-avoidance, compliance, satisfaction) may affect physical function, more comprehensive psychosocial evaluations should be evaluated in future trials.
Analyzing the quality and bias risk of the studies
The median quality score of the studies included in the systematic review was moderate. Failure to mention the allocation procedure in some of the studies may have increased the risk of bias. However, the lack of blinding primarily decreased the methodologic quality. The fact that therapists and patients were not blinded in any study may suggest intervention bias. The use of assessor blinding in only three studies may suggest a suspicion of outcome bias. However, it should be emphasized that the effect of assessor bias is weakened when considering that most measurements were patient-reported outcome measures. Especially in studies with sensitive measurements such as muscle strength and physical performance tests, it should be emphasized that assessor blinding will reduce the risk of bias in order to ensure protocol integrity. Future studies should consider CONSORT or STROBE procedures regarding bias and randomization procedures [21, 40, 41].
Analyzing study characteristics
The types of surgery in the enrolled studies varied. In this respect, it should be considered that the difference in surgical procedures may have partially influenced the results regarding the rehabilitation procedure. The most commonly used surgical technique appears to be lumbar microdiskectomy [22, 24, 35, 36]. This finding suggests that especially minimally invasive methods are in the majority, and this advantageous situation for rehabilitation may produce more efficient results in terms of early rehabilitation.
The most preferred assessments in the studies are function and pain with ODI and VAS, respectively. The ODI is the gold standard scale used for many years in evaluating the lumbar region. The validity and reliability of VAS in postoperative patient follow-up have been emphasized in detail [42, 43]. Another point to be mentioned about the characteristics of the studies is that evaluations with non-standardized questionnaires were performed in some studies. Since the validity and reliability of non-standardized instruments have not been established, the consistency and responsiveness of the results are questionable [27]. On the other hand, the absence of studies addressing quality of life, psychosocial status, objective clinical measurements, and heterogeneous methodologies is indicative.
Effectiveness of the early exercise interventions
Pain
In more than half of the studies that addressed pain with VAS, the additional contribution of early rehabilitation was emphasized at follow-up from 3 months to 1 year [24, 29,30,31, 34]. In the meta-analysis, the pain was effective at a low-moderate level of evidence at 1- and 6-months follow-up [25, 29, 31, 33, 36]. In one study, early rehabilitation did not provide more effective results than the control group at a 6-month follow-up regarding pain assessed with the Örebro Musculoskeletal Pain Screening Questionnaire [25]. Early gains in terms of pain may also positively affect the disability levels of individuals. In this respect, the additional improvement gained at the 1-month follow-up suggests the effect of early rehabilitation on individuals regaining their physical functions in the early period. Considering that individuals complain of more pain in the acute period after lumbar spine surgery, short-term pain gain makes early rehabilitation advantageous. On the other hand, the maintenance of similar improvements in pain in the 6 months confirms the advantage of early rehabilitation in terms of pain in the medium term.
Disability
The most apparent gain in physical function was observed in the early period (1-month follow-up) with moderate evidence [33, 36]. Early rehabilitation efficacy was not noticed at an adequate level of evidence in later periods. Four of the studies evaluating physical function with ODI emphasized the superiority of early rehabilitation for a disability [23, 24, 29, 34], while the other five studies reported no additional contribution [22, 25, 30, 33, 36]. A study reporting the evaluation results with the Lumbar Function Scale reported the advantage of early rehabilitation [37]. The fact that improvements in physical function were reported only in the early period may be due to decreased pain in the early period. Although there is no additional advantage for individuals to start rehabilitation early in the middle and late periods, it may be valuable in clinical practice for secondary parameters such as independence in daily life and the shortening of hospitalization in the early period.
Quality of life and psychosocial status
According to the systematic review results, most studies noticed no additional contribution of rehabilitation to quality of life [29, 35, 36]. Meta-analysis results also supported these findings with a low effect size [23, 24, 29]. Since it is understood that gains in quality of life may occur in the long term, early rehabilitation was interpreted as usual when pain and disability outcomes were considered. It should be noted that long-term gains in disability and pain are similar in quality of life.
Psychological status is related to pain and the general condition of individuals. Studies showed that early rehabilitation did not positively affect depression and fear avoidance beliefs. Given the complex relationship of psychological state with other parameters such as pain, disability, satisfaction, complexity, kinesiophobia and heterogeneous study designs, it is difficult to make precise predictions. Future studies should focus more on secondary psychological parameters such as patient-oriented satisfaction and kinesiophobia [38, 39].
Study limitations
Some databases (e.g., EMBASE) could not be searched because the authors did not have access. Non-standardized assessment tools in the studies may have provided some results of questionable validity and reliability. The effects of surgical techniques on the study could not be addressed. Since 14 studies were included, an exclusion criterion related to the surgical procedure would have reduced the number of studies included in the meta-analysis, reducing the efficiency of effect size analyzes. However, the possible effect of surgical procedures may be a limitation affecting the study results. Finally, different rehabilitation protocols applied within the scope of early rehabilitation may suggest heterogeneity in the studies considered in pooling analyzes.
Conclusions
This systematic review demonstrated that early rehabilitation mainly improved disability in the early period (1-month follow-up). Regarding pain, short-term (1 month) and mid-term (6 months) follow-ups showed the most significant additional benefit. There is insufficient evidence for the effectiveness of early rehabilitation in terms of quality of life and psychosocial status. The positive effects of starting rehabilitation early after surgery on pain may have positively affected disability, specifically in the early period (1 month). Future trials should elaborate on which types of exercises may be more effective in early rehabilitation.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- SG:
-
Study group
- CG:
-
Control group
- F:
-
Female
- VAS:
-
Visual Analog Scale
- ODI:
-
Oswestry Disability Index
- SES:
-
Self-Efficacy Scale
- TSK:
-
Tampa Scale for Kinesiophobia
- BBQ:
-
Back Beliefs Questionnaire
- BI:
-
Barthel Index
- CSQ-CAT:
-
Catastrophizing Subscale of Coping Strategy Questionnaire
- CSQ-COP:
-
Coping strategies to control pain
- CSQ-ADP:
-
Coping strategies to decrease pain
- CCF-S:
-
Craniocervical flexion strength test
- CCF-E:
-
Craniocervical flexion endurance test
- DPQ:
-
Dallas Pain Questionnaire
- MPI:
-
Multidimensional Pain Inventory
- EQ-5D:
-
European Quality of Life Questionnaire
- BDI:
-
Beck Depression Index
- FABQ:
-
Fear-Avoidance Beliefs Questionnaire
- NPRS:
-
Numeric Pain Rating Scale
- PSFS:
-
Patient-Specific Functional Scale
- SF-36:
-
Short form health survey
- CST:
-
Chair stand test
- SRH:
-
Standing reach height test
- 6MWT:
-
6-Minute walking test
References
Gatchel RJ, Neblett R, Kishino N, Ray CT. Fear-avoidance beliefs and chronic pain. J Orthop Sports Phys Ther. 2016;46(2):38–43.
Turner JA, Ersek M, Herron L, Deyo R. Surgery for lumbar spinal stenosis: attempted meta-analysis of the literature. Spine. 1992;17(1):1–8.
Özden F. The effect of exercise interventions after lumbar decompression surgery: a systematic review and meta-analysis. World Neurosur. 2022.
Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1):S31.
Ilves O, Neva MH, Häkkinen K, Dekker J, Järvenpää S, Kyrölä K, et al. Effectiveness of a 12-month home-based exercise program on trunk muscle strength and spine function after lumbar spine fusion surgery: a randomized controlled trial. Disabil Rehabil. 2022;44(4):549–57.
Moseley AM, Herbert RD, Sherrington C, Maher CG. Evidence for physiotherapy practice: a survey of the Physiotherapy Evidence Database (PEDro). Aust J Physiother. 2002;48(1):43–9.
Abbott AD, Tyni-Lenné R, Hedlund R. Early rehabilitation targeting cognition, behavior, and motor function after lumbar fusion: a randomized controlled trial. LWW; 2010.
Greenwood J, McGregor A, Jones F, Mullane J, Hurley M. Rehabilitation following lumbar fusion surgery: a systematic review and meta-analysis. Spine. 2016;41(1):E28–36.
Souslian FG, Patel PD. Review and analysis of modern lumbar spinal fusion techniques. Br J Neurosurg. 2021;6:1–7.
Gibson JNA, Waddell G. Surgery for degenerative lumbar spondylosis: updated Cochrane review. Spine. 2005;30(20):2312–20.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. New York: Wiley; 2019.
Choi G, Raiturker PP, Kim M-J, Chung DJ, Chae Y-S, Lee S-H. The effect of early isolated lumbar extension exercise program for patients with herniated disk undergoing lumbar diskectomy. Neurosurgery. 2005;57(4):764–72.
Ogutluler Ozkara G, Özgen M, Ozkara E, Armagan O, Arslantaş A, Atasoy M. Effectiveness of physical therapy and rehabilitation programs starting immediately after lumbar disk surgery. Turk Neurosurg. 2015;25:3.
Beheshti A, Chavanon M-L, Christiansen H. Emotion dysregulation in adults with attention deficit hyperactivity disorder: a meta-analysis. BMC Psychiatry. 2020;20(1):1–11.
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. J Pharmacol Pharmacother. 2010;1(2):100–7.
Özden F. The effectiveness of physical exercise after lumbar fusion surgery: a systematic review and meta-analysis. World Neurosurg. 2022.
Sumida M, Fujimoto M, Tokuhiro A, Tominaga T, Magara A, Uchida R. Early rehabilitation effect for traumatic spinal cord injury. Arch Phys Med Rehabil. 2001;82(3):391–5.
Oosterhuis T, Ostelo RW, van Dongen JM, Peul WC, de Boer MR, Bosmans JE, et al. Early rehabilitation after lumbar disk surgery is not effective or cost-effective compared to no referral: a randomized trial and economic evaluation. J Physiother. 2017;63(3):144–53.
Newsome R, May S, Chiverton N, Cole A. A prospective, randomized trial of immediate exercise following lumbar microdiskectomy: a preliminary study. Physiotherapy. 2009;95(4):273–9.
Danielsen JM, Johnsen R, Kibsgaard SK, Hellevik E. Early aggressive exercise for postoperative rehabilitation after diskectomy. LWW; 2000.
Donceel P, Du Bois M, Lahaye D. Return to work after surgery for lumbar disk herniation: a rehabilitation-oriented approach in insurance medicine. Spine. 1999;24(9):872–6.
He W, Wang Q, Hu J, Lin S, Zhang K, Wang F, et al. A randomized trial on the application of a nurse-led early rehabilitation program after minimally invasive lumbar internal fixation. Ann Palliat Med. 2021;10(9):9820–9.
Kernc D, Strojnik V, Vengust R. Early initiation of a strength training based rehabilitation after lumbar spine fusion improves core muscle strength: a randomized controlled trial. J Orthop Surg Res. 2018;13:1–8.
Kjellby-Wendt G, Carlsson SG, Styf J. Results of early active rehabilitation 5–7 years after surgical treatment for lumbar disk herniation. Clin Spine Surg. 2002;15(5):404–9.
LeBlanc L, Moldovan ID, Sabri E, Phan P, Agbi C, Mohammed S, et al. Comparing the effects of early versus late exercise intervention on pain and neurodynamic mobility following unilateral lumbar microdiskectomy: a pilot study. Spine. 2021;46(18):E998–1005.
Oestergaard LG, Christensen FB, Nielsen CV, Bünger CE, Fruensgaard S, Sogaard R. Early versus late initiation of rehabilitation after lumbar spinal fusion: economic evaluation alongside a randomized controlled trial. LWW; 2013.
Zhang R, Zhang S, Wang X. Postoperative functional exercise for patients who underwent percutaneous transforaminal endoscopic diskectomy for lumbar disk herniation. Eur Rev Med Pharmacol Sci. 2018;22(1 Suppl):15–22.
Ciol MA, Deyo RA, Howell E, Kreif S. An assessment of surgery for spinal stenosis: time trends, geographic variations, complications, and reoperations. J Am Geriatr Soc. 1996;44(3):285–90.
Siebert E, Prüss H, Klingebiel R, Failli V, Einhäupl KM, Schwab JM. Lumbar spinal stenosis: syndrome, diagnostics and treatment. Nat Rev Neurol. 2009;5(7):392–403.
Reisener M-J, Pumberger M, Shue J, Girardi FP, Hughes AP. Trends in lumbar spinal fusion—a literature review. J Spine Surg. 2020;6(4):752.
Ibrahim T, Tleyjeh I, Gabbar O. Surgical versus non-surgical treatment of chronic low back pain: a meta-analysis of randomized trials. Int Orthop. 2008;32:107–13.
Bogaert L, Thys T, Depreitere B, Dankaerts W, Amerijckx C, Van Wambeke P, et al. Rehabilitation to improve outcomes of lumbar fusion surgery: a systematic review with meta-analysis. Eur Spine J. 2022;31(6):1525–45.
Lim S, Bazydlo M, Macki M, Haider S, Hamilton T, Hunt R, et al. Validation of the benefits of ambulation within 8 hours of elective cervical and lumbar surgery: a michigan spine surgery improvement collaborative study. Neurosurgery. 2022;91(3):505–12.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88: 105906.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:1–10.
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–21.
Prinsen CA, Mokkink LB, Bouter LM, Alonso J, Patrick DL, De Vet HC, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27:1147–57.
Monticone M, Ferrante S, Teli M, Rocca B, Foti C, Lovi A, et al. Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomized controlled trial. Eur Spine J. 2014;23:87–95.
Fairbank JC, Pynsent PB. The Oswestry disability index. Spine. 2000;25(22):2940–53.
Markman JD, Gewandter JS, Frazer ME, Pittman C, Cai X, Patel KV, et al. Evaluation of outcome measures for neurogenic claudication: a patient-centered approach. Neurology. 2015;85(14):1250–6.
Vlaeyen JW, Kole-Snijders AM, Rotteveel AM, Ruesink R, Heuts PH. The role of fear of movement/(re) injury in pain disability. J Occup Rehabil. 1995;5:235–52.
Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr, Shekelle P, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–91.
Zanoli G, Strömqvist B, Jönsson B. Visual analog scales for interpretation of back and leg pain intensity in patients operated for degenerative lumbar spine disorders. Spine. 2001;26(21):2375–80.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors made a significant contribution to the work reported, whether that was in the conception, study design, execution, acquisition of data, analysis and interpretation; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agreed to be account- able for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors report no conflicts of interest and certify that no funding has been received for this study and/or preparation of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix: Keywords
Appendix: Keywords
Search strategy PubMed
Search ID# | Search terms | Search options |
|---|---|---|
S1 | Lumbar surgery AND Early rehabilitation | Boolean/Phrase |
S2 | Lumbar surgery AND Enhanced rehabilitation | Boolean/Phrase |
S3 | Lumbar surgery AND Accelerated rehabilitation | Boolean/Phrase |
S4 | Lumbar surgery AND Fast-track rehabilitation | Boolean/Phrase |
Search strategy web of science
Search ID# | Search terms | Search options |
|---|---|---|
S1 | Lumbar surgery AND Early rehabilitation | Boolean/Phrase |
S2 | Lumbar surgery AND Enhanced rehabilitation | Boolean/Phrase |
S3 | Lumbar surgery AND Accelerated rehabilitation | Boolean/Phrase |
S4 | Lumbar surgery AND Fast-track rehabilitation | Boolean/Phrase |
Search strategy Scopus
Search ID# | Search Terms | Search Options |
|---|---|---|
S1 | Lumbar surgery AND Early rehabilitation | Boolean/Phrase |
S2 | Lumbar surgery AND Enhanced rehabilitation | Boolean/Phrase |
S3 | Lumbar surgery AND Accelerated rehabilitation | Boolean/Phrase |
S4 | Lumbar surgery AND Fast-track rehabilitation | Boolean/Phrase |
Search strategy ScienceDirect
Search ID# | Search terms | Search options |
|---|---|---|
S1 | Lumbar surgery AND Early rehabilitation | Boolean/Phrase |
S2 | Lumbar surgery AND Enhanced rehabilitation | Boolean/Phrase |
S3 | Lumbar surgery AND Accelerated rehabilitation | Boolean/Phrase |
S4 | Lumbar surgery AND Fast-track rehabilitation | Boolean/Phrase |
Total result literature searches: 1183 references |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Özden, F., Koçyiğit, G.Z. The effect of early rehabilitation after lumbar spine surgery: a systematic review and meta-analysis. Egypt J Neurosurg 39, 8 (2024). https://doi.org/10.1186/s41984-024-00270-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-024-00270-z