Abstract
Purpose
Recognition of intraoperative hypovolemia is important for fluid management. Previous studies demonstrated functional preload parameter pulse pressure variation (PPV) could predict volume changes in response to fluid loading and loss. In this study, we examined the correlation between PPV and other two cardiac preload indicators, central venous pressure (CVP) or initial distribution volume of glucose (IDVG), in patients after anesthesia induction.
Methods
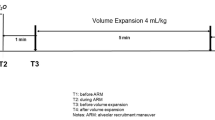
In 30 patients undergoing scheduled craniotomy surgery, we compared measurement of PPV (%) using the Ohmeda monitor method to simultaneously measure CVP and IDVG after anesthesia induction through correlation analysis and receiver operating characteristic (ROC) curves.
Results
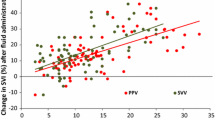
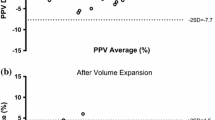
Pulse pressure variation has negative linear correlation with IDVG (r = −0.65, P < 0.01). IDVG values (n = 13) when PPV ≥ 11% showed a significant difference compared with those (n = 17) when PPV < 11% (P < 0.001). The ROC curve showed the best cutoff value of IDVG is 122 ml/kg, equivalent to the threshold of PPV (11%) for predicting fluid responsiveness. However, there is no significant correlation between CVP in normal ranges (4–9 mmHg) and PPV (r = −0.12, P > 0.05).
Conclusion
As an indicator of cardiac preload, PPV has a negative linear correlation with IDVG in patients after anesthesia induction. It does not correlate well with CVP in the normal range. Our results imply that an individual PPV, not CVP, is equivalent to IDVG in assessing volume status after induction.



Similar content being viewed by others
References
Boldt J, Lenz M, Kumle B, Papsdorf M. Volume replacement strategies on intensive care units: results from a postal survey. Intensive Care Med. 1998;24:147–51.
Ishihara H, Suzuki A, Okawa H, Sakai I, Tsubo T, Matsuki A. The initial distribution volume of glucose rather than indocyanine green derived plasma volume is correlated with cardiac output following major surgery. Intensive Care Med. 2000;26:1441–8.
Suzuki A, Ishihara H, Okawa H, Tsubo T, Matsuki A. Can initial distribution volume of glucose predict hypovolemic hypotension after radical surgery for esophageal cancer? Anesth Analg. 2001;92:1146–51.
Orban JC, Blasin-Chadoutaud A, Zolfaghari P, Ishihara H, Grimaud D, Ichai C. Hypovolaemic hypotension after abdominal aortic surgery is predicted by initial distribution volume of glucose. Eur J Anaesthesiol. 2010;27:364–8.
Hofer CK, Müller SM, Furrer L, Klaghofer R, Genoni M, Zollinger A. Stroke volume and pulse pressure variation for prediction of fluid responsiveness in patients undergoing off-pump coronary artery bypass grafting. Chest. 2005;128:848–54.
Kramer A, Zygun D, Hawes H, Easton P, Ferland A. Pulse pressure variation predicts fluid responsiveness following coronary artery bypass surgery. Chest. 2004;126:1563–8.
Pestel GJ, Hiltebrand LB, Fukui K, Cohen D, Hager H, Kurz AM. Assessing intravascular volume by difference in pulse pressure in pigs submitted to graded hemorrhage. Shock. 2006;26:391–5.
Mutoh T, Ishikawa T, Nishino K, Yasui N. Evaluation of the FloTrac uncalibrated continuous cardiac output system for perioperative hemodynamic monitoring after subarachnoid hemorrhage. J Neurosurg Anesthesiol. 2009;21:218–25.
Durga P, Jonnavittula N, Muthuchellappan R, Ramachandran G. Measurement of systolic pressure variation during graded volume loss using simple tools on Datex Ohmeda S/5 monitor. J Neurosurg Anesth. 2009;21:161–4.
Qiao H, Zhang J, Liang WM. Validity of pulse pressure and systolic blood pressure variation data obtained from a Datex Ohmeda S/5 monitor for predicting fluid responsiveness during surgery. J Neurosurg Anesthesiol. 2010;22:316–22.
Ishihara H, Shimodate Y, Koh H, Isozaki K, Tsubo T, Matsuki A. The initial distribution volume of glucose and cardiac output in the critically ill. Can J Anaesth. 1993;40:28–31.
Hirota K, Ishihara H, Tsubo T, Matsuki A. Estimation of the initial distribution volume of glucose by an incremental plasma glucose level at 3 min after i.v. glucose in humans. Br J Clin Pharmacol. 1999;47:361–4.
Bamboat ZM, Bordeianou L. Perioperative fluid management. Clin Colon Rectal Surg. 2009;22:28–33.
Cannesson M. Arterial pressure variation and goal-directed fluid therapy. J Cardiothorac Vasc Anesth. 2010;24:487–97.
Jacob M, Chappell D, Conzen P, Finsterer U, Rehm M. Blood volume is normal after pre-operative overnight fasting. Acta Anaesthesiol Scand. 2008;52:522–9.
Brock H, Rapf B, Necek S, Gabriel C, Peterlik C, Pölz W, Schimetta W, Bergmann H. Vergleichende untersuchungen zur postoperativen volumentherapie bei kardiochirurgischen patienten. Anaesthesist. 1995;44:486–92.
Shippy CR, Appel PL, Shoemaker WL. Reliability of clinical monitoring to assess blood volume in critically ill patients. Crit Care Med. 1984;12:107–12.
Sakka SG, Bredle DL, Reinhart K, Meier-Hellmann A. Comparison between intrathoracic blood volume and cardiac filling pressures in the early phase of hemodynamic instability of patients with septic shock. J Crit Care. 1999;14:78–83.
Kumar A, Anel R, Bunnell E, Habet K, Zanotti S, Marshall S, Neumann A, Ali A, Cheang M, Kavinsky C, Parrillo JE. Pulmonary artery occlusion pressure and central venous pressure fail to predict ventricular filling volume, cardiac performance, or the response to volume infusion in normal subjects. Crit Care Med. 2004;32:691–9.
Marik PE. Techniques for assessment of intravascular volume in critically ill patients. J Intensive Care Med. 2009;24:329–37.
Cavallaro F, Sandroni C, Antonelli M. Functional hemodynamic monitoring and dynamic indices of fluid responsiveness. Minerva Anestesiol. 2008;74:123–35.
Wyffels PA, Sergeant P, Wouters PF. The value of pulse pressure and stroke volume variation as predictors of fluid responsiveness during open chest surgery. Anaesthesia. 2009;65:704–9.
Biais M, Bernard O, Ha JC, Degryse C, Sztark F. Abilities of pulse pressure variations and stroke volume variations to predict fluid responsiveness in prone position during scoliosis surgery. Br J Anaesth. 2010;104:407–13.
Bliacheriene F, Machado SB, Fonseca EB, Otsuke D, Auler JO Jr, Michard F. Pulse pressure variation as a tool to detect hypovolaemia during pneumoperitoneum. Acta Anaesthesiol Scand. 2007;51:1268–72.
Kubitz JC, Forkl S, Annecke T, Kronas N, Goetz AE, Reuter DA. Systolic pressure variation and pulse pressure variation during modifications of arterial pressure. Intensive Care Med. 2008;34:1520–4.
Marik PE, Cavallazzi R, Vasu T, Hirani A. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med. 2009;37:2642–7.
Fujita Y, Yamamoto T, Sano I, Yoshioka N, Hinenoya H. A comparison of changes in cardiac preload variables during graded hypovolemia and hypervolemia in mechanically ventilated dogs. Anesth Analg. 2004;99:1780–6.
Cannesson M, Slieker J, Desebbe O, Bauer C, Chiari P, Hénaine R, Lehot JJ. The ability of a novel algorithm for automatic estimation of the respiratory variations in arterial pulse pressure to monitor fluid responsiveness in the operating room. Anesth Analg. 2008;106:1195–200.
Umbrello M, Formenti P, Galimberti A, Curti M, Zaniboni M, Iapichino G. On-line measurement of systolic pressure variation and pulse pressure variation on a multiparametric monitor. Intensive Care Med. 2008;34:386–7.
Deflandre E, Bonhomme V, Hans P. Delta down compared with delta pulse pressure as an indicator of volaemia during intracranial surgery. Br J Anaesth. 2008;100:245–50.
Ishihara H, Takamura K, Iwakawa T, Tsubo T, Matsuki A. Does the initial distribution of glucose reflect the central ECF volume status in critically ill patients? Infusionther Transfus Med. 1996;23:196–201.
Gabbanelli V, Pantanetti S, Donati A, Montozzi A, Carbini C, Pelaia P. Initial distribution volume of glucose as noninvasive indicator of cardiac preload: comparison with intrathoracic blood volume. Intensive Care Med. 2004;30:2067–73.
Nakamura H, Ishihara H, Okawa H, Yatsu Y, Tsubo T, Matsuki A. Initial distribution volume of glucose is correlated with intrathoracic blood volume in hypovolaemia and following volume loading in dogs. Eur J Anaesthesiol. 2005;22:202–8.
Ishihara H, Nakamura H, Okawa H, Yatsu Y, Tsubo T, Hirota K. Comparison of initial distribution volume of glucose and intrathoracic blood volume during hemodynamically unstable states early after esophagectomy. Chest. 2005;128:1713–9.
Harvey M, Voss L, Sleigh J. Preload response in patients after cardiac surgery: a comparison of systolic blood pressure and systolic area variability and initial volume of distribution of glucose. Crit Care Resusc. 2003;5:171–6.
Ishihara H. Initial distribution volume of glucose early after cardiac surgery. Anesth Analg. 2006;102:1904.
Monnet X, Teboul JL. Volume responsiveness. Curr Opin Crit Care. 2007;13:549–53.
Haruna M, Kumon K, Yahagi N, Watanabe Y, Ishida Y, Kobayashi N, Aoyagi T. Blood volume measurement at the bedside using ICG pulse spectrophotometry. Anesthesiology. 1998;89:1322–8.
van Tulder L, Michaeli B, Chioléro R, Berger MM, Revelly JP. An evaluation of the initial distribution volume of glucose to assess plasma volume during a fluid challenge. Anesth Analg. 2005;101:1089–93.
Rose BO, Ishihara H, Okawa H, Panning B, Piepenbrock S, Matsuki A. Repeatability of measurements of the initial distribution volume of glucose in haemodynamically stable patients. J Clin Pharm Ther. 2004;29:317–23.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
He, Z., Qiao, H., Zhou, W. et al. Assessment of cardiac preload status by pulse pressure variation in patients after anesthesia induction: comparison with central venous pressure and initial distribution volume of glucose. J Anesth 25, 812–817 (2011). https://doi.org/10.1007/s00540-011-1225-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-011-1225-1