Abstract
Objective: To assess volume replacement strategies on intensive care units (ICUs) in Germany.
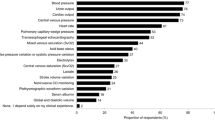
Design: A postal survey questionnaire of 18 questions was sent to 451 ICUs in Germany. The questionnaire was sent to general, surgical, anesthesiology, neurosurgery, cardiac surgery, and medical ICUs of hospitals with more than 200 beds.
Results: 286 questionnaires (64 % ) were returned and analysed. Hydroxyethylstarch (HES) solution is the solution most often used for volume replacement (total: 193 ICUs, exclusively HES: 93 ICUs), crystalloids are next (crystalloids exclusively: 61 ICUs), and human albumin is used rarely as a first choice. Clinical experience is a very important argument for administering volume. Diagnostic tools, e. g. measurement of central venous pressure or pulmonary capillary wedge pressure, also play an important role. Albumin/total protein and colloid osmotic pressure (COP) are measured often on ICUs (albumin measured routinely: 173 ICUs; COP measured routinely: 33 ICUs). Critical values for albumin/total protein are defined in most ICUs. Reduced plasma levels of albumin/total protein was the indication most often cited for administering human albumin. Only 149 ICUs (52%) have a financial budget for their unit. Costs still do not play a major role in the choice of volume replacement on 30 ICUs (10%).
Conclusions: The kind of volume therapy differs widely among the different ICUs. This questionnaire supported the supposition that no standards exist for volume therapy in intensive care patients. New results concerning the abuse of albumin in the critically ill have not yet influenced strategies of volume replacement.
Similar content being viewed by others
Change history
12 April 2023
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1007/s00134-023-07058-z
References
Sibbald WJ (1994) Fluid therapy in sepsis. In: Reinhart K, Eyrich K, Sprung C (eds) Sepsis — current perspectives in pathophysiology and therapy. (Update in intensive care and emergency medicine, vol 18) Springer, Berlin Heidelberg New York, pp 266–273
Thijs LG (1995) Fluid therapy in septic shock. In: Sibbald WJ, Vincent JL (eds) Clinical trials for the treatment of sepsis. (Update in intensive care and emergency medicine, vol 19) Springer, Berlin Heidelberg New York, pp 167–190
Prough DS, Johnston WE (1989) Fluid restoration in septic shock: no solution yet. Anesth Analg 69: 699–704
Brinkmeyer S, Safar P, Motoyama E (1981) Superiority of colloids over electrolyte solution for fluid resuscitation (severe normovolemic hemodilution). Crit Care Med 9: 369–344
Davidson I (1989) Fluid resuscitation of shock: current controversies. Crit Care Med 17:1078–1080
Beards SC, Watt T, Edwards JD, Nightingale P, Farragher EB (1994) Comparison of the hemodynamic and oxygen transport responses to modified fluid gelatin and hetastarch in critically ill patients: a prospective, randomized trial. Crit Care Med 22: 600–605
Kapila A, Waldman CS, Uncles DR, Addy EV (1995) Survey of colloid usage in British intensive care units. Clin Intensive Care 6: A201
Grootendorst AF, van Wilgenburg MG, deLaat PH, van der Hoven B (1988) Albumin abuse in intensive care medicine. Intensive Care Med 14: 554–557
Stockwell MA, Scott A, Day A, Riley B, Soni N (1992) Colloid solutions in the critically ill. Anaesthesia 47: 3–9
McClusky A, Thomas AN, Bowles BJ, Kishen R (1996) The prognostic value of serial measurement of serum albumin concentration in patients admitted to an intensive care unit. Anaesthesia 51: 724–727
Blackburn GL, Discroll DF (1992) Time to abandon routine albumin supplementation. Crit Care Med 20: 157–158
Golub R, Sorrento J, Cantu R, Nierman DM, Moideen A, Stein HD (1994) Efficacy of albumin supplementation in the surgical intensive care unit: a prospective, randomized study. Crit Care Med 22:613–619
Foley EF, Borlasse DC, Dzik WH et al (1990) Albumin supplementation in the critically ill. A prospective, randomized trial. Arch Surg 125: 739–742
Guthrie RD, Hines C (1991) Use of intravenous albumin in the critically ill patient. Am J Gastroenterol 86: 255–263
Rubin H, Carlson S, DeMeo M, Ganger D, Craig RM (1997) Randomized, double-blind study of intravenous human albumin in hypoalbuminemic patients receiving total parenteral nutrition. Crit Care Med 25: 249–252
Finch JS, Reid C, Bandy K, Kickle D (1983) Compared effects of selected colloids on extravascular lung water in dogs after oleic acid induced lung injury and severe hemorrhage. Crit Care Med 11:267–270
Lucas CE, Ledgerwood AM, Higgins RF (1980) Impaired pulmonary function after albumin resuscitation from shock. J Trauma 20: 447–451
Strauss RG (1988) Volume replacement and coagulation: a comparative review. J Cardiothorac Anesth 2 [Suppl 1]: 24–32
Boldt J, Müller M, Heesen M, Heyn O, Hempelmann G (1996) Influence of different volume therapy on platelet function in the critically ill. Intensive Care Med 22:1075–1081
Collis RE, Collins PW, Gutteridge CN et al (1994) The effect of hydroxy ethyl starch and other plasma volume substitutes on endothelial cell activation; an in vitro study. Intensive Care Med 20: 37–41
Schmand JF, Ayala A, Chaudry IH (1994) Influence of hydroxyethylstarch (HES) on inflammatory cytokine release following trauma and hemorrhagic shock. Intensive Care Med 20: 325
Gold MS, Russo J, Tissot M, Weinhouse G, Riles T (1990) Comparison of hetastarch to albumin for perioperative bleeding patients undergoing abdominal aortic aneurysm surgery: a prospective, randomized study. Ann Surg 211: 482–485
Author information
Authors and Affiliations
About this article
Cite this article
Boldt, J., Lenz, M., Kumle, B. et al. RETRACTED ARTICLE: Volume replacement strategies on intensive care units: results from a postal survey. Intensive Care Med 24, 147–151 (1998). https://doi.org/10.1007/s001340050536
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s001340050536