Abstract
Purpose
Chemotherapy-induced nausea and vomiting (CINV) are common side effects in pediatric oncology treatment. Besides 5-HT3-antagonists, both dexamethasone and aprepitant are cornerstone drugs in controlling these side effects. Based on results of adult studies, the dexamethasone dose is reduced by 50% when combined with aprepitant, because of a drug-drug interaction, even though data on the interaction in children is lacking. The current study was developed to investigate the effect of aprepitant on dexamethasone clearance (CL) in children, in order to assess if dexamethasone dose reduction for concomitant use of aprepitant is appropriate in the current antiemetic regimen.
Methods
In total, 65 children (0.6–17.9 years), receiving intravenous or oral antiemetic therapy (dexamethasone ± aprepitant) as standard of care, were included. 305 dexamethasone plasma concentrations were determined using LC–MS/MS. An integrated dexamethasone and aprepitant pharmacokinetic model was developed using non-linear mixed effects modelling in order to investigate the effect of aprepitant administration on dexamethasone CL.
Results
In this population, dexamethasone CL in patients with concomitant administration of aprepitant was reduced by approximately 30% of the uninhibited CL (23.3 L/h (95% confidence interval 20.4–26.0)). This result is not consistent with the results of adult studies (50% reduction). This difference was not age dependent, but might be related to the route of administration of dexamethasone. Future studies are needed to assess the difference in oral/intravenous dexamethasone.
Conclusion
When dexamethasone is given intravenously as a component of triple therapy to prevent CINV in children, we advise to reduce the dexamethasone dose by 30% instead of 50%.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy-induced nausea and vomiting (CINV) are one of the most common side effects of pediatric oncology treatment. International guidelines for management and prevention of these side effects have been developed [1,2,3,4]. Different treatment levels are based on the emetogenicity classification of the Canadian Pediatric Oncology Group of Ontario [1, 5]. The overall backbone of antiemetic supportive care consist of a 5-HT3 receptor antagonist for low emetogenic chemotherapy, addition of dexamethasone for moderate emetogenic chemotherapy (MEC) and, for highly emetogenic chemotherapy (HEC), addition of the NK1 receptor antagonist, aprepitant.
Dexamethasone shows a bioavailability of approximately 86% after oral administration [6]. It is rapidly distributed and about 77% is bound to plasma proteins [7]. Dexamethasone is metabolized by cytochrome P450-3A4 (CYP3A4)[7], the elimination half-life is 3–6 h for adults which is higher in children or infants (3–8 h and 2–10 h, respectively) [8]. Aprepitant is administered orally and shows a bioavailability of 59–67%. Aprepitant is highly bound to plasma proteins (97%). The metabolism of aprepitant occurs mainly via oxidation and CYP3A4, and the half-life is 9–13 h in adults [9, 10]. Fosaprepitant is a water soluble prodrug, the intravenous formulation of aprepitant. Within 30 min after administration, fosaprepitant is converted to aprepitant, after which it shows similar pharmacokinetics (PK) [10].
Besides being a substrate for CYP3A4, (fos)aprepitant is a weak to moderate inhibitor of CYP3A4. (Fos)aprepitant therapy can result in higher plasma levels of CYP3A4 metabolized agents (e.g. dexamethasone). In adult studies, it has been shown that concurrent use of aprepitant resulted in lower dexamethasone clearances (CL) and a higher exposure to dexamethasone of approximately twofold, and thus, a 50% dexamethasone dose reduction is recommended [11,12,13,14]. However, for children, this reduction is based on extrapolation of adult data, and it is not known if the magnitude of this interaction is the same [15].
Moreover, despite standardized prophylaxis, children receiving HEC achieve 20–30% less CINV control compared to adults[16,17,18], which might be explained by suboptimal dexamethasone therapy, due to a possible different interaction in children compared to adults. (Fos)aprepitant and dexamethasone doses used in children are different than in adults, which could lead to a different magnitude of the interaction. Moreover, developmental changes occur over age (e.g. development of liver enzymes), which could lead to altered PK in young children [19].
In this study, we studied the effect of aprepitant on dexamethasone PK in pediatric oncology patients, in order to assess whether dexamethasone dose reduction for concomitant aprepitant use is appropriate in the current antiemetic regimen.
Methods
Patients, sampling, and bioanalysis
A prospective observational study was performed in Princess Máxima Center for Pediatric Oncology, the Netherlands. Patients aged 0.5–18 years with a new oncological diagnosis, having a central venous line, planned to receive chemotherapy with granisetron/ondansetron; dexamethasone and/or aprepitant as standard of care were screened for eligibility. Patients could be included twice: once for oral aprepitant and once for intravenous fosaprepitant, if applicable. Patients using strong CYP3A4-substrates and/or -inhibitors within 7 days or strong CYP3A4-inducers within 30 days before the start of antiemetic therapy were excluded (Supplementary Table S1). Patients with Down syndrome were excluded due to possible altered PK as compared to children without Down syndrome. Written informed consent was obtained prior to participation. Ethical approval by the institutional Medical Ethics Committee of the Erasmus MC was obtained. The study was registered in the Dutch Trial Registry as NTR7720.
Patients were treated with dexamethasone with (HEC) or without (MEC) (fos)aprepitant according to the antiemetic guidelines of the Dutch Childhood Oncology Group (Table 1). Blood samples of 1 mL were collected from the central venous line before and after administration of the antiemetics on day 1, 2, or 3. A pre-dose sample was taken when dexamethasone was administered in the previous 7 days. Post-dose, a maximum of six samples were taken over 24 h (Supplementary Table S2). The exact number of collected samples depended on the availability of the central venous line (especially in patients with a single lumen line and continuous chemotherapy infusions). Patients with at least one sample post-dose were included in the analysis.
Plasma samples were stored at − 80 °C until analyzation. Plasma concentrations of dexamethasone and aprepitant were measured using a validated liquid chromatography mass spectrometry method, with a lower limit of quantification (LLOQ) of 1 µg/L and 0.1 µg/L respectively, as described previously [20]. The first post-dose samples below LLOQ were included as a plasma concentration of 0.5 µg/L (1/2 LLOQ for dexamethasone); other samples below LLOQ were omitted [21].
Sample size
In order to study age-related differences, children ≤ 18 years were divided in three age groups (≥ 0.5–6 years; ≥ 6–12 years and ≥ 12 years) treated with dexamethasone with/without (fos)aprepitant. We planned to include 30 children in each age category, with the aim to distinguish 15 children using dexamethasone without (fos)aprepitant and 15 children using dexamethasone with (fos)aprepitant. We planned to evaluate at least 5 children across all age groups, based on previous experience in similar projects.
Dexamethasone model development
Starting point for model development for dexamethasone were one- and two-compartment models with first-order absorption [22,23,24,25]. Allometric scaling using body weight was a priori included on all parameters [26].
Interindividual variability (IIV) was evaluated for all parameters, using an exponential function [27]. Since data of multiple dexamethasone doses were available (sampling over 24 h, while dexamethasone was administered twice or four times daily), interoccasion variability (IOV) was implemented similarly as IIV, with each dose and subsequent sampling defined as a separate occasion. This variability was evaluated for all parameters to diagnose potential time-dependent trends and allow for random unaccounted variability between dosing moments. Residual unexplained variability was evaluated as a proportional error model or as a combination of a proportional and additive error model.
Dexamethasone covariate analysis
Following structural model development, the influence of patient-specific factors for variability in PK parameters was evaluated. Assessed covariates included age and (fos)aprepitant treatment to study the effect of (fos)aprepitant treatment on dexamethasone CL. Continuous covariates were evaluated using a power function. (Fos)aprepitant treatment was described as a binary categorical variable: 1 when (fos)aprepitant was administered concomitantly and 0 when no (fos)aprepitant was administered. (Fos)aprepitant as a covariate was tested on CL as follows:
where Pcov represents the estimated proportional factor by which CL changes at a specific covariate value.
Integrated dexamethasone and aprepitant model development
In order to thoroughly investigate the drug-drug interaction, an integrated PK model of dexamethasone and (fos)aprepitant was developed. The PK of (fos)aprepitant was assumed to be described by a one-compartment model with absorption transit compartments, as described by Nijstad et al. [28]. The dataset that was used for the current model was previously used for the solely (fos)aprepitant model [28].
Two (hypothetical) enzyme compartments (enzymeactive and enzymeinactive) were added as previously described by Huitema et al. [29]. Elimination of dexamethasone was directly proportional to the amount of enzymeactive present in the compartment. The amount of enzymeactive was set to 1 and enzymeinactive to 0 at t = 0. The conversion of enzymeactive to enzymeinactive was driven by the amount of aprepitant in the central compartment.
Model evaluation
Discrimination between models was guided by physiological plausibility, goodness-of-fit (GOF) plots, precision of parameter estimates, and change in objective function value (dOFV). A drop of ≥ 3.84 points, corresponding to a P < 0.05 (χ2 distribution with one degree of freedom (df)), was considered a significant improved fit for hierarchical models. The adequacy of the models was assessed by GOF plots and visual predictive checks (VPC) [30]. Parameter precision was assessed by the sampling importance resampling procedure [31].
Drug-drug interaction between dexamethasone and aprepitant
Since patients in both groups (dexamethasone with/without (fos)aprepitant) were not treated with the same dexamethasone doses (Table 1), it is difficult to compare the observed areas under the curve (AUCs) between the two groups, in order to assess the influence of (fos)aprepitant on the AUC of dexamethasone. For this reason, simulations were carried out. Patients included in this study were used for the simulations and individuals were replicated to attain a total of 2000 patients per group. All patients were hypothetically treated, once with a single dose of intravenous dexamethasone alone and once with a single dose of intravenous dexamethasone plus oral aprepitant (doses according to Table 1, HEC day 1). In the first simulations, the hypothetical dexamethasone dose in both groups was the same (100%, 6 mg/m2), to compare AUCs. Subsequently, dexamethasone dose reductions (50% and 33%) were tested to test which dose regimen would lead to comparable (assessed visually and by range) AUCs for both groups. The AUCt0-∞ (in mg/L*h) was calculated using a dummy compartment in the final population PK model. The results of these simulated AUCs are used for the dexamethasone dose reduction recommendations.
Software
Nonlinear mixed-effects modelling was performed using NONMEM (version 7.3.0, ICON development Solutions, Ellicott City, MD, USA) and Pearl-speaks-NONMEM (PsN, version 4.7.0) with First-Order Conditional Estimation with interaction (FOCE-I) as estimation method [32, 33]. Pirana (version 2.9.9) was used as graphical user interface for NONMEM [34]. R (version 3.4.3) was used for data handling and visualization [35].
Results
Patients and sampling
In total, 222 patients were eligible for inclusion in the study. Of these patients, 93 gave informed consent, 39 patients did not gave informed consent, 87 patients were screen failures before informed consent was given and 3 patients did not response before the study was closed. 65 of the 93 included patients with a median age of 8.8 years (range 0.6–17.9) were available for sampling in this study, and were included between March 2019 and April 2021. For trial profile, see Fig. 1. A total of 28 children were excluded after receiving informed consent. In 12 of these children, dexamethasone was stopped as antiemetic drug due to hypertension (n = 3), behavioral problems (n = 6), or a combination of those two (n = 1), bradycardia (n = 1) or no complaints of nausea (n = 1). No patients were included in the study twice.
Of the 65 sampled patients, 18 patients were treated with dexamethasone without aprepitant and 47 patients with dexamethasone plus aprepitant. We experienced a lower median age in the dexamethasone group compared to the dexamethasone with aprepitant group. In 80% of the patients, samples were taken on day 1 of antiemetic treatment. In total, 62 of the patients (95%) were treated with intravenous dexamethasone. Detailed patient characteristics are shown in Table 2. In total, 305 dexamethasone samples were available for analysis, of which 12 were below LLOQ (all single below LLOQ samples post-dose). No outliers were observed in our data. Supplementary Figure S1 displays the observed plasma concentrations over time.
Dexamethasone model development
A two-compartment model with first-order absorption was appropriate to describe the dexamethasone PK. The absorption rate constant (ka) could not be estimated due to the small number of patients that were treated with dexamethasone orally, so ka was fixed to 1.5 h−1 [36, 37]. Interindividual variability (IIV) was included on CL, Q, and Vc, and interoccasion variability (IOV) on CL and Vc.
Inclusion of aprepitant as categorical covariate on CL led to an improved model fit (dOFV − 7.2). The proportional factor by which CL changes was estimated at 0.74 (95% confidence interval (CI) 0.56 − 1.01), signifying a 26% lower CL when aprepitant is administrated concomitantly.
Integrated dexamethasone and aprepitant model development
The model was further optimized by integrating the dexamethasone and aprepitant models. A graphical representation of the combined model is showed in Supplementary Figure S3. The inhibition of dexamethasone CL was modelled by an aprepitant concentration-dependent reversible inhibition of enzymes. As mentioned in the methods, the total amount of enzymes consisted of an active and inactive part. Mass transport between enzymeactive and enzymeinactive was modelled using an inhibition rate constant kinh and a reactivation rate constant kreac. No age-related effects on any of the PK parameters were found.
The final model consisted of a two-compartment model with first-order absorption for dexamethasone, a one-compartment model with absorption transit compartments and two enzyme compartments describing the aprepitant concentration-dependent reversible inhibition of enzymes. The final estimates and 95%CI are shown in Table 3.
The GOF plots (Supplementary Figure S3A and B) showed accurate population and individual predictions, without signs for over- or underprediction. CWRES are evenly distributed over the whole plasma concentration range (Supplementary Figure S3C) and time interval (Supplementary Figure S3D). The VPC demonstrated that the median and the 95%CI of the observed data were in line with those from the simulation-based predictions from the model (Supplementary Figure S4).
Drug-drug interaction between dexamethasone and aprepitant
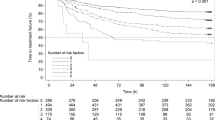
Simulations were carried out and AUCs were calculated (Supplementary Table S2 and Fig. 2). Patients treated with 6 mg/m2 dexamethasone without aprepitant achieved a 54% higher median AUCt0-∞ than patients treated with 6 mg/m2 dexamethasone with aprepitant. When the patients with aprepitant were hypothetically treated with 3 mg/m2 dexamethasone (50% reduction), we observed that the dexamethasone AUCt0-∞ of patients with aprepitant was 23% lower than the AUCt0-∞ of patients without aprepitant. This again shows that a dose reduction of dexamethasone of 50% is not accurate to achieve comparable exposure. A dexamethasone dose of 4 mg/m2 (dose reduction of 33%) for patients receiving concurrent aprepitant was tested. This resulted in a comparable exposure between the two groups.
Discussion
This population PK model is the first to describe the PK of dexamethasone (with and without aprepitant) as antiemetic agent in children. Dexamethasone PK was best described using a two compartment model, which is consistent with previously published models [22,23,24,25]. Firstly, a sole dexamethasone model was developed, including aprepitant as a categorical covariate. With concurrent aprepitant, dexamethasone CL changes with a proportional factor of 0.74 (95%CI 0.56–1.01), meaning a 26% lower CL with concurrent aprepitant. However, this solely model did not reflect clinical practice properly, since we expect the interaction to be dependent on the aprepitant plasma concentration. Therefore, we attributed the fact that the 95%CI of the interaction component includes 1 to a modelling artefact. An integrated dexamethasone-aprepitant model was developed subsequently, in order to accurately examine the influence of aprepitant on dexamethasone CL. We found that aprepitant reduced the dexamethasone CL by approximately 30%. This is not consistent with the results of studies in adults and current practice in children [11,12,13,14]. These studies all described a reduction of dexamethasone CL of approximately 50% or a doubling of the exposure to dexamethasone when combined with aprepitant.
At first, a possible explanation for the clinically relevant discrepancy with the results obtained in adults was thought to be related to age, since the rationale for dexamethasone dose reduction in children was extrapolated from adults. However, in our model development, no reason for testing age as covariate on any of the PK parameters was found. For this, we concluded that age has no obvious effect on the PK of dexamethasone or aprepitant.
Another possible explanation for the difference between adults and children could be found in the route of administration of dexamethasone. In several of the previously published articles, dexamethasone was administered orally [11, 13]. It was hypothesized that the presence of aprepitant reduces dexamethasone metabolism by inhibiting CYP3A4 enzymes in the gastro-intestinal (GI) tract, when dexamethasone is administered orally [15]. The inhibition of CYP3A4 enzymes in the GI-tract will lead to reduction of the first pass effect and thus bioavailability, which leads to a higher systemic dexamethasone exposure. When dexamethasone is administered intravenously, as in 95% of our pediatric patients, this effect will not play a role and only the systemic elimination of dexamethasone is influenced by concurrent use of aprepitant. However, two studies in adults did investigate the effect of aprepitant on intravenous dexamethasone, and also did find a reduction of the dexamethasone CL of approximately 50% [12, 14]. Since the drug-drug interaction with either oral or intravenous dexamethasone was never compared within a previous study, we initiated a future study to examine this. Within this study, patients will receive dexamethasone orally and intravenously in a cross-over design. We will include patients with and without aprepitant in a 1:1 ratio. The difference in PK and the bioavailability of dexamethasone and the influence of aprepitant will be studied in these cohorts (https://www.trialregister.nl/trial/8981).
In the current study, 11 children were excluded after informed consent was given, due to stopping dexamethasone because of off-target side effects like hypertension and/or behavioral problems. Although dexamethasone is strongly recommended in clinical antiemetic guidelines[1,2,3, 38], the side effects are a major issue in daily practice. Moreover, the appropriate dose to control CINV is intensively debated among different hospitals treating pediatric oncology patients. For example, in a survey among 36 children’s oncology institutions, two groups never administered dexamethasone. In the other 34 institutions, 29 different dexamethasone dosing schedules were used for children receiving HEC [39]. A recent systematic review aimed to describe all different dexamethasone doses studied for the prevention of chemotherapy-induced vomiting (CIV) in pediatric patients and their effects on achieving complete acute CIV control [40]. However, due to the heterogeneity of the studies and the wide variety in dosing schedules, no optimal dexamethasone dose to control acute CIV was found. Dosing regimens varied from 6 to 27 mg/m2/day in patients receiving HEC and 0.6–24 mg/m2/day in patients receiving MEC [40].
Translating the results of this study into clinical practice is challenging. On one hand, this current study shows that reduction of the intravenous dexamethasone dose with 50% in children might be too high, since we showed that aprepitant inhibits dexamethasone CL by approximately 30%. Based on the results of the current study, we advise to reduce the intravenous dexamethasone dose with 30% in children, when combined with aprepitant. However, as we already see many side effects of dexamethasone in our current HEC dose schedule, it is not very appealing to upgrade the current dexamethasone dose of 3 mg/m2 4 times daily in presence of aprepitant. Triple therapy is the cornerstone of antiemetic treatment, however dexamethasone is regularly omitted due to side effects. Future studies should address dose reductions of dexamethasone, even as duration of antiemetic therapy in children, as many pediatric chemotherapy courses last much longer than the typical 3 day aprepitant regimen. For these future studies, we suggest to investigate a dose reduction of 30% in presence of aprepitant, and a dosing regimen within the dexamethasone dosing range (6–27 mg/m2/day) as described in the recent systematic review on the different dexamethasone dosing schedules worldwide [40].
Furthermore, our study underlines that extrapolating results from adults to children can be extremely difficult and should be done with caution. In our example, we found a clinically relevant discrepancy with the results in adults. That extrapolations from adults to children should be done with caution was previously described by Cella et al. [41]. They underlined that assuming a linear relationship between body weight and dose is not right for all drugs and that it can lead to either under- of overdosing. They suggested that dose recommendations for children should be derived from an integrated (model-based) analysis of PK data rather than from empiricism. This is in line with the results from our current study.
This study has several strengths. To start with, this is the first study that assessed the PK of dexamethasone as antiemetic agent and the influence of aprepitant on dexamethasone PK in children. Secondly, we used a rich sampling scheme and at least 5 blood samples were collected in 40 patients (62%). Furthermore, we developed an integrated dexamethasone and aprepitant model, where the inhibition of dexamethasone CL was dependent on the plasma concentration of aprepitant. This is closest to the real life situation in patients. To our knowledge, this was not tested before.
However, this study had some limitations too. Dexamethasone was administered intravenously in almost all patients, and therefore the difference of the effect of aprepitant on oral versus intravenous dexamethasone CL could not be identified. Because of this limitation, based on the current study, we can only give recommendations for intravenously administered dexamethasone in children.
Our second limitation refers to our planned sample size. We included 65 of the defined 90 patients. This was due to inclusion difficulties because of Covid-19 restrictions and the loss of eligible patients due to dexamethasone cancellation. The sample size of 90 patients was suggested in order to achieve a diverse population. However, we have shown in this analysis that we were able to accurately develop an integrated PK model with 65 patients. Moreover, we included our planned 5 children across all age groups except for the dexamethasone group of ≥ 6–12 years, in which only 2 children were sampled. The lower median age in the dexamethasone group compared to the dexamethasone plus aprepitant group was thought to be explained by the experience that older patients were treated with triple therapy more frequently than younger patients, due a higher occurrence of HEC chemotherapy courses.
Future studies are needed to optimize antiemetic control in pediatric oncology treatment. From this study we have learned the effect of aprepitant on dexamethasone CL in the pediatric oncology population. This important knowledge on the difference in CL compared to the adult population will be proceeded to the next phase in the optimization of antiemetic control. We are planning to conduct a randomized controlled trial in which we will study prolonged use of aprepitant to evaluate CINV control.
Data availability
Any reasonable requests to share data will be considered by the investigators. Data requests should be sent to the corresponding author.
References
Dupuis LL, Sung L, Molassiotis A et al (2017) 2016 updated MASCC/ESMO consensus recommendations: prevention of acute chemotherapy-induced nausea and vomiting in children. Support Care Cancer 25:323–331. https://doi.org/10.1007/s00520-016-3384-y
Hesketh PJ, Kris MG, Basch E et al (2017) Antiemetics: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 35:3240–3261
Patel P, Robinson PD, Thackray J et al (2017) Guideline for the prevention of acute chemotherapy-induced nausea and vomiting in pediatric cancer patients: a focused update. Pediatr Blood Cancer 64:1–12. https://doi.org/10.1002/pbc.26542
Einhorn LH, Rapoport B, Navari RM et al (2017) 2016 updated MASCC/ESMO consensus recommendations: prevention of nausea and vomiting following multiple-day chemotherapy, high-dose chemotherapy, and breakthrough nausea and vomiting. Support Care Cancer 25:303–308. https://doi.org/10.1007/s00520-016-3449-y
Paw Cho Sing E, Robinson PD, Flank J et al (2019) Classification of the acute emetogenicity of chemotherapy in pediatric patients: a clinical practice guideline. Pediatr Blood Cancer 66:e27646. https://doi.org/10.1002/pbc.27646
Duggan DE, Yeh KC, Matalia N et al (1975) Bioavailability of oral dexamethasone. Clin Pharmacol Ther 18:205–209. https://doi.org/10.1002/cpt1975182205
Dexcel Pharma Technologies (per FDA) (2019) Product Information: HEMADY(TM) oral tablets, dexamethasone oral tablets. Boulder, CO
Richter O, Ern B, Reinhardt D, Becker B (1983) Pharmacokinetics of dexamethasone in children. Pediatr Pharmacol (New York) 3:329–337
Merck Sharp, Dohme BV (2008) Summary of product characteristics: Emend
Merck Sharp, Dohme BV (2013) Summary of product characteristics: Ivemend
McCrea JB, Majumdar AK, Goldberg MR et al (2003) Effects of the neurokinin1 receptor antagonist aprepitant on the pharmacokinetics of dexamethasone and methylprednisolone. Clin Pharmacol Ther 74:17–24. https://doi.org/10.1016/S0009-9236(03)00066-3
Nakade S, Ohno T, Kitagawa J et al (2008) Population pharmacokinetics of aprepitant and dexamethasone in the prevention of chemotherapy-induced nausea and vomiting. Cancer Chemother Pharmacol 63:75–83. https://doi.org/10.1007/s00280-008-0713-y
Marbury TC, Ngo PL, Shadle CR et al (2011) Pharmacokinetics of oral dexamethasone and midazolam when administered with single-dose intravenous 150 mg fosaprepitant in healthy adult subjects. J Clin Pharmacol 51:1712–1720. https://doi.org/10.1177/0091270010387792
Takahashi T, Nakamura Y, Tsuya A et al (2011) Pharmacokinetics of aprepitant and dexamethasone after administration of chemotherapeutic agents and effects of plasma substance P concentration on chemotherapy-induced nausea and vomiting in Japanese cancer patients. Cancer Chemother Pharmacol 68:653–659. https://doi.org/10.1007/s00280-010-1519-2
Aapro MS, Walko CM (2010) Aprepitant: drug–drug interactions in perspective. Ann Oncol 21:2316–2323. https://doi.org/10.1093/annonc/mdq149
Small BE, Holdsworth MT, Raisch DW, Winter SS (2000) Survey ranking of emetogenic control in children receiving chemotherapy. J Pediatr Hematol Oncol 22:125–132. https://doi.org/10.1097/00043426-200003000-00009
Holdsworth MT, Raisch DW, Frost J (2006) Acute and delayed nausea and emesis control in pediatric oncology patients. Cancer 106:931–940. https://doi.org/10.1002/cncr.21631
Dupuis LL, Nathan PC (2010) Optimizing emetic control in children receiving antineoplastic therapy: Beyond the guidelines. Pediatr Drugs 12:51–61
Kearns GL, Abdel-Rahman SM, Alander SW et al (2003) Developmental pharmacology-drug disposition, action, and therapy in infants and children. N Engl J Med 349:1157–1167. https://doi.org/10.1056/NEJMra035092
Nijstad AL, Tibben MM, Gebretensae A et al (2021) Development and validation of a combined liquid chromatography tandem-mass spectrometry assay for the quantification of aprepitant and dexamethasone in human plasma to support pharmacokinetic studies in pediatric patients. J Chromatogr B 1171:122639. https://doi.org/10.1016/j.jchromb.2021.122639
Irby DJ, Ibrahim ME, Dauki AM et al (2021) Approaches to handling missing or “problematic” pharmacology data: pharmacokinetics. CPT Pharmacometrics Syst Pharmacol 10:291–308. https://doi.org/10.1002/psp4.12611
Krzyzanski W, Milad MA, Jobe AH et al (2021) Population pharmacokinetic modeling of intramuscular and oral dexamethasone and betamethasone in Indian women. J Pharmacokinet Pharmacodyn 48:261–272. https://doi.org/10.1007/s10928-020-09730-z
Brady ME, Sartiano GP, Rosenblum SL et al (1987) The pharmacokinetics of single high doses of dexamethasone in cancer patients. Eur J Clin Pharmacol 32:593–596. https://doi.org/10.1007/BF02455994
Gupta SK, Ritchie JC, Ellinwood EH et al (1992) Modeling the pharmacokinetics and pharmacodynamics of dexamethasone in depressed patients. Eur J Clin Pharmacol 43:51–55. https://doi.org/10.1007/BF02280754
Loew D, Schuster O, Graul EH (1986) Dose-dependent pharmacokinetics of dexamethasone. Eur J Clin Pharmacol 30:225–230. https://doi.org/10.1007/BF00614309
West GB, Brown JH, Enquist BJ (1997) A general model for the origin of allometric scaling laws in biology. Science 276:122–126. https://doi.org/10.1126/science.276.5309.122
Bauer RJ (2019) NONMEM tutorial part I: description of commands and options, with simple examples of population analysis. CPT Pharmacometrics Syst Pharmacol 8:525–537. https://doi.org/10.1002/psp4.12404
Nijstad AL, de Vos-Kerkhof E, Enters-Weijnen CF, et al (2022) A simple extemporaneous oral suspension of aprepitant yields sufficient pharmacokinetic exposure in children. J Oncol Pharm Pract 107815522210892. https://doi.org/10.1177/10781552221089243
Huitema ADR, Mathôt RAA, Tibben MM et al (2001) A mechanism-based pharmacokinetic model for the cytochrome P450 drug-drug interaction between cyclophosphamide and thioTEPA and the autoinduction of cyclophosphamide. J Pharmacokinet Pharmacodyn 28:211–230. https://doi.org/10.1023/A:1011543508731
Bergstrand M, Hooker AC, Wallin JE, Karlsson MO (2011) Prediction-corrected visual predictive checks for diagnosing nonlinear mixed-effects models. AAPS J 13:143–151. https://doi.org/10.1208/s12248-011-9255-z
Dosne AG, Bergstrand M, Karlsson MO (2017) An automated sampling importance resampling procedure for estimating parameter uncertainty. J Pharmacokinet Pharmacodyn 44:509–520. https://doi.org/10.1007/s10928-017-9542-0
Lindbom L, Ribbing J, Jonsson EN (2004) Perl-speaks-NONMEM (PsN)–a Perl module for NONMEM related programming. Comput Methods Programs Biomed 75:85–94. https://doi.org/10.1016/j.cmpb.2003.11.003
Boeckmann AJ, Sheiner LB, Beal SL (2011) NONMEM User Guide. NONMEM Part V 2–169. https://doi.org/10.1007/s13398-014-0173-7.2
Keizer RJ, van Benten M, Beijnen JH et al (2011) Piraña and PCluster: a modeling environment and cluster infrastructure for NONMEM. Comput Methods Programs Biomed 101:72–79. https://doi.org/10.1016/j.cmpb.2010.04.018
RC Team (2009) R: a language and environment for statistical computing. R Found Stat Comput Vienna
Yang L, Panetta JC, Cai X et al (2008) Asparaginase may influence dexamethasone pharmacokinetics in acute lymphoblastic leukemia. J Clin Oncol 26:1932–1939. https://doi.org/10.1200/JCO.2007.13.8404
Jackson RK, Liebich M, Berry P et al (2019) Impact of dose and duration of therapy on dexamethasone pharmacokinetics in childhood acute lymphoblastic leukaemia—a report from the UKALL 2011 trial. Eur J Cancer 120:75–85. https://doi.org/10.1016/j.ejca.2019.07.026
Hesketh PJ, Kris MG, Basch E et al (2020) Antiemetics: ASCO Guideline Update. J Clin Oncol 38:2782–2797. https://doi.org/10.1200/JCO.20.01296
Patel P, Robinson PD, Orsey A et al (2016) Chemotherapy-induced nausea and vomiting prophylaxis: practice within the Children’s Oncology Group. Pediatr Blood Cancer 63:887–892. https://doi.org/10.1002/pbc.25915
Patel P, Olteanu A, Cabral S, et al (2020) Dexamethasone dosing for prevention of acute chemotherapy‐induced vomiting in pediatric patients: a systematic review. Pediatr Blood Cancer 67. https://doi.org/10.1002/pbc.28716
Cella M, Knibbe C, Danhof M, Della Pasqua O (2010) What is the right dose for children? Br J Clin Pharmacol 70:597–603. https://doi.org/10.1111/j.1365-2125.2009.03591.x
Funding
This work was supported by Children Cancer-free Foundation (KiKa) project number 320.
Author information
Authors and Affiliations
Contributions
E.d.V., M.v.d.W., W.T., M.Z., and A.H. were responsible for protocol development. E.d.V. and L.N. for implementation of the study and E.d.V., L.N., and C.E. for enrolling patients. Bioanalysis was performed by M.T. and supervised by H.R. Population PK modelling was performed by L.N. M.Z., A.L., and A.H. supervised this work. The first draft of the manuscript was written by L.N. and E.d.V., and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the institutional Medical Ethics Committee of the Erasmus MC (MEC-2018–1578).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nijstad, A.L., de Vos-Kerkhof, E., Enters-Weijnen, C.F. et al. Overestimation of the effect of (fos)aprepitant on intravenous dexamethasone pharmacokinetics requires adaptation of the guidelines for children with chemotherapy-induced nausea and vomiting. Support Care Cancer 30, 9991–9999 (2022). https://doi.org/10.1007/s00520-022-07423-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07423-6