Abstract
Background
Enhanced recovery after bariatric surgery (ERABS) is an approach developed to improve outcomes in obese surgical patients. Unfortunately, it is not evenly implemented in Italy. The Italian Society for the Surgery of Obesity and Metabolic Diseases and the Italian Society of Anesthesia, Analgesia, Resuscitation and Intensive Care joined in drafting an official statement on ERABS.
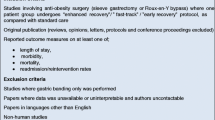
Methods
To assess the effectiveness and safety of ERABS and to develop evidence-based recommendations with regard to pre-, intra-, and post-operative care for obese patients undergoing ERABS, a 13-member expert task force of surgeons and anesthesiologists from Italian certified IFSO center of excellence in bariatric surgery was established and a review of English-language papers conducted. Oxford 2011 Levels of Evidence and U.S. Preventive Services Task Force Grade Definitions were used to grade the level of evidence and the strength of recommendations, respectively. The supporting evidence and recommendations were reviewed and discussed by the entire group at meetings to achieve a final consensus.
Results
Compared to the conventional approach, ERABS reduces the length of hospital stay and does not heighten the risk of major post-operative complications, re-operations, and hospital re-admissions, nor does it increase the overall surgical costs. A total of 25 recommendations were proposed, covering pre-operative evaluation and care (7 items), intra-operative management (1 item, 11 sub-items), and post-operative care and discharge (6 items).
Conclusions
ERABS is an effective and safe approach. The recommendations allow the proper management of obese patients undergoing ERABS for a better outcome.
Similar content being viewed by others
Bariatric surgery is the most effective treatment for morbid obesity. The demand for bariatric surgery continues to grow as the proportion of the population with obesity increases. Bariatric surgery is mainly optional in predominantly high-risk patients. Providing an effective, safe, and economically sustainable approach is challenging for physicians [1, 2].
Enhanced Recovery after Surgery (ERAS) is a modern approach to reduce perioperative stress and help patients recover more quickly following surgery, leading to improved outcomes in postoperative morbidity and length of hospital stay (LOS). ERAS, implemented initially for elective colorectal surgery, has been extended over time to many other surgeries [3], including bariatric surgery [4]. However, the ERAS after bariatric surgery (ERABS) guidelines published in 2016 [4] relied heavily on the evidence and recommendations developed in no-bariatric surgery settings. Afterward, an increasing number of peer-reviewed papers about ERABS have been published, showing the favorable outcomes observed in ERAS.
Despite the evidence, some resistance to adopting ERABS protocols remains in bariatric surgery centers in Italy. The Italian Ministry of Health’s 2018 Annual Report on hospital admission and discharge events reported a total of 25,424 surgical procedures for obesity, with an average LOS of 3.9 days [5]. So, if, on the one hand, this data suggests that the conventional approach is largely adopted in bariatric surgery, on the other, it leaves considerable opportunity for improving bariatric surgery outcomes by adopting the ERABS approach.
Materials and methods
The Italian Society of Surgery of Obesity and Metabolic Diseases (SICOB) and the Italian Society of Anesthesia, Analgesia, Resuscitation and Intensive Care (SIAARTI) undertook a process for drafting an official joint statement on ERABS. The two societies appointed a 13-member expert task force, which met first in October 2019 to define the scope and methods of the project. It was decided that the primary objective was to summarize available evidence supporting ERABS, focusing on the efficacy and safety outcomes. The secondary objective was to review the importance of the individual ERABS protocol items.
Four main areas for investigation were identified: outcomes for the primary endpoint and preoperative, intraoperative, and postoperative care for the secondary endpoint. Corresponding subcommittees were appointed to systematically review ERABS topics, grade the levels of evidence, and propose specific recommendations with supporting evidence for each topic.
A systematic PubMed search of English-language papers published from 1999 to April 2020 was performed combining the following terms: “obesity” and “surgery” or “bariatric surgery” or “fast track” or “enhanced recovery” or “perioperative care” or “perioperative management” or “sleeve gastrectomy” or “gastric bypass.” The levels of evidence were assessed using Oxford 2011 Levels of Evidence (Table 1) [6]. To rate the strength of recommendations, grade definitions based on the U.S. Preventive Services Task Force were used (Tables 2 and 3) [7].
Key issues were discussed at a meeting in January 2020, after which a comprehensive document was circulated and then revised. The panel concluded its work with a Consensus Meeting in July 2020, where supporting evidence and recommendations were reviewed and discussed by the entire group to achieve a final consensus. Subsequently, a draft report was prepared and sent to the panel for comments and modification. Each author approved the final version before it was submitted. Ethics approval and consent were not required for this type of study.
Results
The evidence and recommendations concerning the primary safety and efficiency endpoints are summarized in Table 4. A total of 25 recommendations were proposed, covering pre-operative evaluation and care (7 items), intra-operative management (1 item, 11 sub-items), and post-operative care and discharge (6 items). The levels of evidence and recommendations for each item in the ERABS protocol are summarized in Table 4.
Effectiveness and safety of ERABS
Compared to the conventional approach, ERABS reduces the LOS [8,9,10], independently of the type of surgical procedure performed [11, 12]. The more successful ERABS items the multidisciplinary team adopts, the greater the likelihood of a reduced post-operative LOS [13].
Also, compared to the standard approach, ERABS does not have an increased risk for major postoperative complications, reoperations, and hospital readmissions [8,9,10,11,12, 14]. However, it also does not reduce the number of major complications [8,9,10,11,12, 14]. ERABS, moreover, seems to reduce the total surgical costs compared to the standard approach [8, 15].
Preoperative counseling
Preoperative information and counseling are key items for managing the expectations of patients and preparing them for early discharge [16]. Counseling was one of the most frequently used items in a retrospective multicenter study [17] and one of the key items in 11 of the 13 studies considered in a systematic review [8]. A retrospective study on the safety of an early postoperative discharge following bariatric surgery identified the receipt of preoperative information on early ambulation and refeeding, as well as pain and postoperative nausea and vomiting (PONV) management, as one of the more important protocol items of the ERABS pathway [18].
Preoperative patient optimization
Smoking cessation for at least four weeks reduced postoperative surgical and pulmonary complications by 41% [19], supporting the argument that smoking should be discontinued for at least four weeks before bariatric surgery [20]. Physicians should inform patients of the increased risk of morbidity and mortality in smokers. This risk decreases the longer smoking is ceased before surgery [21].
Preoperative weight loss reduces liver volume and may technically facilitate the operation [22]. However, whether weight loss reduces postoperative complications remains controversial [21, 23]. A Swedish registry study reported a decrease in complications after gastric bypass surgery [24].
Optimizing the preoperative fasting blood glucose level through diet, physical activity, and pharmacotherapy is mandatory [20, 21, 23]. A value greater than 180 mg/dl was associated with increased perioperative complications and mortality [20].
Obstructive sleep apnea (OSA) carries an increased risk of postoperative cardiorespiratory complications [25]. Although this aspect has been debated in bariatric surgery [26, 27], increased complications and LOS have been observed in OSA patients who underwent bariatric surgery [28,29,30]. The use of noninvasive ventilation (NIV) (e.g., continuous positive airway pressure [CPAP]) was reported to improve the preoperative cardiometabolic profile [31] and the postoperative respiratory function [21, 23, 32]. It may be safely adopted for patients undergoing bariatric surgery [32]. Even if postoperative care in a monitored setting may be considered for high-risk obese patients undergoing surgery [20, 33], patients with severe OSA and/or home CPAP selected for ERABS do not require a routine planned postoperative admission into the intensive care unit [20, 21, 27].
Preoperative fasting
Properly managing preoperative fasting may be important to minimize perioperative stress. Maintaining homeostasis avoids or reduces catabolism and related proteolysis, asthenia, or cellular dysfunction [34,35,36,37]. Clear liquids can be taken up to 2 h before surgery and solid food up to 6 h before the induction of anesthesia [3, 38,39,40,41]. No strong evidence supports preoperative oral carbohydrate loading in bariatric surgery. Furthermore, there is some reluctance to adopt preoperative oral carbohydrate loading in patients suffering from diabetes or metabolic syndrome [42]. Absolute or prolonged preoperative fasting is no guarantee of a secretion-free stomach at the induction of anesthesia [42].
Postoperative nausea and vomiting prophylaxis
General anesthesia is associated with an increased risk of PONV [43]. The prevention of PONV in ERABS is recommended [4], and it is consistent with the guidelines for the general surgical population [43]. The polypharmacological approach to PONV prophylaxis is preferable to monotherapy [20, 43] and was reported to decrease the incidence of PONV and the postoperative use of antiemetics, opioid analgesics, and liquid infusion [44].
Venous thromboembolism prophylaxis
The incidence of deep vein thrombosis and pulmonary embolism after bariatric surgery is approximately 0.1–0.5% and, in the vast majority of cases, occurs after the patient is discharged [21, 45, 46]. A multimodal venous thromboembolism prophylaxis via chemoprophylaxis, mechanical aids, and/or patient mobilization is suggested [4, 20, 21, 47,48,49]. It is reported as a key item in ERABS [12, 34, 39, 50,51,52,53,54,55,56,57,58,59,60,61]. Chemoprophylaxis with low-molecular-weight heparin (LMWH) after surgery and home discharge is considered effective [20, 48, 52, 53] and is associated with a lower bleeding risk [52]. However, there is insufficient evidence to recommend a specific dose and duration of the LMWH treatment [20, 47,48,49, 52]. Early ambulation in the postoperative period is considered a useful component of multimodal venous thromboembolism prophylaxis [20, 47, 49].
Antibiotic prophylaxis
The incidence of surgical site infections in obese patients varies from 1 to 21.7%, depending on the procedure type [62]. The use of preoperative antibiotic prophylaxis is then recommended [20, 21, 23]. It should follow the standard guidelines for perioperative antibiotic prophylaxis [63]. The most frequently used antibiotic is cefazolin (dosage 1–4 g), with clindamycin recommended as an alternative in allergic patients [54, 64]. A dose adjustment based on the patient’s weight compared to a fixed dose of 2 g administered intravenously before surgical incision is preferable [65, 66]. Higher dosages (cefazolin 3 g) in patients weighing > 120 kg should be considered [20]. Literature does not support prophylactic vancomycin or cefoxitin [64]. Intestinal preparation by antibiotic prophylaxis (whether or not combined with mechanical preparation) is not recommended in bariatric surgery [60]. Preoperative antibiotic prophylaxis, administered intravenously at the induction of anesthesia or 30–60 min before surgical incision, is reported to be one of the important items in ERABS [12, 17, 60, 67].
Monitoring
The standard for anesthesia monitoring should be ensured in the perioperative period [4, 20, 33, 68]. In obese patients, anesthesia depth monitoring ensures a more accurate induction of anesthesia with propofol and reduces the risk of awareness from inadequate dosing [69], as well as during intravenous and inhalational anesthesia [70]. The monitoring of the neuromuscular function helps reduce the risk of postoperative respiratory complications [71]. Temperature monitoring reduces the risk of hypothermia, improving postoperative recovery [72].
Standardized anesthesia approach
The standardized ERABS approach showed favorable outcomes compared to a non-standardized one [8,9,10,11,12,13,14]. Advances in the perioperative care of obese patients translated into a standardized anesthesiological approach have been proven to be effective and safe [73] in the ERABS context as well [39].
Airway management
In obese surgical patients, airway management can present challenges. Difficult mask ventilation has been reported in 8.8% of obese patients, and 11% of those have morbid obesity. Difficult intubation has been reported in 3.3–16.7% of patients [20]. Difficult airway management predictors include males, OSA, increased waist-to-hip ratio (> 0.8 in women and > 0.9 in men), BMI (> 50 kg/m2), and neck circumference (> 41 cm in women and > 43 cm in men) [20, 33, 74,75,76]. OSA risk stratification is then suggested using validated questionnaires, such as STOP-BANG, and reserving the time-consuming and expensive polysomnography for patients at high risk of severe OSA (e.g., STOP-BANG ≥ 5) [3, 21, 23, 28,29,30,31, 33, 77,78,79,80,81]. The ramp position improves the likelihood of successful airway management in obese patients [20, 23].
Pre-oxygenation
Adequate pre-oxygenation aiming for end-tidal oxygen concentrations of ≥ 90% before the induction of general anesthesia is suggested. Pre-oxygenation has been reported as important in prolonging safe apnea times following general anesthesia induction [82, 83]. The NO DESAT (nasal oxygen during efforts securing a tube) technique, which uses a simple nasal cannula with standard cold dry oxygen may be considered [82]. Pre-oxygenation using a high-flow nasal cannula or positive pressure by CPAP/NIV seems more effective than the standard approach [82, 84,85,86,87,88,89,90,91] and may be beneficial for high-risk obese patients [20, 32, 33, 82].
Tracheal intubation
An appropriate planned approach is recommended for airway management in obese patients [3, 20, 33]. In obese patients, videolaryngoscopes compared with Macintosh laryngoscopes increases the likelihood of successful intubation on the first attempt at laryngoscopy [92]. This result seems to be ensured more by the use of a videolaryngoscope with a tracheal tube guide than one without [93].
Second-generation extraglottic devices were recommended as rescue devices for pulmonary oxygenation/ventilation in the case of difficult airway management and possible fibroscope-guided intubation [94,95,96,97,98]. The fibroscopic/endoscopic technique was essential when intubating conscious patients [99]. In awake patient, video laryngoscopy has been suggested as a valid alternative to fiberoptic intubation in experienced practitioners [100,101,102].
General anesthesia
General anesthesia is the approach of choice in ERABS [3, 4, 20, 33]. There is no evidence supporting the superiority of inhalation versus intravenous anesthesia [3, 4, 20, 33]. Anesthesia strategies based on short-acting, low-accumulation drugs that promote rapid recovery from general anesthesia are suggested [4, 20, 33]. Desflurane has been associated with faster postoperative awakening and recovery than other inhalational anesthetics and propofol [103,104,105,106]. Intravenous anesthesia with propofol has demonstrated a lower risk of PONV in the general population [107] and in obese surgical patients [108]. PONV prophylaxis has been observed to reduce the risk of PONV incidence [109], particularly with inhalational anesthesia [20].
Analgesia and opioid
In the general surgical population, opioid use was associated with an increased risk of PONV [110], as well as upper airway obstruction and hypoventilation [111]. In obese patients, intraoperative opioid use was associated with an increased risk of PONV [112] and postoperative respiratory complications [113]. Opioid-sparing or opioid-free anesthesia should be preferred when managing obese surgical patients [20, 33] under ERABS [4], as it is associated with a lower incidence of PONV [112].
Opioids with rapid elimination kinetics, such as remifentanil, have demonstrated faster postoperative awakening and recovery of respiratory functions in general surgical populations compared to other opiods [114]. In obese patients, remifentanil has demonstrated reduced recovery time from general anesthesia, respiratory complications, and LOS [115]. Patient-controlled analgesia has also been successfully used in obese surgical patients [116] and should be preferred over continuous infusion in the postoperative period [3, 20].
Multimodal analgesia
Multimodal analgesia as a pain control strategy using analgesics (e.g., nonsteroidal anti-inflammatory drugs, paracetamol) in combination with analgesic adjuvants and local anesthetics is recommended in ERABS to optimize pain control after surgery and to reduce or eliminate the postoperative use of opioids [4, 20, 33, 34, 117] and related adverse events [118]. Adjuvant analgesics, such as ketamine [119, 120], clonidine [119, 121], dexmedetomidine [121,122,123], magnesium [123,124,125], lidocaine [126], pregabalin [127, 128], and gabapentin [129], alone or in combination, significantly reduced postoperative pain compared with controls.
Locoregional analgesia
Intraperitoneal local anesthetics [130,131,132,133] and the ultrasound-guided TAP (transversus abdominis plane) block [134,135,136] showed a significant effect on reducing pain scores at recovery from general anesthesia [137, 138]. The benefit may be increased by the infiltration of trocar insertions and wound closures with local anesthetics at the end of the surgical procedure [20, 135]. Notably, these pain control benefits did not affect the LOS [130,131,132,133,134,135,136]. Epidural analgesia may be considered in selected patients [139].
Neuromuscular blockade
Neuromuscular blockade (NMB) is suggested at the induction of general anesthesia to facilitate airway management and subsequent pulmonary ventilation [20, 33, 82]. Deep compared to moderate NMB optimizes the surgical field view, reduces procedural complications in laparoscopic surgery [140], and is associated with less postoperative pain [140, 141]. Sugammadex compared to cholinesterase inhibitors provides a more rapid and predictable recovery of rocuronium-induced NMB [142, 143] and is associated with less pain and PONV in the postoperative period [141, 144] and faster discharge to the surgical ward [143, 144]. Quantitative monitoring and complete recovery of the neuromuscular function at the end of surgery are highly recommended [4, 20, 33].
Protective ventilation
Protective mechanical lung ventilation should be preferred for obese patients undergoing general anesthesia for bariatric surgery [20] because it is associated with reduced postoperative respiratory complications, LOS, and mortality in both non-obese and obese surgical patients [145,146,147].
Slow abdominal insufflation with a maximum intra-abdominal pressure of less than 15 mmHg is advised, when possible, during laparoscopy [20] to favor mechanical lung ventilation [20, 148]. This strategy, combined with limiting surgical time, is associated with a reduction in the risk of postoperative respiratory complications [148,149,150].
Goal-directed fluid therapy
Proper perioperative fluid management avoiding overhydration helps to minimize the risk of PONV, postoperative complications, and prolonged LOS [151,152,153]. A goal-directed fluid therapy (GDFT) has been suggested as an adequate strategy to reduce these risks [154], even in bariatric surgery [155,156,157]. In bariatric surgery, excessive fluid should be avoided, and GDFT should be considered a useful strategy [155,156,157]. A GDFT guided by noninvasive indices, such as the Pleth Variability Index, may be a more acceptable monitoring option to GDFT based on invasive methods [155] and, consequently, more widely used in bariatric surgery, even in the ERABS context [155,156,157]. Postoperative fluid infusions should be discontinued as soon as possible, with preference given to the enteral route [60, 153, 158]. Intraoperative hypotension (mean arterial pressure of ≤ 65 mmHg), even for a few minutes, is a predictor of renal and myocardial damage [159]. It should thus be avoided or promptly treated in the perioperative period [154, 159].
Protected extubation
The extubation should be performed on an awake patient in the ramped position and/or reverse Trendelenburg position, which improves lung volume, oxygenation, and respiratory mechanics [20, 33, 160, 161]. Oxygen therapy with nasal goggles or HFNC was associated with a reduced risk of post-extubation desaturation [160] and reintubation [162]. CPAP or NIV was recommended for awakening moderate-severe OSA patients or those suffering from the obese hypoventilation syndrome who are already receiving home treatment or who will require opioid therapy postoperatively [20, 32, 163]. CPAP and NIV do not appear to negatively affect the outcome of the surgical procedure [32].
Nasogastric tube
In abdominal surgery, avoiding the routine use of nasogastric tubes (NGTs) results in a faster recovery of the bowel function, a decrease in pulmonary complications, and a shorter LOS without any associated increase in anastomotic dehiscence [164]. In ERABS, compared to the conventional approach, avoiding NGT use demonstrated better postoperative recovery without an increase in complications [11,12,13, 41], reducing postoperative pain and PONV, promoting early mobilization and resumption of liquid diet, and resulting in better compliance at discharge [38, 39, 55]. Society positions in favor of abandoning, when possible, the routine use of postoperative NGT are already available [3, 54].
Abdominal drainage
Many gastrointestinal surgeries can be performed safely without prophylactic drainage [165]. In bariatric surgery, the evidence is limited [166]. A retrospective study of a gastric bypass population reported no difference in anastomotic dehiscence and reintervention rates in patients receiving abdominal drainage compared to those who are not [167]. Avoiding abdominal drainage was found to be a key item in the ERABS [3, 11, 12, 14, 17, 19, 59, 67, 168]. Society positions in favor of abandoning the routine use of abdominal drainage, when possible, are available [3, 54].
Bladder catheter
Avoidance or early removal of bladder catheters resulted in early mobilization and prevented urinary tract infection [169,170,171]. In ERABS, compared to the conventional approach, avoiding bladder catheters was associated with early mobilization and reduced LOS, readmission rate, and minor complications, such as urinary tract infection [3, 10, 14, 18, 50, 67, 168, 172]. Society positions in favor of abandoning the routine use of bladder catheter, when possible, are available [54].
Early mobilization
Early postoperative mobilization is recommended in obese patients undergoing bariatric surgery [4, 11, 14, 20, 21, 33]. Independent mobilization for at least 4 h during the first 24 h following surgery was significantly associated with a lower rate of postoperative complications and a shorter LOS [173]. Early postoperative mobilization was reported as a key element of better postoperative recovery in ERABS [17,18,19,20, 29, 39, 54,55,56,57,58,59, 67, 168, 172], and adequate independent mobilization was a condition for a home discharge [14, 18, 21, 39, 54, 56, 58, 59, 67].
Early refeeding
The advantage of early oral refeeding has been reported in both ERAS [3] and ERABS [39,40,41, 173] and seems particularly associated with an earlier restoration of bowel function, faster wound healing, less infection, and lower risk of postoperative complications [36, 37, 174]. Early oral refeeding was associated with a reduced LOS and mortality [44, 60]. Conversely, prolonged postoperative fasting was associated with thirst, emotional fixation on food, and a phobia about the reintroduction of food [36, 37, 174].
Discharge
Discharge on postoperative day 1 or 2 was not associated with an increase in the complication rate, readmission, or telephone consultations in both ERAS [3, 18] and ERABS [11, 12, 175], particularly in the absence of significant comorbidities [176, 177]. Caution should be taken in the presence of suspected clinical conditions (e.g., tachycardia) and/or abnormal level of serological markers (e.g., C-reactive protein, procalcitonin) as predictors of risk of postoperative complications [178,179,180,181]. However, there is no consensus on which serological markers should be assessed and at which postoperative time point [182,183,184,185]. Routine postoperative contrast imaging examination increased costs and LOS [186, 187] and was not considered to be a reliable assessment of postoperative complications [188,189,190].
Discharge on the day of surgery was reported as feasible in selected patients [190,191,192]. However, there was some disagreement around the safety of same-day discharge [193, 194]. The adoption and verification of a discharge checklist may be a useful tool for a safe discharge [57]. The minimum criteria for a discharge included vital parameters within the normal range, adequate pain control by nonopioid analgesics, adequate water intake, ability to tolerate liquid diet, and no evidence of sepsis or signs of postoperative complication. Finally, predischarge education concerning signs and symptoms of possible postoperative complications and procedures for contacting the staff were also identified as a key component of a successful discharge [11, 12, 39, 55].
Discussion
Literature review supports ERABS in reducing LOS without increasing complications and costs [8,9,10]. Producing a statement on ERABS standardizes the ERABS approach across bariatric surgery centers, benefiting both patients and hospitals [195]. The standardization of the approach may also allow the evaluation of ERABS’s effective impact on the postoperative complications and total costs compared to the standard approach [196]. Notably, it became clear from this statement that the more items in the protocol that are adopted, the more efficient the ERABS approach will be [13].
Perioperative management involves a multidisciplinary team, where a full collaboration among anesthesiologists, surgeons, and staff members may lead to the best results [73]. The ERABS statement, drafted thanks to this collaboration, is, therefore, addressed not only to anesthesiologists or surgeons, but also to everyone involved in the perioperative care of obese patients in bariatric surgery centers.
References
Gloy VL, Briel M, Bhatt DL, Kashyap SR, Schauer PR, Mingrone G, Bucher HC, Nordmann AJ (2013) Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ 347:f5934
Colquitt JL, Picot J, Loveman E, Clegg AJ (2009) Surgery for obesity. Cochrane Database Syst Rev 2:CD003641
Smith TW Jr, Wang X, Singer MA, Godellas CV, Vaince FT (2020) Enhanced recovery after surgery: a clinical review of implementation across multiple surgical subspecialties. Am J Surg 219:530–534
Thorell A, MacCormick AD, Awad S, Reynolds N, Roulin D, Demartines N, Vignaud M, Alvarez A, Singh PM, Lobo DN (2016) Guidelines for perioperative care in bariatric surgery: Enhanced Recovery After Surgery (ERAS) society recommendations. World J Surg 40:2065–2083
The Italian Ministry of Health (2018) Annual report on hospitalization activity. http://www.salute.gov.it/imgs/C_17_pubblicazioni_2898_allegato.pdf
OCEBM Levels of Evidence Working Group*. The Oxford 2011 levels of evidence. https://www.cebm.net/wp-content/uploads/2014/06/CEBM-Levels-of-Evidence-2.1.pdf
7Grade Definitions. U.S. preventive services task force. October 2018. https://uspreventiveservicestaskforce.org/uspstf/grade-definitions
Ahmed OS, Rogers AC, Bolger JC, Mastrosimone A, Robb WB (2018) Meta-analysis of enhanced recovery protocols in bariatric surgery. J Gastrointest Surg 22:964–972
Singh PM, Panwar R, Borle A, Goudra B, Trikha A, van Wagensveld BA, Sinha A (2017) Efficiency and safety effects of applying ERAS protocols to bariatric surgery: a systematic review with meta-analysis and trial sequential analysis of evidence. Obes Surg 27:489–501
Małczak P, Pisarska M, Piotr M, Wysocki M, Budzyński A, Pędziwiatr M (2017) Enhanced recovery after bariatric surgery: systematic review and meta-analysis. Obes Surg 27:226–235
Lemanu DP, Singh PP, Berridge K, Burr M, Birch C, Babor R, MacCormick AD, Arroll B, Hill AG (2013) Randomized clinical trial of enhanced recovery versus standard care after laparoscopic sleeve gastrectomy. Br J Surg 100:482–489
Ruiz-Tovar J, Garcia A, Ferrigni C, Gonzalez J, Castellon C, Duran M (2019) Impact of implementation of an enhanced recovery after surgery (ERAS) program in laparoscopic Roux-en-Y gastric bypass: a prospective randomized clinical trial. Surg Obes Relat Dis 15:228–235
Brethauer SA, Grieco A, Fraker T, Evans-Labok K, Smith A, McEvoy MD, Saber AA, Morton JM, Petrick A (2019) Employing Enhanced Recovery Goals in Bariatric Surgery (ENERGY): a national quality improvement project using the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program. Surg Obes Relat Dis 15:1977–1989
Geubbels N, Evren I, Acherman YIZ, Bruin SC, van de Laar AWJM, Hoen MB, de Brauw LM (2019) Randomized clinical trial of an enhanced recovery after surgery programme versus conventional care in laparoscopic Roux-en-Y gastric bypass surgery. BJS Open 3:274–281
Simonelli V, Goergen M, Orlando GG, Arru L, Zolotas CA, Geeroms M, Poulain V, Azagra JS (2016) Fast-track in bariatric and metabolic surgery: feasibility and cost analysis through a matched-cohort study in a single centre. Obes Surg 26:1970–1977
Elliott JA, Patel VM, Kirresh A, Ashrafian H, Le Roux CW, Olbers T, Athanasiou T, Zacharakis E (2013) Fast-track laparoscopic bariatric surgery: a systematic review. Updates Surg 65:85–94
Deneuvy A, Slim K, Sodji M, Blanc P, Gallet D, Blanchet MC (2018) Implementation of enhanced recovery programs for bariatric surgery. Results from the Francophone large-scale database. Surg Obes Relat Dis 14:99–105
Lam J, Suzuki T, Bernstein D, Zhao B, Maeda C, Pham T, Sandler BJ, Jacobsen GR, Cheverie JN, Horgan S (2019) An ERAS protocol for bariatric surgery: is it safe to discharge on post-operative day 1? Surg Endosc 33:580–586
Mills E, Eyawo O, Lockhart I, Kelly S, Wu P, Ebbert JO (2011) Smoking cessation reduces postoperative complications: a systematic review and meta-analysis. Am J Med 124:144–154
Carron M, Safaee Fakhr B, Ieppariello G, Foletto M (2020) Perioperative care of the obese patient. Br J Surg 107:e39–e55
Mechanick JI, Apovian C, Brethauer S, Garvey WT, Joffe AM, Kim J, Kushner RF, Lindquist R, Pessah-Pollack R, Seger J, Urman RD, Adams S, Cleek JB, Correa R, Figaro MK, Flanders K, Grams J, Hurley DL, Kothari S, Seger MV, Still CD (2020) Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures—2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surg Obes Relat Dis 16:175–247
Edholm D, Kullberg J, Haenni A, Karlsson FA, Ahlström A, Hedberg J, Ahlström H, Sundbom M (2011) Preoperative 4-week low-calorie diet reduces liver volume and intrahepatic fat, and facilitates laparoscopic gastric bypass in morbidly obese. Obes Surg 21:345–350
Di Lorenzo N, Antoniou SA, Batterham RL, Busetto L, Godoroja D, Iossa A, Carrano FM, Agresta F, Alarçon I, Azran C, Bouvy N, Balaguè Ponz C, Buza M, Copaescu C, De Luca M, Dicker D, Di Vincenzo A, Felsenreich DM, Francis NK, Fried M, Gonzalo Prats B, Goitein D, Halford JCG, Herlesova J, Kalogridaki M, Ket H, Morales-Conde S, Piatto G, Prager G, Pruijssers S, Pucci A, Rayman S, Romano E, Sanchez-Cordero S, Vilallonga R, Silecchia G (2020) Clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) on bariatric surgery: update 2020 endorsed by IFSO-EC, EASO and ESPCOP. Surg Endosc 34:2332–2358
Anderin C, Gustafsson UO, Heijbel N, Thorell A (2015) Weight loss before bariatric surgery and postoperative complications: data from the Scandinavian Obesity Registry (SOReg). Ann Surg 261:909–913
Kaw R, Chung F, Pasupuleti V, Mehta J, Gay PC, Hernandez AV (2012) Meta-analysis of the association between obstructive sleep apnoea and postoperative outcome. Br J Anaesth 109:897–906
de Raaff CA, Coblijn UK, de Vries N, van Wagensveld BA (2016) Is fear for postoperative cardiopulmonary complications after bariatric surgery in patients with obstructive sleep apnea justified? A systematic review. Am J Surg 211:793–801
Goucham AB, Coblijn UK, Hart-Sweet HB, de Vries N, Lagarde SM, van Wagensveld BA (2016) Routine postoperative monitoring after bariatric surgery in morbidly obese patients with severe obstructive sleep Apnea: ICU admission is not necessary. Obes Surg 26:737–742
Corso R, Russotto V, Gregoretti C, Cattano D (2018) Perioperative management of obstructive sleep apnea: a systematic review. Minerva Anestesiol 84:81–93
Devaraj U, Rajagopala S, Kumar A, Ramachandran P, Devereaux PJ, D’Souza GA (2017) Undiagnosed obstructive sleep Apnea and postoperative outcomes: a prospective observational study. Respiration 94:18–25
Nepomnayshy D, Hesham W, Erickson B, MacDonald J, Iorio R, Brams D (2013) Sleep apnea: is routine preoperative screening necessary? Obes Surg 23:287–291
Romero-Corral A, Caples SM, Lopez-Jimenez F, Somers VK (2010) Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest 137:711–719
Carron M, Zarantonello F, Tellaroli P, Ori C (2016) Perioperative noninvasive ventilation in obese patients: a qualitative review and meta-analysis. Surg Obes Relat Dis 12:681–691
Petrini F, Di Giacinto I, Cataldo R, Esposito C, Pavoni V, Donato P, Trolio A, Merli G, Sorbello M, Pelosi P, Obesity Task Force for the SIAARTI Airway Management Study Group (2016) Perioperative and periprocedural airway management and respiratory safety for the obese patient: 2016 SIAARTI Consensus. Minerva Anestesiol 82:1314–1335
Alvarez A, Goudra BG, Singh PM (2017) Enhanced recovery after bariatric surgery. Curr Opin Anaesthesiol 30:133–139
Grant MC, Gibbons MM, Ko CY, Wick EC, Cannesson M, Scott MJ, McEvoy MD, King AB, Wu CL (2019) Evidence review conducted for the agency for healthcare research and quality safety program for improving surgical care and recovery: focus on anesthesiology for bariatric surgery. Anesth Analg 129:51–60
Tsang E, Lambert E, Carey S (2018) Fasting leads to fasting: examining the relationships between perioperative fasting times and fasting for symptoms in patients undergoing elective abdominal surgery. Asia Pac J Clin Nutr 27:968–974
Lambert E, Carey S (2016) Practice guideline recommendations on perioperative fasting: a systematic review. JPEN J Parenter Enteral Nutr 40:1158–1165
Major P, Małczak P, Wysocki M, Torbicz G, Gajewska N, Pędziwiatr M, Budzyński A (2018) Bariatric patients’ nutritional status as a risk factor for postoperative complications, prolonged length of hospital stay and hospital readmission: a retrospective cohort study. Int J Surg 56:210–214
Trotta M, Ferrari C, D’Alessandro G, Sarra G, Piscitelli G, Marinari GM (2019) Enhanced recovery after bariatric surgery (ERABS) in a high-volume bariatric center. Surg Obes Relat Dis 15:1785–1792
Goretti G, Marinari GM, Vanni E, Ferrari C (2020) Value-based healthcare and enhanced recovery after surgery implementation in a high-volume bariatric center in Italy. Obes Surg 30:2519–2527
Prabhakaran S, Misra S, Magila M, Kumar SS, Kasthuri S, Palanivelu C, Raj PP (2020) Randomized controlled trial comparing the outcomes of enhanced recovery after surgery and standard recovery pathways in laparoscopic sleeve gastrectomy. Obes Surg 30:3273–3279
Pędziwiatr M, Mavrikis J, Witowski J, Adamos A, Major P, Nowakowski M, Budzyński A (2018) Current status of enhanced recovery after surgery (ERAS) protocol in gastrointestinal surgery. Med Oncol 35:95
Gan TJ, Diemunsch P, Habib AS, Kovac A, Kranke P, Meyer TA, Watcha M, Chung F, Angus S, Apfel CC, Bergese SD, Candiotti KA, Chan MT, Davis PJ, Hooper VD, Lagoo-Deenadayalan S, Myles P, Nezat G, Philip BK, Tramèr MR, Society for Ambulatory Anesthesia (2014) Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg 118:85–113
Benevides ML, Oliveira SS, de Aguilar-Nascimento JE (2013) The combination of haloperidol, dexamethasone, and ondansetron for prevention of postoperative nausea and vomiting in laparoscopic sleeve gastrectomy: a randomized double-blind trial. Obes Surg 23:1389–1396
Stein PD, Matta F (2013) Pulmonary embolism and deep venous thrombosis following bariatric surgery. Obes Surg 23:663–668
Gambhir S, Inaba CS, Alizadeh RF, Nahmias J, Hinojosa M, Smith BR, Nguyen NT, Daly S (2020) Venous thromboembolism risk for the contemporary bariatric surgeon. Surg Endosc 34:3521–3526
American Society for Metabolic and Bariatric Surgery Clinical Issues Committee (2013) ASMBS updated position statement on prophylactic measures to reduce the risk of venous thromboembolism in bariatric surgery patients. Surg Obes Relat Dis 9:493–497
Venclauskas L, Maleckas A, Arcelus JI, ESA VTE Guidelines Task Force (2018) European guidelines on perioperative venous thromboembolism prophylaxis: surgery in the obese patient. Eur J Anaesthesiol 35:147–153
Bartlett MA, Mauck KF, Daniels PR (2015) Prevention of venous thromboembolism in patients undergoing bariatric surgery. Vasc Health Risk Manag 11:461–477
Ma P, Lloyd A, McGrath M, Moore R, Jackson A, Boone K, Higa K (2020) Reduction of opioid use after implementation of enhanced recovery after bariatric surgery (ERABS). Surg Endosc 34:2184–2190
Sinha A, Jayaraman L, Punhani D, Chowbey P (2017) Enhanced recovery after bariatric surgery in the severely obese, morbidly obese, super-morbidly obese and super-super morbidly obese using evidence-based clinical pathways: a comparative study. Obes Surg 27:560–568
Altieri MS, Yang J, Hajagos J, Spaniolas K, Park J, Gasparis AP, Bates AT, Docimo S, Talamini M, Shroyer AL, Pryor AD (2018) Evaluation of VTE prophylaxis and the impact of alternate regimens on post-operative bleeding and thrombotic complications following bariatric procedures. Surg Endosc 32:4805–4812
Raftopoulos I, Martindale C, Cronin A, Steinberg J (2008) The effect of extended post-discharge chemical thromboprophylaxis on venous thromboembolism rates after bariatric surgery: a prospective comparison trial. Surg Endosc 22:2384–2391
Dang JT, Szeto VG, Elnahas A, Ellsmere J, Okrainec A, Neville A, Malik S, Yorke E, Hong D, Biertho L, Jackson T, Karmali S (2020) Canadian Consensus Statement: enhanced recovery after surgery in bariatric surgery. Surg Endosc 34:1366–1375
Mannaerts GHH, Allatif REA, Al Hashmi FY, Bhosale A, Hammo AN, Isied SH, Qureshi WA, Al Hamad OS, Kayyal Y, Al Afari HST (2019) First successful large-scale introduction of an Enhanced Recovery after Bariatric Surgery (ERABS) Program in the Middle East: The Results and Lessons Learned of Tawam Hospital/Johns Hopkins, a Tertiary Governmental Center in the UAE. Obes Surg 29:2100–2109
Nagliati C, Troian M, Pennisi D, Balani A (2019) Enhanced recovery after bariatric surgery: 202 consecutive patients in an Italian Bariatric Center. Obes Surg 29:3133–3141
Gondal AB, Hsu CH, Serrot F, Rodriguez-Restrepo A, Hurbon AN, Galvani C, Ghaderi I (2019) Enhanced recovery in bariatric surgery: a study of short-term outcomes and compliance. Obes Surg 29:492–498
Awad S, Carter S, Purkayastha S, Hakky S, Moorthy K, Cousins J, Ahmed AR (2014) Enhanced recovery after bariatric surgery (ERABS): clinical outcomes from a tertiary referral bariatric centre. Obes Surg 24:753–758
Meunier H, Le Roux Y, Fiant AL, Marion Y, Bion AL, Gautier T, Contival N, Lubrano J, Fobe F, Zamparini M, Piquet MA, Savey V, Alves A, Menahem B (2019) Does the implementation of enhanced recovery after surgery (ERAS) guidelines improve outcomes of bariatric surgery? A propensity score analysis in 464 patients. Obes Surg 29:2843–2853
Major P, Wysocki M, Torbicz G, Gajewska N, Dudek A, Małczak P, Pędziwiatr M, Pisarska M, Radkowiak D, Budzyński A (2018) Risk factors for prolonged length of hospital stay and readmissions after laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y Gastric Bypass. Obes Surg 28:323–332
Proczko M, Kaska L, Twardowski P, Stepaniak P (2016) Implementing enhanced recovery after bariatric surgery protocol: a retrospective study. J Anesth 30:170–173
Fischer MI, Dias C, Stein A, Meinhardt NG, Heineck I (2014) Antibiotic prophylaxis in obese patients submitted to bariatric surgery. A systematic review. Acta Cir Bras 29:209–217
Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, Fish DN, Napolitano LM, Sawyer RG, Slain D, Steinberg JP, Weinstein RA, American Society of Health-System Pharmacists; Infectious Disease Society of America; Surgical Infection Society; Society for Healthcare Epidemiology of America (2013) Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm 70:195–283
Ferraz ÁAB, Santa-Cruz F, Edmiston CE Jr (2020) Antibiotic prophylaxis in bariatric surgical procedures: Is there an ideal antimicrobial agent? Surg Infect (Larchmt) 21:654–658
Chen X, Brathwaite CE, Barkan A, Hall K, Chu G, Cherasard P, Wang S, Nicolau DP, Islam S, Cunha BA (2017) Optimal cefazolin prophylactic dosing for bariatric surgery: no need for higher doses or intraoperative redosing. Obes Surg 27:626–629
Blum S, Cunha CB, Cunha BA (2019) Lack of pharmacokinetic basis of weight-based dosing and intra-operative re-dosing with cefazolin surgical prophylaxis in obese patients: implications for antibiotic stewardship. Surg Infect (Larchmt) 20:439–443
Hahl T, Peromaa-Haavisto P, Tarkiainen P, Knutar O, Victorzon M (2016) Outcome of laparoscopic gastric bypass (LRYGB) with a program for enhanced recovery after surgery (ERAS). Obes Surg 26:505–511
Checketts MR, Alladi R, Ferguson K, Gemmell L, Handy JM, Klein AA, Love NJ, Misra U, Morris C, Nathanson MH, Rodney GE, Verma R, Pandit JJ, Association of Anaesthetists of Great Britain and Ireland (2016) Recommendations for standards of monitoring during anaesthesia and recovery 2015: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia 71:85–93
Subramani Y, Riad W, Chung F, Wong J (2017) Optimal propofol induction dose in morbidly obese patients: a randomized controlled trial comparing the bispectral index and lean body weight scalar. Can J Anaesth 64:471–479
Gaszyński T, Wieczorek A (2016) A comparison of BIS recordings during propofol-based total intravenous anaesthesia and sevoflurane-based inhalational anaesthesia in obese patients. Anaesthesiol Intensive Ther 48:239–247
Blobner M, Hunter JM, Meistelman C, Hoeft A, Hollmann MW, Kirmeier E, Lewald H, Ulm K (2020) Use of a train-of-four ratio of 0.95 versus 0.9 for tracheal extubation: an exploratory analysis of POPULAR data. Br J Anaesth 124:63–72
Mason DS, Sapala JA, Wood MH, Sapala MA (1998) Influence of a forced air warming system on morbidly obese patients undergoing Roux-en-Y gastric bypass. Obes Surg 8:453–460
Carron M, Ieppariello G, Safaee Fakhr B, Foletto M (2020) Perioperative care of the obese patient: a successful approach. Br J Surg 107:772–773
Leoni A, Arlati S, Ghisi D, Verwej M, Lugani D, Ghisi P, Cappelleri G, Cedrati V, El Tantswi Ali Alsheraei A, Pocar M, Ceriani V, Aldegheri G (2014) Difficult mask ventilation in obese patients: analysis of predictive factors. Minerva Anestesiol 80:149–157
Riad W, Vaez MN, Raveendran R, Tam AD, Quereshy FA, Chung F, Wong DT (2016) Neck circumference as a predictor of difficult intubation and difficult mask ventilation in morbidly obese patients: a prospective observational study. Eur J Anaesthesiol 33:244–249
Moon TS, Fox PE, Somasundaram A, Minhajuddin A, Gonzales MX, Pak TJ, Ogunnaike B (2019) The influence of morbid obesity on difficult intubation and difficult mask ventilation. J Anesth 33:96–102
Ravesloot MJ, van Maanen JP, Hilgevoord AA, van Wagensveld BA, de Vries N (2012) Obstructive sleep apnea is underrecognized and underdiagnosed in patients undergoing bariatric surgery. Eur Arch Otorhinolaryngol 269:1865–1871
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep Apnea: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med 13:479–504
de Raaff CA, Pierik AS, Coblijn UK, de Vries N, Bonjer HJ, van Wagensveld BA (2017) Value of routine polysomnography in bariatric surgery. Surg Endosc 31:245–248
Khan A, King WC, Patterson EJ, Laut J, Raum W, Courcoulas AP, Atwood C, Wolfe BM (2013) Assessment of obstructive sleep apnea in adults undergoing bariatric surgery in the longitudinal assessment of bariatric surgery-2 (LABS-2) study. J Clin Sleep Med 9:21–29
Lockhart EM, Willingham MD, Abdallah AB, Helsten DL, Bedair BA, Thomas J, Duntley S, Avidan MS (2013) Obstructive sleep apnea screening and postoperative mortality in a large surgical cohort. Sleep Med 14:407–415
Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, O’Sullivan EP, Woodall NM, Ahmad I, Difficult Airway Society intubation guidelines working group (2015) Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth 115:827–848
Altermatt FR, Muñoz HR, Delfino AE, Cortínez LI (2005) Pre-oxygenation in the obese patient: effects of position on tolerance to apnoea. Br J Anaesth 95:706–709
Guitton C, Ehrmann S, Volteau C, Colin G, Maamar A, Jean-Michel V, Mahe PJ, Landais M, Brule N, Bretonnière C, Zambon O, Vourc’h M (2019) Nasal high-flow preoxygenation for endotracheal intubation in the critically ill patient: a randomized clinical trial. Intensive Care Med 45:447–458
Vourc’h M, Huard D, Feuillet F, Baud G, Guichoux A, Surbled M, Tissot M, Chiffoleau A, Guitton C, Jaber S, Asehnoune K (2019) Preoxygenation in difficult airway management: high-flow oxygenation by nasal cannula versus face mask (the PREOPTIDAM study). Protocol for a single-centre randomised study. BMJ Open 9(4):e025909
Cressey DM, Berthoud MC, Reilly CS (2001) Effectiveness of continuous positive airway pressure to enhance pre-oxygenation in morbidly obese women. Anaesthesia 56:680–684
Coussa M, Proietti S, Schnyder P, Frascarolo P, Suter M, Spahn DR, Magnusson L (2004) Prevention of atelectasis formation during the induction of general anesthesia in morbidly obese patients. Anesth Analg 98:1491–1495
Gander S, Frascarolo P, Suter M, Spahn DR, Magnusson L (2005) Positive end-expiratory pressure during induction of general anesthesia increases duration of nonhypoxic apnea in morbidly obese patients. Anesth Analg 100:580–584
Edmark L, Östberg E, Scheer H, Wallquist W, Hedenstierna G, Zetterström H (2016) Preserved oxygenation in obese patients receiving protective ventilation during laparoscopic surgery: a randomized controlled study. Acta Anaesthesiol Scand 60:26–35
Georgescu M, Tanoubi I, Fortier LP, Donati F, Drolet P (2012) Efficacy of preoxygenation with non-invasive low positive pressure ventilation in obese patients: crossover physiological study. Ann Fr Anesth Reanim 31:e161–e165
Harbut P, Gozdzik W, Stjernfält E, Marsk R, Hesselvik JF (2014) Continuous positive airway pressure/pressure support pre-oxygenation of morbidly obese patients. Acta Anaesthesiol Scand 58:675–680
Hoshijima H, Denawa Y, Tominaga A, Nakamura C, Shiga T, Nagasaka H (2018) Videolaryngoscope versus Macintosh laryngoscope for tracheal intubation in adults with obesity: a systematic review and meta-analysis. J Clin Anesth 44:69–75
Carron M, Ieppariello G, Linassi F (2021) Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in obese adults: a meta-analysis. J Clin Anesth 71:110216
Sinha A, Jayaraman L, Punhani D (2013) ProSeal™ LMA increases safe apnea period in morbidly obese patients undergoing surgery under general anesthesia. Obes Surg 23:580–584
Natalini G, Franceschetti ME, Pantelidi MT, Rosano A, Lanza G, Bernardini A (2003) Comparison of the standard laryngeal mask airway and the ProSeal laryngeal mask airway in obese patients. Br J Anaesth 90:323–326
Cook TM, Woodall N, Frerk C, Fourth National Audit Project (2011) Major complications of airway management in the UK: results of the Fourth National Audit Project of the royal college of anaesthetists and the difficult airway society. Part 1: anaesthesia. Br J Anaesth 106:617–631
Cook TM, Woodall N, Harper J, Benger J, Fourth National Audit Project (2011) Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: intensive care and emergency departments. Br J Anaesth 106:632–642
Nicholson A, Cook TM, Smith AF, Lewis SR, Reed SS (2013) Supraglottic airway devices versus tracheal intubation for airway management during general anaesthesia in obese patients. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD010105.pub2
Ahmad I, El-Boghdadly K, Bhagrath R, Hodzovic I, McNarry AF, Mir F, O’Sullivan EP, Patel A, Stacey M, Vaughan D (2020) Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia 75:509–528
Abdelmalak BB, Bernstein E, Egan C, Abdallah R, You J, Sessler DI, Doyle DJ (2011) GlideScope® vs flexible fibreoptic scope for elective intubation in obese patients. Anaesthesia 66:550–555
Rosenstock CV, Thøgersen B, Afshari A, Christensen AL, Eriksen C, Gätke MR (2012) Awake fiberoptic or awake video laryngoscopic tracheal intubation in patients with anticipated difficult airway management: a randomized clinical trial. Anesthesiology 116:1210–1216
Abdellatif AA, Ali MA (2014) GlideScope videolaryngoscope versus flexible fiberoptic bronchoscope for awake intubation of morbidly obese patient with predicted difficult intubation. Middle East J Anaesthesiol 22:385–392
Juvin P, Vadam C, Malek L, Dupont H, Marmuse JP, Desmonts JM (2000) Postoperative recovery after desflurane, propofol, or isoflurane anesthesia among morbidly obese patients: a prospective, randomized study. Anesth Analg 91:714–719
La Colla L, Albertin A, La Colla G, Mangano A (2007) Faster wash-out and recovery for desflurane vs sevoflurane in morbidly obese patients when no premedication is used. Br J Anaesth 99:353–358
McKay RE, Malhotra A, Cakmakkaya OS, Hall KT, McKay WR, Apfel CC (2010) Effect of increased body mass index and anaesthetic duration on recovery of protective airway reflexes after sevoflurane vs desflurane. Br J Anaesth 104:175–182
Liu FL, Cherng YG, Chen SY, Su YH, Huang SY, Lo PH, Lee YY, Tam KW (2015) Postoperative recovery after anesthesia in morbidly obese patients: a systematic review and meta-analysis of randomized controlled trials. Can J Anaesth 62:907–917
Sneyd JR, Carr A, Byrom WD, Bilski AJ (1998) A meta-analysis of nausea and vomiting following maintenance of anaesthesia with propofol or inhalational agents. Eur J Anaesthesiol 15:433–445
Carron M, Tessari I, Linassi F, Navalesi P (2021) Desflurane versus propofol for general anesthesia maintenance in obese patients: a pilot meta-analysis. J Clin Anesth 68:110103
De Baerdemaeker L, Margarson M (2016) Best anaesthetic drug strategy for morbidly obese patients. Curr Opin Anaesthesiol 29:119–128
Frauenknecht J, Kirkham KR, Jacot-Guillarmod A, Albrecht E (2019) Analgesic impact of intra-operative opioids vs. opioid-free anaesthesia: a systematic review and meta-analysis. Anaesthesia 74:651–662
Ehsan Z, Mahmoud M, Shott SR, Amin RS, Ishman SL (2016) The effects of anesthesia and opioids on the upper airway: a systematic review. Laryngoscope 126:270–284
Ziemann-Gimmel P, Goldfarb AA, Koppman J, Marema RT (2014) Opioid-free total intravenous anaesthesia reduces postoperative nausea and vomiting in bariatric surgery beyond triple prophylaxis. Br J Anaesth 112:906–911
Mulier JP, Dillemans B (2019) Anaesthetic factors affecting outcome after bariatric surgery, a retrospective levelled regression analysis. Obes Surg 29:1841–1850
Komatsu R, Turan AM, Orhan-Sungur M, McGuire J, Radke OC, Apfel CC (2007) Remifentanil for general anaesthesia: a systematic review. Anaesthesia 62:1266–1280
Sudré EC, de Batista PR, Castiglia YM (2015) Longer immediate recovery time after anesthesia increases risk of respiratory complications after laparotomy for bariatric surgery: a randomized clinical trial and a cohort study. Obes Surg 25:2205–2212
Choi YK, Brolin RE, Wagner BK, Chou S, Etesham S, Pollak P (2000) Efficacy and safety of patient-controlled analgesia for morbidly obese patients following gastric bypass surgery. Obes Surg 10:154–159
Andersen LP, Werner MU, Rosenberg J, Gögenur I (2014) Analgesic treatment in laparoscopic gastric bypass surgery: a systematic review of randomized trials. Obes Surg 24:462–470
Ng JJ, Leong WQ, Tan CS, Poon KH, Lomanto D, So JBY, Shabbir A (2017) Multimodal analgesic protocol reduces opioid-related adverse events and improves patient outcomes in laparoscopic sleeve gastrectomy. Obes Surg 27:3075–3081
Sollazzi L, Modesti C, Vitale F, Sacco T, Ciocchetti P, Idra AS, Tacchino RM, Perilli V (2009) Preinductive use of clonidine and ketamine improves recovery and reduces postoperative pain after bariatric surgery. Surg Obes Relat Dis 5:67–71
Kasputytė G, Karbonskienė A, Macas A, Maleckas A (2020) Role of ketamine in multimodal analgesia protocol for bariatric surgery. Medicine (Kaunas) 56:96
Naja ZM, Khatib R, Ziade FM, Moussa G, Naja ZZ, Naja AS, Kanawati S (2014) Effect of clonidine versus dexmedetomidine on pain control after laparoscopic gastric sleeve: a prospective, randomized, double-blinded study. Saudi J Anaesth 8(Suppl 1):S57-62
Bakhamees HS, El-Halafawy YM, El-Kerdawy HM, Gouda NM, Altemyatt S (2007) Effects of dexmedetomidine in morbidly obese patients undergoing laparoscopic gastric bypass. Middle East J Anaesthesiol 19:537–551
Zarif P, Abdelaal Ahmed Mahmoud A, Abdelhaq MM, Mikhail HM, Farag A (2016) Dexmedetomidine versus magnesium sulfate as adjunct during anesthesia for laparoscopic colectomy. Anesthesiol Res Pract 2016:7172920
El Mourad MB, Arafa SK (2019) Effect of intravenous versus intraperitoneal magnesium sulfate on hemodynamic parameters and postoperative analgesia during laparoscopic sleeve gastrectomy—a prospective randomized study. J Anaesthesiol Clin Pharmacol 35:242–247
Kizilcik N, Koner O (2018) Magnesium sulfate reduced opioid consumption in obese patients undergoing sleeve gastrectomy: a prospective, randomized clinical trial. Obes Surg 28:2783–2788
De Oliveira GS, Duncan K, Fitzgerald P, Nader A, Gould RW, McCarthy RJ (2014) Systemic lidocaine to improve quality of recovery after laparoscopic bariatric surgery: a randomized double-blinded placebo-controlled trial. Obes Surg 24:212–218
Salama AK, Abdallah NM (2016) Multimodal analgesia with pregabalin and dexmedetomidine in morbidly obese patients undergoing laparoscopic sleeve gastrectomy: a prospective randomized double blind placebo controlled study. Egypt J Anaesth 32:293–298
Alimian M, Imani F, Faiz SH, Pournajafian A, Navadegi SF, Safari S (2012) Effect of oral pregabalin premedication on post-operative pain in laparoscopic gastric bypass surgery. Anesth Pain Med 2:12–16
Rupniewska-Ladyko A, Malec-Milewska M, Kraszewska E, Pirozynski M (2018) Gabapentin before laparoscopic sleeve gastrectomy reduces postoperative oxycodone consumption in obese patients: a randomized double-blind placebo-controlled trial. Minerva Anestesiol 84:565–571
Alkhamesi NA, Kane JM, Guske PJ, Wallace JW, Rantis PC (2008) Intraperitoneal aerosolization of bupivacaine is a safe and effective method in controlling postoperative pain in laparoscopic Roux-en-Y gastric bypass. J Pain Res 1:9–13
Omar I, Abualsel A (2019) Efficacy of intraperitoneal instillation of bupivacaine after bariatric surgery: randomized controlled trial. Obes Surg 29:1735–1741
Safari S, Rokhtabnak F, Djalali Motlagh S, Ghanbari Garkani M, Pournajafian A (2020) Effect of intraperitoneal bupivacaine on postoperative pain in laparoscopic bariatric surgeries. Surg Obes Relat Dis 16:299–305
Ruiz-Tovar J, Gonzalez J, Garcia A, Cruz C, Rivas S, Jimenez M, Ferrigni C, Duran M (2016) Intraperitoneal ropivacaine irrigation in patients undergoing bariatric surgery: a prospective randomized clinical trial. Obes Surg 26:2616–2621
Albrecht E, Kirkham KR, Endersby RV, Chan VW, Jackson T, Okrainec A, Penner T, Jin R, Brull R (2013) Ultrasound-guided transversus abdominis plane (TAP) block for laparoscopic gastric-bypass surgery: a prospective randomized controlled double-blinded trial. Obes Surg 23:1309–1314
Ruiz-Tovar J, Gonzalez G, Sarmiento A, Carbajo MA, Ortiz-de-Solorzano J, Castro MJ, Jimenez JM, Zubiaga L (2020) Analgesic effect of postoperative laparoscopic-guided transversus abdominis plane (TAP) block, associated with preoperative port-site infiltration, within an enhanced recovery after surgery protocol in one-anastomosis gastric bypass: a randomized clinical trial. Surg Endosc 34:5455–5460
Mittal T, Dey A, Siddhartha R, Nali A, Sharma B, Malik V (2018) Efficacy of ultrasound-guided transversus abdominis plane (TAP) block for postoperative analgesia in laparoscopic gastric sleeve resection: a randomized single blinded case control study. Surg Endosc 32:4985–4989
Carron M, De Cassai A, Linassi F, Navalesi P (2020) Multimodal analgesia in bariatric surgery: not just an intravenous approach. Surg Obes Relat Dis 16:2133–2135
Hamid HKS, Ahmed AY, Saber AA, Emile SH, Ibrahim M, Ruiz-Tovar J (2020) Transversus abdominis plane block using a short-acting local anesthetic reduces pain and opioid consumption after laparoscopic bariatric surgery: a meta-analysis. Surg Obes Relat Dis 16:1349–1357
Ruiz-Tovar J, Muñoz JL, Gonzalez J, Zubiaga L, García A, Jimenez M, Ferrigni C, Durán M (2017) Postoperative pain after laparoscopic sleeve gastrectomy: comparison of three analgesic schemes (isolated intravenous analgesia, epidural analgesia associated with intravenous analgesia and port-sites infiltration with bupivacaine associated with intravenous analgesia). Surg Endosc 31:231–236
Fuchs-Buder T, Schmartz D, Baumann C, Hilt L, Nomine-Criqui C, Meistelman C, Brunaud L (2019) Deep neuromuscular blockade improves surgical conditions during gastric bypass surgery for morbid obesity: a randomised controlled trial. Eur J Anaesthesiol 36:486–493
Torensma B, Martini CH, Boon M, Olofsen E, In’t Veld B, Liem RS, Knook MT, Swank DJ, Dahan A (2016) Deep neuromuscular block improves surgical conditions during bariatric surgery and reduces postoperative pain: a randomized double blind controlled trial. PLoS One 11:e0167907
Gaszynski T, Szewczyk T, Gaszynski W (2012) Randomized comparison of sugammadex and neostigmine for reversal of rocuronium-induced muscle relaxation in morbidly obese undergoing general anaesthesia. Br J Anaesth 108:236–239
Carron M, Veronese S, Foletto M, Ori C (2013) Sugammadex allows fast-track bariatric surgery. Obes Surg 23:1558–1563
Castro DS Jr, Leão P, Borges S, Gomes L, Pacheco M, Figueiredo P (2014) Sugammadex reduces postoperative pain after laparoscopic bariatric surgery: a randomized trial. Surg Laparosc Endosc Percutan Tech 24:420–423
Writing Committee for the PROBESE Collaborative Group of the PROtectiveVEntilation Network (PROVEnet) for the Clinical Trial Network of the European Society of Anaesthesiology, Bluth T, Serpa Neto A, Schultz MJ, Pelosi P, Gama de Abreu M; PROBESE Collaborative Group, Bluth T, Bobek I, Canet JC, Cinnella G, de Baerdemaeker L, Gama de Abreu M, Gregoretti C, Hedenstierna G, Hemmes SNT, Hiesmayr M, Hollmann MW, Jaber S, Laffey J, Licker MJ, Markstaller K, Matot I, Mills GH, Mulier JP, Pelosi P, Putensen C, Rossaint R, Schmitt J, Schultz MJ, Senturk M, Serpa Neto A, Severgnini P, Sprung J, Vidal Melo MF, Wrigge H (2019) Effect of intraoperative high positive end-expiratory pressure (PEEP) with recruitment maneuvers vs low PEEP on postoperative pulmonary complications in obese patients: a randomized clinical trial. JAMA 321:2292–2305
Ball L, Hemmes SNT, Serpa Neto A, Bluth T, Canet J, Hiesmayr M, Hollmann MW, Mills GH, Vidal Melo MF, Putensen C, Schmid W, Severgnini P, Wrigge H, Gama de Abreu M, Schultz MJ, Pelosi P, LAS VEGAS investigators; PROVE Network; Clinical Trial Network of the European Society of Anaesthesiology (2018) Intraoperative ventilation settings and their associations with postoperative pulmonary complications in obese patients. Br J Anaesth 121:899–908
O’Gara B, Talmor D (2018) Perioperative lung protective ventilation. BMJ 2018(362):k3030
Nguyen NT, Wolfe BM (2005) The physiologic effects of pneumoperitoneum in the morbidly obese. Ann Surg 241:219–226
Atkinson TM, Giraud GD, Togioka BM, Jones DB, Cigarroa JE (2017) Cardiovascular and ventilatory consequences of laparoscopic surgery. Circulation 135:700–710
Costa Souza GM, Santos GM, Zimpel SA, Melnik T (2020) Intraoperative ventilation strategies for obese patients undergoing bariatric surgery: systematic review and meta-analysis. BMC Anesthesiol 20:36
Schol PB, Terink IM, Lancé MD, Scheepers HC (2016) Liberal or restrictive fluid management during elective surgery: a systematic review and meta-analysis. J Clin Anesth 35:26–39
Pösö T, Kesek D, Aroch R, Winsö O (2013) Morbid obesity and optimization of preoperative fluid therapy. Obes Surg 23:1799–1805
Schuster R, Alami RS, Curet MJ, Paulraj N, Morton JM, Brodsky JB, Brock-Utne JG, Lemmens HJ (2006) Intra-operative fluid volume influences postoperative nausea and vomiting after laparoscopic gastric bypass surgery. Obes Surg 16:848–851
Brienza N, Biancofiore G, Cavaliere F, Corcione A, De Gasperi A, De Rosa RC, Fumagalli R, Giglio MT, Locatelli A, Lorini FL, Romagnoli S, Scolletta S, Tritapepe L (2019) Clinical guidelines for perioperative hemodynamic management of non-cardiac surgical adult patients. Minerva Anestesiol 85:1315–1333
Demirel İ, Bolat E, Altun AY, Özdemir M, Beştaş A (2018) Efficacy of goal-directed fluid therapy via pleth variability index during laparoscopic Roux-en-Y gastric bypass surgery in morbidly obese patients. Obes Surg 28:358–363
Jain AK, Dutta A (2010) Stroke volume variation as a guide to fluid administration in morbidly obese patients undergoing laparoscopic bariatric surgery. Obes Surg 20:709–715
Muñoz JL, Gabaldón T, Miranda E, Berrio DL, Ruiz-Tovar J, Ronda JM, Esteve N, Arroyo A, Pérez A (2016) Goal-directed fluid therapy on laparoscopic sleeve gastrectomy in morbidly obese patients. Obes Surg 26:2648–2653
Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American society of Anesthesiologists task force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration (2017) Anesthesiology 126:376–393
Salmasi V, Maheshwari K, Yang D, Mascha EJ, Singh A, Sessler DI, Kurz A (2017) Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology 126:47–65
Difficult Airway Society Extubation Guidelines Group, Popat M, Mitchell V, Dravid R, Patel A, Swampillai C, Higgs A (2012) Difficult Airway Society Guidelines for the management of tracheal extubation. Anaesthesia 67:318–340
Members of the Working Party, Nightingale CE, Margarson MP, Shearer E, Redman JW, Lucas DN, Cousins JM, Fox WT, Kennedy NJ, Venn PJ, Skues M, Gabbott D, Misra U, Pandit JJ, Popat MT, Griffiths R; Association of Anaesthetists of Great Britain; Ireland Society for Obesity and Bariatric Anaesthesia (2015) Peri-operative management of the obese surgical patient 2015: Association of Anaesthetists of Great Britain and Ireland Society for Obesity and Bariatric Anaesthesia. Anaesthesia 70:859–876
Rochwerg B, Einav S, Chaudhuri D, Mancebo J, Mauri T, Helviz Y, Goligher EC, Jaber S, Ricard JD, Rittayamai N, Roca O, Antonelli M, Maggiore SM, Demoule A, Hodgson CL, Mercat A, Wilcox ME, Granton D, Wang D, Azoulay E, Ouanes-Besbes L, Cinnella G, Rauseo M, Carvalho C, Dessap-Mekontso A, Fraser J, Frat JP, Gomersall C, Grasselli G, Hernandez G, Jog S, Pesenti A, Riviello ED, Slutsky AS, Stapleton RD, Talmor D, Thille AW, Brochard L, Burns KEA (2020) The role for high flow nasal cannula as a respiratory support strategy in adults: a clinical practice guideline. Intensive Care Med 46:2226–2237
Zaremba S, Shin CH, Hutter MM, Malviya SA, Grabitz SD, MacDonald T, Diaz-Gil D, Ramachandran SK, Hess D, Malhotra A, Eikermann M (2016) Continuous positive airway pressure mitigates opioid-induced worsening of sleep-disordered breathing early after bariatric surgery. Anesthesiology 125:92–104
Nelson R, Edwards S, Tse B (2007) Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev 2007:CD004929
Petrowsky H, Demartines N, Rousson V, Clavien PA (2004) Evidence-based value of prophylactic drainage in gastrointestinal surgery: a systematic review and meta-analyses. Ann Surg 240:1074–1084
Liscia G, Scaringi S, Facchiano E, Quartararo G, Lucchese M (2014) The role of drainage after Roux-en-Y gastric bypass for morbid obesity: a systematic review. Surg Obes Relat Dis 10:171–176
Kavuturu S, Rogers AM, Haluck RS (2012) Routine drain placement in Roux-en-Y gastric bypass: an expanded retrospective comparative study of 755 patients and review of the literature. Obes Surg 22:177–181
Hoehn RS, Seitz AP, Singer KE, Thompson JR, Watkins BM (2019) Enhanced recovery protocol for laparoscopic sleeve gastrectomy: Are narcotics necessary? J Gastrointest Surg 23:1541–1546
Ronellenfitsch U, Schwarzbach M, Kring A, Kienle P, Post S, Hasenberg T (2012) The effect of clinical pathways for bariatric surgery on perioperative quality of care. Obes Surg 22:732–739
Saint S, Lipsky BA (1999) Preventing catheter-related bacteriuria: should we? Can we? How? Arch Intern Med 159:800–808
Klevens RM, Edwards JR, Richards CL Jr, Horan TC, Gaynes RP, Pollock DA, Cardo DM (2007) Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep 122:160–166
Taylor J, Canner J, Cronauer C, Prior D, Coker A, Nguyen H, Magnuson T, Adrales G, Schweitzer M (2020) Implementation of an enhanced recovery program for bariatric surgery. Surg Endosc 34:2675–2681
Małczak P, Wysocki M, Twardowska H, Dudek A, Tabiś J, Major P, Pisarska M, Pędziwiatr M (2020) Impact of adherence to the ERAS® protocol on short-term outcomes after bariatric surgery. Obes Surg 30:1498–1505
Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery: a review. JAMA Surg 152:292–298
Major P, Stefura T, Małczak P, Wysocki M, Witowski J, Kulawik J, Wierdak M, Pisarska M, Pędziwiatr M, Budzyński A (2018) Postoperative care and functional recovery after laparoscopic sleeve gastrectomy vs. laparoscopic Roux-en-Y gastric bypass among patients under ERAS protocol. Obes Surg 28:1031–1039
Balla A, Batista Rodríguez G, Corradetti S (2017) Outcomes after bariatric surgery according to large databases: a systematic review. Langenbecks Arch Surg 402:885–899
Ardila-Gatas J, Sharma G, Lloyd SJ, Khorgami Z, Tu C, Schauer PR, Brethauer SA, Aminian A (2019) A nationwide safety analysis of discharge on the first postoperative day after bariatric surgery in selected patients. Obes Surg 29:15–22
Chiappetta S, Jamadar P, Stier C, Bottino V, Weiner RA, Runkel N (2020) The role of C-reactive protein after surgery for obesity and metabolic disorders. Surg Obes Relat Dis 16:99–108
Muñoz JL, Ruiz-Tovar J, Miranda E, Berrio DL, Moya P, Gutiérrez M, Flores R, Picó C, Pérez A (2016) C-Reactive protein and procalcitonin as early markers of septic complications after laparoscopic sleeve gastrectomy in morbidly obese patients within an enhanced recovery after surgery program. J Am Coll Surg 222:831–837
Bona D, Micheletto G, Bonitta G, Panizzo V, Cavalli M, Rausa E, Cirri S, Aiolfi A (2019) Does C-reactive protein have a predictive role in the early diagnosis of postoperative complications after bariatric surgery? Systematic review and Bayesian meta-analysis. Obes Surg 29:3448–3456
Lee Y, McKechnie T, Doumouras AG, Handler C, Eskicioglu C, Gmora S, Anvari M, Hong D (2019) Diagnostic value of C-reactive protein levels in postoperative infectious complications after bariatric surgery: a systematic review and meta-analysis. Obes Surg 29:2022–2029
Williams M, McMeekin S, Wilson J, Miller G, Langlands F, Wong W, Peter M, Giles M (2017) Predictive value of C-reactive protein for complications post-laparoscopic Roux-En-Y Gastric bypass-author reply. Obes Surg 27:2462–2463
Kassir R, Blanc P, Bruna Tibalbo LM, Breton C, Lointier P (2015) C-Reactive protein and procalcitonin for the early detection of postoperative complications after sleeve gastrectomy: preliminary study in 97 patients. Surg Endosc 29:1439–1444
Williams MR, McMeekin S, Wilson RJ, Miller GV, Langlands FE, Wong W, Peter M, Giles MS (2017) Predictive value of C-reactive protein for complications post-laparoscopic Roux-En-Y Gastric bypass. Obes Surg 27:709–715
Williams M, Langlands F, Giles M (2020) Does C-reactive protein day 1 post-surgery have a predictive role for post-operative complications: a single-centre perspective following published meta-analysis. Obes Surg 30:347–348
Rebibo L, Cosse C, Robert B, Chivot C, Yzet T, Dhahri A, Regimbeau JM (2017) Eliminating routine upper gastrointestinal contrast studies after sleeve gastrectomy decreases length of stay and hospitalization costs. Surg Obes Relat Dis 13:553–559
Rahman U, Docimo S, Pryor AD, Bates A, Obeid NR, Spaniolas K (2018) Routine contrast imaging after bariatric surgery and the effect on hospital length of stay. Surg Obes Relat Dis 14:517–520
Diaz Vico T, Elli EF (2019) Utility of immediate postoperative upper gastrointestinal contrast study in bariatric surgery. Obes Surg 29:1130–1133
Brockmeyer JR, Simon TE, Jacob RK, Husain F, Choi Y (2012) Upper gastrointestinal swallow study following bariatric surgery: institutional review and review of the literature. Obes Surg 22:1039–1043
Quartararo G, Facchiano E, Scaringi S, Liscia G, Lucchese M (2014) Upper gastrointestinal series after Roux-en-Y gastric bypass for morbid obesity: effectiveness in leakage detection. a systematic review of the literature. Obes Surg 24:1096–1101
Leepalao MC, Arredondo D, Speights F, Duncan TD (2020) Same-day discharge on laparoscopic Roux-en-Y gastric bypass patients: an outcomes review. Surg Endosc 34:3614–3617
Aftab H, Fagerland MW, Gondal G, Ghanima W, Olsen MK, Nordby T (2019) Gastric sleeve resection as day-case surgery: what affects the discharge time? Surg Obes Relat Dis 15:2018–2024
Inaba CS, Koh CY, Sujatha-Bhaskar S, Pejcinovska M, Nguyen NT (2018) How safe is same-day discharge after laparoscopic sleeve gastrectomy? Surg Obes Relat Dis 14:1448–1453
Inaba CS, Koh CY, Sujatha-Bhaskar S, Zhang L, Nguyen NT (2018) Same-day discharge after laparoscopic Roux-en-Y gastric bypass: an analysis of the metabolic and bariatric surgery accreditation and quality improvement program database. J Am Coll Surg 226:868–873
Leeman M, van Mil SR, Biter LU, Apers JA, Verhoef K, Dunkelgrun M (2021) Reducing complication rates and hospital readmissions while revising the enhanced recovery after bariatric surgery (ERABS) protocol. Surg Endosc 35:612–619
Patil S, Cornett EM, Jesunathadas J, Belani K, Fox CJ, Kaye AD, Lambert LA, Urman RD (2019) Implementing enhanced recovery pathways to improve surgical outcomes. J Anaesthesiol Clin Pharmacol 35(Suppl 1):S24–S28
Acknowledgements
The authors acknowledge Medtronic as the sponsor of the meeting organized in order to realize the activities.
Funding
Open access funding provided by Università degli Studi di Padova within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs Giuseppe Marinari, Mirto Foletto, Carlo Nagliati, Giuseppe Navarra, Vincenzo Borrelli, Vincenzo Bruni, Giovanni Fantola, Roberto Moroni, Luigi Tritapepe, Roberta Monzani, Daniela Sanna, Michele Carron, Rita Cataldo have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Marinari, G., Foletto, M., Nagliati, C. et al. Enhanced recovery after bariatric surgery: an Italian consensus statement. Surg Endosc 36, 7171–7186 (2022). https://doi.org/10.1007/s00464-022-09498-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09498-y