Abstract
Background
This is the second updated Enhanced Recovery After Surgery (ERAS®) Society guideline, presenting a consensus for optimal perioperative care in bariatric surgery and providing recommendations for each ERAS item within the ERAS® protocol.
Methods
A principal literature search was performed utilizing the Pubmed, EMBASE, Cochrane databases and ClinicalTrials.gov through December 2020, with particular attention paid to meta-analyses, randomized controlled trials and large prospective cohort studies. Selected studies were examined, reviewed and graded according to the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) system. After critical appraisal of these studies, the group of authors reached consensus regarding recommendations.
Results
The quality of evidence for many ERAS interventions remains relatively low in a bariatric setting and evidence-based practices may need to be extrapolated from other surgeries.
Conclusion
A comprehensive, updated evidence-based consensus was reached and is presented in this review by the ERAS® Society.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of bariatric surgery in the treatment for severe obesity has several benefits in terms of sustainable weight loss, improvements or resolution of several metabolic comorbidities as well as improved life expectancy [1, 2]. These benefits, in combination with continuously reducing complication rates, have led the way to a marked increase in the demand for bariatric surgical procedures worldwide [3].
The use of a multimodal stress-minimizing approach can reduce the rates of morbidity after major gastrointestinal surgery [4] and may shorten functional recovery as well as length-of-stay (LOS) in bariatric surgery [5, 6]. A first version of evidence-based guidelines for the perioperative care of patients undergoing bariatric surgery was published by the Enhanced Recovery After Surgery (ERAS) Society in 2016 [7]. Given the continued increase in bariatric surgery being performed worldwide, as well as the increasing popularity of novel surgical techniques, the evidence underpinning the recommendations is continuously evolving. Therefore, clinical guidelines need to be challenged and updated on a regular basis.
This document represents an updated consensus-based review of perioperative care for bariatric surgery based on best currently available evidence.
Methods
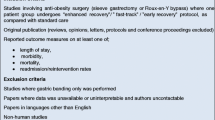
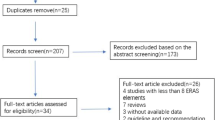
Based on the first version of the ERAS Society guidelines for bariatric surgery published in 2016, the first and last author reviewed previous topics for a new update or removal and considered new topics for inclusion [7]. International authors with diverse expertise in the perioperative care of patients undergoing bariatric surgery (including surgery, anaesthesiology and nutrition) were invited by the ERAS Society to participate. All authors received instructions for the literature search and quality assessment [8].
Search terms and sources
A principal literature search was performed utilizing the Pubmed, EMBASE, Cochrane databases and ClinicalTrials.gov through December 2020. Keywords included “obesity”, “morbid obesity”, “bariatric surgery”, “metabolic surgery”, “gastric bypass”, “sleeve gastrectomy”, one anastomosis gastric bypass”, “mini gastric bypass”, “gastric banding”, “fast track”, and “enhanced recovery”. Medical subheading terms were used as were accompanying entry terms for patient groups, interventions and outcomes. The references of each relevant study were also scrutinized for additional eligible studies. Meta-analyses of randomized controlled trials (RCTs) or observational studies, RCTs, and large cohort studies were eligible for inclusion. Retrospective, smaller cohort studies were considered when no higher-level evidence was available.
Grading of evidence and recommendations
The quality of evidence supporting each recommendation was reviewed by one or two authors in conjunction with the first and last author. The Cochrane checklist was used to assess the methodological quality of each study [9]. The quality of evidence overall was then evaluated using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) system [10]. The level of evidence was categorized into four categories, high, moderate, low, or very low in accordance with the GRADE system [11].
The strength of the recommendations was likewise evaluated using the GRADE system. To generate strength of recommendations, all authors reviewed each recommendation with the accompanying evidence and GRADE rating of quality. The strength of each recommendation was determined by all authors and, if there was disagreement regarding the strength, a Delphi process was undertaken to reach consensus.
The criteria for rating strength of recommendations were as follows:
Strong recommendation The panel is confident that the desirable effects of adherence to the recommendation outweigh the undesirable effects.
Weak recommendation: The desirable effects to adherence to the recommendation probably outweigh the undesirable effects, but the panel is less confident.
Results: evidence base and recommendations
The evidence and recommendations for ERAS items are presented in four different headings: preadmission, preoperative, intraoperative and postoperative and are numbered in the order they are to be used in clinical practice. Summary tables, Tables 1, 2, 3, 4, show an overview of the quality of evidence and grade of recommendation for each item.
Preadmission items
Information, education and counselling
The patient scheduled for bariatric surgery must be well informed of the impact of extensive changes associated with life after bariatric surgery. They must be motivated and willing to participate in the long-term care, change in dietary patterns and to embrace the revised lifestyle after the operation. A preoperative educational program is often recommended in order to ensure realistic expectations, and to reduce anxiety, wound complications, postoperative pain and LOS [7, 12,13,14,15,16]. Results however, remain ambivalent. In a meta-analysis covering patients undergoing cancer surgery, education reduced anxiety and health care costs while simultaneously increasing the knowledge and satisfaction of patients [17]. A more recent RCT of 73 patients with colorectal cancer, reported improved body image after surgery and enhanced recovery of self-reported global health status and reduced LOS after extra preoperative group education [18]. However, meta-analyses on education for patients undergoing elective spinal surgery as well as a cluster RCT in patients undergoing visceral surgery did not report any sustained benefit on the majority of clinical outcome [19, 20]. The educational intervention proves hard to standardize, and there is a paucity in research assessing its benefits for bariatric surgery.
While the grade of evidence remains low, a formal psycho-social evaluation including environmental, familiar, nutritional and behavioural factors in line with current recommendations from the American Society for Metabolic and Bariatric Surgery (ASMBS) should be performed prior to bariatric surgery [21].
Despite the low grade of evidence, preoperative information and education are strongly recommended as a necessary step of informed consent in order to improve knowledge, ensure adequate risk perception, and allow active patient participation in making well-informed choices (Table 1).
Indications and contraindications for surgery
The current indications for bariatric surgery are BMI ≥ 40 kg/m2 alone or BMI ≥ 35 kg/m2 and an obesity-related comorbidity that could be expected to improve/resolve by surgery-induced weight loss maintenance. These were established in a consensus meeting in 1991 and subsequently confirmed by more recent guidelines [22, 23]. The major addition to the indications for bariatric or rather, metabolic surgery, has been provided by the international consensus conference of Diabetes Surgery Summit, established in 2007 recommending the use of gastrointestinal surgery to treat type-2 diabetes mellitus (T2D), including individuals with class-I obesity. The joint statement by international diabetes organizations in 2016 recommends that metabolic surgery should be considered as an option to treat T2D in patients with class-I obesity (BMI 30.0–34.9 kg/m2) and inadequately controlled hyperglycaemia despite optimal medical treatment [24] (Table 1).
Preoperative optimization
Smoking and alcohol cessation
Cessation of smoking at least 4–8 weeks before surgery reduces postoperative complications after non-bariatric surgery, in particular wound and cardiovascular complications [25]. For bariatric surgery, smoking has been associated with increased risk of marginal ulcers, infectious and respiratory complications [26, 27]. Although there is a lack of RCTs addressing smoking cessation prior to bariatric surgery, a recent systematic review of 28 non-RCTs [28] reported a reduction in postoperative morbidity. While the optimal timing of cessation remains unknown, an intervention beginning at least 4 weeks before surgery including weekly counselling and use of nicotine replacement therapy is the most likely approach to impact complications and long-term smoking cessation [29]. Despite best efforts, achieving cessation appears to be difficult, in particular in the long term [30] (Table 1).
High alcohol consumption can increase the risk of postoperative complications—mainly infectious and related to wound healing [31]. The effect of preoperative alcohol cessation was addressed in a Cochrane review including three RCTs with a combined total of 140 patients who underwent colorectal or orthopaedic surgery. The pooled estimate from these studies suggested a significant reduction in risk (RR 0.62, 95%CI 0.40–0.96) for postoperative complications following preoperative counselling and a short, but intensive intervention for patients with increased consumption [32]. The complex nature of mandatory behavioural changes in combination with an increased risk of postoperative alcohol overconsumption and dependency in particular for patients with previous substance abuse, is the basis for the current recommendations of a 1–2 year period of documented alcohol abstinence for patients with earlier overconsumption [33]. The level of evidence for this recommendation remains low (Table 1).
Preoperative weight loss
In contrast to so-called Insurance-mandated preoperative weight loss programs, a 2–4 week period of Low Calorie Diet (LCD, 1000–1200 kcal/d) or Very Low Calorie Diet (VLCD, 800 kcal/d) is usually recommended prior to bariatric surgery. This regimen has been shown to reduce liver volume and a surgeon´s perceived complexity of the procedure [34, 35]. Furthermore, VLCD for two weeks is associated with improved whole-body insulin sensitivity as demonstrated in another RCT [36]. In a previous systematic review which included 11 non-randomized patient cohorts, preoperative weight loss was associated with reduced postoperative complications [37], which has later been confirmed in one RCT and two large retrospective studies [38,39,40]. The effect may be more pronounced in patients with a higher BMI [40].
However, two recent meta-analyses and one retrospective study failed to demonstrate the effect of diet on postoperative morbidity [41, 42], but one of the meta-analyses reported a statistically significant (27%) reduction in LOS in patients submitted to preoperative weight loss [43].
An improvement in postoperative weight loss in patients who lost weight preoperatively has been reported from observational studies [39, 44]. The effect of preoperative weight loss was also evaluated in an ERAS setting showing reduced operating time as well as improved postoperative weight loss [41]. There also seems to be an improvement in postoperative weight loss in patients who achieve preoperative weight loss > 10% [39, 44].
The effect of preoperative weight loss in patients with obesity and T2D has not been specifically addressed in any RCT or large retrospective study.
The optimal composition of preoperative low-calorie diet is yet to be determined. Most protocols adhere to a commercially available composition, but data from comparisons between these are sparse [45].
Overall, there is high level of evidence that 2–4 weeks of either a LCD or a VLCD reduces liver volume, moderate evidence of a reduction of postoperative complications, and low-quality evidence of postoperative weight loss (Table 1).
Prehabilitation and exercise
The concept of prehabilitation includes interventions aiming at increasing physical functioning before surgery, which in turn may improve recovery and reduce morbidity postoperatively. In a recent meta-analysis, including all RCTs in patients undergoing various types of abdominal surgery published between 1966 and 2017, a reduction in overall postoperative morbidity in the prehabilitation group (OR 0.63, 95%CI 0.46–0.87) with a composite pulmonary morbidity endpoint (OR 0.40, 95%CI 0.23–0.68), and borderline significance for reduction in LOS was seen [46]. There was a heterogeneity between protocols with a length of the preoperative interventions between 2 and 4 weeks. No difference was found for the six-minute walking test. However, a previous meta-analysis indicated that complications as well as LOS were reduced in patients undergoing prehabilitation [47].
Some relatively small RCTs have addressed the effect of prehabilitation in patients scheduled for bariatric surgery. A 12-week exercise program including endurance training was associated with reduced weight, cardiometabolic risk factors as well as improved general physical fitness [48, 49]. A 6-week preoperative training was also associated with maintained improvement in physical activity 6 months postoperatively [50]. Specific inspiratory muscular training preoperatively improved immediate (12 h) postoperative oxygenation and increased inspiratory muscular strength [50]. None of these studies have reported outcome in terms of recovery or morbidity.
Although prehabilitation is a promising intervention which seems to have the potential to reduce morbidity in some surgical settings, the extrapolation of the results to patients undergoing bariatric surgery remains questionable (Table 1).
Preoperative items
Supportive pharmacological intervention
In order to reduce the stress response during and after surgery, several pharmacological interventions have been suggested, as described below.
Glucocorticoids
Glucocorticoids are known for their anti-inflammatory properties, thus potentially reducing the perioperative stress response. In patients undergoing surgery for gastrointestinal cancer, corticosteroids administered preoperatively or following induction of anaesthesia has been associated with fewer complications and a milder systemic inflammatory response (SIR) [51, 52]. In elective surgery for inflammatory bowel disease, a single dose of 8 mg dexamethasone upon induction of anaesthesia reduced postoperative ileus, the intensity of postoperative pain, and LOS [53]. Perioperative dexamethasone for total joint arthroplasty patients was also associated with reduced LOS, postoperative pain and stress response as reported in one meta-analysis including 17 RCTs [54]. A single dose of dexamethasone seems safe as the side effects were limited to a physiological rise in blood glucose levels [54]. Furthermore, previous systematic reviews and meta-analyses have demonstrated that administration of dexamethasone preoperatively did not increase postoperative (wound or systemic) infections or anastomotic leakage [55,56,57]. There is still a paucity of studies reporting the perioperative use of dexamethasone in bariatric surgery.
Statins
In a systematic review, perioperative use of statins in patients undergoing various types of abdominal surgery was associated with reduced mortality, systemic infection and anastomotic leak [58]. Subsequent cohort studies further confirmed the association between perioperative statin usage and a reduction of postoperative complications [59,60,61,62,63,64]. However, two RCTs comparing statins vs placebo in patients undergoing non-cardiac surgery and major colorectal surgery found no difference in postoperative complications [65, 66], although simvastatin attenuated the early proinflammatory response to surgery after colorectal surgery [65]. Furthermore, a meta-analysis of 5 RCTs found no evidence for statins to reduce the postoperative risk of infection [67]. Literature on statin use in bariatric surgery specifically is absent. Routine perioperative administration of statins to patients undergoing bariatric surgery for prevention of complications is therefore not recommended.
Beta-blockade
It has been hypothesized that beta-blockers, by decreasing the effect of surgical stress on the heart, can reduce complications such as myocardial infarction, stroke and cardiac arrhythmias. The most recent meta-analysis of 83 RCTs, including an international multicentre trial in which a potential harmful effect (increased mortality and risk of stroke) was detected for preoperative use of metoprolol, also reported low-certainty evidence for a reduction in atrial fibrillation and myocardial infarction after beta-blocker usage in non-cardiac surgery [68, 69]. Bradycardia and hypotension were both increased with low- and moderate-certainty level evidence, respectively. The evidence for early all-cause mortality was uncertain. Subsequent cohort studies assessing the continuous use of beta-blockers in gastrointestinal cancer surgery reported decreased risk of postoperative cardiovascular complications, anastomotic leakage and sepsis and reduced mortality rates at 90-days and 1-year after surgery [70, 71]. Only one retrospective study assessed the association between preoperative beta-blocker therapy and postoperative outcome for patients undergoing laparoscopic RYGB. There was no evidence for a beneficial effect on moderate- and long-term survival and postoperative complications [72]. At present, it is not recommended to routinely use perioperative beta-blockers in patients undergoing bariatric surgery. However, patients at high risk of cardiovascular events who are already on beta-blockade can safely continue this treatment through the perioperative process [73].
Preoperative fasting
Previous studies have demonstrated no differences in residual gastric fluid volume (RGFV), pH [74, 75] or gastric emptying rates following an intake of semi-solid meals [76, 77] or drinks [78] in patients with obesity when compared to patients with normal weight. No differences were found in RGFV and pH in a RCT of patients with severe obesity who drank 300 ml of clear fluid 2 h before induction of anaesthesia, compared with those who fasted after midnight [79, 80]. RGFV and pH were also similar following an overnight fast in patients with obesity and diabetes (with and without autonomic neuropathy) compared with controls without diabetes [80,81,82].
While the level of evidence remains low, preoperative fasting for solids (equivalent to a light meal) of at least 6 h and clear fluids of 2 h before induction of anaesthesia is recommended, if there are no contraindications (Table 2).
Carbohydrate loading
Preoperative carbohydrate conditioning, using iso-osmolar drinks (CHO) ingested 2–3 h before induction of anaesthesia, attenuated development of postoperative insulin resistance, reduced postoperative nitrogen and protein losses and maintained lean body mass [83]. Two meta-analyses demonstrated CHO to be associated with reduction in hospital LOS by about 1 day after major abdominal surgery [84, 85]. A similar reduction was reported from a small RCT of 20 patients undergoing SG [86]. When CHO were administered to patients with T2D (mean BMI 28.6 kg/m2), no differences were noted in gastric emptying times compared with healthy subjects [87]. However, postprandial glucose concentrations reached a higher peak and were elevated for longer time in patients with diabetes [87]. In addition, CHO did not lead to an increase in aspiration-related complications in patients undergoing laparoscopic RYGB, even in patients with diabetes and delayed gastric emptying [88,89,90]. Two further studies have used CHO in bariatric surgery within an enhanced recovery pathway [91, 92]. In a RCT comparing enhanced recovery versus standard care in bariatric patients (including CHO), no differences in overall complication rate were noted [91]. In addition, compliance with CHO was only 15% [91]. Another study of 90 patients randomized to either carbohydrate-rich drink, protein-rich drink or tap water did not show any effect on nausea after gastric bypass surgery [93].
Currently, there is insufficient evidence to support routine use of preoperative carbohydrate loading in bariatric surgery (Table 2).
Prevention of nausea and vomiting
Patients undergoing bariatric surgery are frequently female and non-smokers, undergoing laparoscopic or robotic procedures of more than one hour in duration and receive perioperative opioid analgesia—all of which are risk factors for PONV. Gastric surgery, history of acid reflux and reduction in gastric size, in particular after sleeve gastrectomy may further contribute to PONV [94,95,96].
Recent guidelines recommend a multimodal approach including total intravenous anaesthesia with Propofol (TIVA), avoidance of volatile anaesthetics and fluid overload, and minimization of intra- and postoperative opioids [97].
Compared to volatile opioid anaesthesia with opioids, opioid-free TIVA was associated with a significantly lower rate and severity of PONV in a RCT including 119 patients [98]. In addition, one antiemetic agent from three of the following six classes is recommended: 5-hydroxytryptamine receptor antagonists, long-acting corticosteroid like dexamethasone, butyrophenones, neurokinin-1 receptor antagonists, antihistamines and anticholinergics [99]. In addition, multimodal analgesia and regional anaesthesia techniques are recommended, as opioid-sparing strategies to further reduce the risk of PONV [99].
The evidence for a multimodal PONV regimen based on current RCTs is strong, but there are limited data on the use of TIVA (Table 2).
Intraoperative items
Perioperative fluid management
Obesity can cause changes in different fluid compartments and affect body composition, leading to an increase in absolute fluid volume and subsequently in cardiac output [100]. Therefore, it remains a challenge in the perioperative period to estimate fluid requirements needed to maintain normovolemia and hence optimized tissue perfusion and oxygenation.
Intraoperative hyper- as well as hypovolemia is associated with worse outcome [101,102,103]. There is some evidence to suggest that restrictive fluid administration in both non-bariatric [104] and bariatric surgery [105] can increase complications as well as LOS and mortality. On the other hand, high intravenous volume of fluids administered on the day of surgery is associated with increased LOS as well [106].
At present, individualized goal-directed fluid therapy (GDFT) is the most effective way to optimize cardiac performance and to improve oxygen delivery in the perioperative period [107].
In a RCT of 60 patients undergoing laparoscopic bariatric surgery, GDFT was associated with improved tissue oxygenation in the early postoperative period [108]. Additionally, GDFT guided by stroke volume optimization according to arterial pressure waveform analysis or by Pleth Variability Index (PVI) can decrease the incidence of postoperative nausea and vomiting and shorten hospital LOS [109]. GDFR can continue in the surgical ward guided by non-invasive measurements [21].
Regarding the type of fluid, crystalloids leave the circulation more quickly than colloids, and therefore, may increase the risk of tissue oedema and impaired tissue oxygenation [110]. The intravascular effects of colloids are context-sensitive and therefore affected by fluid status [111]. During hypovolemia, colloids remain longer intravascularly [112] and might consequently better maintain hemodynamic stability, which might in turn lead to improved tissue perfusion and oxygenation [113, 114]. There is a paucity of studies comparing crystalloid and colloid solution in bariatric surgery. No difference in intra- and postoperative subcutaneous tissue oxygen tension (PsqO2) [107], cytokine and inflammatory marker levels [115], or postoperative complications [116] has been seen when comparing crystalloids with colloids or hydroxyethyl starch during abdominal surgery. Data from several RCTs suggest the benefit of using balanced crystalloids and limiting the use of 0.9% normal saline [117,118,119].
There is moderate evidence supporting an individual goal-directed fluid therapy, avoiding both restrictive and liberal strategies (Table 3).
Standardized anaesthetic protocol
Short-acting agents and minimal opioid use during the operation is of importance to enhance recovery. Anaesthesia induction should preferably be based on lean body weight to avoid hypotension [120], while using TBW may be more appropriate for a maintenance infusion [121]. Classic target-controlled infusion (TCI) models have poor predictive ability when used in patients with obesity [122]. Propofol is the most frequently used induction agent, and it has not be shown to increase the incidence of propofol infusion syndrome-related rhabdomyolysis in patients with severe obesity during standard bariatric surgery [123]. If volatile anaesthetics are used for maintenance, desflurane may offer faster wake up times compared to sevoflurane or isoflurane in patients with a BMI > 30 kg/m2 [124]. However, unlike sevoflurane with its bronchodilator effects, desflurane can induce increased airway resistance as well as hypertension and tachycardia. The decision regarding which inhalational agent to use should therefore be determined based on existing comorbidities and other related factors.
Bispectral index (BIS) represents one of several ways to monitor depth of anaesthesia, with the goal of decreasing intraoperative awareness and reducing the amount of administered anaesthetic [125]. For monitoring of intraoperative awareness, BIS or end-tidal anaesthetic gas (ETAG) monitoring might be used. Both of these have been shown to similarly reduce rates of intraoperative awareness compared to using only clinical signs [125, 126].
Patients with obesity generally show an increased sensitivity towards opioid sedative effects and consequently higher susceptibility towards respiratory depression [127]. In an effort to reduce the incidence and severity of postsurgical pain, multimodal analgesia using limited doses of opioids has been advocated [128,129,130]. Lidocaine, dexmedetomidine, ketamine and magnesium, when used as part of opioid-free anaesthesia, may have better anti-inflammatory effects than classical opioid-based anaesthesia and may therefore be preferable [131]. In addition, appropriate use of nonsteroidal anti-inflammatory drugs (NSAIDs) reduces opioid consumption [132, 133]. One limitation of most NSAIDs is that they are “low-ceiling” analgesics. Paracetamol is free of bleeding, gastric and renal side effects that limit the use of NSAIDs.
Regional anaesthetic techniques have been demonstrated to be highly efficient in reducing opioid requirements. Epidural analgesia for postoperative pain is effective but is not required in laparoscopic surgery. Ultrasound-guided transversus abdominis plane block can decrease pain scores and opioid requirement, and improve ambulation after bariatric surgery [134]. Infiltration of bupivacaine 0.5% before incision results in a reduction in opioid consumption and postoperative pain [135]. Other promising strategies are intraperitoneal instillation of bupivacaine [136] and erector spinae plane block [137].
Although current evidence does not allow recommending of specific anaesthetic agents or techniques, there is high level of evidence in support of using multimodal, opioid-sparing analgesia approaches to improve postoperative recovery (Table 3).
Airway management
Some studies have reported an association between severe obesity and difficult intubation [138]. In a comprehensive analysis of a single centre experience, the overall incidence of difficult intubation in patients with severe obesity was 4.2% and difficult mask ventilation 2.9% [139]. Factors associated with difficult intubation were age > 46 years, male gender, airway class 3–4 according to the Mallampatti score, thyromental distance (distance from the thyroid notch to the tip of the jaw with the head extended) < 6 cm and presence of intact dentition. Male patients with severe obesity, especially ones with BMI more than 50 and OSA, as well patients with a neck circumference > 42 cm had a higher risk of difficult mask ventilation and intubation [139]. The use of simple nasal or high flow nasal cannula should be considered as an adjunct during mask ventilation in patients with a suspected or known difficult intubation. This has been demonstrated to help maintain oxygenation by increasing apnoea time up to 40% and can reduce peri-intubation desaturation during anaesthesia induction [140, 141].
The use of a videolaryngoscope (VL) may improve glottis visualization of the trachea and increase first attempt success rate of intubation compared to regular laryngoscope blades, especially in the setting of a difficult airway [142, 143]. However, regarding its efficacy results remain heterogeneous [144]. If a tracheostomy needs to be performed in a patient with significant obesity, it may take much longer than it would in a patient without obesity and it is associated with higher complication rates [145].
If baseline oxygen levels cannot be maintained immediately after extubation, use of continuous positive airway pressure (CPAP) therapy is recommended. Positive airway pressure should be continued until the patient’s respiratory rate and effort return to normal and there are no episodes of hypopnea and apnoea for at least one hour [146] (Table 3).
Ventilation strategies
While different strategies may play a role for protective ventilation, suggested measures to protect lungs from ventilated-induced lung injury include low tidal volumes (VT) and low positive end-expiratory pressure (PEEP) level without recruitment manoeuvres [147, 148].
Lung volume does not increase proportionally with body weight in patients with obesity [149]. Using the Predicted Body Weight (PBW), which takes in to consideration the patient´s height and sex, rather than the actual body weight, may be preferred when estimating VT. A low physiological VT can be lung protective in patients with acute respiratory distress syndrome (ARDS) [150], as well as in patients with healthy lungs under general anaesthesia [151, 152]. Current evidence suggests that a tidal volume in the range of 6–8 mg/kg of PBW can reduce pulmonary complications and should be employed for all patients with healthy lungs regardless of obesity [153].
Patients with obesity are predisposed to developing atelectasis mainly in dependent lung regions, making the combination of recruitment manoeuvers (RMs) and PEEP a strategy to improve gas exchange and lung mechanics [154,155,156]. There is much uncertainty regarding the optimal level of PEEP for patients with obesity and healthy lungs, and the role of PEEP and RM to avoid postoperative pulmonary complications remains unclear [157]. The PEEP requirements vary extensively among patients [158]. Receiving low VT during anaesthesia and individualized PEEP settings can reduce postoperative atelectasis while improving intraoperative gas exchange and driving pressures, suggesting that individualized levels of PEEP targeted to physiological goals could be used to protect the lungs [158].
High driving pressure (the difference between plateau pressure and PEEP) may be associated with an increased risk of severe adverse outcomes in patients with acute respiratory distress syndrome [159] as well as in patients undergoing elective surgery [152, 160]. Patients with obesity may require higher cut-off values of protective driving pressure than patients without obesity due to low lung capacity or physiologic changes occurring during the surgical procedure [161].
Pressure-controlled ventilation (PCV) may promote more homogeneous ventilation within different lung compartments, which in turn mitigates alveolar overdistention and improves oxygenation [162, 163]. On the other hand, volume-controlled ventilation (VCV) allows better control of VT during procedures intermittently affecting chest wall compliance and might be associated with lower incidence of postoperative pulmonary complications [164].
There is moderate evidence in support of using lung protective ventilation with avoidance of high values of PEEP. PCV or VCV can be used with inversed respiratory ratio, ideally avoiding increases in driving pressure from adjustments in PEEP, but the level of evidence remains low (Table 3).
Neuromuscular blockade
Neuromuscular blockade (NMB) is essential for laparoscopic or robot-assisted surgery for weight reduction [165, 166]. Even though controversial studies exist, current data are suggestive of benefit with deep NMB in patients undergoing bariatric procedures [167,168,169,170,171,172].
Deep NMB requires its prompt and complete reversal at the end of surgery. While the effects of residual NMB have not been specifically studied in bariatric surgery, many of the physiological findings associated with this condition may have increased relevance to the bariatric surgery population [173,174,175]. This puts patients with severe obesity at an increased risk of postoperative pulmonary complications, such as pulmonary atelectasis, pneumonia and even respiratory failure [176]. Patients should be fully reversed and carefully monitored with objective methods of residual neuromuscular blockade assessment during surgery and following reversal at the end of surgery [7, 168].
Nerve-stimulated TOF-ratio ≥ 0.9 translates into recovery benefits by avoiding recurarization and reintubations related to persistent blockade [177,178,179,180]. Sugammadex reverses moderate block 6.5 times faster than neostigmine, and deep neuromuscular blockade 16.8 times more rapidly than neostigmine [181], and have been associated with fewer adverse events compared with traditional reversal agents [181,182,183].
Sugammadex dose should be adjusted to the level of NMB and body weight to allow complete and rapid reversal. A dose of 2 mg/kg IBW + 40% seems to provide balance between speedy and complete recovery and favourable side effect profile [184,185,186]. The incidence of confirmed hypersensitivity is around 5% and anaphylaxis 0.3%, with the anaphylaxis occurring only with the dose of 16 mg/kg [187, 188]. In reality, the incidence of hypersensitivity reactions seems to be reported at a much lower rate and a dose of 2 mg/kg IBW + 40% seems to be most appropriate for the bariatric surgery population.
Deep NMB should generally be employed, with the understanding that it may not be reversible with traditional reversal agents until TOF is ≥ 3, while reversal with sugammadex would allow faster recovery and optimal operating room time (Table 3).
Surgical technique, volume and training
Laparoscopic surgery is today the self-evident gold standard in bariatric surgery. However, most studies comparing laparoscopic and open technique in bariatric surgery were performed in the beginning of the laparoscopic era. Thus, the current evidence level regarding the comparison between laparoscopic and open surgery hardly corresponds to current clinical practice. Compared to open surgery, there is moderate-quality evidence that laparoscopic approach in bariatric surgery is associated with a shorter LOS and earlier recovery, and high-quality evidence of an association with reduced rate of wound infections and hernias. For complications in general, duration of surgery and reoperation risk, the limited evidence is in favour for laparoscopy [189,190,191,192].
In 2016, the three most commonly performed primary surgical bariatric/metabolic procedures worldwide were sleeve gastrectomy (SG, 54%), Roux-en-Y gastric bypass (RYGB, 30%) with 30%, and one anastomosis gastric bypass (OAGB, 5%), respectively [193].
There are no studies comparing the feasibility of enhanced recovery between different bariatric procedures. The two most recent meta-analyses identified five RCTs and 12 observational studies assessed the application of ERAS for patients undergoing bariatric surgery and almost all of these studies included patients undergoing SG or RYGB [5, 194]. The safety and benefits of ERAS protocols in OAGB were assessed in one prospective study reporting shorter LOS and reduced emergency room visits and readmissions after surgery [195], and in one comparative study between OAGB and SG showing that the program was equally safe with both procedures [196]. The benefits and safety with the use of an ERAS protocol have been shown after all of the most common bariatric surgeries [5, 194].
There are limited data on the effect of hospital volume on perioperative safety in an ERAS environment [197]. However, the effect of hospital volume in traditional perioperative care has been actively studied for bariatric surgery. A recent study evaluated almost 40,000 bariatric surgery procedures performed in 19 high-volume centres, reported bench mark complication rates of 7.2% for RYGB and 6.2% for SG [198]. A systematic review [199] showed evidence of improved patient outcomes in high-volume surgeons and institutions, which was also confirmed by a large nationwide registry study [200]. Thus, there is low quality evidence in support of improved outcome at high-volume centres.
While recognizing a fast track pathway, many centres are involved in the training of new bariatric surgeons. During the learning curve process, longer operation times and even higher complication rates might be expected [201]. Previous experience with laparoscopic surgery, as well as adopting an individualized and comprehensive training programme, may improve surgical technical skills [202, 203]. Furthermore, active coaching and mentoring from experienced bariatric surgeons may result in shorter operative time and lower complication rates during surgical training [204,205,206,207] (Table 3).
Abdominal drainage and nasogastric decompression
The sensitivity of abdominal drainage (between 0 and 94%) in detecting postoperative leakage after RYGB has previously been assessed in a systematic review including 18 cohort studies [208]. A subsequent observational study including more than 140.000 patients showed no beneficial effects of routine abdominal drainage after bariatric surgery, but rather an increased morbidity rate [209]. Two small RCTs comparing routine use of abdominal drains to no drains reported similar complication rates, but more postoperative pain for the groups with drains [210, 211]. One cohort study [212] and one RCT [213] could not confirm any reduction in anastomotic leak with nasogastric decompression in patients undergoing bariatric surgery. There is no evidence supporting routine abdominal drainage or nasogastric decompression following bariatric surgery (Table 3).
Postoperative items
Postoperative oxygenation
Obesity is associated with increased work of breathing as well as higher risk of perioperative atelectasis persisting for longer duration compared to patients with normal weight [214, 215]. In addition, OSA is a common condition among patients with severe obesity [216]. It is associated with increased risk of cardiopulmonary events and a significant mortality rate, in particular in cases with high Apnoea-Hypopnea index (AHI) [217]. The STOP-BANG (Snoring, Tiredness during daytime, Observed apnoea, high blood Pressure, Body mass index, Age, Neck circumference, Gender) questionnaire might be used in the preoperative evaluation to identify patients with high risk of suffering from this comorbidity [218]. Patients with OSA have historically been considered to be at a high risk of perioperative complications, particularly those of respiratory nature [7]. Patients with obesity hypoventilation syndrome may exhibit even higher risk of cardiopulmonary complications and longer hospital stay, compared to patients with OSA alone [219].
Modern minimally invasive surgical techniques, combined with an emphasis on opioid-sparing analgesic approaches, and the use of CPAP/BiPAP treatment when necessary, can decrease the risk of cardiopulmonary complications in patients with OSA who undergo bariatric surgery [220].
Since the majority of the potentially dangerous hypoxic events occur in close proximity to the discontinuation of anaesthesia or after opioids are given, a standard or slightly prolonged observation in the PACU will be sufficient for most patients [221]. A postoperative positioning in a head-elevated, semi-seated position prevents further development of atelectasis and may improve oxygenation [215]. Supplemental oxygen improves oxygen saturation but may increase the duration and time to detection of apnoea/hypopnoea as well as carbon dioxide retention and should therefore be used with caution [222]. Positive airway pressure treatment can be used to prevent hypoxic events in the postoperative phase and should be continued in patients using CPAP/BiPAP treatment before surgery in order to reduce the risk for apnoea and other complications [223,224,225].
In addition, in patients with hypoxemia (defined as an oxygen saturation < 90%) during the immediate postoperative period, non-invasive positive pressure treatment such as CPAP or NIPPV (with or without supplemental oxygen) should be used liberally [226]. Standardized discharge criteria can be used to determine when the patient is ready to be discharged from the PACU, in addition to a satisfactory clinical evaluation to ensure that the patient has stable vital signs, including adequate respiratory rate and depth. Finally, as stated previously, it is recommended to minimize systemic opioid use in order to reduce episodes of apnoea/hypopnea (Table 4).
Thromboprophylaxis
Thromboembolic complications continue to represent a main cause of morbidity and mortality after bariatric surgery [227]. Risk factors, in addition to obesity itself, include history of venous thromboembolism, increased age, smoking, varicose veins, heart or respiratory failure, OSA, thrombophilia and oestrogen oral contraception [228].
There is wide variation in bariatric surgery practice, particularly in terms of treatment duration and dose adjustment [229, 230], and there is paucity of the literature for high-quality studies to inform clinical practice [231].
A Cochrane review from 2018 concluded with moderate-quality evidence that combining intermittent pneumatic leg compression and pharmacological prophylaxis decreases the incidence of deep venous thrombosis (DVT), and pulmonary embolism [232]. In addition, a different Cochrane review concluded that with high-quality evidence graduated compression stockings by itself are effective in reducing the risk of DVT in hospitalized patients who have undergone general surgery [233].
The ASMBS guideline suggests thromboprophylaxis, including unfractionated heparin or low-molecular-weight heparin (LMWH) given within 24 h postoperatively, for all patients after bariatric surgery [21].
A systematic review including 20 studies suggested that for thromboprophylaxis with LMWH, enoxaparin 40 mg twice daily, dalteparin 5000 IE twice daily or tinzaparin 75 IU/kg once daily should be considered for patients with BMI ≥ 40 kg/m2 [234].
A study of 105 patients using antifactor Xa (aFXa) assay demonstrated that BMI-based thromboprophylactic dosing of enoxaparin after bariatric surgery could be suboptimal in 15% of patients and overdosing was more common than underdosing [235]. For optimization of dosage, it has been suggested that in high-risk bariatric surgery patients, the measurement of aFXa should be considered [235, 236].
In a large study, it was reported a 28-fold increase in mortality risk in patients with venous thromboembolic events and that more than 80% occurred after discharge [237]. Therefore, routine post-discharge pharmacoprophylaxis extending beyond standard treatment should be considered for high-risk patients [21, 237]. This is also supported from mechanistic data and studies of surgical patients undergoing non-bariatric surgery [238,239,240].
Regarding the use of retrievable inferior vena cava filters in the context of bariatric surgery, a systematic review suggested that there was no evidence to suggest that the potential benefits outweigh the significant risks [241].
An emerging thromboembolic complication is portomesentric and splenic vein thrombosis. A systematic review suggested that it is most common after SG and that the portal vein is the most commonly involved vessel [242]. Another systematic review focusing on SG exclusively suggested that the incidence ranged from 0.37% to 1% [243]. Further studies on the impact of prophylaxis strategies to reduce this specific complication are needed (Table 4).
Early postoperative nutritional care
As part of the assessment and preparation for bariatric surgery, patients should have access to a comprehensive nutrition and dietetic assessment [244,245,246,247,248,249]. A clear liquid meal regimen can usually be initiated a couple of hours postoperatively before moving on to nourishing fluids [245, 250]. The dietetic consultations will include advice on texture progression specific to the surgical procedure and the bariatric centre’s usual practice [245, 250].
Patients will continue to progress the introduction of food and different textures at home. They are encouraged to eat slowly, chew their food well and avoid drinking with food [245, 250]. In the early postoperative weeks, patients are at risk of developing thiamine deficiency because of the relatively small depots in combination with fast weight loss and poor nutritional intake. This risk is further increased in the presence of vomiting, diarrhoea or non-adherence to the vitamin and mineral supplements [244,245,246,247, 250]. If risk of thiamine deficiency is suspected, it must be treated immediately.
The dietitian will advise on protein intake. Generally, following the adjustable gastric band, SG and RYGB, at least 60–80 g/day total protein intake or 1.0–1.5 g/kg ideal body weight (IBW) is recommended. However, hypoabsorptive procedures such as the biliopancreatic diversion with duodenal switch, OAGB and single anastomosis duodenal-ileal bypass increase the risk of protein-energy malnutrition [251, 252]. Consequently, a protein intake of at least 90 g/day or as high as 2.1 g/kg IBW is then recommended [245] (Table 4).
Supplementation of vitamins and minerals
Postoperative dietetic follow-up is essential. After bariatric surgery, there is an increased risk of deficiencies of iron, folate, vitamin B12, vitamin D and trace minerals zinc, copper and selenium. Hypoabsorptive procedures can further increase the risk of vitamin A, E and K deficiencies [251, 252]. Consequently, patients are required to adhere to a regimen of life-long vitamin and mineral supplementation and nutritional biochemical monitoring. The supplements and biochemical monitoring differ by surgical procedure and full details may be found in bariatric surgery nutritional guidelines [244, 247] (Table 4).
Postoperative prophylaxis
Proton pump inhibitors
A systematic review reported an overall incidence rate of marginal ulcers of 4.6% after RYGB. However, the range between included studies varied from 0.6–25% [253]. Several studies have reported a significant reduction in marginal ulcers if PPIs are used prophylactic in the perioperative phase in particular when used for longer duration such as 3 months [254, 255]. However, when using a standardized surgical technique, with a small gastric pouch, the need for PPI prophylaxis has been questioned [256]. While recognizing the weak evidence of support, prophylactic use of PPI is safe and without significant cost. These medications can therefore be considered for postoperative prophylaxis after RYGB. If used, higher doses than standard should be given after gastric bypass surgery due to the reduced uptake [257]. In addition, opening of the capsules could improve postoperative uptake and should be considered [258].
There are no studies addressing the benefits of PPI use following sleeve gastrectomy. While high rates of reflux and reflux-related complications are reported in some studies [259,260,261,262], there is insufficient evidence to give any firm recommendations on the use of PPI after sleeve gastrectomy (Table 4).
Gallstone prevention
Five RCTs (four addressing RYGB, and one SG) including a total of 616 patients reported significant reduction in postoperative gallstone formation by the use of ursodeoxycholic acid in patients without gallstones at the time of surgery [263,264,265,266,267]. While the optimal dose remains controversial, these studies suggest that 500–600 mg may be sufficient. The results are further strengthened by a meta-analysis addressing three studies for RYGB and three for SG of different study designs showing a benefit for patients prescribed ursodeoxycholic acid for postoperative prophylaxis [268]. A placebo controlled RCT is underway with a planned inclusion of 900 patients given a dose of 900 mg for 6 months after surgery [269]. If this study confirms the results of previous studies, ursodeoxycholic acid should likely be recommended as prophylaxis against gallstone formation in patients without gallstones at the time of surgery. There is no data available on the potential effect of ursodeoxycholic acid to prevent progression of prevalent gall stones (Table 4). A systematic review of observational studies concluded that concomitant cholecystectomy for patients with symptomatic gallstones disease can be considered to be safe [270]. However, a sequential approach with a cholecystectomy before the bariatric surgery may be equally safe and efficient [271]. While the grade of evidence remains low, it is strongly recommended to consider cholecystectomy either before or at the time of bariatric surgery for patients with symptomatic gallstones disease.
Specific considerations in patients with diabetes
The consideration of diabetes is an addition to these guidelines [89].
In most reports of patients undergoing bariatric surgery, 15–20% of patients have T2D [200, 272, 273]. Carbohydrate loading is associated with an exaggerated hyperglycaemia in patients with diabetes. It is also recognized in several studies in patients undergoing non-bariatric surgery that hyperglycaemia is associated with worse outcomes, including increased complications and mortality in severe cases [274,275,276]. Therefore, the need to focus on the care of these patients is critical and the need for guidelines imminent.
In contrast to other types of surgery, bariatric surgery improves glucose homeostasis in patients with T2D, due to a variety of mechanisms, as early as in the immediate postoperative period [277]. Therefore, dose-adjustments in the glucose-lowering medications prescribed are often needed [278, 279]. This should be considered as early as possible since appropriate planning may facilitate early discharge and reduce LOS. Patients with diabetes who are prescribed preoperative LCD/VLCD should also be aware of the risk of hypoglycaemia during this period and might therefore be in need of adjustments of antidiabetic agents as well.
It should also be noted that some of the lessons learned from ERAS care in patients with diabetes undergoing bariatric surgery might be of relevance for other types of GI surgery, particularly oesophagogastric resections for cancer [280].
Final words
ERAS pathways include evidence-based items designed to reduce perioperative stress and maintain postoperative physiological function. The pathways were first adopted for colorectal surgery in 2005, but today ERAS guidelines are available for several fields of surgery [281]. Adherence to an updated ERAS protocol has been associated with reduced short- and long-term morbidity, as well as to improved recovery, shortened hospital LOS and reduced medical costs following major abdominal surgery [282, 283]. In modern bariatric surgery, the use of several items of the ERAS protocol has been widely accepted and shown to be associated with low rates of perioperative complications and faster recovery. However, the quality of evidence for many ERAS interventions is relatively low in a bariatric setting and evidence-based practices may need to be extrapolated from other surgeries. Higher quality of evidence would need additional confirmation from RCTs or large registries, and since some may often not be justified from an ethical perspective, or otherwise may not be feasible, the quality of evidence could be assumed to remain low. There is also a lack of studies addressing patient reported outcome measures as well as cost-effectiveness of some interventions. Although such studies may not improve quality of evidence in support of specific items, they may increase knowledge and provide a more complete understanding of the impact of specific interventions as well as clinical protocols.
Thus, the benefits of the adherence to an ERAS protocol in bariatric surgery have so far only been possible to demonstrate with high quality of evidence for functional recovery and hospital LOS [5, 6].
Since the first version of the ERAS guidelines for bariatric surgery was published in 2016 [7], results from new studies have impacted the level of evidence for certain recommendations, while others remain the same. The details of an ERAS pathway for patients with specific comorbidities who may have potentially more complex perioperative course, such as those with diabetes, cardiovascular and psychiatric comorbidities, deserve further focus. With the well documented effect of ERAS on reducing perioperative stress, the gains in terms of reduced perioperative morbidity could be expected to be particularly evident in these patient populations.
Change history
29 January 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00268-022-06459-3
References
Sundbom M, Hedberg J, Marsk R et al (2017) Substantial decrease in comorbidity 5 years after gastric bypass: a population-based study from the scandinavian obesity surgery registry. Ann Surg 265(6):1166–1171
Schauer DP, Arterburn DE, Livingston EH et al (2015) Impact of bariatric surgery on life expectancy in severely obese patients with diabetes: a decision analysis. Ann Surg 261(5):914–919
Angrisani L, Santonicola A, Iovino P, Ramos A, Shikora S, Bariatric KL, Survey S (2018) Similarities and disparities among the 5 IFSO chapters. Obes Surg 2021:1–12
Khoo CK, Vickery CJ, Forsyth N, Vinall NS, Eyre-Brook IA (2007) A prospective randomized controlled trial of multimodal perioperative management protocol in patients undergoing elective colorectal resection for cancer. Ann Surg 245(6):867–872
Parisi A, Desiderio J, Cirocchi R, Trastulli S (2020) Enhanced recovery after surgery (ERAS): a systematic review of randomised controlled trials (RCTs) in bariatric surgery. Obes Surg 30(12):5071–5085
Geubbels N, Evren I, Acherman YIZ et al (2019) Randomized clinical trial of an enhanced recovery after surgery programme versus conventional care in laparoscopic Roux-en-Y gastric bypass surgery. BJS Open 3(3):274–281
Thorell A, MacCormick AD, Awad S et al (2016) Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg 40(9):2065–2083
Brindle M, Nelson G, Lobo DN, Ljungqvist O, Gustafsson UO (2020) Recommendations from the ERAS® Society for standards for the development of enhanced recovery after surgery guidelines. BJS Open 4(1):157–163
An Glossary. In: Green SH, J, ed. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5. The Cochrane Collaboration. www.cochrane.org/resources/glossary.htm2005.
Guyatt GH, Oxman AD, Kunz R et al (2008) Going from evidence to recommendations. BMJ 336(7652):1049–1051
Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ (2008) What is “quality of evidence” and why is it important to clinicians? BMJ 336(7651):995–998
Mechanick JI, Youdim A, Jones DB et al (2013) Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient–2013 update: cosponsored by american association of clinical endocrinologists, the obesity society, and american society for metabolic & bariatric surgery. Obesity (Silver Spring) 21(Suppl 1):S1-27
Hathaway D (1986) Effect of preoperative instruction on postoperative outcomes: a meta-analysis. Nurs Res 35(5):269–275
Devine EC, Cook TD (1983) A meta-analytic analysis of effects of psychoeducational interventions on length of postsurgical hospital stay. Nurs Res 32(5):267–274
Egbert LD, Battit GE, Welch CE, Bartlett MK (1964) Reduction of postoperative pain by encouragement and instruction of patients. a study of doctor-patient rapport. N Engl J Med 270:825–827
Porras-González MH, Barón-López FJ, García-Luque MJ, Morales-Gil IM (2015) Effectiveness of the nursing methodology in pain management after major ambulatory surgery. Pain Manag Nurs 16(4):520–525
Waller A, Forshaw K, Bryant J, Carey M, Boyes A, Sanson-Fisher R (2015) Preparatory education for cancer patients undergoing surgery: a systematic review of volume and quality of research output over time. Patient Educ Couns S0738–3991(15):00229–00233
Koet LL, Kraima A, Derksen I et al (2021) Effectiveness of preoperative group education for patients with colorectal cancer: managing expectations. Support Care Cancer 29(9):5263–5271
Burgess LC, Arundel J, Wainwright TW (2019) The effect of preoperative education on psychological, clinical and economic outcomes in elective spinal surgery: a systematic review. Healthcare Basel 7(1):48
Klaiber U, Stephan-Paulsen LM, Bruckner T et al (2018) Impact of preoperative patient education on the prevention of postoperative complications after major visceral surgery: the cluster randomized controlled PEDUCAT trial. Trials 19(1):288
Mechanick JI, Apovian C, Brethauer S et al (2019) Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures - 2019 update: cosponsored by american association of clinical endocrinologists/american college of endocrinology, the obesity society, american society for metabolic & bariatric surgery, obesity medicine association, and american society of anesthesiologists - executive summary. Endocr Pract 25(12):1346–1359
NIH conference (1991) Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med, 115(12):956–961
NICE. Obesity: identification, assessment and management. Published 2014. Accessed at www.nice.org.uk/guidance/cg189 on May 11, 2021
Rubino F, Nathan DM, Eckel RH et al (2016) Metabolic Surgery in the Treatment Algorithm for Type 2 Diabetes: A Joint Statement by International Diabetes Organizations. Diabetes Care 39(6):861–877
Moller AM, Villebro N, Pedersen T, Tonnesen H (2002) Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet 359(9301):114–117
Haskins IN, Amdur R, Vaziri K (2014) The effect of smoking on bariatric surgical outcomes. Surg Endosc 28(11):3074–3080
Inadomi M, Iyengar R, Fischer I, Chen X, Flagler E, Ghaferi AA (2018) Effect of patient-reported smoking status on short-term bariatric surgery outcomes. Surg Endosc 32(2):720–726
Chow A, Neville A, Kolozsvari N (2021) Smoking in bariatric surgery: a systematic review. Surg Endosc 35(6):3047–3066
Thomsen T, Villebro N, Moller AM (2014) Interventions for preoperative smoking cessation. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD002294.pub4
Webb AR, Coward L, Soh L et al (2020) Smoking cessation in elective surgical patients offered free nicotine patches at listing: a pilot study. Anaesthesia 75(2):171–178
Nath B, Li Y, Carroll JE, Szabo G, Tseng JF, Shah SA (2010) Alcohol exposure as a risk factor for adverse outcomes in elective surgery. J Gastrointest Surg 14(11):1732–1741
Egholm JW, Pedersen B, Møller AM, Adami J, Juhl CB, Tønnesen H (2018) Perioperative alcohol cessation intervention for postoperative complications. Cochrane Database Syst Rev 11(11):Cd008343
Kanji S, Wong E, Akioyamen L, Melamed O, Taylor VH (2019) Exploring pre-surgery and post-surgery substance use disorder and alcohol use disorder in bariatric surgery: a qualitative scoping review. Int J Obes (Lond) 43(9):1659–1674
Gils Contreras A, Bonada Sanjaume A, Montero Jaime M et al (2018) Effects of two preoperatory weight loss diets on hepatic volume, metabolic parameters, and surgical complications in morbid obese bariatric surgery candidates: a randomized clinical trial. Obes Surg 28(12):3756–3768
Bakker N, van den Helder RS, Geenen RWF et al (2019) Four weeks of preoperative omega-3 fatty acids reduce liver volume: a randomised controlled trial. Obes Surg 29(7):2037–2044
Pournaras DJ, Nygren J, Hagstrom-Toft E, Arner P, le Roux CW, Thorell A (2016) Improved glucose metabolism after gastric bypass: evolution of the paradigm. Surg Obes Relat Dis 12(8):1457–1465
Cassie S, Menezes C, Birch DW, Shi X, Karmali S (2011) Effect of preoperative weight loss in bariatric surgical patients: a systematic review. Surg Obes Relat Dis 7(6):760–767
Van Nieuwenhove Y, Dambrauskas Z, Campillo-Soto A et al (2011) Preoperative very low-calorie diet and operative outcome after laparoscopic gastric bypass: a randomized multicenter study. Arch Surg 146(11):1300–1305
Giordano S, Victorzon M (2014) The impact of preoperative weight loss before laparoscopic gastric bypass. Obes Surg 24(5):669–674
Anderin C, Gustafsson UO, Heijbel N, Thorell A (2015) Weight loss before bariatric surgery and postoperative complications: data from the Scandinavian Obesity Registry (SOReg). Ann Surg 261(5):909–913
Stefura T, Droś J, Kacprzyk A et al (2019) Influence of preoperative weight loss on outcomes of bariatric surgery for patients under the enhanced recovery after surgery protocol. Obes Surg 29(4):1134–1141
Holderbaum M, Casagrande DS, Sussenbach S, Buss C (2018) Effects of very low calorie diets on liver size and weight loss in the preoperative period of bariatric surgery: a systematic review. Surg Obes Relat Dis 14(2):237–244
Roman M, Monaghan A, Serraino GF et al (2019) Meta-analysis of the influence of lifestyle changes for preoperative weight loss on surgical outcomes. Br J Surg 106(3):181–189
Gerber P, Anderin C, Gustafsson UO, Thorell A (2016) Weight loss before gastric bypass and postoperative weight change: data from the Scandinavian Obesity Registry (SOReg). Surg Obes Relat Dis 12(3):556–562
Ross LJ, Wallin S, Osland EJ, Memon MA (2016) Commercial very low energy meal replacements for preoperative weight loss in obese patients: a systematic review. Obes Surg 26(6):1343–1351
Hughes MJ, Hackney RJ, Lamb PJ, Wigmore SJ, Christopher Deans DA, Skipworth RJE (2019) Prehabilitation before major abdominal surgery: a systematic review and meta-analysis. World J Surg 43(7):1661–1668
Valkenet K, van de Port IG, Dronkers JJ, de Vries WR, Lindeman E, Backx FJ (2011) The effects of preoperative exercise therapy on postoperative outcome: a systematic review. Clin Rehabil 25(2):99–111
Marc-Hernández A, Ruiz-Tovar J, Aracil A, Guillén S, Moya-Ramón M (2019) Impact of exercise on body composition and cardiometabolic risk factors in patients awaiting bariatric surgery. Obes Surg 29(12):3891–3900
Baillot A, Mampuya WM, Dionne IJ, Comeau E, Méziat-Burdin A, Langlois MF (2016) Impacts of supervised exercise training in addition to interdisciplinary lifestyle management in subjects awaiting bariatric surgery: a randomized controlled study. Obes Surg 26(11):2602–2610
Lloréns J, Rovira L, Ballester M et al (2015) Preoperative inspiratory muscular training to prevent postoperative hypoxemia in morbidly obese patients undergoing laparoscopic bariatric surgery. A randomized clinical trial Obes Surg 25(6):1003–1009
McSorley ST, Roxburgh CSD, Horgan PG, McMillan DC (2017) The impact of preoperative dexamethasone on the magnitude of the postoperative systemic inflammatory response and complications following surgery for colorectal cancer. Ann Surg Oncol 24(8):2104–2112
McSorley ST, Horgan PG, McMillan DC (2016) The impact of preoperative corticosteroids on the systemic inflammatory response and postoperative complications following surgery for gastrointestinal cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol 101:139–150
Zhang T, Xu Y, Yao Y, et al. (2021) Randomized Controlled Trial: Perioperative Dexamethasone Reduces Excessive Postoperative Inflammatory Response and Ileus After Surgery for Inflammatory Bowel Disease. Inflamm Bowel Dis. Online ahead of print.
Lex JR, Edwards TC, Packer TW, Jones GG, Ravi B (2021) Perioperative systemic dexamethasone reduces length of stay in total joint arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Arthroplasty 36(3):1168–1186
Polderman JA, Farhang-Razi V, Van Dieren S et al (2018) Adverse side effects of dexamethasone in surgical patients. Cochrane Database Syst Rev 8(8):Cd011940
Srinivasa S, Kahokehr AA, Yu TC, Hill AG (2011) Preoperative glucocorticoid use in major abdominal surgery: systematic review and meta-analysis of randomized trials. Ann Surg 254(2):183–191
Waldron NH, Jones CA, Gan TJ, Allen TK, Habib AS (2013) Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis. Br J Anaesth 110(2):191–200
Singh PP, Srinivasa S, Lemanu DP, Maccormick AD, Hill AG (2012) Statins in abdominal surgery: a systematic review. J Am Coll Surg 214(3):356–366
Komatsu R, Yilmaz HO, Makarova N et al (2020) Association between preoperative statin use and respiratory complications after noncardiac surgery: a retrospective cohort analysis. Anesth Analg 133(1):123–132
London MJ, Schwartz GG, Hur K, Henderson WG (2017) Association of perioperative statin use with mortality and morbidity after major noncardiac surgery. JAMA Intern Med 177(2):231–242
Pourlotfi A, Ahl R, Sjolin G et al (2021) Statin therapy and postoperative short-term mortality after rectal cancer surgery. Colorectal Dis 23(4):875–881
Im C, Oh TK, Song IA, Jeon YT (2019) Preoperative Statin Use and 90-Day Mortality after Noncardiac Surgery: A Hospital Registry Study. Ann Surg. 2019. Online ahead of print
Ma BX, Li H, Li JS, Wu SS (2015) Effect of statins on preventing infectious complications after surgery: systematic review and meta-analysis. J Int Med Res 43(5):610–618
Berwanger O, Le Manach Y, Suzumura EA et al (2016) Association between pre-operative statin use and major cardiovascular complications among patients undergoing non-cardiac surgery: the VISION study. Eur Heart J 37(2):177–185
Singh PP, Lemanu DP, Soop M, Bissett IP, Harrison J, Hill AG (2016) Perioperative simvastatin therapy in major colorectal surgery: a prospective, double-blind randomized controlled trial. J Am Coll Surg 223(2):308-320.e301
Berwanger O, de Barros ESPG, Barbosa RR et al (2017) Atorvastatin for high-risk statin-naïve patients undergoing noncardiac surgery: the Lowering the Risk of Operative Complications Using Atorvastatin Loading Dose (LOAD) randomized trial. Am Heart J 184:88–96
Li H, Lin YL, Diao SL, Ma BX, Liu XL (2016) Does short preoperative statin therapy prevent infectious complications in adults undergoing cardiac or non-cardiac surgery? A meta-analysis of 5 randomized placebo-controlled trials. Saudi Med J 37(5):492–497
Blessberger H, Lewis SR, Pritchard MW et al (2019) Perioperative beta-blockers for preventing surgery-related mortality and morbidity in adults undergoing non-cardiac surgery. Cochrane Database Syst Rev 9(9):Cd013438
Devereaux PJ, Yang H, Yusuf S et al (2008) Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet 371(9627):1839–1847
Ahl R, Matthiessen P, Fang X et al (2020) Beta-blockade in rectal cancer surgery: a simple measure of improving outcomes. Ann Surg 271(1):140–146
Ahl R, Matthiessen P, Fang X et al (2019) Effect of beta-blocker therapy on early mortality after emergency colonic cancer surgery. Br J Surg 106(4):477–483
Stenberg E, Mohseni S, Cao Y, Naslund E (2020) Limited effect of beta-blockade on postoperative outcome after laparoscopic gastric bypass surgery. Obes Surg 30(1):139–145
Jørgensen ME, Andersson C, Venkatesan S, Sanders RD (2018) Beta-blockers in noncardiac surgery: did observational studies put us back on safe ground? Br J Anaesth 121(1):16–25
Harter RL, Kelly WB, Kramer MG, Perez CE, Dzwonczyk RR (1998) A comparison of the volume and pH of gastric contents of obese and lean surgical patients. Anesth Analg 86(1):147–152
Juvin P, Fevre G, Merouche M, Vallot T, Desmonts JM (2001) Gastric residue is not more copious in obese patients. Anesth Analg 93(6):1621–1622
Cardoso-Junior A, Coelho LG, Savassi-Rocha PR et al (2007) Gastric emptying of solids and semi-solids in morbidly obese and non-obese subjects: an assessment using the 13C-octanoic acid and 13C-acetic acid breath tests. Obes Surg 17(2):236–241
Buchholz V, Berkenstadt H, Goitein D, Dickman R, Bernstine H, Rubin M (2013) Gastric emptying is not prolonged in obese patients. Surg Obes Relat Dis 9(5):714–717
Seimon RV, Brennan IM, Russo A et al (2013) Gastric emptying, mouth-to-cecum transit, and glycemic, insulin, incretin, and energy intake responses to a mixed-nutrient liquid in lean, overweight, and obese males. Am J Physiol Endocrinol Metab 304(3):E294-300
Maltby JR, Pytka S, Watson NC, Cowan RA, Fick GH (2004) Drinking 300 mL of clear fluid two hours before surgery has no effect on gastric fluid volume and pH in fasting and non-fasting obese patients. Can J Anaesth 51(2):111–115
Maltby JR (2006) Fasting from midnight–the history behind the dogma. Best Pract Res Clin Anaesthesiol 20(3):363–378
Ishihara H, Singh H, Giesecke AH (1994) Relationship between diabetic autonomic neuropathy and gastric contents. Anesth Analg 78(5):943–947
Bertin E, Schneider N, Abdelli N et al (2001) Gastric emptying is accelerated in obese type 2 diabetic patients without autonomic neuropathy. Diabetes Metab 27(3):357–364
Ljungqvist O, Jonathan E (2012) Rhoads lecture 2011: Insulin resistance and enhanced recovery after surgery. JPEN J Parenter Enteral Nutr 36(4):389–398
Awad S, Varadhan KK, Ljungqvist O, Lobo DN (2013) A meta-analysis of randomised controlled trials on preoperative oral carbohydrate treatment in elective surgery. Clin Nutr 32(1):34–44
Smith MD, McCall J, Plank L, Herbison GP, Soop M, Nygren J (2014) Preoperative carbohydrate treatment for enhancing recovery after elective surgery. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD009161.pub2
Pimenta GP, Capellan DA, de Aguilar-Nascimento JE (2015) Sleeve gastrectomy with or without a multimodal perioperative care. A Randomized Pilot Study Obes Surg 25(9):1639–1646
Gustafsson UO, Nygren J, Thorell A et al (2008) Pre-operative carbohydrate loading may be used in type 2 diabetes patients. Acta Anaesthesiol Scand 52(7):946–951
Azagury DE, Ris F, Pichard C, Volonte F, Karsegard L, Huber O (2015) Does perioperative nutrition and oral carbohydrate load sustainably preserve muscle mass after bariatric surgery? A randomized control trial. Surg Obes Relat Dis 11(4):920–926
Albalawi Z, Laffin M, Gramlich L, Senior P, McAlister FA (2017) Enhanced recovery after surgery (ERAS(®)) in Individuals with diabetes: a systematic review. World J Surg 41(8):1927–1934
Jones KL, Horowitz M, Wishart MJ, Maddox AF, Harding PE, Chatterton BE (1995) Relationships between gastric emptying, intragastric meal distribution and blood glucose concentrations in diabetes mellitus. J Nucl Med 36(12):2220–2228
Lemanu DP, Singh PP, Berridge K et al (2013) Randomized clinical trial of enhanced recovery versus standard care after laparoscopic sleeve gastrectomy. Br J Surg 100(4):482–489
Ronellenfitsch U, Schwarzbach M, Kring A, Kienle P, Post S, Hasenberg T (2012) The effect of clinical pathways for bariatric surgery on perioperative quality of care. Obes Surg 22(5):732–739
Karlsson A, Wendel K, Polits S, Gislason H, Hedenbro JL (2016) Preoperative nutrition and postoperative discomfort in an ERAS setting: a randomized study in gastric bypass surgery. Obes Surg 26(4):743–748
Halliday TA, Sundqvist J, Hultin M, Walldén J (2017) Post-operative nausea and vomiting in bariatric surgery patients: an observational study. Acta Anaesthesiol Scand 61(5):471–479
Groene P, Eisenlohr J, Zeuzem C, Dudok S, Karcz K, Hofmann-Kiefer K (2019) Postoperative nausea and vomiting in bariatric surgery in comparison to non-bariatric gastric surgery. Wideochir Inne Tech Maloinwazyjne 14(1):90–95
Kushner BS, Freeman D, Sparkman J, Salles A, Eagon JC, Eckhouse SR (2020) Assessment of postoperative nausea and vomiting after bariatric surgery using a validated questionnaire. Surg Obes Relat Dis 16(10):1505–1513
Gan TJ, Belani KG, Bergese S et al (2020) Fourth consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg 131(2):411–448
Ziemann-Gimmel P, Goldfarb AA, Koppman J, Marema RT (2014) Opioid-free total intravenous anaesthesia reduces postoperative nausea and vomiting in bariatric surgery beyond triple prophylaxis. Br J Anaesth 112(5):906–911
Bamgbade OA, Oluwole O, Khaw RR (2018) Perioperative antiemetic therapy for fast-track laparoscopic bariatric surgery. Obes Surg 28(5):1296–1301
Alpert MA (2001) Obesity cardiomyopathy: pathophysiology and evolution of the clinical syndrome. Am J Med Sci 321(4):225–236
Mythen MG, Webb AR (1995) Perioperative plasma volume expansion reduces the incidence of gut mucosal hypoperfusion during cardiac surgery. Arch Surg 130(4):423–429
Shoemaker WC, Montgomery ES, Kaplan E, Elwyn DH (1973) Physiologic patterns in surviving and nonsurviving shock patients Use of sequential cardiorespiratory variables in defining criteria for therapeutic goals and early warning of death. Arch Surg 106(5):630–636
Shoemaker WC, Appel PL, Kram HB (1992) Role of oxygen debt in the development of organ failure sepsis, and death in high-risk surgical patients. Chest 102(1):208–215
Myles PS, Bellomo R, Corcoran T et al (2018) Restrictive versus liberal fluid therapy for major abdominal surgery. N Engl J Med 378(24):2263–2274
Chen F, Rasouli MR, Ellis AR et al (2020) Associations between perioperative crystalloid volume and adverse outcomes in five surgical populations. J Surg Res 251:26–32
Major P, Wysocki M, Torbicz G et al (2018) Risk factors for prolonged length of hospital stay and readmissions after laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass. Obes Surg 28(2):323–332
Reiterer C, Kabon B, Zotti O, Obradovic M, Kurz A, Fleischmann E (2019) Effect of goal-directed crystalloid- versus colloid-based fluid strategy on tissue oxygen tension: a randomised controlled trial. Br J Anaesth 123(6):768–776
Muhlbacher J, Luf F, Zotti O, Herkner H, Fleischmann E, Kabon B (2021) Effect of intraoperative goal-directed fluid management on tissue oxygen tension in obese patients: a randomized controlled trial. Obes Surg 31(3):1129–1138
Munoz JL, Gabaldon T, Miranda E et al (2016) Goal-directed fluid therapy on laparoscopic sleeve gastrectomy in morbidly obese patients. Obes Surg 26(11):2648–2653
Myburgh JA, Mythen MG (2013) Resuscitation fluids. N Engl J Med 369(13):1243–1251
Jacob M, Chappell D, Rehm M (2007) Clinical update: perioperative fluid management. Lancet 369(9578):1984–1986
Hahn RG (2010) Volume kinetics for infusion fluids. Anesthesiology 113(2):470–481
Kimberger O, Arnberger M, Brandt S et al (2009) Goal-directed colloid administration improves the microcirculation of healthy and perianastomotic colon. Anesthesiology 110(3):496–504
Rehm M, Zahler S, Lotsch M et al (2004) Endothelial glycocalyx as an additional barrier determining extravasation of 6% hydroxyethyl starch or 5% albumin solutions in the coronary vascular bed. Anesthesiology 100(5):1211–1223
Obradovic M, Kurz A, Kabon B et al (2020) The effect of intraoperative goal-directed crystalloid versus colloid administration on perioperative inflammatory markers - a substudy of a randomized controlled trial. BMC Anesthesiol 20(1):210
Kabon B, Sessler DI, Kurz A (2019) Crystalloid-colloid study t effect of intraoperative goal-directed balanced crystalloid versus colloid administration on major postoperative morbidity: a randomized trial. Anesthesiology 130(5):728–744
Chowdhury AH, Cox EF, Francis ST, Lobo DN (2014) A randomized, controlled, double-blind crossover study on the effects of 1-L infusions of 6% hydroxyethyl starch suspended in 0.9% saline (voluven) and a balanced solution (Plasma Volume Redibag) on blood volume, renal blood flow velocity, and renal cortical tissue perfusion in healthy volunteers. Ann Surg 259(5):881–887
Weinberg L, Li M, Churilov L et al (2018) Associations of fluid amount, type, and balance and acute kidney injury in patients undergoing major surgery. Anaesth Intensive Care 46(1):79–87
Pfortmueller CA, Funk GC, Reiterer C et al (2018) Normal saline versus a balanced crystalloid for goal-directed perioperative fluid therapy in major abdominal surgery: a double-blind randomised controlled study. Br J Anaesth 120(2):274–283
Ingrande J, Brodsky JB, Lemmens HJ (2011) Lean body weight scalar for the anesthetic induction dose of propofol in morbidly obese subjects. Anesth Analg 113(1):57–62
Servin F, Farinotti R, Haberer JP, Desmonts JM (1993) Propofol infusion for maintenance of anesthesia in morbidly obese patients receiving nitrous oxide. A clinical and pharmacokinetic study Anesthesiology 78(4):657–665
Cortínez LI, De la Fuente N, Eleveld DJ et al (2014) Performance of propofol target-controlled infusion models in the obese: pharmacokinetic and pharmacodynamic analysis. Anesth Analg 119(2):302–310
Lehavi A, Sandler O, Mahajna A, Weissman A, Katz YS (2015) Comparison of rhabdomyolysis markers in patients undergoing bariatric surgery with propofol and inhalation-based anesthesia. Obes Surg 25(10):1923–1927
Singh PM, Borle A, McGavin J, Trikha A, Sinha A (2017) Comparison of the recovery profile between desflurane and sevoflurane in patients undergoing bariatric surgery-a meta-analysis of randomized controlled trials. Obes Surg 27(11):3031–3039
Avidan MS, Jacobsohn E, Glick D et al (2011) Prevention of intraoperative awareness in a high-risk surgical population. N Engl J Med 365(7):591–600
Mashour GA, Shanks A, Tremper KK et al (2012) Prevention of intraoperative awareness with explicit recall in an unselected surgical population: a randomized comparative effectiveness trial. Anesthesiology 117(4):717–725
Oderda GM, Senagore AJ, Morland K et al (2019) Opioid-related respiratory and gastrointestinal adverse events in patients with acute postoperative pain: prevalence, predictors, and burden. J Pain Palliat Care Pharmacother 33(3–4):82–97
Brown EN, Pavone KJ, Naranjo M (2018) Multimodal general anesthesia: theory and practice. Anesth Analg 127(5):1246–1258
Falcão LFRFA, Silva BD (2018) Anestesia livre de opioides. In: Nunes RRBA, Duarte LTD (eds) PROANESTESIA Programa de Atualização em Anestesiologia, vol 3. Artmed Panamericana, Porto Alegre, pp 141–172
Mulier J (2017) Opioid free general anesthesia: A paradigm shift? Rev Esp Anestesiol Reanim 64(8):427–430
Mulier JPDB (2018) A prospective randomized controlled trial comparing a multitarget opioid free anaesthesia (OFA) and a 3-Liter volume calculated airseal carbon dioxide insufflator with a balanced anaesthesia using sufentanil-sevoflurane and a standard 15 MmHg carbon dioxide pressure pneumoperitoneum insufflator in a 2x2 factorial design. J Clin Anesth Pain Med 2(2):6
Govindarajan R, Ghosh B, Sathyamoorthy MK et al (2005) Efficacy of ketorolac in lieu of narcotics in the operative management of laparoscopic surgery for morbid obesity. Surg Obes Relat Dis 1(6):530–535
Beloeil H, Albaladejo P, Sion A et al (2019) Multicentre, prospective, double-blind, randomised controlled clinical trial comparing different non-opioid analgesic combinations with morphine for postoperative analgesia: the OCTOPUS study. Br J Anaesth 122(6):e98–e106
Foldi M, Soos A, Hegyi P et al (2021) Transversus abdominis plane block appears to be effective and safe as a part of multimodal analgesia in bariatric surgery: a meta-analysis and systematic review of randomized controlled trials. Obes Surg 31(2):531–543
Boerboom SL, de Haes A, Vd Wetering L et al (2018) Preperitoneal bupivacaine infiltration reduces postoperative opioid consumption, acute pain, and chronic postsurgical pain after bariatric surgery: a randomized controlled trial. Obes Surg 28(10):3102–3110
Omar I, Abualsel A (2019) Efficacy of intraperitoneal instillation of bupivacaine after bariatric surgery: randomized controlled trial. Obes Surg 29(6):1735–1741
Chin KJ, Malhas L, Perlas A (2017) The Erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: a report of 3 Cases. Reg Anesth Pain Med 42(3):372–376
Collins JS, Lemmens HJ, Brodsky JB (2006) Obesity and difficult intubation: where is the evidence?. Anesthesiology, 104(3):617; author reply 618–619
Moon TS, Fox PE, Somasundaram A et al (2019) The influence of morbid obesity on difficult intubation and difficult mask ventilation. J Anesth 33(1):96–102
Wong DT, Dallaire A, Singh KP et al (2019) High-flow nasal oxygen improves safe apnea time in morbidly obese patients undergoing general anesthesia: a randomized controlled trial. Anesth Analg 129(4):1130–1136
Fattahi T, Chafin C, Bunnell A (2017) Tracheostomy in the morbidly obese: difficulties and challenges. J Oral Maxillofac Surg 75(7):1372–1375
Lewis SR, Butler AR, Parker J, Cook TM, Smith AF (2016) Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation. Cochrane Database Syst Rev 11(11):Cd011136
Pieters BMA, Maas EHA, Knape JTA, van Zundert AAJ (2017) Videolaryngoscopy vs direct laryngoscopy use by experienced anaesthetists in patients with known difficult airways: a systematic review and meta-analysis. Anaesthesia 72(12):1532–1541
Downey AW, Duggan LV, Adam LJ (2021) A systematic review of meta-analyses comparing direct laryngoscopy with videolaryngoscopy. Can J Anaesth 68(5):706–714
Cordes SR, Best AR, Hiatt KK (2015) The impact of obesity on adult tracheostomy complication rate. Laryngoscope 125(1):105–110
Nightingale CE, Margarson MP, Shearer E et al (2015) Peri-operative management of the obese surgical patient 2015: association of Anaesthetists of Great Britain and Ireland Society for Obesity and Bariatric Anaesthesia. Anaesthesia 70(7):859–876
Writing Committee for the PCGotPVNftCTNotESoA, Bluth T, Serpa Neto A, Schultz MJ, Pelosi P, Gama de Abreu M 2019 Effect of Intraoperative High Positive End-Expiratory Pressure (PEEP) With Recruitment Maneuvers vs Low PEEP on Postoperative Pulmonary Complications in Obese Patients: A Randomized Clinical Trial. JAMA, 321(23):2292–2305
Young CC, Harris EM, Vacchiano C et al (2019) Lung-protective ventilation for the surgical patient: international expert panel-based consensus recommendations. Br J Anaesth 123(6):898–913
Villar J, Kacmarek RM, Hedenstierna G (2004) From ventilator-induced lung injury to physician-induced lung injury: why the reluctance to use small tidal volumes? Acta Anaesthesiol Scand 48(3):267–271
Rackley CR, MacIntyre NR (2019) Low tidal volumes for everyone? Chest 156(4):783–791
Borges JB, Amato MBP, Hedenstierna G (2017) The increasing call for protective ventilation during anesthesia. JAMA Surg 152(9):893–894
Neto AS, Hemmes SN, Barbas CS et al (2016) Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med 4(4):272–280
Futier E, Constantin JM, Paugam-Burtz C et al (2013) A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 369(5):428–437
Aldenkortt M, Lysakowski C, Elia N, Brochard L, Tramer MR (2012) Ventilation strategies in obese patients undergoing surgery: a quantitative systematic review and meta-analysis. Br J Anaesth 109(4):493–502
Pelosi P, Ravagnan I, Giurati G et al (1999) Positive end-expiratory pressure improves respiratory function in obese but not in normal subjects during anesthesia and paralysis. Anesthesiology 91(5):1221–1231
Costa Souza GM, Santos GM, Zimpel SA, Melnik T (2020) Intraoperative ventilation strategies for obese patients undergoing bariatric surgery: systematic review and meta-analysis. BMC Anesthesiol 20(1):36
Ball L, Hemmes SNT, Serpa Neto A et al (2018) Intraoperative ventilation settings and their associations with postoperative pulmonary complications in obese patients. Br J Anaesth 121(4):899–908
Pereira SM, Tucci MR, Morais CCA et al (2018) Individual Positive End-expiratory Pressure Settings Optimize Intraoperative Mechanical Ventilation and Reduce Postoperative Atelectasis. Anesthesiology 129(6):1070–1081
Amato MB, Meade MO, Slutsky AS et al (2015) Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 372(8):747–755
Ladha K, Vidal Melo MF, McLean DJ et al (2015) Intraoperative protective mechanical ventilation and risk of postoperative respiratory complications: hospital based registry study. BMJ 351:h3646
Ball L, Pelosi P (2019) How I ventilate an obese patient. Crit Care 23(1):176
Cadi P, Guenoun T, Journois D, Chevallier JM, Diehl JL, Safran D (2008) Pressure-controlled ventilation improves oxygenation during laparoscopic obesity surgery compared with volume-controlled ventilation. Br J Anaesth 100(5):709–716
Fernandez-Bustamante A, Hashimoto S, Serpa Neto A, Moine P, Vidal Melo MF, Repine JE (2015) Perioperative lung protective ventilation in obese patients. BMC Anesthesiol 15:56
Bagchi A, Rudolph MI, Ng PY et al (2017) The association of postoperative pulmonary complications in 109,360 patients with pressure-controlled or volume-controlled ventilation. Anaesthesia 72(11):1334–1343
Martini CH, Boon M, Bevers RF, Aarts LP, Dahan A (2014) Evaluation of surgical conditions during laparoscopic surgery in patients with moderate vs deep neuromuscular block. Br J Anaesth 112(3):498–505
Staehr-Rye AK, Rasmussen LS, Rosenberg J et al (2014) Surgical space conditions during low-pressure laparoscopic cholecystectomy with deep versus moderate neuromuscular blockade: a randomized clinical study. Anesth Analg 119(5):1084–1092
Barrio J, Errando CL, García-Ramón J, Sellés R, San Miguel G, Gallego J (2017) Influence of depth of neuromuscular blockade on surgical conditions during low-pressure pneumoperitoneum laparoscopic cholecystectomy: a randomized blinded study. J Clin Anesth 42:26–30
Kopman AF, Naguib M (2015) Laparoscopic surgery and muscle relaxants: is deep block helpful? Anesth Analg 120(1):51–58
Özdemir-van Brunschot DMD, Braat AE, van der Jagt MFP et al (2018) Deep neuromuscular blockade improves surgical conditions during low-pressure pneumoperitoneum laparoscopic donor nephrectomy. Surg Endosc 32(1):245–251
Torensma B, Martini CH, Boon M et al (2016) Deep neuromuscular block improves surgical conditions during bariatric surgery and reduces postoperative pain: a randomized double blind controlled trial. PLoS ONE 11(12):e0167907
Fuchs-Buder T, Schmartz D, Baumann C et al (2019) Deep neuromuscular blockade improves surgical conditions during gastric bypass surgery for morbid obesity: a randomised controlled trial. Eur J Anaesthesiol 36(7):486–493
Mulier JP, Dillemans B (2019) Anaesthetic factors affecting outcome after bariatric surgery, a retrospective levelled regression analysis. Obes Surg 29(6):1841–1850
Batistaki C, Tentes P, Deligiannidi P, Karakosta A, Florou P, Kostopanagiotou G (2016) Residual neuromuscular blockade in a real life clinical setting: correlation with sugammadex or neostigmine administration. Minerva Anestesiol 82(5):550–558
Fortier LP, McKeen D, Turner K et al (2015) The RECITE study: a canadian prospective, multicenter study of the incidence and severity of residual neuromuscular blockade. Anesth Analg 121(2):366–372
Schreiber JU (2014) Management of neuromuscular blockade in ambulatory patients. Curr Opin Anaesthesiol 27(6):583–588
Reinius H, Jonsson L, Gustafsson S et al (2009) Prevention of atelectasis in morbidly obese patients during general anesthesia and paralysis: a computerized tomography study. Anesthesiology 111(5):979–987
Murphy GS, Brull SJ (2010) Residual neuromuscular block: lessons unlearned Part I: definitions, incidence, and adverse physiologic effects of residual neuromuscular block. Anesth Analg 111(1):120–128
Stewart PA, Liang SS, Li QS et al (2016) The impact of residual neuromuscular blockade, oversedation, and hypothermia on adverse respiratory events in a postanesthetic care unit: a prospective study of prevalence, predictors, and outcomes. Anesth Analg 123(4):859–868
Butterly A, Bittner EA, George E, Sandberg WS, Eikermann M, Schmidt U (2010) Postoperative residual curarization from intermediate-acting neuromuscular blocking agents delays recovery room discharge. Br J Anaesth 105(3):304–309
Sauer M, Stahn A, Soltesz S, Noeldge-Schomburg G, Mencke T (2011) The influence of residual neuromuscular block on the incidence of critical respiratory events. A randomised, prospective, placebo-controlled trial. Eur J Anaesthesiol 28(12):842–848
Hristovska AM, Duch P, Allingstrup M, Afshari A (2018) The comparative efficacy and safety of sugammadex and neostigmine in reversing neuromuscular blockade in adults. A Cochrane systematic review with meta-analysis and trial sequential analysis. Anaesthesia 73(5):631–641
De Robertis E, Zito Marinosci G, Romano GM et al (2016) The use of sugammadex for bariatric surgery: analysis of recovery time from neuromuscular blockade and possible economic impact. Clinicoecon Outcomes Res 8:317–322
Kheterpal S, Vaughn MT, Dubovoy TZ et al (2020) Sugammadex versus neostigmine for reversal of neuromuscular blockade and postoperative pulmonary complications (STRONGER): a multicenter matched cohort analysis. Anesthesiology 132(6):1371–1381
Loupec T, Frasca D, Rousseau N, Faure JP, Mimoz O, Debaene B (2016) Appropriate dosing of sugammadex to reverse deep rocuronium-induced neuromuscular blockade in morbidly obese patients. Anaesthesia 71(3):265–272
Li D, Wang Y, Zhou Y, Yin C (2021) Efficacy and safety of sugammadex doses calculated on the basis of corrected body weight and total body weight for the reversal of deep neuromuscular blockade in morbidly obese patients. J Int Med Res 49(1):300060520985679
Badaoui R, Cabaret A, Alami Y et al (2016) Reversal of neuromuscular blockade by sugammadex in laparoscopic bariatric surgery: in support of dose reduction. Anaesth Crit Care Pain Med 35(1):25–29
de Kam PJ, Nolte H, Good S et al (2018) Sugammadex hypersensitivity and underlying mechanisms: a randomised study of healthy non-anaesthetised volunteers. Br J Anaesth 121(4):758–767
Min KC, Bondiskey P, Schulz V et al (2018) Hypersensitivity incidence after sugammadex administration in healthy subjects: a randomised controlled trial. Br J Anaesth 121(4):749–757
Lujan JA, Frutos MD, Hernandez Q et al (2004) Laparoscopic versus open gastric bypass in the treatment of morbid obesity: a randomized prospective study. Ann Surg 239(4):433–437
Nguyen NT, Goldman C, Rosenquist CJ et al (2001) Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg 234(3):279–289
Westling A, Gustavsson S (2001) Laparoscopic vs open Roux-en-Y gastric bypass: a prospective, randomized trial. Obes Surg 11(3):284–292
Buchwald H, Estok R, Fahrbach K, Banel D, Sledge I (2007) Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery 142(4):621–632
Angrisani L, Santonicola A, Iovino P et al (2018) IFSO Worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg 28(12):3783–3794
Zhou J, Du R, Wang L et al (2021) The application of enhanced recovery after surgery (ERAS) for patients undergoing bariatric surgery: a systematic review and meta-analysis. Obes Surg 31(3):1321–1331
Aktimur R, Kirkil C, Yildirim K, Kutluer N (2018) Enhanced recovery after surgery (ERAS) in one-anastomosis gastric bypass surgery: a matched-cohort study. Surg Obes Relat Dis 14(12):1850–1856
Blanchet MC, Gignoux B, Matussiere Y et al (2017) Experience with an enhanced recovery after surgery (ERAS) program for bariatric surgery: comparison of MGB and LSG in 374 patients. Obes Surg 27(7):1896–1900
Hahl T, Peromaa-Haavisto P, Tarkiainen P, Knutar O, Victorzon M (2016) OutCOME OF LAPAROSCOPIC GASTRIC BYPAss (LRYGB) with a program for enhanced recovery after surgery (ERAS). Obes Surg 26(3):505–511
Gero D, Raptis DA, Vleeschouwers W et al (2019) Defining global benchmarks in bariatric surgery: a retrospective multicenter analysis of minimally invasive roux-en-y gastric bypass and sleeve gastrectomy. Ann Surg 270(5):859–867
Zevin B, Aggarwal R, Grantcharov TP (2012) Volume-outcome association in bariatric surgery: a systematic review. Ann Surg 256(1):60–71
Stenberg E, Szabo E, Agren G et al (2014) Early complications after laparoscopic gastric bypass surgery: results from the scandinavian obesity surgery registry. Ann Surg 260(6):1040–1047
El-Kadre L, Tinoco AC, Tinoco RC, Aguiar L, Santos T (2013) Overcoming the learning curve of laparoscopic Roux-en-Y gastric bypass: a 12-year experience. Surg Obes Relat Dis 9(6):867–872
Bonrath EM, Dedy NJ, Gordon LE, Grantcharov TP (2015) Comprehensive surgical coaching enhances surgical skill in the operating room: a randomized controlled trial. Ann Surg 262(2):205–212
Breaux JA, Kennedy CI, Richardson WS (2007) Advanced laparoscopic skills decrease the learning curve for laparoscopic Roux-en-Y gastric bypass. Surg Endosc 21(6):985–988
Wolter S, Duprée A, ElGammal A et al (2019) Mentorship programs in bariatric surgery reduce perioperative complication rate at equal short-term outcome-results from the OPTIMIZE trial. Obes Surg 29(1):127–136
Pournaras DJ, Jafferbhoy S, Titcomb DR et al (2010) Three hundred laparoscopic Roux-en-Y gastric bypasses: managing the learning curve in higher risk patients. Obes Surg 20(3):290–294
Sánchez-Santos R, Estévez S, Tomé C et al (2012) Training programs influence in the learning curve of laparoscopic gastric bypass for morbid obesity: a systematic review. Obes Surg 22(1):34–41
van Rijswijk AS, Moes DE, Geubbels N et al (2018) Can a laparoscopic Roux-en-Y gastric bypass be safely performed by surgical residents in a bariatric center-of-excellence? The learning curve of surgical residents in bariatric surgery. Surg Endosc 32(2):1012–1020
Liscia G, Scaringi S, Facchiano E, Quartararo G, Lucchese M (2014) The role of drainage after Roux-en-Y gastric bypass for morbid obesity: a systematic review. Surg Obes Relat Dis 10(1):171–176
Doumouras AG, Maeda A, Jackson TD (2017) The role of routine abdominal drainage after bariatric surgery: a metabolic and bariatric surgery accreditation and quality improvement program study. Surg Obes Relat Dis 13(12):1997–2003
Peña ME, Schlottmann F, Laxague F, Sadava EE, Buxhoeveden R (2020) Usefulness of abdominal drain in laparoscopic roux-en-y gastric bypass: a randomized controlled trial. J Laparoendosc Adv Surg Tech A 30(5):538–541
Gundogan E, Kayaalp C, Aktas A et al (2018) Influence of drain placement on postoperative pain following laparoscopic Roux-en-Y gastric bypass for morbid obesity: randomized controlled trial. Obes Surg 28(11):3499–3504
Huerta S, Arteaga JR, Sawicki MP, Liu CD, Livingston EH (2002) Assessment of routine elimination of postoperative nasogastric decompression after Roux-en-Y gastric bypass. Surgery 132(5):844–848
Rossetti G, Fei L, Docimo L et al (2014) Is nasogastric decompression useful in prevention of leaks after laparoscopic sleeve gastrectomy? A randomized trial J Invest Surg 27(4):234–239
Robinson PD (2014) Obesity and its impact on the respiratory system. Paediatr Respir Rev 15(3):219–226
Eichenberger A, Proietti S, Wicky S et al (2002) Morbid obesity and postoperative pulmonary atelectasis: an underestimated problem. Anesth Analg 95(6):1788–1792
Ahlin S, Manco M, Panunzi S et al (2019) A new sensitive and accurate model to predict moderate to severe obstructive sleep apnea in patients with obesity. Medicine (Baltimore) 98(32):e16687
He J, Kryger MH, Zorick FJ, Conway W, Roth T (1988) Mortality and apnea index in obstructive sleep apnea. Experience in 385 male patients. Chest 94(1):9–14
Chung F, Yang Y, Liao P (2013) Predictive performance of the STOP-Bang score for identifying obstructive sleep apnea in obese patients. Obes Surg 23(12):2050–2057
Kaw R, Bhateja P, Paz YMH et al (2016) Postoperative complications in patients with unrecognized obesity hypoventilation syndrome undergoing elective noncardiac surgery. Chest 149(1):84–91
de Raaff CA, Coblijn UK, de Vries N, van Wagensveld BA (2016) Is fear for postoperative cardiopulmonary complications after bariatric surgery in patients with obstructive sleep apnea justified? A systematic review Am J Surg 211(4):793–801
Bolden N, Posner KL, Domino KB et al (2020) Postoperative critical events associated with obstructive sleep Apnea: results from the society of anesthesia and sleep medicine obstructive sleep apnea registry. Anesth Analg 131(4):1032–1041
Mehta V, Vasu TS, Phillips B, Chung F (2013) Obstructive sleep apnea and oxygen therapy: a systematic review of the literature and meta-analysis. J Clin Sleep Med 9(3):271–279
Young LR, Taxin ZH, Norman RG, Walsleben JA, Rapoport DM, Ayappa I (2013) Response to CPAP withdrawal in patients with mild versus severe obstructive sleep apnea/hypopnea syndrome. Sleep 36(3):405–412
Nagappa M, Mokhlesi B, Wong J, Wong DT, Kaw R, Chung F (2015) The effects of continuous positive airway pressure on postoperative outcomes in obstructive sleep apnea patients undergoing surgery: a systematic review and meta-analysis. Anesth Analg 120(5):1013–1023
Kohler M, Stoewhas AC, Ayers L et al (2011) Effects of continuous positive airway pressure therapy withdrawal in patients with obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med 184(10):1192–1199
Practice guidelines for the perioperative management of patients with obstructive sleep apnea: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Anesthesiology. 2014;120(2):268–286.
Daigle CR, Brethauer SA, Tu C et al (2018) Which postoperative complications matter most after bariatric surgery? Prioritizing quality improvement efforts to improve national outcomes. Surg Obes Relat Dis 14(5):652–657
Samama MM (2000) An epidemiologic study of risk factors for deep vein thrombosis in medical outpatients: the Sirius study. Arch Intern Med 160(22):3415–3420
Moulin PA, Dutour A, Ancel P et al (2017) Perioperative thromboprophylaxis in severely obese patients undergoing bariatric surgery: insights from a French national survey. Surg Obes Relat Dis 13(2):320–326
Clark LN, Helm MC, Gould JC (2019) Practice patterns regarding post-discharge chemoprophylaxis for venous thromboembolism following bariatric surgery in the United States. Surg Obes Relat Dis 15(5):703–707
Brotman DJ, Shihab HM, Prakasa KR et al (2013) Pharmacologic and mechanical strategies for preventing venous thromboembolism after bariatric surgery: a systematic review and meta-analysis. JAMA Surg 148(7):675–686
Kakkos SK, Caprini JA, Geroulakos G et al (2016) Combined intermittent pneumatic leg compression and pharmacological prophylaxis for prevention of venous thromboembolism. Cochrane Database Syst Rev 9(9):Cd005258
Sachdeva A, Dalton M, Lees T (2018) Graduated compression stockings for prevention of deep vein thrombosis. Cochrane Database Syst Rev 11(11):Cd001484
Abildgaard A, Madsen SA, Hvas AM (2020) Dosage of anticoagulants in obesity: recommendations based on a systematic review. Semin Thromb Hemost 46(8):932–969
Karas LA, Nor Hanipah Z, Cetin D et al (2021) Assessment of empiric body mass index-based thromboprophylactic dosing of enoxaparin after bariatric surgery: evidence for dosage adjustment using anti-factor Xa in high-risk patients. Surg Obes Relat Dis 17(1):153–160
Stier C, Koschker AC, Stier R, Sosnierz A, Chiappetta S (2020) Are we missing treatment standards for thromboprophylaxis of the obese and super-obese patient population? A prospective systematic cohort study. Obes Surg 30(5):1704–1711
Aminian A, Andalib A, Khorgami Z et al (2017) Who should get extended thromboprophylaxis after bariatric surgery?: a risk assessment tool to guide indications for post-discharge pharmacoprophylaxis. Ann Surg 265(1):143–150
Mossberg KE, Pournaras DJ, Welbourn R, le Roux CW, Brogren H (2017) Differential response of plasma plasminogen activator inhibitor 1 after weight loss surgery in patients with or without type 2 diabetes. Surg Obes Relat Dis 13(1):53–57
Bergqvist D, Agnelli G, Cohen AT et al (2002) Duration of prophylaxis against venous thromboembolism with enoxaparin after surgery for cancer. N Engl J Med 346(13):975–980
Hull RD, Pineo GF, Stein PD et al (2001) Extended out-of-hospital low-molecular-weight heparin prophylaxis against deep venous thrombosis in patients after elective hip arthroplasty: a systematic review. Ann Intern Med 135(10):858–869
Rowland SP, Dharmarajah B, Moore HM et al (2015) Inferior vena cava filters for prevention of venous thromboembolism in obese patients undergoing bariatric surgery: a systematic review. Ann Surg 261(1):35–45
Shoar S, Saber AA, Rubenstein R et al (2018) Portomesentric and splenic vein thrombosis (PMSVT) after bariatric surgery: a systematic review of 110 patients. Surg Obes Relat Dis 14(1):47–59
Shaheen O, Siejka J, Thatigotla B, Pham DT (2017) A systematic review of portomesenteric vein thrombosis after sleeve gastrectomy. Surg Obes Relat Dis 13(8):1422–1431
Parrott J, Frank L, Rabena R, Craggs-Dino L, Isom KA, Greiman L (2017) American society for metabolic and bariatric surgery integrated health nutritional guidelines for the surgical weight loss patient 2016 update: micronutrients. Surg Obes Relat Dis 13(5):727–741
Parrott JM, Craggs-Dino L, Faria SL, O’Kane M (2020) The optimal nutritional programme for bariatric and metabolic surgery. Curr Obes Rep 9(3):326–338
O’Kane M (2021) Nutritional consequences of bariatric surgery - prevention, detection and management. Curr Opin Gastroenterol 37(2):135–144
O’Kane M, Parretti HM, Pinkney J et al (2020) British obesity and metabolic surgery society guidelines on perioperative and postoperative biochemical monitoring and micronutrient replacement for patients undergoing bariatric surgery-2020 update. Obes Rev 21(11):e13087
Di Lorenzo N, Antoniou SA, Batterham RL et al (2020) Clinical practice guidelines of the european association for endoscopic surgery (EAES) on bariatric surgery: update 2020 endorsed by IFSO-EC. EASO and ESPCOP Surg Endosc 34(6):2332–2358
Sherf-Dagan S, Sinai T, Goldenshluger A et al (2021) Nutritional assessment and preparation for adult bariatric surgery candidates: clinical practice. Adv Nutr 12(3):1020–1031
Sherf Dagan S, Goldenshluger A, Globus I et al (2017) Nutritional recommendations for adult bariatric surgery patients: clinical practice. Adv Nutr 8(2):382–394
Shoar S, Poliakin L, Rubenstein R, Saber AA (2018) Single anastomosis duodeno-ileal switch (SADIS): a systematic review of efficacy and safety. Obes Surg 28(1):104–113
Homan J, Betzel B, Aarts EO et al (2015) Vitamin and mineral deficiencies after biliopancreatic diversion and biliopancreatic diversion with duodenal switch–the rule rather than the exception. Obes Surg 25(9):1626–1632
Coblijn UK, Goucham AB, Lagarde SM, Kuiken SD, van Wagensveld BA (2014) Development of ulcer disease after Roux-en-Y gastric bypass, incidence, risk factors, and patient presentation: a systematic review. Obes Surg 24(2):299–309
Ying VW, Kim SH, Khan KJ et al (2015) Prophylactic PPI help reduce marginal ulcers after gastric bypass surgery: a systematic review and meta-analysis of cohort studies. Surg Endosc 29(5):1018–1023
Kang X, Zurita-Macias L, Hong D, Cadeddu M, Anvari M, Gmora S (2016) A comparison of 30-day versus 90-day proton pump inhibitor therapy in prevention of marginal ulcers after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 12(5):1003–1007
Wennerlund J, Gunnarsson U, Strigård K, Sundbom M (2020) Acid-related complications after laparoscopic Roux-en-Y gastric bypass: risk factors and impact of proton pump inhibitors. Surg Obes Relat Dis 16(5):620–625
Collares-Pelizaro RVA, Santos JS, Nonino CB, dos Reis Dias LA, Gaitani CM, Salgado W Jr (2017) Omeprazole absorption and fasting gastrinemia after Roux-en-Y gastric bypass. Obes Surg 27(9):2303–2307
Schulman AR, Chan WW, Devery A, Ryan MB, Thompson CC (2017) Opened Proton Pump Inhibitor Capsules Reduce Time to Healing Compared With Intact Capsules for Marginal Ulceration Following Roux-en-Y Gastric Bypass. Clin Gastroenterol Hepatol 15(4):494-500.e491
Mandeville Y, Van Looveren R, Vancoillie PJ et al (2017) Moderating the enthusiasm of sleeve gastrectomy: up to fifty percent of reflux symptoms after ten years in a consecutive series of one hundred laparoscopic sleeve gastrectomies. Obes Surg 27(7):1797–1803
Kraljević M, Cordasco V, Schneider R et al (2021) Long-term effects of laparoscopic sleeve gastrectomy: what are the results beyond 10 years? Obes Surg 31(8):3427–3433
Braghetto I, Korn O (2019) Late esophagogastric anatomic and functional changes after sleeve gastrectomy and its clinical consequences with regards to gastroesophageal reflux disease. Dis Esophagus 32(6):doz020
Sebastianelli L, Benois M, Vanbiervliet G et al (2019) Systematic endoscopy 5 years after sleeve gastrectomy results in a high rate of barrett’s esophagus: results of a multicenter study. Obes Surg 29(5):1462–1469
Adams LB, Chang C, Pope J, Kim Y, Liu P, Yates A (2016) Randomized, prospective comparison of ursodeoxycholic acid for the prevention of gallstones after sleeve gastrectomy. Obes Surg 26(5):990–994
Sakran N, Dar R, Assalia A et al (2020) The use of ursolit for gallstone prophylaxis following bariatric surgery: a randomized-controlled trial. Updates Surg 72(4):1125–1133
Miller K, Hell E, Lang B, Lengauer E (2003) Gallstone formation prophylaxis after gastric restrictive procedures for weight loss: a randomized double-blind placebo-controlled trial. Ann Surg 238(5):697–702
Wudel LJ Jr, Wright JK, Debelak JP, Allos TM, Shyr Y, Chapman WC (2002) Prevention of gallstone formation in morbidly obese patients undergoing rapid weight loss: results of a randomized controlled pilot study. J Surg Res 102(1):50–56
Sugerman HJ, Brewer WH, Shiffman ML et al (1995) A multicenter, placebo-controlled, randomized, double-blind, prospective trial of prophylactic ursodiol for the prevention of gallstone formation following gastric-bypass-induced rapid weight loss. Am J Surg 169(1):91–96
Magouliotis DE, Tasiopoulou VS, Svokos AA et al (2017) Ursodeoxycholic acid in the prevention of gallstone formation after bariatric surgery: an updated systematic review and meta-analysis. Obes Surg 27(11):3021–3030
Boerlage TCC, Haal S, Maurits de Brauw L et al (2017) Ursodeoxycholic acid for the prevention of symptomatic gallstone disease after bariatric surgery: study protocol for a randomized controlled trial (UPGRADE trial). BMC Gastroenterol 17(1):164
Leyva-Alvizo A, Arredondo-Saldaña G, Leal-Isla-Flores V et al (2020) Systematic review of management of gallbladder disease in patients undergoing minimally invasive bariatric surgery. Surg Obes Relat Dis 16(1):158–164
Wanjura V, Szabo E, Osterberg J, Ottosson J, Enochsson L, Sandblom G (2018) Morbidity of cholecystectomy and gastric bypass in a national database. Br J Surg 105(1):121–127
Pournaras DJ, Aasheim ET, Bueter M et al (2012) Effect of bypassing the proximal gut on gut hormones involved with glycemic control and weight loss. Surg Obes Relat Dis 8(4):371–374
Poelemeijer YQM, Liem RSL, Vage V et al (2020) Gastric bypass versus sleeve gastrectomy: patient selection and short-term outcome of 47,101 primary operations from the Swedish, Norwegian, and Dutch national quality registries. Ann Surg 272(2):325–333
Frisch A, Chandra P, Smiley D et al (2010) Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care 33(8):1783–1788
Kwon S, Thompson R, Dellinger P, Yanez D, Farrohki E, Flum D (2013) Importance of perioperative glycemic control in general surgery: a report from the Surgical Care and Outcomes Assessment Program. Ann Surg 257(1):8–14
King JT Jr, Goulet JL, Perkal MF, Rosenthal RA (2011) Glycemic control and infections in patients with diabetes undergoing noncardiac surgery. Ann Surg 253(1):158–165
Pournaras DJ, Osborne A, Hawkins SC et al (2010) Remission of type 2 diabetes after gastric bypass and banding: mechanisms and 2 year outcomes. Ann Surg 252(6):966–971
Fenske WK, Pournaras DJ, Aasheim ET et al (2012) Can a protocol for glycaemic control improve type 2 diabetes outcomes after gastric bypass? Obes Surg 22(1):90–96
Thorell A, Hagström-Toft E (2012) Treatment of diabetes prior to and after bariatric surgery. J Diabetes Sci Technol 6(5):1226–1232
Pournaras DJ, Hardwick RH, le Roux CW (2017) Gastrointestinal surgery for obesity and cancer: 2 sides of the same coin. Surg Obes Relat Dis 13(4):720–721
Fearon KC, Ljungqvist O, Von Meyenfeldt M et al (2005) Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 24(3):466–477
Tian YL, Cao SG, Liu XD et al (2020) Short- and long-term outcomes associated with enhanced recovery after surgery protocol vs conventional management in patients undergoing laparoscopic gastrectomy. World J Gastroenterol 26(37):5646–5660
Gustafsson UO, Scott MJ, Hubner M et al (2019) Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS(®)) society recommendations: 2018. World J Surg 43(3):659–695
Acknowledgements
The authors thank Dr. Mark Smeets, Groene Hart Hospital and Leiden University Medical Center, the Netherlands, for his assistance in part of the literature review.
Funding
Open access funding provided by Örebro University. This study was supported by grants from Region Örebro County (Grant No. OLL-939106), The Bengt Ihre Foundation, and The Erling-Persson Family foundation (Grant No. 140604).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
ES has received a speaker honorarium from Johnson & Johnson Medical. LF has received speaker honorarium from Merck Sharp & Dohme, Pfizer and Baxter. MK has received speaker honoraria and personal fees from NovoNordisk, speaker honoraria from Johnson & Johnson Medical, and is member of the IFSO Executive Board and Chair of the IFSO Integrated health Committee, Trustee of the ASO, Committee Member of the BDA Obesity Specialist Group, and Member of the Byband Sleeve Trial Management Group. RL has received speaker honorarium from Johnson & Johnson Medical, and Medtronic, and is the past president of the DSMBS. DP has received consulting fees and speaker honorarium from Johnson & Johnson Medical, speaker honorarium from Medtronic and NovoNordisk. PS has received speaker honorarium from OrionPharma and Merck, and is a member of the BEST-study data safety monitoring committee. RU reports grants and/or consulting fees from Merck, Medtronic, AcelRx, Acacia, Heron and Pfizer; grant support from NIH, NSF and AHRQ. He also reports leadership roles in the ERAS USA and ISPCOP societies. AW is the President of ISPCOP. UG is a member of the ERAS Society Executive committee. AT has received unrestricted research grants (to institution) from Ethicon Endo-Surgery, is a member of advisory board for Novo Nordisk and Ethicon Endo-Surgery and has received speakers honoraria from Kabi Fresenius and Ethicon Endo-Surgery.
Ethical approval
The study was conducted in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The Conflict of Interest statement was corrected.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Stenberg, E., dos Reis Falcão, L.F., O’Kane, M. et al. Guidelines for Perioperative Care in Bariatric Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations: A 2021 Update. World J Surg 46, 729–751 (2022). https://doi.org/10.1007/s00268-021-06394-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06394-9