Abstract
Background
Laparoscopic sleeve gastrectomy is the most commonly performed bariatric surgery in the world. Enhanced recovery after surgery (ERAS) protocols have been shown to reduce complications and decrease length of stay for various types of surgeries. In this study, we propose an ERAS protocol for laparoscopic sleeve gastrectomy and compare the clinical outcomes with patients who received standard care.
Methods
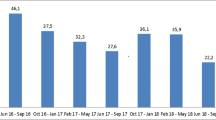
We performed a single-institution retrospective analysis in patients who underwent laparoscopic sleeve gastrectomy from February 2015 to December 2017. Patients were stratified into standard care and ERAS protocol groups. The ERAS protocol consisted of goal-directed patient education, specific pre- and post-op multi-modal medication regimen, early ambulation, and early oral intake. Patients were discharged on their first post-operative day if they met appropriate post-surgical milestones. The primary outcomes were length of stay, 7- and 30-day readmission rates, and complication rates. Secondary outcomes included anti-emetic and pain medication utilization, post-operative emesis episodes per day, post-operative pain scores, and mortality.
Results
We included 214 consecutive patients who underwent sleeve gastrectomy, 130 were in the ERAS group and 84 were in the standard care group. Median hospital stay was significantly shorter in the ERAS group compared to the standard care group (1 vs. 2 days; p < 0.001). There were no differences in 7- or 30-day readmission rates (1.5 vs. 1.2%; p = 0.838, 2.3 vs. 2.4%; p = 0.966) or post-operative complications (6.2 vs. 3.6%; p = 0.410). The ERAS group also had decreased median intra-operative opioid consumption and self-reported pain scores on post-operative day 1 (27.5 MME vs. 27.4 MME; p = 0.044, 3.3 vs. 3.9; p = 0.046). Mortality rate was 0% overall.
Conclusion
A cost-effective ERAS protocol for laparoscopic sleeve gastrectomy results in shorter length of stay, without increase in peri-operative morbidity or readmission rates.

Similar content being viewed by others
References
Regan JP, Inabnet WB, Gagner M, Pomp A (2003) Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese patient. Obes Surg 13(6):861–864. https://doi.org/10.1381/096089203322618669
Ren CJ, Patterson E, Gagner M (2000) Early results of laparoscopic biliopancreatic diversion with duodenal switch: a case series of 40 consecutive patients. Obes Surg 10(6):514–523. https://doi.org/10.1381/096089200321593715 discussion 524.
Dapri G, Cadière GB, Himpens J Superobese and super-superobese patients: 2-step laparoscopic duodenal switch. Surg Obes Relat Dis 7 (6):703–708. https://doi.org/10.1016/j.soard.2011.09.007
Cottam D, Qureshi FG, Mattar SG, Sharma S, Holover S, Bonanomi G, Ramanathan R, Schauer P (2006) Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high-risk patients with morbid obesity. Surg Endosc Other Intervent Tech 20(6):859–863. https://doi.org/10.1007/s00464-005-0134-5
English WJ, DeMaria EJ, Brethauer SA, Mattar SG, Rosenthal RJ, Morton JM (2018) American society for metabolic and bariatric surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis 14(3):259–263. https://doi.org/10.1016/j.soard.2017.12.013
Himpens J, Dobbeleir J, Peeters G (2010) Long-term Results of Laparoscopic Sleeve Gastrectomy for Obesity. Ann Surg 252(2):319–324. https://doi.org/10.1097/SLA.0b013e3181e90b31
D’Hondt M, Vanneste S, Pottel H, Devriendt D, Van Rooy F, Vansteenkiste F (2011) Laparoscopic sleeve gastrectomy as a single-stage procedure for the treatment of morbid obesity and the resulting quality of life, resolution of comorbidities, food tolerance, and 6-year weight loss. Surg Endosc 25(8):2498–2504. https://doi.org/10.1007/s00464-011-1572-x
Sarela AI, Dexter SPL, O’Kane M, Menon A, McMahon MJ (2012) Long-term follow-up after laparoscopic sleeve gastrectomy: 8–9-year results. Surg Obes Relat Dis 8 (6):679–684. https://doi.org/10.1016/j.soard.2011.06.020
Ma IT, Madura JA 2nd (2015) Gastrointestinal complications after bariatric surgery. Gastroenterol Hepatol 11(8):526–535
Kehlet H, Mogensen T (1999) Hospital stay of 2 days after open sigmoidectomy with a multimodal rehabilitation programme. Br J Surg 86(2):227–230. https://doi.org/10.1046/j.1365-2168.1999.01023.x
Varadhan KK, Neal KR, Dejong CHC, Fearon KCH, Ljungqvist O, Lobo DN (2010) The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr 29 (4):434–440. https://doi.org/10.1016/j.clnu.2010.01.004
Lassen K, Soop M, Nygren J et al (2009) Consensus review of optimal perioperative care in colorectal surgery: enhanced recovery after surgery (eras) group recommendations. Arch Surg 144(10):961–969. https://doi.org/10.1001/archsurg.2009.170
Ni T-G, Yang H-T, Zhang H, Meng H-P, Li B (2015) Enhanced recovery after surgery programs in patients undergoing hepatectomy: a meta-analysis. WJG 21(30):9209–9216. https://doi.org/10.3748/wjg.v21.i30.9209
Coolsen MM, van Dam RM, van der Wilt AA, Slim K, Lassen K, Dejong CH (2013) Systematic review and meta-analysis of enhanced recovery after pancreatic surgery with particular emphasis on pancreaticoduodenectomies. World J Surg 37(8):1909–1918. https://doi.org/10.1007/s00268-013-2044-3
Tyson MD, Chang SS (2016) Enhanced recovery pathways versus standard care after cystectomy: a meta-analysis of the effect on perioperative outcomes. Eur Urol 70(6):995–1003. https://doi.org/10.1016/j.eururo.2016.05.031
Thorell A, MacCormick AD, Awad S, Reynolds N, Roulin D, Demartines N, Vignaud M, Alvarez A, Singh PM, Lobo DN (2016) Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg 40(9):2065–2083. https://doi.org/10.1007/s00268-016-3492-3
Kahokehr A, Sammour T, Zargar-Shoshtari K, Thompson L, Hill AG (2009) Implementation of ERAS and how to overcome the barriers. Int J Surg (London England) 7(1):16–19. https://doi.org/10.1016/j.ijsu.2008.11.004
Alawadi ZM, Leal I, Phatak UR, Flores-Gonzalez JR, Holihan JL, Karanjawala BE, Millas SG, Kao LS (2016) Facilitators and barriers of implementing enhanced recovery in colorectal surgery at a safety net hospital: a provider and patient perspective. Surgery 159(3):700–712. https://doi.org/10.1016/j.surg.2015.08.025
Stone AB, Grant MC, Pio Roda C, Hobson D, Pawlik T, Wu CL, Wick EC (2016) Implementation costs of an enhanced recovery after surgery program in the United States: a financial model and sensitivity analysis based on experiences at a quaternary academic medical center. J Am Coll Surg 222(3):219–225. https://doi.org/10.1016/j.jamcollsurg.2015.11.021
Lemanu DP, Singh PP, Berridge K, Burr M, Birch C, Babor R, MacCormick AD, Arroll B, Hill AG (2013) Randomized clinical trial of enhanced recovery versus standard care after laparoscopic sleeve gastrectomy. Br J Surg 100(4):482–489. https://doi.org/10.1002/bjs.9026
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Spanjersberg WR, Reurings J, Keus F, van Laarhoven CJ (2011) Fast track surgery versus conventional recovery strategies for colorectal surgery. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD007635.pub2
Ljungqvist O, Thanh NX, Nelson G (2017) ERAS—value based surgery. J Surg Oncol 116(5):608–612. https://doi.org/10.1002/jso.24820 doi
Simonelli V, Goergen M, Orlando GG, Arru L, Zolotas CA, Geeroms M, Poulain V, Azagra JS (2016) Fast-track in bariatric and metabolic surgery: feasibility and cost analysis through a matched-cohort study in a single centre. Obes Surg 26(8):1970–1977. https://doi.org/10.1007/s11695-016-2255-4
Rebibo L, Dhahri A, Badaoui R, Dupont H, Regimbeau J-M (2014) Laparoscopic sleeve gastrectomy as day-case surgery (without overnight hospitalization), vol 11. https://doi.org/10.1016/j.soard.2014.08.017
Inaba C, Koh C, Sujatha-Bhaskar S, Nguyen N (2017) How safe is same-day discharge for laparoscopic sleeve gastrectomy? Surg Obes Relat Dis 13(10):S15. https://doi.org/10.1016/j.soard.2017.09.035
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Bryan J. Sandler reports Consulting Fee for ValenTx, Inc, and Honoraria for Gore and Bard-Davol; Garth R. Jacobsen reports Honoraria for Gore, Bard-Davol, and Ethicon. Santiago Horgan reports Consulting Fee for Fortimedix, Stryker and ValenTx, Inc. and Speaker for Ethicon. Authors Jenny Lam, Toshiaki Suzuki, Carlos Maeda, Beiqun Zhao, David Bernstein, and Thach Pham have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Lam, J., Suzuki, T., Bernstein, D. et al. An ERAS protocol for bariatric surgery: is it safe to discharge on post-operative day 1?. Surg Endosc 33, 580–586 (2019). https://doi.org/10.1007/s00464-018-6368-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6368-9