Abstract
Introduction
High-resolution esophageal manometry (HREM) is essential in characterizing achalasia subtype and the extent of affected segment to plan the myotomy starting point during per-oral endoscopic myotomy (POEM). However, evidence is lacking that efficacy is improved by tailoring myotomy to the length of the spastic segment on HREM. We sought to investigate whether utilizing HREM to dictate myotomy length in POEM impacts postoperative outcomes.
Methods
Comparative analysis of HREM-tailored to non-tailored patients from a prospectively collected database of all POEMs at our institution January 2011 through July 2017. A tailored myotomy is defined as extending at least the length of the diseased segment, as initially measured on HREM.
Results
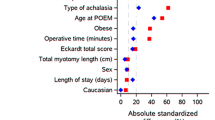
Forty patients were included (11 tailored versus 29 non-tailored). There were no differences in patient age (p = 0.6491) or BMI (p = 0.0677). Myotomy lengths were significantly longer for tailored compared to non-tailored overall (16.6 ± 2.2 versus 13.5 ± 1.8; p < 0.0001), and for only type III achalasia (15.9 ± 2.4 versus 12.7 ± 1.2; p = 0.0453), likely due to more proximal starting position in tailored cases (26.0 ± 2.2 versus 30.0 ± 2.7; p < 0.0001). Procedure success (Eckardt < 3) was equivalent across groups overall (p = 0.5558), as was postoperative Eckardt score (0.2 ± 0.4 versus 0.8 ± 2.3; p = 0.4004). Postoperative Eckardt score was significantly improved in the tailored group versus non-tailored for type III only (0.2 ± 0.4 versus 1.3 ± 1.5; p = 0.0435). A linear correlation was seen between increased length and greater improvement in Eckardt score in the non-tailored group (p = 0.0170).
Conclusions
Using HREM to inform surgeons of the proximal location of the diseased segment resulted in longer myotomies, spanning the entire affected segment in type III achalasia, and in lower postoperative Eckardt scores. Longer myotomy length is often more easily achieved with POEM than with Heller myotomy, which raises the question of whether POEM results in better outcomes for type III achalasia, as types I and II do not generally have measurable spastic segments.


Similar content being viewed by others
Abbreviations
- LES:
-
Lower esophageal sphincter
- HREM:
-
High-resolution esophageal manometry
- POEM:
-
Per-oral endoscopic myotomy
- EGJOO:
-
Esophagogastric junction outflow obstruction
- LHM:
-
Laparoscopic Heller myotomy
- BMI:
-
Body mass index
- IRP:
-
Integrated relaxation pressure
- Botox:
-
Botulinum toxin
References
Pandolfino JE, Gawron AJ (2015) Achalasia: a systematic review. JAMA 313(18):1841–1852
Sadowski DC, Ackah F, Jiang B, Svenson LW (2010) Achalasia: incidence, prevalence, and survival. A population-based study. Neurogastroenterol Motil 22:256–261
Eckardt VF (2001) Clinical presentation and complications of achalasia. Gastrointest Endosc Clin N Am 11:281–292
Chandrasekhara V, Desilets D, Falk GW, Inoue H, Romanelli JR, Savides TJ, Stavropoulos SN, Swanstrom LL, ASGE PIVI Committee (2015) The American Society for Gastrointestinal Endoscopy PIVI (Preservation and incorporation of valuable endoscopic innovations on peroral endoscopic myotomy). Gastrointest Endosc 81:1087–1099
Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB et al (2007) Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy 39:761–764
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M et al (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42:265–271
Inoue H, Sato H, Ikeda H, Onimaru M, Sato C, et al. (2015) Per-oral endoscopic myotomy: a series of 500 patients. JACS 221:256–264
Bechara R, Onimaru M, Ikeda H, Inoue H (2016) Per-oral endoscopic myotomy, 1000 cases later: pearls, pitfalls, and practical considerations. Gastrointest Endosc 84:330–338
Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJ, International High Resolution Manometry Working Group (2012) Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil 24(Suppl 1):57–65
Rohof WO, Salvador R, Annese V, Bruley des Varannes S, Chaussade S, Costantini M, Elizalde JI, Gaudric M, Smout AJ, Tack J, Busch OR, Zaninotto G, Boeckxstaens GE (2013) Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterology 144(4):718–725 (quiz e13–e14)
Salvador R, Costantini M, Zaninotto G, Morbin T, Rizzetto C, Zanatta L, Ceolin M, Finotti E, Nicoletti L, Da Dalt G, Cavallin F (2010) The preoperative manometric pattern predicts the outcome of surgical treatment for esophageal achalasia. J Gastrointest Surg 14(11):1635–1645
Kim WH, Cho JY, Ko WJ, Hong SP, Hahm KB, Cho JH, Lee TH, Hong SJ (2009) Comparison of the outcomes of peroral endoscopic myotomy for achalasia according to manometric subtype. Gut Liver 11(5):642–647
Pandolfino JE, Fox MR, Bredenoord AJ, Kahrilas PJ (2009) High-resolution manometry in clinical practice: utilizing pressure topography to classify oesophageal motility abnormalities. Neurogastroenterol Motil 21:796–806
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S et al (2015) The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27(2):160–174
Kahrilas PJ, Katzka D, Richter JE (2017 Nov) Clinical practice update: the use of per-oral endoscopic myotomy in achalasia: expert review and best practice advice from the AGA institute. Gastroenterology 153(5):1205–1211
Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ (2008) Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 135:1526–1533
Pratap N, Kalapala R, Darisetty S, Joshi N, Ramchandani M, Banerjee R, Lakhtakia S, Gupta R, Tandan M, Rao GV, Reddy DN (2011) Achalasia cardia subtyping by high-resolution manometry predicts the therapeutic outcome of pneumatic balloon dilatation. J Neurogastroenterol Motil 17:48–53
Ou YH, Nie XM, Li LF, Wei ZJ, Jiang B (2016) High-resolution manometric subtypes as a predictive factor for the treatment of achalasia: a meta-analysis and systematic review. J Dig Dis 17:222–235
Rahden BH, Filser J, Al-Nasser M, Germer CT (2017) Surgical treatment of achalasia—endoscopic or laparoscopic? Proposal for a tailored approach. Chirurg 88(3):204–210
Lee H, Chung H, Lee TH, Hong KS, Youn YH, Park JH, Park HS, Park H, Korean Achalasia Study Team (KAST) (2017) Therapeutic outcome of achalasia based on high-resolution manometry: a Korean multicenter study. Am J Ther
Crespin OM, Tatum RP, Xiao K, Martin AV, Khandelwal S, Pellegrini CA, Oelschlager BK (2017) The relationship between manometric subtype and outcomes of surgical treatment for patients with achalasia: Achalasia: manometric subtypes. Surg Endosc 31:5066–5075
Kumbhari V, Tieu AH, Onimaru M, El Zein MH, Teitelbaum EN et al (2015) Peroral endoscopic myotomy (POEM) vs laparoscopic Heller myotomy (LHM) for the treatment of type III achalasia in 75 patients: a multicenter comparative study. Endosc Int Open 3:E195–E201
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJPM, Pandolfino JE (2017) Advances in the management of oesophageal motility disorders in the era of high-resolution manometry: a focus on achalasia syndromes. Gastroenterol Hepatol 14:677–688
Ihara E, Muta K, Fukaura K, Nakamura K (2017) Diagnosis and treatment strategy of achalasia subtypes and esophagogastric junction outflow obstruction based on high-resolution manometry. Digestion 95(5):29–35
Greene CL, Chang EJ, Oh DS, Worell SG, Hagen JA, DeMeester SR (2015) High resolution manometry sub-classification of achalasia: does it really matter? Surg Endosc 29(6):1363–1367
Chen X, Li Q-p, Ji G-z, Ge X-x, Zhang X-h, Miao L (2015) Two-year follow-up for 45 patients with achalasia who underwent peroral endoscopic myotomy. Eur J Cardiothroac Surg 47:890–896
Zhang W, Linghu E-Q (2017) Peroral endoscopic myotomy for type III achalasia of Chicago classification: outcomes with a minimum follow-up of 24 months. J Gastrointest Surg 21:785–791
Khashab MA, Messallam AA, Onimaru M, Teitelbaum EN, Ujiki MB, Gitelis ME, Modayil RJ, Hungness ES, Stavropoulos SN, El Zein MH, Shiwaku H, Kunda R, Repici A, Minami H, Chiu PW, Ponsky J, Kumbhari V, Saxena P, Maydeo AP, Inoue H (2015) International multicenter experience with peroral endoscopic myotomy for the treatment of spastic esophageal disorders refractory to medical therapy (with video). Gastrointest Endosc 81(5):1170–1177
Martinek J, Svecova H, Vackova Z, Dolezel R, Ngo O, Krajciova J, Kieslichova E, Janousek R, Pazdro A, Harustiak T, Zdrhova L, Loudova P, Stirand P, Spicak J (2018) Per-oral endoscopic myotomy (POEM): mid-term efficacyand safety. Surg Endosc 32(3):1293–1302
Khan MA, Kumbhari V, Ngamruenengphong S, Ismail A, Chen Y et al (2017) Is POEM the answer for management of spastic esophageal disorders? A systematic review and meta-analysis. Dig Dis Sci 62:35–44
Guo H, Yang H, Zhang X, Wang L, Lv Y, Zou X, Ling T (2017) Long-term outcomes of peroral endoscopic myotomy for patients with achalasia: a retrospective single-center study. Dis Esophagus 30(5):1–6
Ju H, Ma Y, Liang K, Zhang C, Tian Z (2016) Function of high-resolution manometry in the analysis of peroral endoscopic myotomy for achalasia. Surg Endosc 30:1094–1099
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. John R. Romanelli is a consultant for Covidien but no funding or support was received for this work. Drs. David J. Desilets, Vikram Budhraja, and Erica D. Kane have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Kane, E.D., Budhraja, V., Desilets, D.J. et al. Myotomy length informed by high-resolution esophageal manometry (HREM) results in improved per-oral endoscopic myotomy (POEM) outcomes for type III achalasia. Surg Endosc 33, 886–894 (2019). https://doi.org/10.1007/s00464-018-6356-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6356-0