Abstract
Introduction
The American Society of Anesthesiologists (ASA) physical status classification system was developed as a simple categorization of patients’ physiological status that predicts the operative risk. Peroral endoscopic myotomy (POEM) is a less invasive alternative to surgical myotomy in achalasia. As such, POEM seems to be an appealing option for high-risk patients with achalasia. However, there are no studies which systematically analyzed the outcomes of POEM among patients with different ASA classes. Hence, we aimed to compare the safety and efficacy of POEM in patients with lower and higher ASA classes.
Methods
Medical records of all achalasia patients who underwent POEM at our institution between April 2014 and May 2019 were reviewed. Patients were categorized arbitrarily into two groups, lower ASA class (ASA I and II combined) and higher ASA class (ASA class III and IV combined). Demographic and procedural details, timed barium swallow (TBE), high-resolution esophageal manometry (HREM), pH study findings and Eckardt scores were compared between the two groups. Baseline characteristics were compared using Chi-square test and two-sample t-test for categorical and continuous variables, respectively.
Results
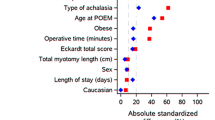
A total of 144 patients met our study criteria (lower ASA class, n = 44; and higher ASA class, n = 100). Patients in higher ASA class were significantly more obese and older. More patients in lower ASA class had prior Heller myotomy and more patients in higher ASA Class had prior botulinum toxin injections. Procedural parameters were similar in both groups. Procedural complications were infrequent and were also similar in the two groups. The length of stay, 30-day readmission rate, reflux symptoms and esophageal pH study findings were also comparable between the two groups. Treatment success was similar in both groups, 97.7% in lower ASA class versus 92% in higher ASA class (p = 0.19). At 2-month follow-up, both groups had significant improvement in HREM and TBE parameters.
Conclusion
POEM is a very safe and highly effective treatment option for achalasia patients with advanced ASA class similar to lower ASA class patients. POEM may be considered as the preferred choice for myotomy in these high-risk achalasia patients due to its low morbidity and high efficacy.


Similar content being viewed by others
References
Arulampalam T, Patterson-Brown S, Morris AJ, Parker MC. Natural orifice transluminal endoscopic surgery. Ann R Coll Surg Engl. 2009;91(6):456–9. https://doi.org/10.1308/003588409X464487.
Marano L, Pallabazzer G, Solito B, et al. Surgery or peroral esophageal myotomy for Achalasia: A systematic review and meta-analysis. Med (United States). 2016;95(10):e3001.
Schlottmann F, Luckett DJ, Fine J, Shaheen NJ, Patti MG. Laparoscopic Heller Myotomy Versus Peroral Endoscopic Myotomy (POEM) for Achalasia: a systematic review and meta-analysis. Ann Surg. 2018;267(3):451–60. https://doi.org/10.1097/SLA.0000000000002311.
Hungness ES, Sternbach JM, Teitelbaum EN, Kahrilas PJ, Pandolfino JE, Soper NJ. Per-oral endoscopic myotomy (POEM) after the learning curve: durable long-term results with a low complication rate. Ann Surg. 2016;264(3):508–15. https://doi.org/10.1097/SLA.0000000000001870.
Hernández-Mondragón OV, Solórzano-Pineda OM, González-Martínez M, Blancas-Valencia JM. Gastroesophageal reflux disease after peroral endoscopic myotomy: short-term, medium-term, and long-term results. Rev Gastroenterol Mex. 2020;85(1):4–11. https://doi.org/10.1016/j.rgmx.2019.04.001.
Werner YB, Hakanson B, Martinek J, et al. Endoscopic or surgical myotomy in patients with idiopathic Achalasia. N Engl J Med. 2019;381(23):2219–29. https://doi.org/10.1056/NEJMoa1905380.
Inoue H, Shiwaku H, Iwakiri K, et al. Clinical practice guidelines for peroral endoscopic myotomy. Dig Endosc. 2018;30(5):563–79. https://doi.org/10.1111/den.13239.
Khashab MA, Vela MF, Thosani N, et al. ASGE guideline on the management of achalasia. Gastrointest Endosc. 2020;91(2):213-227.e6. https://doi.org/10.1016/j.gie.2019.04.231.
Moonesinghe SR, Mythen MG, Das P, Rowan KM, Grocott MPW. Risk stratification tools for predicting morbidity and mortality in adult patients undergoing major surgery: qualitative systematic review. Anesthesiology. 2013;119(4):959–81. https://doi.org/10.1097/ALN.0b013e3182a4e94d.
Doyle DJ, Garmon EH. American Society of Anesthesiologists Classification (ASA Class). StatPearls Publishing; 2018. http://www.ncbi.nlm.nih.gov/pubmed/28722969. Accessed 16 Mar 2020.
Prause G, Offner A, Ratzenhofer-Komenda B, Vicenzi M, Smolle J, Smolle-Jü Ttner F. Comparison of Two Preoperative Indices to Predict Perioperative Mortality in Non-Cardiac Thoracic Surgery1997; vol 11. https://academic.oup.com/ejcts/article-abstract/11/4/670/350170. Accessed 5 Apr 2020.
Vacanti CJ, VanHouten RJ, Hill RC. A statistical analysis of the relationship of physical status to postoperative mortality in 68,388 cases. Anesth Analg. 49(4):564–566. http://www.ncbi.nlm.nih.gov/pubmed/5534668. Accessed 30 Apr 2020.
Hopkins TJ, Raghunathan K, Barbeito A, et al. Associations between ASA Physical Status and postoperative mortality at 48 h: a contemporary dataset analysis compared to a historical cohort. Perioper Med. 2016. https://doi.org/10.1186/s13741-016-0054-z.
Sanaka MR, Hayat U, Thota PN, et al. Efficacy of peroral endoscopic myotomy vs other Achalasia treatments in improving esophageal function. World J Gastroenterol. 2016;22(20):4918–25. https://doi.org/10.3748/wjg.v22.i20.4918.
Doyle DJ, Garmon EH. American Society of Anesthesiologists Classification (ASA Class). StatPearls Publishing; 2018. http://www.ncbi.nlm.nih.gov/pubmed/28722969. Accessed 12 Oct 2020
Stavropoulos SN, Desilets DJ, Fuchs KH, et al. Per-oral endoscopic myotomy white paper summary. Gastrointest Endosc. 2014;80(1):1–15. https://doi.org/10.1016/j.gie.2014.04.014.
Greenleaf EK, Winder JS, Hollenbeak CS, Haluck RS, Mathew A, Pauli EM. Cost-effectiveness of per oral endoscopic myotomy relative to laparoscopic Heller myotomy for the treatment of achalasia. Surg Endosc. 2018;32(1):39–45. https://doi.org/10.1007/s00464-017-5629-3.
Li QL, Wu QN, Zhang XC, et al. Outcomes of per-oral endoscopic myotomy for treatment of esophageal achalasia with a median follow-up of 49 months. Gastrointest Endosc. 2018;87(6):1405-1412.e3. https://doi.org/10.1016/j.gie.2017.10.031.
Nabi Z, Ramchandani M, Chavan R, et al. Per-oral endoscopic myotomy for achalasia cardia: outcomes in over 400 consecutive patients. Endosc Int Open. 2017;05(05):E331–9. https://doi.org/10.1055/s-0043-105517.
Awaiz A, Yunus RM, Khan S, Memon B, Memon MA. Systematic review and meta-analysis of Perioperative Outcomes of Peroral Endoscopic Myotomy (POEM) and Laparoscopic Heller Myotomy (LHM) for Achalasia. Surg Laparosc Endosc Percutaneous Tech. 2017;27(3):123–31. https://doi.org/10.1097/SLE.0000000000000402.
Repici A, Fuccio L, Maselli R, et al. GERD after per-oral endoscopic myotomy as compared with Heller’s myotomy with fundoplication: a systematic review with meta-analysis. Gastrointest Endosc. 2018;87(4):934-943.e18. https://doi.org/10.1016/j.gie.2017.10.022.
Nabi Z, Reddy DN, Ramchandani M. Adverse events during and after per-oral endoscopic myotomy: prevention, diagnosis, and management. Gastrointest Endosc. 2018;87(1):4–17. https://doi.org/10.1016/j.gie.2017.09.029.
Hopkins J, Switzer NJ, Karmali S. Update on novel endoscopic therapies to treat gastroesophageal reflux disease: a review. World J Gastrointest Endosc. 2015;7(11):1039. https://doi.org/10.4253/wjge.v7.i11.1039.
Familiari P, Greco S, Gigante G, et al. Gastroesophageal reflux disease after peroral endoscopic myotomy: analysis of clinical, procedural and functional factors, associated with gastroesophageal reflux disease and esophagitis. Dig Endosc. 2016;28(1):33–41. https://doi.org/10.1111/den.12511.
Shiwaku H, Inoue H, Sasaki T, et al. A prospective analysis of GERD after POEM on anterior myotomy. Surg Endosc. 2016;30(6):2496–504. https://doi.org/10.1007/s00464-015-4507-0.
Sankar A, Johnson SR, Beattie WS, Tait G, Wijeysundera DN. Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br J Anaesth. 2014;113(3):424–32. https://doi.org/10.1093/bja/aeu100.
Gupta PK, Gupta H, Sundaram A, et al. Development and validation of a risk calculator for prediction of cardiac risk after surgery. Circulation. 2011;124(4):381–7. https://doi.org/10.1161/CIRCULATIONAHA.110.015701.
Han K, Kim HL, Pantuck AJ, Dorey FJ, Figlin RA, Belldegrun AS. Use of American Society of Anesthesiologists physical status classification to assess perioperative risk in patients undergoing radical nephrectomy for renal cell carcinoma. Urology. 2004;63(5):841–6. https://doi.org/10.1016/j.urology.2003.12.048 (discussion 846–7).
Skaga NO, Eken T, Søvik S, Jones JM, Steen PA. Pre-injury ASA physical status classification is an independent predictor of mortality after trauma. J Trauma. 2007;63(5):972–8. https://doi.org/10.1097/TA.0b013e31804a571c.
Vacanti CJ, VanHouten RJ, Hill RC. A statistical analysis of the relationship of physical status to postoperative mortality in 68388 cases. Anesth Analg. 1970;49(4):564–6 (Accessed 10 Apr 2020).
Wolters U, Wolf T, Stützer H, Schröder T. ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth. 1996;77(2):217–22. https://doi.org/10.1093/bja/77.2.217.
Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100(10):1043–9. https://doi.org/10.1161/01.CIR.100.10.1043.
Hungness ES, Teitelbaum EN, Santos BF, et al. Comparison of Perioperative Outcomes between Peroral Esophageal Myotomy (POEM) and Laparoscopic Heller Myotomy. J Gastrointest Surg. 2013;17(2):228–35. https://doi.org/10.1007/s11605-012-2030-3.
Zhang Y, Wang H, Chen X, et al. Per-Oral Endoscopic Myotomy versus Laparoscopic Heller Myotomy for Achalasia. Med (United States). 2016. https://doi.org/10.1097/MD.0000000000002736.
Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL. A comparative study on comprehensive, objective outcomes of laparoscopic heller myotomy with Per-Oral Endoscopic Myotomy (POEM) for achalasia. Ann Surg. 2014;259(6):1098–103. https://doi.org/10.1097/SLA.0000000000000268.
Ujiki MB, Yetasook AK, Zapf M, Linn JG, Carbray JM, Denham W. Peroral endoscopic myotomy: a short-term comparison with the standard laparoscopic approach. Surg (United States). 2013;154(4):893–900. https://doi.org/10.1016/j.surg.2013.04.042.
Khashab MA, Kumbhari V, Tieu AH, et al. Peroral endoscopic myotomy achieves similar clinical response but incurs lesser charges compared to robotic heller myotomy. Saudi J Gastroenterol. 2017;23(2):91–6. https://doi.org/10.4103/1319-3767.203360.
Boeckxstaens GE, Annese V, Des Varannes SB, et al. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med. 2011;364(19):1807–16. https://doi.org/10.1056/NEJMoa1010502.
Prakash Gyawali C, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: The Lyon Consensus. Gut. 2018;67(7):1351–62. https://doi.org/10.1136/gutjnl-2017-314722.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Madhusudhan R Sanaka, Dr. Pravallika Chadalavada, Dr. Fahrettin Covut, Dr. Rajat Garg, Dr. Prashanthi Thota, Dr. Scott Gabbard, Dr. Mohammad Alomari, Dr. Sudish Murthy, and Dr. Siva Raja have no conflicts of interest or financial ties to disclose pertinent to this article.
Ethical Statement
All procedures followed were in accordance with the ethical standards of the responsible committee on Human experimentation and with the Helsinki declaration of 1964 and later versions. This retrospective study was approved by the Institutional Board Review of Cleveland Clinic.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This manuscript has not been published and is not under consideration for publication elsewhere. However, the preliminary data was accepted in abstract form for a poster presentation at the Digestive Disease Week, DDW 2020 conference (May 2nd–5th, 2020 | Chicago, Illinois).
Rights and permissions
About this article
Cite this article
Sanaka, M.R., Chadalavada, P., Covut, F. et al. Peroral endoscopic myotomy is equally safe and highly effective treatment option in achalasia patients with both lower and higher ASA classification status. Esophagus 18, 932–940 (2021). https://doi.org/10.1007/s10388-021-00840-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-021-00840-2