Abstract
Background
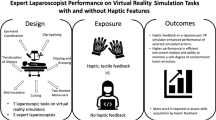
The benefits of haptic feedback in laparoscopic surgery training simulators is a topic of debate in the literature. It is hypothesized that novice surgeons may not benefit from the haptic information, especially during the initial phase of learning a new task. Therefore, provision of haptic feedback to novice trainees in the early stage of training may be distracting and detrimental to learning. A controlled experiment was conducted to examine the effect of haptic feedback on the learning curve of a complex laparoscopic suturing and knot-tying task.
Methods
The ProMIS and the MIST-VR surgical simulators were used to represent conditions with and without haptic feedback, respectively. A total of 20 novice subjects (10 per simulator) were trained to perform suturing and knot-tying and practiced the tasks in 18 sessions of 1 h each.
Results
At the end of the 3-week training period, the subjects performed equally fast but more consistently with haptics (ProMIS) than without haptics (MIST-VR). The subjects showed a slightly higher learning rate and reached the first plateau of the learning curve earlier with haptic feedback.
Conclusion
In general, learning with haptic feedback was significantly better than learning without it for a laparoscopic suturing and knot-tying task, but only during the first 5 h of training. Haptic feedback may not be warranted in laparoscopic surgical trainers. The benefits of a shorter time to the first performance plateau and more consistent initial performance should be balanced with the cost of implementing haptic feedback in surgical simulators.








Similar content being viewed by others
References
Picod G, Jambon AC, Vinatier D, Dubois P (2005) What can the operator actually feel when performing a laparoscopy? Surg Endosc 19:95–100
Perreault JO, Cao CGL (2006) Effects of vision and friction on haptic perception. Hum Factors 48:574–586
Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Anderson DK, Satava RM (2002) Virtual reality training improves operating room performance. Ann Surg 236:458–464
Sutherland LM, Middleton PF, Anthony A, Hamdorf J, Cregan P, Scott D, Maddern GJ (2006) Surgical simulation: a systematic review. Ann Surg 243:291–300
Grantcharov TP, Kristiansen VB, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P (2004) Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 91:146–150
Lathan CE, Tracey MR, Sebrechts MM, Clawson DM, Higgins GA (2002) Using virtual environments as training simulators: measuring transfer. In: Stanney KM (ed) Handbook of virtual environments: design Implementation and applications. Lawrence Erlbaum Associates, Mahwah, pp 414–434
Lamb GD (1983) Tactile discrimination of textured surfaces: psychophysical performance measurements in humans. J Physiol London 338:551–565
Lederman SJ (1981) The perception of surface roughness by active and passive touch. Bull Psychonomic Soc 18:253–255
Lederman SJ (1983) Tactual roughness perception: spatial and temporal determinants. Can J Psychol 37:498–511
Srinivasan M, LaMotte R (1996) Tactual discrimination of softness: abilities and mechanisms. In: Franzen O, Johansson R, Terenius L (eds) Somesthesis and the neurobiology of the somatosensory cortex. Birkhauser, Berlin, pp 123–136
Lederman SJ, Klatzky RL (2004) Haptic identification of common objects: effects of constraining the manual exploration process. Percept Psychophys 66:618–628
Klatzky RL, Lederman SJ, Hamilton CL, Grindley M, Swendsen RH (2003) Feeling textures through a probe: effects of probe and surface geometry and exploratory factors. Percept Psychophys 65:613–631
Brydges R, Carnahan H, Dubrowski A (2005) Surface exploration using laparoscopic surgical instruments: the perception of surface roughness. Ergonomics 48:874–894
Botden SMBI, Torab F, Buzink SN, Jakimowicz JJ (2007) The importance of haptic feedback in laparoscopic suturing training and the additive value of virtual reality simulation. Surg Endosc 22:1214–1222
Kitagawa M, Dokko D, Okamura AM, Yuh DD (2005) Effect of sensory substitution on suture manipulation forces for robotic surgical systems. J Thorac Cardiov Surg 129:151–158
Moody L, Baber C, Arvanitis TN (2002) Objective surgical performance evaluation based on haptic feedback. Stud Health Technol Inform 85:304–310
Wagner CR, Stylopoulos N, Howe RD (2002) The role of force feedback in surgery: analysis of blunt dissection. In: Proceedings of the 10th Symposium on Haptic Interfaces for Virtual Environment and Teleoperator Systsem (HAPTICS’02), pp 68–74
Strom P, Hedman L, Sarna L, Kjellin A, Wredmark T, Fellander-Tsai L (2006) Early exposure to haptic feedback enhances performance in surgical simulator training: a prospective randomized crossover study in surgical residents. Surg Endosc 20:1383–1388
Smith CD, Farrell TM, McNatt SS, Metreveli RE (2001) Assessing laparoscopic manipulative skills. Am J Surg 181:547–550
O’Connor A, Schwaitzberg SD, Cao CGL (2007) How much feedback is necessary for learning to suture? Surg Endosc 22:1614–1619
Kothari SN, Kaplan BJ, DeMaria EJ, Broderick TJ, Merrell RC (2002) Training in laparoscopic suturing skills using a new computer-based virtual reality simulator (MIST-VR) provides results comparable to those with an established pelvic trainer system. J Laparoendosc Adv Surg Tech 12:167–173
Gallagher AG, Satava RM (2002) Virtual reality as a metric for the assessment of laparoscopic psychomotor skills. Surg Endosc 16:1746–1752
Pearson AM, Gallagher AG, Rosser JC, Satava RM (2002) Evaluation of structured and quantitative training methods for teaching intracorporeal knot tying. Surg Endosc 16:130–137
Champion HR, Higgins GA (2000) Meta-analysis and planning for SIMTRAUMA: medical simulation for combat trauma. U.S. Army Medical Research and Materiel Command, Fort Detrick, MD
Cao CGL, Zhou M, Jones DB, Schwaitzberg SD (2007) Can surgeons think and operate with haptics at the same time? J Gastrointest Surg 11:1564–1569
Hassan I, Maschuw K, Rothmund M, Koller M, Gerdes B (2006) Novices in surgery are the target group of a virtual reality training laboratory. Eur Surg Res 38:109–113
Aggarwal R, Black SA, Hance JR, Darzi A, Cheshire NJW (2006) Virtual reality simulation training can improve inexperienced surgeons’ endovascular skills. Eur J Vasc Endovasc 31:588–593
Konz S, Johnson S (2000) Work design industrial ergonomics. Holcomb Hathaway, Scottsdale
Acknowledgments
This work was supported in part by a National Science Foundation Career Award (IIS-0238284) and a Society of American Gastrointestinal Endoscopic Surgeons (SAGES) Research Grant Award.
Disclosures
Dr. M. Zhou, and Ms. S. Tse, have no conflicts of interest or financial ties to disclose. Dr. A. Derevianko has consulted with Elsevier, Inc. and the Medical Education Advisory Board. Dr. D. B. Jones has consulted with Stryker Endoscopy and Olympus; has performed research with Allergan, Coviden; and has received institutional training grants from Covidien and Ethicon Endosurgery. He has no conflicts of interest with this manuscript. Dr. S. D. Schwaitzberg has consulted for MMDI, Endocore, and Olympus, and has served on the advisory committee for MITI, Stryker, Surgiquest, Cambridge Endo, Neatstitch, and Acuity Bio. He has no conflicts of interest with this manuscript. Dr. C. G. L. Cao has consulted for St. Jude Medical. She has no conflicts of interest with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhou, M., Tse, S., Derevianko, A. et al. Effect of haptic feedback in laparoscopic surgery skill acquisition. Surg Endosc 26, 1128–1134 (2012). https://doi.org/10.1007/s00464-011-2011-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-2011-8