Abstract
Cerebrovascular disease (CVD) and Alzheimer’s disease (AD) have more in common than their association with ageing. They share risk factors and overlap neuropathologically. Most patients with AD have Aβ amyloid angiopathy and degenerative changes affecting capillaries, and many have ischaemic parenchymal abnormalities. Structural vascular disease contributes to the ischaemic abnormalities in some patients with AD. However, the stereotyped progression of hypoperfusion in this disease, affecting first the precuneus and cingulate gyrus, then the frontal and temporal cortex and lastly the occipital cortex, suggests that other factors are more important, particularly in early disease. Whilst demand for oxygen and glucose falls in late disease, functional MRI, near infrared spectroscopy to measure the saturation of haemoglobin by oxygen, and biochemical analysis of myelin proteins with differential susceptibility to reduced oxygenation have all shown that the reduction in blood flow in AD is primarily a problem of inadequate blood supply, not reduced metabolic demand. Increasing evidence points to non-structural vascular dysfunction rather than structural abnormalities of vessel walls as the main cause of cerebral hypoperfusion in AD. Several mediators are probably responsible. One that is emerging as a major contributor is the vasoconstrictor endothelin-1 (EDN1). Whilst there is clearly an additive component to the clinical and pathological effects of hypoperfusion and AD, experimental and clinical observations suggest that the disease processes also interact mechanistically at a cellular level in a manner that exacerbates both. The elucidation of some of the mechanisms responsible for hypoperfusion in AD and for the interactions between CVD and AD has led to the identification of several novel therapeutic approaches that have the potential to ameliorate ischaemic damage and slow the progression of neurodegenerative disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The relationship between age-associated cerebrovascular disease (CVD) and Alzheimer’s disease (AD) is complex. They share multiple risk factors and overlap more often than not, to an extent that increases with age. Whilst there is clearly an additive component to the clinical and pathological effects of CVD and AD, increasing evidence suggests that the disease processes also interact mechanistically at a cellular level, probably in a manner that exacerbates both. However, partly because it has proven difficult to model either of these diseases accurately individually, let alone in combination, it has been difficult to determine the extent of that interaction or to establish which of the many potential mechanisms are biologically relevant.
This review covers some of the evidence of pathophysiological interaction between CVD and AD and considers possible mechanisms and therapeutic implications.
Clinical and pathological associations between CVD and AD
CVD and AD share many risk factors, including APOE ε4 [102, 141]; diabetes mellitus [139]; atrial fibrillation [38, 123]; ‘non-Mediterranean’ diet [87]; hyperhomocysteinaemia [92]; midlife hypertension, obesity and hypercholesterolaemia [30, 104, 160]; and, of course, age. The presence of vascular risk factors was reported to predict the development of AD or the conversion from mild cognitive impairment (MCI) to AD [35, 61, 90, 99]. Not all studies have found an association between vascular risk factors and AD [31, 134], and there are several potential confounders that should be considered in interpreting studies of shared risk factors or overlapping pathology, particularly as CVD and AD also overlap clinically. Concurrent ischaemic cerebrovascular disease may simply lower the threshold for clinical manifestation of AD pathology [64, 134, 143, 149]. Conversely, a history of hypertension or diabetes in patients with AD may bias clinicians towards a misdiagnosis of vascular dementia, underestimating the contribution of AD. The timing of several of the putative shared risk factors is of interest—coincident with the initial, presymptomatic deposition of Aβ in midlife (and in some studies associated with the extent of that presymptomatic deposition), rather than the maximum severity of disease as would be expected if the effects of these risk factors on CVD and AD were simply additive. Meta-analysis of data from three large-scale genome-wide association studies highlighted the involvement of cardiovascular disease-related pathways in AD [94].
Abnormalities broadly described as ‘cerebrovascular’ are common in AD. The relevant neuropathological literature was reviewed in detail by Attems and Jellinger [8]. In most cases of neuropathologically confirmed AD, post-mortem examination also reveals parenchymal vascular disease—both Aβ amyloid angiopathy and arteriolosclerotic small vessel disease (SVD) [75]. Cerebral infarcts or foci of haemorrhage can be demonstrated in over 50 % of AD brains, a figure that rises with age [46, 74, 75, 152]. Yet, other studies did not find any relationship between the burden of ischaemic vascular pathology and AD [31, 143].
Some studies suggest that AD is also associated with extracerebral atherosclerotic disease [65]. AD was associated with coronary artery disease in one study [151] but two other studies found no relationship between the severity of coronary artery disease and the Aβ plaque load [37, 86].
In several large post-mortem cohorts, AD was associated with atherosclerosis of the Circle of Willis [13, 67, 135, 172]. The age- and sex-adjusted severity of the atherosclerosis correlated with neuritic plaque [13, 67, 135, 172], tangle [13, 135, 172] and CAA severity scores [172], independent of APOE genotype [13, 172]. In contrast, there was no relationship between severity of the atherosclerosis and AD pathology in a series of elderly Japanese [73] or in the Baltimore Longitudinal Study of Aging cohort [37]. The explanation for the discrepant finding between these studies is not clear.
Two recent biomarker studies provided additional evidence of an association between CVD and AD. Hughes et al. [69] looked at the relationship between pulse wave velocity (an indicator of artery wall stiffness) and cerebral accumulation of Aβ over 2 years, as measured by positron emission tomography with Pittsburgh compound B, in 82 non-demented people aged 83 years or older. The authors found a significant relationship between vascular stiffness in larger central arteries (as indicated by carotid-femoral and heart-femoral pulse wave velocity) and cerebral Aβ accumulation over the two-year period. In another study, Kester et al. [83] analysed brain magnetic resonance imaging (MRI) findings and cerebrospinal fluid (CSF) tau and Aβ levels in 914 consecutive participants in the Amsterdam Dementia Cohort. The cohort included 30 people with a clinical diagnosis of vascular dementia, and 337 who had subjective memory complaints but were normal on cognitive testing. In both groups, white matter hyperintensities were associated with reduced Aβ42 in the CSF, as in AD. Microbleeds were associated with lower CSF Aβ42 in the vascular dementia group and higher CSF tau in the participants with subjective memory complaints. The associations were largely attributable to the APOE ϵ4 carriers in these groups.
Structural disease of cerebral blood vessels in ageing in AD
Most patients with AD have Aβ amyloid angiopathy. Arteriolar Aβ amyloid angiopathy is demonstrable post-mortem in over 90 % of patients with AD compared with about 30 % of elderly controls [27, 44, 50, 95, 98, 101, 161, 162, 171]. The angiopathy predominantly affects the cerebral leptomeninges and cortex but sometimes also the cerebellum and, very occasionally, the brain stem. It tends to be more severe in AD than controls, particularly in APOE ϵ4-positive patients [27, 52, 131, 142]. In controls, arteriolar Aβ amyloid angiopathy is more strongly associated with APOE ϵ2 [95].
Accumulation of Aβ amyloid in cerebral arterioles may be accompanied by its accumulation in capillaries, a finding strongly associated with APOE ϵ4 and usually also with AD [1, 7, 95, 157]. In a series of 51 AD cases and 14 controls assessed independently by neuropathologists in three different centres, capillary amyloid angiopathy was detected in 35–45 % of the AD cases, predominantly in the occipital lobe, but in only a single control brain [95].
It is unclear whether or not patients with AD are more likely to have (non-amyloid) SVD. Numerous imaging and pathological studies have reported an increased prevalence of ‘small vessel disease’ in AD but most have conflated parenchymal ischaemic lesions—particularly in the white matter—with structural disease of cerebral blood vessels. APOE genotype influences the likelihood of ischaemic changes in AD. Morgen et al. [109] found that AD carriers of the APOE ϵ4 allele had a significantly greater volume of white matter hyperintensities than did non-carriers.
Whilst it is possible that many of the ischaemic lesions in patients with AD are attributable to cerebral SVD, some may have resulted from amyloid angiopathy or basal artery atherosclerosis, and a range of extracranial processes may also have contributed, including atherothrombotic or cholesterol emboli from carotid or aortic plaques, orthostatic hypotension [9, 81, 82, 150], cardiac valvular disease and cardiac arrhythmias [153], particularly atrial fibrillation [38, 123]. To try to address this, some of the studies excluded or adjusted for cardiovascular risk factors [140] but there remains a paucity of direct evidence linking SVD and AD, or indeed linking SVD and white matter lesions in AD: a post-mortem study of 125 cases of AD did not find any association between several objective measures of white matter damage (extent of immunolabelling for glial fibrillary acidic protein, axonal accumulation of Aβ precursor protein, axon density in superficial and deep white matter, intensity of staining for myelin) and severity of basal artery atherosclerosis, cerebral arteriolosclerosis or Aβ amyloid angiopathy, or APOE genotype [26].
Indirect evidence that SVD is more marked in AD comes from functional MRI analysis of regional cerebrovascular resistance (CVRi). In a study of CVRi in 12 patients with AD, 23 with MCI and 46 normal elderly controls, Nation et al. [114] found that cerebrovascular resistance was increased in several regions in AD and, to a lesser extent, in MCI. The increase was most marked in the thalamus and caudate nucleus, regions that are spared in Aβ amyloid angiopathy but have a predilection for SVD. Limitations of the study included the small cohort size and the use of non-contemporaneous measurements of peripheral rather than central blood pressure to calculate the CVRi, and in the absence of neuropathological confirmation the precise substrate of the increase in vascular resistance remains a matter of speculation.
Several studies have reported that the degeneration of cerebral capillaries in AD exceeds that in age-matched controls [10, 25, 70, 144]. The degeneration affects both endothelial cells and pericytes and leads eventually to an increase in the number of ‘string’ vessels consisting solely of tubes of collagen. This is not accompanied by a compensatory increase in the formation of new capillaries [11, 70, 158]. The degeneration of pericytes and endothelial cells is probably interrelated.
CVD exacerbates neurological dysfunction and brain damage in AD
The most obvious impact of CVD is on cerebral perfusion. There is a substantial literature documenting the association of Aβ amyloid angiopathy and SVD with infarcts (Fig. 1) and other ischaemic abnormalities [21, 23, 32, 33, 43, 45, 121, 122, 133, 134, 136, 161]. The mechanisms include susceptibility to thrombosis [21, 97], permanent reduction in blood flow as a result of reduced calibre of more severely affected blood vessels, and impaired modulation of the calibre in response to haemodynamic stress and alteration in metabolic demand.
Infarction associated with Aβ amyloid angiopathy. a Microinfarct in cerebral cortex. The lesion is rarefied and gliotic, and includes a few macrophages. b Aβ immunohistochemistry on an adjacent section revealed moderately severe Aβ amyloid angiopathy. Note the circumferential deposition of Aβ in a sulcal arteriole overlying the microinfarct. Bar 250 μm
Patients with AD have impaired autoregulation (i.e. reduced ability to maintain cerebral perfusion when perfusion pressure changes, usually as a result of hypotension) and reduced vasomotor reactivity to hypercapnia [36]. Patients with probable Aβ amyloid angiopathy (diagnosed according to the Boston criteria [84]) also show neurovascular decoupling, as evidenced by impaired functional hyperaemia [39, 130] (i.e. a reduced regional increase in blood flow in response to increased local metabolic demand). Similar abnormalities in regulation of cerebral blood flow were demonstrated in mouse models of cerebral Aβ accumulation [71, 117] and Aβ amyloid angiopathy [129, 147]. In patients with Aβ amyloid angiopathy, reduced primary visual cortex fMRI responsiveness to a visual task correlated with the volume of white matter hyperintensities, an indicator of the severity of white matter ischaemia [130].
In a series of studies of human brain tissue and animal models, Weller, Carare, Hawkes and colleagues showed that interstitial fluid drains from the brain along perivascular spaces and basement membranes [164, 174], and that Aβ within the interstitial fluid tends to precipitate within the perivascular basement membranes [165, 166]. Further evidence that Aβ amyloid angiopathy reflected the precipitation of Aβ from the interstitial fluid came from the finding of Jucker and colleagues that neuron-specific overexpression of Aβ precursor protein caused the development of Aβ amyloid angiopathy in APP23 mice [22, 63]. Vascular deposition of Aβ is increased by possession of APOE ϵ4 [27]; this is probably partly related to elevation of the ratio Aβ40:42 [48, 63] and partly to alterations in the composition of the perivascular basement membranes [60]. Vascular deposition of Aβ is also increased if drainage is impeded by Aβ amyloid angiopathy or by age-related changes to the perivascular basement membranes [58, 59, 76, 166]. The full range of downstream effects of impeded drainage of solutes in Aβ amyloid angiopathy remains to be determined. One probable consequence is an increase in the phosphorylation of tau, as evidenced by the more abundant neurofibrillary pathology around Aβ-laden than non-Aβ-laden parenchymal arterioles in AD (Fig. 2) [169]. A similar increase in neurofibrillary pathology was demonstrated adjacent to parenchymal arterioles in the amyloid angiopathy of familial British dementia, in which there is vascular deposition of ABri [66], which, like vascular Aβ, probably impedes the drainage of interstitial fluid.
Other ways in which AD-associated structural vascular disease exacerbates neurological dysfunction and brain damage include increased susceptibility to haemorrhage and, possibly, impaired blood–brain barrier (BBB) function. Carrano et al. [24] noted the loss of several components of endothelial tight junctions in Aβ-laden capillaries in post-mortem brain tissue from patients with Aβ amyloid angiopathy, and similar findings were documented in several in vitro and ex vivo experimental studies, in which exposure of endothelial cells to Aβ40 or Aβ42 caused loss or mislocation of tight junction proteins [57, 85, 100, 154]. Hartz et al. [57] reported that 2 of 19 patients who fulfilled clinical criteria for probable Aβ amyloid angiopathy had MRI evidence of BBB leakage and posterior reversible encephalopathy syndrome.
Degeneration of pericytes probably contributes to the impairment of BBB function in AD. In mice pericytes were shown to be needed for maintenance of the blood–brain barrier and capillary perfusion [3, 14]. Sengillo et al. [144] found the loss of pericytes in cerebral cortex and hippocampus from AD patients to correlate with the extent of disruption of the blood–brain barrier, as demonstrated by extravasation of immunoglobulin G and perivascular deposition of fibrin. In contrast, a study of a range of mouse models of AD did not find increased permeability of the BB to antibodies [17].
Numerous studies have documented that patients with Aβ amyloid angiopathy are prone to cerebral haemorrhage, particularly lobar haemorrhage and cortical microhaemorrhage (Fig. 3) [43, 50, 51, 97, 111, 115, 131, 161, 171]. Both the ε2 and ε4 alleles of APOE increase the risk of Aβ amyloid angiopathy-associated lobar haemorrhage [52, 53, 116]; ε4 may do so by promoting the accumulation of Aβ in the walls of arterioles, and ε2 by promoting the development of vasculopathic changes, particularly fibrinoid necrosis, in the amyloid-laden vessels [54, 103]. Patients with Aβ amyloid angiopathy are also prone to develop superficial cortical siderosis [29, 93].
Cerebral hypoperfusion is an early feature of AD
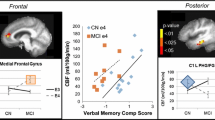
Cerebral hypoperfusion is demonstrable several years before the onset of clinical AD. Imaging studies in people with MCI [6, 18, 34], healthy carriers of the APOE ϵ4 allele [89] and those with gene mutations known to cause autosomal dominant AD [15] have shown that the distribution and spread of the hypoperfusion are highly stereotyped, and mirror the accumulation of Aβ amyloid within the brain parenchyma, particularly during the preclinical phases of disease. The first affected region is the precuneus, about 10 years before the development of dementia (Fig. 4). From there the hypoperfusion spreads to involve the cingulate gyrus and the lateral part of the parietal lobe, then the frontal and temporal lobes and eventually most of the cerebrum.
Stereotyped pattern of spread of hypoperfusion in AD. The arrows in this diagram indicate the progression of hypoperfusion, starting from the precuneus, well before the onset of dementia, and spreading to the rest of the parietal cortex and the cingulate gyrus, then the frontal and temporal cortex, largely sparing the occipital cortex until late disease
At least in preclinical early AD, the primary abnormality is one of inadequate blood supply, not reduced metabolic demand, in that the reduction in oxygenation is not commensurate with the decline in blood flow. Several fMRI studies have found that the regional oxygen extraction fraction (rOEF) is significantly elevated in AD, particularly in the parietal cortex [112, 113, 159], and Tarumi et al. [156] found the tissue oxygenation index (TOI, a measure of the saturation of haemoglobin by oxygen, determined by near infrared spectroscopy) to be significantly increased in the cortex in people with amnestic MCI. Were the decline in blood flow to be a response to decreased metabolic demand, the rOEF would be reduced and the TOI increased.
We recently developed a post-mortem biochemical method to study hypoperfusion in brain tissue [11, 12, 96]. The method is based on the differential susceptibility of different myelin proteins to ischaemia. The myelin proteins are synthesised in the oligodendrocyte cell body and require energy-dependent transport to reach their sites of insertion into the myelin sheath. Myelin-associated glycoprotein (MAG) is one of the myelin proteins inserted furthest away from the cell body, in the adaxonal loop of myelin, the first part of the sheath to degenerate when blood supply is insufficient to meet the energy demands of the oligodendrocyte. Measurement of the ratio of MAG to another myelin protein such as proteolipid protein-1 (PLP1), present throughout the myelin sheath, indicates the extent to which the blood supply meets the energy requirements of the oligodendrocyte (Fig. 5).
Schematic illustration of the distribution of MAG (Pink dots) and PLP1 (Green dots) in the myelin sheath. When the supply of oxygen and glucose is insufficient to meet the metabolic needs of the oligodendrocyte, as occurs in hypoperfusion, the first part of the cell to degenerate is the adaxonal loop of myelin—the part of the oligodendrocyte that is furthest away from the cell body (so-called dying-back oligodendrogliopathy). Because MAG is restricted to the adaxonal loop of myelin whereas PLP1 is widely distributed throughout the myelin sheath, hypoperfusion leads to greater loss of MAG than PLP1. In contrast, degeneration of nerve fibres causes loss of both MAG and PLP1. The severity of ante-mortem hypoperfusion can be assessed by measuring the MAG:PLP1 ratio
In the deep parietal white matter in an elderly cohort that included AD, VaD and cognitively normal cases, MAG:PLP1 showed a highly significant negative correlation with severity of SVD and a highly significant positive correlations with the concentration of the vasoconstrictor endothelin-1 (EDN1) and with the concentration of vascular endothelial growth factor (VEGF) [11, 12]. These biochemical relationships were confirmed in deep frontal white matter in an Oxford cohort that had excluded brains with more than mild AD or Lewy body pathology [12]. Our interpretation was that as SVD severity increased, EDN1 production had been downregulated and VEGF production upregulated in response to the reduced tissue oxygenation.
Having established the utility of this post-mortem biochemical assessment of ante-mortem oxygenation of brain tissue, we examined mid-frontal cortex from AD and control brains, to determine whether there was evidence that any reduction in perfusion exceeded the decline in metabolic demand, and to try to identify possible mediators of hypoperfusion [158]. Our findings confirmed that perfusion was indeed pathologically reduced in AD. More recently, we examined precuneus, the region first affected by hypoperfusion in AD [106]. MAG:PLP1 in this region was reduced ~50 % in early AD (Braak stage III–IV). Although MAG:PLP1 in the precuneus remained low in advanced AD (stage V–VI), the reduction was less pronounced, possibly reflecting falling oxygen demand.
The main cause of cerebral hypoperfusion in AD is probably non-structural vascular dysfunction rather than structural pathology
Although structural disease of blood vessels contributes to cerebral hypoperfusion in at least some patients with AD, we did not find Aβ amyloid angiopathy, SVD or reduced microvessel density to contribute significantly to the reduction in MAG:PLP1 in the frontal cortex, medial parietal cortex or parietal white matter in most cases [11, 106, 158]. It is of note that the consistent distribution of hypoperfusion in early AD, involving the precuneus and, to a lesser extent, the cingulate gyrus, is not in a watershed region, as might be expected if postural hypotension or basal atheroma were responsible. If SVD were the explanation, the hypoperfusion would be more likely to involve the deep white matter and basal ganglia. Lastly, the distribution of Aβ amyloid angiopathy is quite variable but it tends to be most severe in the occipital region, which is affected by hypoperfusion only in the late stages of AD.
There is a range of potential non-structural substrates of hypoperfusion in AD, several of which involve pathways that are strongly influenced by Aβ. Elevated Aβ was previously shown to cause vasoconstriction, reduce cerebral perfusion and prevent functional hyperaemia and autoregulation in mice transgenic for mutant human APP [71, 117, 118, 129]; to increase expression of endothelin-converting enzyme-1 and -2 (ECE1 and ECE2) by human cerebrovascular endothelial cells and neuroblastoma cells, respectively, leading to elevated EDN1 production [126–128]; to inhibit endothelial nitric oxide synthase activity [49, 88], reducing endothelial production of the vasodilator nitric oxide; and to increase the neuronal expression and activity of angiotensin-converting enzyme (ACE) [107], which catalyses the production of the vasoconstrictor angiotensin II (AngII). Support for the pathogenic relevance of several of these experimental observations comes from the demonstration of elevated EDN1 level and ACE activity in post-mortem temporal and frontal cortex from patients with AD [105, 127, 158]. Aβ is a substrate of ECE1 and ECE2 [40–42, 124] and also of ACE [62, 68, 120], and it seems possible that the upregulation of production of EDN1 and AngII may be a side effect of over-activation of these enzyme systems by the accumulation of substrate.
More recently, we looked at MAG:PLP1, SVD, Aβ amyloid angiopathy, EDN1 level, ACE level and activity, and AngII level in precuneus from post-mortem human brains showing a spectrum of severity of AD (as indicated by Braak tangle stage). We showed that MAG:PLP1 declined in the precuneus even in early AD (i.e. in Braak stage III–IV disease) (Fig. 6). Indeed, despite progressive elevation in EDN1 concentration with disease progression, the MAG:PLP1 ratio was lower in early than in late AD (Fig. 7), presumably reflecting falling metabolic demand with increasing synaptic and neuronal damage. In the precuneus, unlike in the frontal cortex in advanced AD, we did not find elevation of ACE or AngII.
Oxygenation of the precuneus is reduced in early Alzheimer’s disease. a Bar chart showing a reduction in the ratio of myelin glycoprotein (MAG) to proteolipid-1 protein (PLP-1) (MAG:PLP1) in the precuneus in AD. The bars indicate the mean and SEM. b Bar chart showing marked variation in MAG:PLP1 (P = 0.027) with disease stage. For this analysis, control and AD cases were combined and grouped according to Braak tangle stage (0–II, III–IV and V–VI). Post hoc analysis revealed that MAG:PLP1 was significantly reduced in early AD (Braak stage III–IV) compared to controls (P = 0.027). c Bar chart showing elevated vascular endothelial growth factor (VEGF), an independent marker of cerebral perfusion, in AD. d Scatterplot showing the highly significant negative correlation between MAG:PLP1 and VEGF concentration in the precuneus (r = −0.40, P = 0.0007). The best-fit linear regression line and 95 % confidence interval are superimposed. **P < 0.001, ***P < 0.0001. Reproduced with permission from [106]
Reduced oxygenation of the precuneus in AD is associated with elevated endothelin-1 (EDN1). a Bar chart showing significantly increased EDN1 in AD within the precuneus. b Bar chart showing increased EDN1 levels in relation to disease severity when control and AD cases were subdivided according to Braak tangle stage (0–II, III–IV and V–VI) irrespective of the presence or absence of a history of dementia. Scatterplots showing the inverse correlation between EDN1 concentration and MAG:PLP1 ratio (r = −0.31) (c), and the positive correlation between EDN1 and VEGF (r = 0.29) (d). *P < 0.05, ***P < 0.001, ****P < 0.0001. Reproduced with permission from [106]
EDN1 in the cortex correlated highly significantly with the levels of both soluble and insoluble Aβ42, which we showed previously to upregulate neuronal ECE2 [126], but not with Aβ40, which we found to upregulate endothelial ECE1 [127]. The findings suggest that reduced oxygenation of the precuneus in early AD is likely to result, at least in part, from Aβ42-mediated upregulation of ECE2.
MAG:PLP1 was also reduced in the parietal white matter in AD but here the decline correlated positively with the level of EDN1, in keeping with a protective vasodilatory response to reduced oxygenation. However, the decline of MAG:PLP1 in the white matter was associated with increasing EDN1 in the overlying cortex, perhaps reflecting EDN1-mediated vasoconstriction of perforating arterioles, which traverse the cortex to perfuse the white matter.
Although the main focus of studies of functional rather than structural vascular abnormalities has been on changes in arteriolar calibre, biochemical alterations in AD may also affect vascular permeability. In particular, several lines of evidence indicate that Aβ upregulates the plasma kallikrein-kinin system, leading to the production of bradykinin, which causes dilatation and increased permeability of venules and, at higher concentration, dilatation of arterioles as well [2]. The activating enzyme, plasma kallikrein, circulates as an inactive zymogen and is activated through a cleavage process involving Factor XIIa. Active plasma kallikrein cleaves its major substrate, high molecular weight kininogen (HK) to liberate bradykinin and activated HK. Aβ was shown to stimulate the production of bradykinin by endothelial cells [16, 146, 170]. Cerebroventricular infusion of Aβ40 in rats caused a 10-fold increase of bradykinin in the CSF and accumulation of degradation fragments of bradykinin in brain tissue [72]. Ashby et al. [5] demonstrated that plasma kallikrein mRNA was significantly increased in the frontal cortex in AD, and plasma kallikrein activity was significantly increased in the frontal and temporal cortex in AD.
Cerebral hypoperfusion probably accelerates the progression of AD
As noted above, ischaemic brain damage is common in AD and in many cases contributes to the cognitive impairment. Ischaemia may also contribute to the progression of AD itself. Ischaemia in animal models, or its in vitro stimulation, is associated with increased production of Aβ42 (for reviews see [31, 96]). Acute cerebral ischaemia or hypoxia caused overexpression of APP mRNA [145], upregulation of BACE1 mRNA and protein, increased β-secretase activity and the production of Aβ peptide [55, 91, 167, 175]. BACE1 and Aβ (but not APP) level were also elevated in a chronic hypoperfusion model [176]. Transient ischaemia increased PSEN1 mRNA in the gerbil hippocampus [155] and repeated episodes of hypoxia enhanced β-secretase-mediated cleavage of APP, and the level of APH-1a, another component of γ-secretase complex [91]. In other in vitro studies, hypoxia and/or oxidative modification reduced the activity of the Aβ-degrading enzymes neprilysin and insulin-degrading enzyme [47, 148, 163]. Lastly, transient cerebral ischaemia caused hyperphosphorylation of tau in cortical neurons [168].
Although most evidence that cerebral hypoperfusion may accelerate the progression of AD comes from in vitro and animal studies, some clinical observations support this possibility. In several clinical studies of cerebral blood flow and glucose utilisation in patients with a clinical diagnosis of AD or MCI, hypoperfusion predicted the development or rate of cognitive decline [19, 20, 28]. Patients who survived transient cerebral hypoperfusion as a result of cardiac arrest had elevated serum Aβ42 over several days [173]. And whilst that might be explained by non-specific ‘leakage’ of Aβ42 from damaged brain tissue, the same explanation could not be applied to the sustained elevation of serum Aβ42 in a study of patients with diffuse TBI with brain swelling and presumably at least some hypoperfusion, as they showed a concomitant reduction of Aβ42 in the CSF [108].
Implications for therapy
The identification of functionally important non-structural abnormalities of the cerebral vasculature in ageing and dementia, particularly in AD, raises the prospect that pharmacotherapy targeting the relevant biochemical pathways might slow the progression of dementia, by improving cerebral perfusion and reducing permeability of the BBB. An obvious potential target is the endothelin system, for which there are already several well-tolerated antagonists. Bosentan, a non-selective endothelin receptor (EDNR) antagonist [138], has been licenced since 2001 for the treatment of pulmonary hypertension, another disease in which there is upregulation of ECEs and increased production of EDN1 [132, 137]. Bosentan produces significant, clinically useful, sustained improvement in pulmonary blood flow and exercise tolerance in patients with pulmonary hypertension. Bosentan was also shown to prevent the attenuation of endothelium-dependent aortic and carotid vasodilatation that is seen in Tg2576 mice (which overexpress a mutant form of APP bearing the Swedish double mutation). However, EDN1 is thought to act on EDNRA receptors (the predominant EDN1 receptor type in cerebral vessels) to reduce CBF in AD, and there are selective EDNRA receptor antagonists such as zibotentan [56, 110] which offer potential advantages over non-selective EDNR antagonists [125]. Other targets might include the plasma kallikrein-kinin [5] and renin-angiotensin systems [78]. The therapeutic potential of inhibiting the renin-angiotensin system in AD is attracting a great deal of interest and clinical investigation [4, 77, 79, 80, 119].
References
Allen N, Robinson AC, Snowden J, Davidson YS, Mann DM (2014) Patterns of cerebral amyloid angiopathy define histopathological phenotypes in Alzheimer’s disease. Neuropathol Appl Neurobiol 40:136–148. doi:10.1111/nan.12070
Altura BM, Hershey SG, Altura BT (1970) Microcirculatory actions of polypeptides and their use in the treatment of experimental shock. In: Sicuteri F, Rocha e Silva M, Back N (eds) Bradykinin and related kinins: cardiovascular, biochemical, and neural actions. Plenum Press, New York, pp 239–248
Armulik A, Genove G, Mae M, Nisancioglu MH, Wallgard E, Niaudet C, He L, Norlin J, Lindblom P, Strittmatter K et al (2010) Pericytes regulate the blood–brain barrier. Nature 468:557–561. doi:10.1038/nature09522
Ashby EL, Kehoe PG (2013) Current status of renin-aldosterone angiotensin system-targeting anti-hypertensive drugs as therapeutic options for Alzheimer’s disease. Expert Opin Investig Drugs 22:1229–1242. doi:10.1517/13543784.2013.812631
Ashby EL, Love S, Kehoe PG (2012) Assessment of activation of the plasma kallikrein–kinin system in frontal and temporal cortex in Alzheimer’s disease and vascular dementia. Neurobiol Aging 33:1345–1355. doi:10.1016/j.neurobiolaging.2010.09.024
Asllani I, Habeck C, Scarmeas N, Borogovac A, Brown TR, Stern Y (2008) Multivariate and univariate analysis of continuous arterial spin labeling perfusion MRI in Alzheimer’s disease. J Cereb Blood Flow Metab 28:725–736. doi:10.1038/sj.jcbfm.9600570
Attems J, Jellinger KA (2004) Only cerebral capillary amyloid angiopathy correlates with Alzheimer pathology—a pilot study. Acta Neuropathol 107:83–90. doi:10.1007/s00401-003-0796-9
Attems J, Jellinger KA (2014) The overlap between vascular disease and Alzheimer’s disease—lessons from pathology. BMC Med 12:206. doi:10.1186/s12916-014-0206-2
Ballard C, Shaw F, McKeith I, Kenny R (1998) High prevalence of neurovascular instability in neurodegenerative dementias. Neurology 51:1760–1762
Baloyannis SJ, Baloyannis IS (2012) The vascular factor in Alzheimer’s disease: a study in Golgi technique and electron microscopy. J Neurol Sci 322:117–121. doi:10.1016/j.jns.2012.07.010
Barker R, Ashby EL, Wellington D, Barrow VM, Palmer JC, Kehoe PG, Esiri MM, Love S (2014) Pathophysiology of white matter perfusion in Alzheimer’s disease and vascular dementia. Brain 137:1524–1532. doi:10.1093/brain/awu040
Barker R, Wellington D, Esiri MM, Love S (2013) Assessing white matter ischemic damage in dementia patients by measurement of myelin proteins. J Cereb Blood Flow Metab 33:1050–1057. doi:10.1038/jcbfm.2013.46
Beach TG, Wilson JR, Sue LI, Newell A, Poston M, Cisneros R, Pandya Y, Esh C, Connor DJ, Sabbagh M et al (2007) Circle of Willis atherosclerosis: association with Alzheimer’s disease, neuritic plaques and neurofibrillary tangles. Acta Neuropathol 113:13–21. doi:10.1007/s00401-006-0136-y
Bell RD, Winkler EA, Sagare AP, Singh I, LaRue B, Deane R, Zlokovic BV (2010) Pericytes control key neurovascular functions and neuronal phenotype in the adult brain and during brain aging. Neuron 68:409–427. doi:10.1016/j.neuron.2010.09.043
Benzinger TL, Blazey T, Jack CR Jr, Koeppe RA, Su Y, Xiong C, Raichle ME, Snyder AZ, Ances BM, Bateman RJ et al (2013) Regional variability of imaging biomarkers in autosomal dominant Alzheimer’s disease. Proc Natl Acad Sci USA 110:E4502–E4509. doi:10.1073/pnas.1317918110
Bergamaschini L, Donarini C, Foddi C, Gobbo G, Parnetti L, Agostoni A (2001) The region 1-11 of Alzheimer amyloid-β is critical for activation of contact-kinin system. Neurobiol Aging 22:63–69
Bien-Ly N, Boswell CA, Jeet S, Beach TG, Hoyte K, Luk W, Shihadeh V, Ulufatu S, Foreman O, Lu Y et al (2015) Lack of widespread BBB disruption in Alzheimer’s disease models: focus on therapeutic antibodies. Neuron 88:289–297. doi:10.1016/j.neuron.2015.09.036
Binnewijzend MA, Kuijer JP, Benedictus MR, van der Flier WM, Wink AM, Wattjes MP, van Berckel BN, Scheltens P, Barkhof F (2013) Cerebral blood flow measured with 3D pseudocontinuous arterial spin-labeling MR imaging in Alzheimer disease and mild cognitive impairment: a marker for disease severity. Radiology 267:221–230. doi:10.1148/radiol.12120928
Borroni B, Perani D, Broli M, Colciaghi F, Garibotto V, Paghera B, Agosti C, Giubbini R, Di Luca M, Padovani A (2005) Pre-clinical diagnosis of Alzheimer disease combining platelet amyloid precursor protein ratio and rCBF spect analysis. J Neurol 252:1359–1362. doi:10.1007/s00415-005-0867-z
Brown DR, Hunter R, Wyper DJ, Patterson J, Kelly RC, Montaldi D, McCullouch J (1996) Longitudinal changes in cognitive function and regional cerebral function in Alzheimer’s disease: a SPECT blood flow study. J Psychiatr Res 30:109–126
Cadavid D, Mena H, Koeller K, Frommelt RA (2000) Cerebral β amyloid angiopathy is a risk factor for cerebral ischemic infarction. A case control study in human brain biopsies. J Neuropathol Exp Neurol 59:768–773
Calhoun ME, Burgermeister P, Phinney AL, Stalder M, Tolnay M, Wiederhold KH, Abramowski D, Sturchler-Pierrat C, Sommer B, Staufenbiel M et al (1999) Neuronal overexpression of mutant amyloid precursor protein results in prominent deposition of cerebrovascular amyloid. Proc Natl Acad Sci USA 96:14088–14093
Caplan LR (2015) Lacunar infarction and small vessel disease: pathology and pathophysiology. J Stroke 17:2–6. doi:10.5853/jos.2015.17.1.2
Carrano A, Hoozemans JJ, van der Vies SM, Rozemuller AJ, van Horssen J, de Vries HE (2011) Amyloid β induces oxidative stress-mediated blood-brain barrier changes in capillary amyloid angiopathy. Antioxid Redox Signal 15:1167–1178. doi:10.1089/ars.2011.3895
Challa VR, Thore CR, Moody DM, Anstrom JA, Brown WR (2004) Increase of white matter string vessels in Alzheimer’s disease. J Alzheimers Dis 6:379–383 (discussion 443–379)
Chalmers K, Wilcock G, Love S (2005) Contributors to white matter damage in the frontal lobe in Alzheimer’s disease. Neuropathol Appl Neurobiol 31:623–631. doi:10.1111/j.1365-2990.2005.00678.x
Chalmers K, Wilcock GK, Love S (2003) APOE ϵ4 influences the pathological phenotype of Alzheimer’s disease by favouring cerebrovascular over parenchymal accumulation of Aβ protein. Neuropathol Appl Neurobiol 29:231–238
Chao LL, Buckley ST, Kornak J, Schuff N, Madison C, Yaffe K, Miller BL, Kramer JH, Weiner MW (2010) ASL perfusion MRI predicts cognitive decline and conversion from MCI to dementia. Alzheimer Dis Assoc Disord 24:19–27. doi:10.1097/WAD.0b013e3181b4f736
Charidimou A, Linn J, Vernooij MW, Opherk C, Akoudad S, Baron JC, Greenberg SM, Jager HR, Werring DJ (2015) Cortical superficial siderosis: detection and clinical significance in cerebral amyloid angiopathy and related conditions. Brain 138:2126–2139. doi:10.1093/brain/awv162
Chuang YF, An Y, Bilgel M, Wong DF, Troncoso JC, O’Brien RJ, Breitner JC, Ferruci L, Resnick SM, Thambisetty M (2015) Midlife adiposity predicts earlier onset of Alzheimer’s dementia, neuropathology and presymptomatic cerebral amyloid accumulation. Mol Psychiatry: doi:10.1038/mp.2015.129
Chui HC, Zheng L, Reed BR, Vinters HV, Mack WJ (2012) Vascular risk factors and Alzheimer’s disease: are these risk factors for plaques and tangles or for concomitant vascular pathology that increases the likelihood of dementia? An evidence-based review. Alzheimers Res Ther 4:1. doi:10.1186/alzrt98
Chung YA, JH O, Kim JY, Kim KJ, Ahn KJ (2009) Hypoperfusion and ischemia in cerebral amyloid angiopathy documented by 99mTc-ECD brain perfusion SPECT. J Nucl Med 50:1969–1974. doi:10.2967/jnumed.109.062315
Conijn MM, Kloppenborg RP, Algra A, Mali WP, Kappelle LJ, Vincken KL, van der Graaf Y, Geerlings MI, SMART Study Group (2011) Cerebral small vessel disease and risk of death, ischemic stroke, and cardiac complications in patients with atherosclerotic disease: the Second Manifestations of ARTerial disease-Magnetic Resonance (SMART-MR) study. Stroke 42:3105–3109. doi:10.1161/STROKEAHA.110.594853
Dai W, Lopez OL, Carmichael OT, Becker JT, Kuller LH, Gach HM (2009) Mild cognitive impairment and alzheimer disease: patterns of altered cerebral blood flow at MR imaging. Radiology 250:856–866. doi:10.1148/radiol.2503080751
de Bruijn RF, Ikram MA (2014) Cardiovascular risk factors and future risk of Alzheimer’s disease. BMC Med 12:130. doi:10.1186/s12916-014-0130-5
den Abeelen AS, Lagro J, van Beek AH, Claassen JA (2014) Impaired cerebral autoregulation and vasomotor reactivity in sporadic Alzheimer’s disease. Curr Alzheimer Res 11:11–17
Dolan H, Crain B, Troncoso J, Resnick SM, Zonderman AB, Obrien RJ (2010) Atherosclerosis, dementia, and Alzheimer disease in the Baltimore Longitudinal Study of Aging cohort. Ann Neurol 68:231–240. doi:10.1002/ana.22055
Dublin S, Anderson ML, Haneuse SJ, Heckbert SR, Crane PK, Breitner JC, McCormick W, Bowen JD, Teri L, McCurry SM et al (2011) Atrial fibrillation and risk of dementia: a prospective cohort study. J Am Geriatr Soc 59:1369–1375. doi:10.1111/j.1532-5415.2011.03508.x
Dumas A, Dierksen GA, Gurol ME, Halpin A, Martinez-Ramirez S, Schwab K, Rosand J, Viswanathan A, Salat DH, Polimeni JR et al (2012) Functional magnetic resonance imaging detection of vascular reactivity in cerebral amyloid angiopathy. Ann Neurol 72:76–81. doi:10.1002/ana.23566
Eckman EA, Adams SK, Troendle FJ, Stodola BA, Kahn MA, Fauq AH, Xiao HD, Bernstein KE, Eckman CB (2006) Regulation of steady-state β-amyloid levels in the brain by neprilysin and endothelin-converting enzyme but not angiotensin-converting enzyme. J Biol Chem 281:30471–30478. doi:10.1074/jbc.M605827200
Eckman EA, Reed DK, Eckman CB (2001) Degradation of the Alzheimer’s amyloid β peptide by endothelin-converting enzyme. J Biol Chem 276:24540–24548. doi:10.1074/jbc.M007579200
Eckman EA, Watson M, Marlow L, Sambamurti K, Eckman CB (2003) Alzheimer’s disease β-amyloid peptide is increased in mice deficient in endothelin-converting enzyme. J Biol Chem 278:2081–2084. doi:10.1074/jbc.C200642200
Ellis RJ, Olichney JM, Thal LJ, Mirra SS, Morris JC, Beekly D, Heyman A (1996) Cerebral amyloid angiopathy in the brains of patients with Alzheimer’s disease: the CERAD experience, part XV. Neurology 46:1592–1596
Esiri MM, Wilcock GK (1986) Cerebral amyloid angiopathy in dementia and old age. J Neurol Neurosurg Psychiatry 49:1221–1226
Esiri MM, Wilcock GK, Morris JH (1997) Neuropathological assessment of the lesions of significance in vascular dementia. J Neurol Neurosurg Psychiatry 63:749–753
Fernando MS, Ince PG, MRC Cognitive Function and Ageing Neuropathology Study Group (2004) Vascular pathologies and cognition in a population-based cohort of elderly people. J Neurol Sci 226:13–17. doi:10.1016/j.jns.2004.09.004
Fisk L, Nalivaeva NN, Boyle JP, Peers CS, Turner AJ (2007) Effects of hypoxia and oxidative stress on expression of neprilysin in human neuroblastoma cells and rat cortical neurones and astrocytes. Neurochem Res 32:1741–1748. doi:10.1007/s11064-007-9349-2
Fryer JD, Simmons K, Parsadanian M, Bales KR, Paul SM, Sullivan PM, Holtzman DM (2005) Human apolipoprotein E4 alters the amyloid-β 40:42 ratio and promotes the formation of cerebral amyloid angiopathy in an amyloid precursor protein transgenic model. J Neurosci 25:2803–2810. doi:10.1523/JNEUROSCI.5170-04.2005
Gentile MT, Vecchione C, Maffei A, Aretini A, Marino G, Poulet R, Capobianco L, Selvetella G, Lembo G (2004) Mechanisms of soluble β-amyloid impairment of endothelial function. J Biol Chem 279:48135–48142. doi:10.1074/jbc.M407358200
Gilbert JJ, Vinters HV (1983) Cerebral amyloid angiopathy: incidence and complications in the aging brain. I. Cerebral hemorrhage. Stroke 14:915–923
Greenberg SM (1998) Cerebral amyloid angiopathy: prospects for clinical diagnosis and treatment. Neurology 51:690–694
Greenberg SM, Briggs ME, Hyman BT, Kokoris GJ, Takis C, Kanter DS, Kase CS, Pessin MS (1996) Apolipoprotein E ϵ4 is associated with the presence and earlier onset of hemorrhage in cerebral amyloid angiopathy. Stroke 27:1333–1337
Greenberg SM, Rebeck GW, Vonsattel JP, Gomez-Isla T, Hyman BT (1995) Apolipoprotein E ϵ4 and cerebral hemorrhage associated with amyloid angiopathy. Ann Neurol 38:254–259. doi:10.1002/ana.410380219
Greenberg SM, Vonsattel JP, Segal AZ, Chiu RI, Clatworthy AE, Liao A, Hyman BT, Rebeck GW (1998) Association of apolipoprotein E ε2 and vasculopathy in cerebral amyloid angiopathy. Neurology 50:961–965
Guglielmotto M, Aragno M, Autelli R, Giliberto L, Novo E, Colombatto S, Danni O, Parola M, Smith MA, Perry G et al (2009) The up-regulation of BACE1 mediated by hypoxia and ischemic injury: role of oxidative stress and HIF1α. J Neurochem 108:1045–1056. doi:10.1111/j.1471-4159.2008.05858.x
Haque SU, Dashwood MR, Heetun M, Shiwen X, Farooqui N, Ramesh B, Welch H, Savage FJ, Ogunbiyi O, Abraham DJ et al (2013) Efficacy of the specific endothelin a receptor antagonist zibotentan (ZD4054) in colorectal cancer: a preclinical study. Mol Cancer Ther 12:1556–1567. doi:10.1158/1535-7163.MCT-12-0975
Hartz AM, Bauer B, Soldner EL, Wolf A, Boy S, Backhaus R, Mihaljevic I, Bogdahn U, Klunemann HH, Schuierer G et al (2012) Amyloid-β contributes to blood-brain barrier leakage in transgenic human amyloid precursor protein mice and in humans with cerebral amyloid angiopathy. Stroke 43:514–523. doi:10.1161/STROKEAHA.111.627562
Hawkes CA, Gatherer M, Sharp MM, Dorr A, Yuen HM, Kalaria R, Weller RO, Carare RO (2013) Regional differences in the morphological and functional effects of aging on cerebral basement membranes and perivascular drainage of amyloid-β from the mouse brain. Aging Cell 12:224–236. doi:10.1111/acel.12045
Hawkes CA, Hartig W, Kacza J, Schliebs R, Weller RO, Nicoll JA, Carare RO (2011) Perivascular drainage of solutes is impaired in the ageing mouse brain and in the presence of cerebral amyloid angiopathy. Acta Neuropathol 121:431–443. doi:10.1007/s00401-011-0801-7
Hawkes CA, Sullivan PM, Hands S, Weller RO, Nicoll JA, Carare RO (2012) Disruption of arterial perivascular drainage of amyloid-β from the brains of mice expressing the human APOE ϵ4 allele. PLoS ONE 7:e41636. doi:10.1371/journal.pone.0041636
Helzner EP, Luchsinger JA, Scarmeas N, Cosentino S, Brickman AM, Glymour MM, Stern Y (2009) Contribution of vascular risk factors to the progression in Alzheimer disease. Arch Neurol 66:343–348. doi:10.1001/archneur.66.3.343
Hemming ML, Selkoe DJ (2005) Amyloid β-protein is degraded by cellular angiotensin-converting enzyme (ACE) and elevated by an ACE inhibitor. J Biol Chem 280:37644–37650. doi:10.1074/jbc.M508460200
Herzig MC, Van Nostrand WE, Jucker M (2006) Mechanism of cerebral β-amyloid angiopathy: murine and cellular models. Brain Pathol 16:40–54
Heyman A, Fillenbaum GG, Welsh-Bohmer KA, Gearing M, Mirra SS, Mohs RC, Peterson BL, Pieper CF (1998) Cerebral infarcts in patients with autopsy-proven Alzheimer’s disease: CERAD, part XVIII. Consortium to establish a registry for Alzheimer’s Disease. Neurology 51:159–162
Hofman A, Ott A, Breteler MM, Bots ML, Slooter AJ, van Harskamp F, van Duijn CN, Van Broeckhoven C, Grobbee DE (1997) Atherosclerosis, apolipoprotein E, and prevalence of dementia and Alzheimer’s disease in the Rotterdam Study. Lancet 349:151–154
Holton JL, Ghiso J, Lashley T, Rostagno A, Guerin CJ, Gibb G, Houlden H, Ayling H, Martinian L, Anderton BH et al (2001) Regional distribution of amyloid-Bri deposition and its association with neurofibrillary degeneration in familial British dementia. Am J Pathol 158:515–526. doi:10.1016/S0002-9440(10)63993-4
Honig LS, Kukull W, Mayeux R (2005) Atherosclerosis and AD: analysis of data from the US National Alzheimer’s Coordinating Center. Neurology 64:494–500. doi:10.1212/01.WNL.0000150886.50187.30
Hu J, Igarashi A, Kamata M, Nakagawa H (2001) Angiotensin-converting enzyme degrades Alzheimer amyloid β-peptide (Aβ); retards Aβ aggregation, deposition, fibril formation; and inhibits cytotoxicity. J Biol Chem 276:47863–47868. doi:10.1074/jbc.M104068200
Hughes TM, Kuller LH, Barinas-Mitchell EJ, McDade EM, Klunk WE, Cohen AD, Mathis CA, Dekosky ST, Price JC, Lopez OL (2014) Arterial stiffness and β-amyloid progression in nondemented elderly adults. JAMA Neurol 71:562–568. doi:10.1001/jamaneurol.2014.186
Hunter JM, Kwan J, Malek-Ahmadi M, Maarouf CL, Kokjohn TA, Belden C, Sabbagh MN, Beach TG, Roher AE (2012) Morphological and pathological evolution of the brain microcirculation in aging and Alzheimer’s disease. PLoS ONE 7:e36893. doi:10.1371/journal.pone.0036893
Iadecola C (2004) Neurovascular regulation in the normal brain and in Alzheimer’s disease. Nat Rev Neurosci 5:347–360. doi:10.1038/nrn1387
Iores-Marcal LM, Viel TA, Buck HS, Nunes VA, Gozzo AJ, Cruz-Silva I, Miranda A, Shimamoto K, Ura N, Araujo MS (2006) Bradykinin release and inactivation in brain of rats submitted to an experimental model of Alzheimer’s disease. Peptides 27:3363–3369. doi:10.1016/j.peptides.2006.08.012
Itoh Y, Yamada M, Sodeyama N, Suematsu N, Matsushita M, Otomo E, Mizusawa H (1999) Atherosclerosis is not implicated in association of APOE ϵ4 with AD. Neurology 53:236–237
Jellinger KA, Attems J (2003) Incidence of cerebrovascular lesions in Alzheimer’s disease: a postmortem study. Acta Neuropathol 105:14–17. doi:10.1007/s00401-002-0634-5
Kalaria RN, Ballard C (1999) Overlap between pathology of Alzheimer disease and vascular dementia. Alzheimer Dis Assoc Disord 13(Suppl 3):S115–S123
Keable A, Fenna K, Yuen HM, Johnston DA, Smyth NR, Smith C, Salman RA, Samarasekera N, Nicoll JA, Attems J et al (2015) Deposition of amyloid β in the walls of human leptomeningeal arteries in relation to perivascular drainage pathways in cerebral amyloid angiopathy. Biochim Biophys Acta. doi:10.1016/j.bbadis.2015.08.024
Kehoe PG (2003) The renin-angiotensin-aldosterone system and Alzheimer s disease? J Renin Angiotensin Aldosterone Syst 4:80–93. doi:10.3317/jraas.2003.017
Kehoe PG, Miners S, Love S (2009) Angiotensins in Alzheimer’s disease—friend or foe? Trends Neurosci 32:619–628. doi:10.1016/j.tins.2009.07.006
Kehoe PG, Passmore PA (2012) The renin-angiotensin system and antihypertensive drugs in Alzheimer’s disease: current standing of the angiotensin hypothesis? J Alzheimers Dis 30(Suppl 2):S251–S268. doi:10.3233/JAD-2012-111376
Kehoe PG, Wilcock GK (2007) Is inhibition of the renin-angiotensin system a new treatment option for Alzheimer’s disease? Lancet Neurol 6:373–378. doi:10.1016/S1474-4422(07)70077-7
Kenny RA, Kalaria R, Ballard C (2002) Neurocardiovascular instability in cognitive impairment and dementia. Ann N Y Acad Sci 977:183–195
Kenny RA, Shaw FE, O’Brien JT, Scheltens PH, Kalaria R, Ballard C (2004) Carotid sinus syndrome is common in dementia with Lewy bodies and correlates with deep white matter lesions. J Neurol Neurosurg Psychiatry 75:966–971
Kester MI, Goos JD, Teunissen CE, Benedictus MR, Bouwman FH, Wattjes MP, Barkhof F, Scheltens P, van der Flier WM (2014) Associations between cerebral small-vessel disease and Alzheimer disease pathology as measured by cerebrospinal fluid biomarkers. JAMA Neurol 71:855–862. doi:10.1001/jamaneurol.2014.754
Knudsen KA, Rosand J, Karluk D, Greenberg SM (2001) Clinical diagnosis of cerebral amyloid angiopathy: validation of the Boston criteria. Neurology 56:537–539
Kook SY, Hong HS, Moon M, Ha CM, Chang S, Mook-Jung I (2012) Aβ(1-42)-RAGE interaction disrupts tight junctions of the blood-brain barrier via Ca(2 +)-calcineurin signaling. J Neurosci 32:8845–8854. doi:10.1523/JNEUROSCI.6102-11.2012
Kosunen O, Talasniemi S, Lehtovirta M, Heinonen O, Helisalmi S, Mannermaa A, Paljarvi L, Ryynanen M, Riekkinen PJ Sr, Soininen H (1995) Relation of coronary atherosclerosis and apolipoprotein E genotypes in Alzheimer patients. Stroke 26:743–748
Koyama A, Weuve J, Jackson JW, Blacker D (2014) “Dietary pattern”. The AlzRisk database. Alzheimer research forum. http://www.alzrisk.org. Accessed 5 July 2015
Lamoke F, Mazzone V, Persichini T, Maraschi A, Harris MB, Venema RC, Colasanti M, Gliozzi M, Muscoli C, Bartoli M et al (2015) Amyloid β peptide-induced inhibition of endothelial nitric oxide production involves oxidative stress-mediated constitutive eNOS/HSP90 interaction and disruption of agonist-mediated Akt activation. J Neuroinflammation 12:84. doi:10.1186/s12974-015-0304-x
Langbaum JB, Chen K, Caselli RJ, Lee W, Reschke C, Bandy D, Alexander GE, Burns CM, Kaszniak AW, Reeder SA et al (2010) Hypometabolism in Alzheimer-affected brain regions in cognitively healthy Latino individuals carrying the apolipoprotein E ϵ4 allele. Arch Neurol 67:462–468. doi:10.1001/archneurol.2010.30
Li J, Wang YJ, Zhang M, Xu ZQ, Gao CY, Fang CQ, Yan JC, Zhou HD (2011) Vascular risk factors promote conversion from mild cognitive impairment to Alzheimer disease. Neurology 76:1485–1491 (WNL.0b013e318217e7a4)
Li L, Zhang X, Yang D, Luo G, Chen S, Le W (2009) Hypoxia increases Aβ generation by altering β- and γ-cleavage of APP. Neurobiol Aging 30:1091–1098. doi:10.1016/j.neurobiolaging.2007.10.011
Li S, Goonesekera S, Weuve J, Jackson JW, Blacker D “Homocysteine”. The AlzRisk database. Alzheimer research forum. http://www.alzrisk.org. Accessed 5 July 2015
Linn J, Halpin A, Demaerel P, Ruhland J, Giese AD, Dichgans M, van Buchem MA, Bruckmann H, Greenberg SM (2010) Prevalence of superficial siderosis in patients with cerebral amyloid angiopathy. Neurology 74:1346–1350. doi:10.1212/WNL.0b013e3181dad605
Liu G, Yao L, Liu J, Jiang Y, Ma G, Genetic and Environmental Risk for Alzheimer's disease (GERAD1) Consortium, Chen Z, Zhao B, Li K (2014) Cardiovascular disease contributes to Alzheimer’s disease: evidence from large-scale genome-wide association studies. Neurobiol Aging 35:786–792. doi:10.1016/j.neurobiolaging.2013.10.084
Love S, Chalmers K, Ince P, Esiri M, Attems J, Jellinger K, Yamada M, McCarron M, Minett T, Matthews F et al (2014) Development, appraisal, validation and implementation of a consensus protocol for the assessment of cerebral amyloid angiopathy in post-mortem brain tissue. Am J Neurodegener Dis 3:19–32
Love S, Miners JS (2015) White matter hypoperfusion and damage in dementia: post-mortem assessment. Brain Pathol 25:99–107. doi:10.1111/bpa.12223
Love S, Miners S, Palmer J, Chalmers K, Kehoe P (2009) Insights into the pathogenesis and pathogenicity of cerebral amyloid angiopathy. Front Biosci (Landmark Ed) 14:4778–4792
Love S, Nicoll JA, Hughes A, Wilcock GK (2003) APOE and cerebral amyloid angiopathy in the elderly. NeuroReport 14:1535–1536. doi:10.1097/01.wnr.0000085694.46774.90
Luchsinger JA, Reitz C, Honig LS, Tang MX, Shea S, Mayeux R (2005) Aggregation of vascular risk factors and risk of incident Alzheimer disease. Neurology 65:545–551. doi:10.1212/01.wnl.0000172914.08967.dc
Marco S, Skaper SD (2006) Amyloid β-peptide1-42 alters tight junction protein distribution and expression in brain microvessel endothelial cells. Neurosci Lett 401:219–224. doi:10.1016/j.neulet.2006.03.047
Masuda J, Tanaka K, Ueda K, Omae T (1988) Autopsy study of incidence and distribution of cerebral amyloid angiopathy in Hisayama, Japan. Stroke 19:205–210
McCarron MO, Delong D, Alberts MJ (1999) APOE genotype as a risk factor for ischemic cerebrovascular disease: a meta-analysis. Neurology 53:1308–1311
McCarron MO, Nicoll JA, Stewart J, Ironside JW, Mann DM, Love S, Graham DI, Dewar D (1999) The apolipoprotein E ϵ2 allele and the pathological features in cerebral amyloid angiopathy-related hemorrhage. J Neuropathol Exp Neurol 58:711–718
Meng XF, Yu JT, Wang HF, Tan MS, Wang C, Tan CC, Tan L (2014) Midlife vascular risk factors and the risk of Alzheimer’s disease: a systematic review and meta-analysis. J Alzheimers Dis 42:1295–1310. doi:10.3233/JAD-140954
Miners JS, Ashby E, Van Helmond Z, Chalmers KA, Palmer LE, Love S, Kehoe PG (2008) Angiotensin-converting enzyme (ACE) levels and activity in Alzheimer’s disease, and relationship of perivascular ACE-1 to cerebral amyloid angiopathy. Neuropathol Appl Neurobiol 34:181–193. doi:10.1111/j.1365-2990.2007.00885.x
Miners JS, Palmer J, Love S (in press) Pathophysiology of hypoperfusion of the precuneus in early Alzheimer’s disease. Brain Pathol. doi: 10.1111/bpa.12331
Miners S, Ashby E, Baig S, Harrison R, Tayler H, Speedy E, Prince JA, Love S, Kehoe PG (2009) Angiotensin-converting enzyme levels and activity in Alzheimer’s disease: differences in brain and CSF ACE and association with ACE1 genotypes. Am J Transl Res 1:163–177
Mondello S, Buki A, Barzo P, Randall J, Provuncher G, Hanlon D, Wilson D, Kobeissy F, Jeromin A (2014) CSF and plasma amyloid-β temporal profiles and relationships with neurological status and mortality after severe traumatic brain injury. Sci Rep 4:6446. doi:10.1038/srep06446
Morgen K, Schneider M, Frolich L, Tost H, Plichta MM, Kolsch H, Rakebrandt F, Rienhoff O, Jessen F, Peters O et al (2015) Apolipoprotein E-dependent load of white matter hyperintensities in Alzheimer’s disease: a voxel-based lesion mapping study. Alzheimers Res Ther 7:27. doi:10.1186/s13195-015-0111-8
Morris CD, Rose A, Curwen J, Hughes AM, Wilson DJ, Webb DJ (2005) Specific inhibition of the endothelin A receptor with ZD4054: clinical and pre-clinical evidence. Br J Cancer 92:2148–2152. doi:10.1038/sj.bjc.6602676
Murshid WR, Nelson RJ, Love S (1994) Spontaneous cerebral haemorrhage from cerebral amyloid angiopathy. Br J Neurosurg 8:457–460
Nagata K, Kondoh Y, Atchison R, Sato M, Satoh Y, Watahiki Y, Hirata Y, Yokoyama E (2000) Vascular and metabolic reserve in Alzheimer’s disease. Neurobiol Aging 21:301–307
Nagata K, Sato M, Satoh Y, Watahiki Y, Kondoh Y, Sugawara M, Box G, Wright D, Leung S, Yuya H et al (2002) Hemodynamic aspects of Alzheimer’s disease. Ann N Y Acad Sci 977:391–402
Nation DA, Wierenga CE, Clark LR, Dev SI, Stricker NH, Jak AJ, Salmon DP, Delano-Wood L, Bangen KJ, Rissman RA et al (2013) Cortical and subcortical cerebrovascular resistance index in mild cognitive impairment and Alzheimer’s disease. J Alzheimers Dis 36:689–698. doi:10.3233/JAD-130086
Ni J, Auriel E, Martinez-Ramirez S, Keil B, Reed AK, Fotiadis P, Gurol EM, Greenberg SM, Viswanathan A (2015) Cortical localization of microbleeds in cerebral amyloid angiopathy: an ultra high-field 7T MRI study. J Alzheimers Dis 43:1325–1330. doi:10.3233/JAD-140864
Nicoll JA, Burnett C, Love S, Graham DI, Dewar D, Ironside JW, Stewart J, Vinters HV (1997) High frequency of apolipoprotein E ϵ2 allele in hemorrhage due to cerebral amyloid angiopathy. Ann Neurol 41:716–721. doi:10.1002/ana.410410607
Niwa K, Kazama K, Younkin L, Younkin SG, Carlson GA, Iadecola C (2002) Cerebrovascular autoregulation is profoundly impaired in mice overexpressing amyloid precursor protein. Am J Physiol Heart Circ Physiol 283:H315–H323. doi:10.1152/ajpheart.00022.2002
Niwa K, Porter VA, Kazama K, Cornfield D, Carlson GA, Iadecola C (2001) Aβ-peptides enhance vasoconstriction in cerebral circulation. Am J Physiol Heart Circ Physiol 281:H2417–H2424
O’Caoimh R, Kehoe PG, Molloy DW (2014) Renin angiotensin aldosterone system inhibition in controlling dementia-related cognitive decline. J Alzheimers Dis 42(Suppl 4):S575–S586. doi:10.3233/JAD-141284
Oba R, Igarashi A, Kamata M, Nagata K, Takano S, Nakagawa H (2005) The N-terminal active centre of human angiotensin-converting enzyme degrades Alzheimer amyloid β-peptide. Eur J Neurosci 21:733–740. doi:10.1111/j.1460-9568.2005.03912.x
Okazaki H, Reagan TJ, Campbell RJ (1979) Clinicopathologic studies of primary cerebral amyloid angiopathy. Mayo Clin Proc 54:22–31
Olichney JM, Hansen LA, Hofstetter CR, Grundman M, Katzman R, Thal LJ (1995) Cerebral infarction in Alzheimer’s disease is associated with severe amyloid angiopathy and hypertension. Arch Neurol 52:702–708
Ott A, Breteler MM, de Bruyne MC, van Harskamp F, Grobbee DE, Hofman A (1997) Atrial fibrillation and dementia in a population-based study. The Rotterdam Study. Stroke 28:316–321
Pacheco-Quinto J, Eckman EA (2013) Endothelin-converting enzymes degrade intracellular β-amyloid produced within the endosomal/lysosomal pathway and autophagosomes. J Biol Chem 288:5606–5615. doi:10.1074/jbc.M112.422964
Palmer J, Love S (2011) Endothelin receptor antagonists: potential in Alzheimer’s disease. Pharmacol Res 63:525–531. doi:10.1016/j.phrs.2010.12.008
Palmer JC, Baig S, Kehoe PG, Love S (2009) Endothelin-converting enzyme-2 is increased in Alzheimer’s disease and up-regulated by Aβ. Am J Pathol 175:262–270. doi:10.2353/ajpath.2009.081054
Palmer JC, Barker R, Kehoe PG, Love S (2012) Endothelin-1 is elevated in Alzheimer’s disease and upregulated by amyloid-β. J Alzheimers Dis 29:853–861. doi:10.3233/JAD-2012-111760
Palmer JC, Tayler HM, Love S (2013) Endothelin-converting enzyme-1 activity, endothelin-1 production, and free radical-dependent vasoconstriction in Alzheimer’s disease. J Alzheimers Dis 36:577–587. doi:10.3233/JAD-130383
Park L, Koizumi K, El Jamal S, Zhou P, Previti ML, Van Nostrand WE, Carlson G, Iadecola C (2014) Age-dependent neurovascular dysfunction and damage in a mouse model of cerebral amyloid angiopathy. Stroke 45:1815–1821. doi:10.1161/STROKEAHA.114.005179
Peca S, McCreary CR, Donaldson E, Kumarpillai G, Shobha N, Sanchez K, Charlton A, Steinback CD, Beaudin AE, Fluck D et al (2013) Neurovascular decoupling is associated with severity of cerebral amyloid angiopathy. Neurology 81:1659–1665. doi:10.1212/01.wnl.0000435291.49598.54
Premkumar DR, Cohen DL, Hedera P, Friedland RP, Kalaria RN (1996) Apolipoprotein E-ϵ4 alleles in cerebral amyloid angiopathy and cerebrovascular pathology associated with Alzheimer’s disease. Am J Pathol 148:2083–2095
Raja SG, Dreyfus GD (2008) Current status of bosentan for treatment of pulmonary hypertension. Ann Card Anaesth 11:6–14
Reijmer YD, van Veluw SJ, Greenberg SM (2015) Ischemic brain injury in cerebral amyloid angiopathy. J Cereb Blood Flow Metab. doi:10.1038/jcbfm.2015.88
Richardson K, Stephan BC, Ince PG, Brayne C, Matthews FE, Esiri MM (2012) The neuropathology of vascular disease in the Medical Research Council Cognitive Function and Ageing Study (MRC CFAS). Curr Alzheimer Res 9:687–696
Roher AE, Esh C, Kokjohn TA, Kalback W, Luehrs DC, Seward JD, Sue LI, Beach TG (2003) Circle of Willis atherosclerosis is a risk factor for sporadic Alzheimer’s disease. Arterioscler Thromb Vasc Biol 23:2055–2062. doi:10.1161/01.ATV.0000095973.42032.44
Rossi R, Joachim C, Geroldi C, Combrinck M, Esiri MM, Smith AD, Frisoni GB (2004) Association between subcortical vascular disease on CT and neuropathological findings. Int J Geriatr Psychiatry 19:690–695. doi:10.1002/gps.1144
Rubin LJ, Badesch DB, Barst RJ, Galie N, Black CM, Keogh A, Pulido T, Frost A, Roux S, Leconte I et al (2002) Bosentan therapy for pulmonary arterial hypertension. N Engl J Med 346:896–903. doi:10.1056/NEJMoa012212
Rubin LJ, Roux S (2002) Bosentan: a dual endothelin receptor antagonist. Expert Opin Investig Drugs 11:991–1002. doi:10.1517/13543784.11.7.991
Sajeev G, Weuve J, McQueen MB, Blacker D “Diabetes”. The AlzRisk database. Alzheimer research forum. http://www.alzrisk.org. Accessed 5 July 2015
Scheltens P, Barkhof F, Valk J, Algra PR, van der Hoop RG, Nauta J, Wolters EC (1992) White matter lesions on magnetic resonance imaging in clinically diagnosed Alzheimer’s disease. Evidence for heterogeneity. Brain 115(Pt 3):735–748
Schilling S, DeStefano AL, Sachdev PS, Choi SH, Mather KA, DeCarli CD, Wen W, Hogh P, Raz N, Au R et al (2013) APOE genotype and MRI markers of cerebrovascular disease: systematic review and meta-analysis. Neurology 81:292–300. doi:10.1212/WNL.0b013e31829bfda4
Schmechel DE, Saunders AM, Strittmatter WJ, Crain BJ, Hulette CM, Joo SH, Pericak-Vance MA, Goldgaber D, Roses AD (1993) Increased amyloid β-peptide deposition in cerebral cortex as a consequence of apolipoprotein E genotype in late-onset Alzheimer disease. Proc Natl Acad Sci USA 90:9649–9653
Schneider JA, Wilson RS, Bienias JL, Evans DA, Bennett DA (2004) Cerebral infarctions and the likelihood of dementia from Alzheimer disease pathology. Neurology 62:1148–1155
Sengillo JD, Winkler EA, Walker CT, Sullivan JS, Johnson M, Zlokovic BV (2013) Deficiency in mural vascular cells coincides with blood-brain barrier disruption in Alzheimer’s disease. Brain Pathol 23:303–310. doi:10.1111/bpa.12004
Shi J, Yang SH, Stubley L, Day AL, Simpkins JW (2000) Hypoperfusion induces overexpression of β-amyloid precursor protein mRNA in a focal ischemic rodent model. Brain Res 853:1–4
Shibayama Y, Joseph K, Nakazawa Y, Ghebreihiwet B, Peerschke EI, Kaplan AP (1999) Zinc-dependent activation of the plasma kinin-forming cascade by aggregated β amyloid protein. Clin Immunol 90:89–99. doi:10.1006/clim.1998.4621
Shin HK, Jones PB, Garcia-Alloza M, Borrelli L, Greenberg SM, Bacskai BJ, Frosch MP, Hyman BT, Moskowitz MA, Ayata C (2007) Age-dependent cerebrovascular dysfunction in a transgenic mouse model of cerebral amyloid angiopathy. Brain 130:2310–2319. doi:10.1093/brain/awm156
Shinall H, Song ES, Hersh LB (2005) Susceptibility of amyloid β peptide degrading enzymes to oxidative damage: a potential Alzheimer’s disease spiral. Biochemistry 44:15345–15350. doi:10.1021/bi050650l
Snowdon DA, Greiner LH, Mortimer JA, Riley KP, Greiner PA, Markesbery WR (1997) Brain infarction and the clinical expression of Alzheimer disease. The Nun Study. JAMA 277:813–817
Sonnesyn H, Nilsen DW, Rongve A, Nore S, Ballard C, Tysnes OB, Aarsland D (2009) High prevalence of orthostatic hypotension in mild dementia. Dement Geriatr Cogn Disord 28:307–313. doi:10.1159/000247586
Sparks DL, Hunsaker JC 3rd, Scheff SW, Kryscio RJ, Henson JL, Markesbery WR (1990) Cortical senile plaques in coronary artery disease, aging and Alzheimer’s disease. Neurobiol Aging 11:601–607
Strozyk D, Dickson DW, Lipton RB, Katz M, Derby CA, Lee S, Wang C, Verghese J (2010) Contribution of vascular pathology to the clinical expression of dementia. Neurobiol Aging 31:1710–1720. doi:10.1016/j.neurobiolaging.2008.09.011
Suter OC, Sunthorn T, Kraftsik R, Straubel J, Darekar P, Khalili K, Miklossy J (2002) Cerebral hypoperfusion generates cortical watershed microinfarcts in Alzheimer disease. Stroke 33:1986–1992
Tai LM, Holloway KA, Male DK, Loughlin AJ, Romero IA (2010) Amyloid-β-induced occludin down-regulation and increased permeability in human brain endothelial cells is mediated by MAPK activation. J Cell Mol Med 14:1101–1112. doi:10.1111/j.1582-4934.2009.00717.x
Tanimukai H, Imaizumi K, Kudo T, Katayama T, Tsuda M, Takagi T, Tohyama M, Takeda M (1998) Alzheimer-associated presenilin-1 gene is induced in gerbil hippocampus after transient ischemia. Brain Res Mol Brain Res 54:212–218
Tarumi T, Dunsky DI, Khan MA, Liu J, Hill C, Armstrong K, Martin-Cook K, Cullum CM, Zhang R (2014) Dynamic cerebral autoregulation and tissue oxygenation in amnestic mild cognitive impairment. J Alzheimers Dis 41:765–778. doi:10.3233/JAD-132018
Thal DR, Ghebremedhin E, Rub U, Yamaguchi H, Del Tredici K, Braak H (2002) Two types of sporadic cerebral amyloid angiopathy. J Neuropathol Exp Neurol 61:282–293
Thomas T, Miners S, Love S (2015) Post-mortem assessment of hypoperfusion of cerebral cortex in Alzheimer’s disease and vascular dementia. Brain 138:1059–1069. doi:10.1093/brain/awv025
Tohgi H, Yonezawa H, Takahashi S, Sato N, Kato E, Kudo M, Hatano K, Sasaki T (1998) Cerebral blood flow and oxygen metabolism in senile dementia of Alzheimer’s type and vascular dementia with deep white matter changes. Neuroradiology 40:131–137
Tolppanen AM, Ngandu T, Kareholt I, Laatikainen T, Rusanen M, Soininen H, Kivipelto M (2014) Midlife and late-life body mass index and late-life dementia: results from a prospective population-based cohort. J Alzheimers Dis 38:201–209. doi:10.3233/JAD-130698
Tomonaga M (1981) Cerebral amyloid angiopathy in the elderly. J Am Geriatr Soc 29:151–157
Vinters HV, Gilbert JJ (1983) Cerebral amyloid angiopathy: incidence and complications in the aging brain. II. The distribution of amyloid vascular changes. Stroke 14:924–928
Wang R, Wang S, Malter JS, Wang DS (2009) Effects of HNE-modification induced by Aβ on neprilysin expression and activity in SH-SY5Y cells. J Neurochem 108:1072–1082. doi:10.1111/j.1471-4159.2008.05855.x
Weller RO, Kida S, Zhang ET (1992) Pathways of fluid drainage from the brain–morphological aspects and immunological significance in rat and man. Brain Pathol 2:277–284
Weller RO, Massey A, Newman TA, Hutchings M, Kuo YM, Roher AE (1998) Cerebral amyloid angiopathy: amyloid β accumulates in putative interstitial fluid drainage pathways in Alzheimer’s disease. Am J Pathol 153:725–733
Weller RO, Subash M, Preston SD, Mazanti I, Carare RO (2008) Perivascular drainage of amyloid-β peptides from the brain and its failure in cerebral amyloid angiopathy and Alzheimer’s disease. Brain Pathol 18:253–266. doi:10.1111/j.1750-3639.2008.00133.x
Wen Y, Onyewuchi O, Yang S, Liu R, Simpkins JW (2004) Increased β-secretase activity and expression in rats following transient cerebral ischemia. Brain Res 1009:1–8. doi:10.1016/j.brainres.2003.09.086
Wen Y, Yang S, Liu R, Simpkins JW (2004) Transient cerebral ischemia induces site-specific hyperphosphorylation of tau protein. Brain Res 1022:30–38. doi:10.1016/j.brainres.2004.05.106
Williams S, Chalmers K, Wilcock GK, Love S (2005) Relationship of neurofibrillary pathology to cerebral amyloid angiopathy in Alzheimer’s disease. Neuropathol Appl Neurobiol 31:414–421. doi:10.1111/j.1365-2990.2005.00663.x
Wirth KJ, Fink E, Rudolphi K, Heitsch H, Deutschlander N, Wiemer G (1999) Amyloid β-(1-40) stimulates cyclic GMP production via release of kinins in primary cultured endothelial cells. Eur J Pharmacol 382:27–33
Yamada M, Tsukagoshi H, Otomo E, Hayakawa M (1987) Cerebral amyloid angiopathy in the aged. J Neurol 234:371–376
Yarchoan M, Xie SX, Kling MA, Toledo JB, Wolk DA, Lee EB, Van Deerlin V, Lee VM, Trojanowski JQ, Arnold SE (2012) Cerebrovascular atherosclerosis correlates with Alzheimer pathology in neurodegenerative dementias. Brain 135:3749–3756. doi:10.1093/brain/aws271
Zetterberg H, Mortberg E, Song L, Chang L, Provuncher GK, Patel PP, Ferrell E, Fournier DR, Kan CW, Campbell TG et al (2011) Hypoxia due to cardiac arrest induces a time-dependent increase in serum amyloid β levels in humans. PLoS ONE 6:e28263. doi:10.1371/journal.pone.0028263
Zhang ET, Richards HK, Kida S, Weller RO (1992) Directional and compartmentalised drainage of interstitial fluid and cerebrospinal fluid from the rat brain. Acta Neuropathol 83:233–239
Zhang X, Zhou K, Wang R, Cui J, Lipton SA, Liao FF, Xu H, Zhang YW (2007) Hypoxia-inducible factor 1α (HIF-1α)-mediated hypoxia increases BACE1 expression and β-amyloid generation. J Biol Chem 282:10873–10880 (M608856200)
Zhiyou C, Yong Y, Shanquan S, Jun Z, Liangguo H, Ling Y, Jieying L (2009) Upregulation of BACE1 and β-amyloid protein mediated by chronic cerebral hypoperfusion contributes to cognitive impairment and pathogenesis of Alzheimer’s disease. Neurochem Res 34:1226–1235. doi:10.1007/s11064-008-9899-y
Acknowledgments
Supported by grants from the Medical Research Council MR/K015397/1; Alzheimer’s Research UK ART-PG2011-1, ARUK-NCG2013A-3, ARUK-PG2015-11; British Heart Foundation PG/10/47/28285; and BRACE (Bristol Research into Alzheimer’s and Care of the Elderly).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Love, S., Miners, J.S. Cerebrovascular disease in ageing and Alzheimer’s disease. Acta Neuropathol 131, 645–658 (2016). https://doi.org/10.1007/s00401-015-1522-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-015-1522-0