Abstract
Liver X receptors (LXRs) are master regulators of metabolism and have been studied for their pharmacological potential in vascular and metabolic disease. Besides their established role in metabolic homeostasis and disease, there is mounting evidence to suggest that LXRs may exert direct beneficial effects in the heart. Here, we aim to provide a conceptual framework to explain the broad mode of action of LXRs and how LXR signaling may be an important local and systemic target for the treatment of heart failure. We discuss the potential role of LXRs in systemic conditions associated with heart failure, such as hypertension, diabetes, and renal and vascular disease. Further, we expound on recent data that implicate a direct role for LXR activation in the heart, for its impact on cardiomyocyte damage and loss due to ischemia, and effects on cardiac hypertrophy, fibrosis, and myocardial metabolism. Taken together, the accumulating evidence supports the notion that LXRs may represent a novel therapeutic target for the treatment of heart failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of heart failure is increasing in our aging society and is associated with significant morbidity and mortality [88]. It is a complex clinical syndrome and diagnosis is based on physical signs and symptoms of dyspnea, fluid retention, and fatigue upon exertion. Heart failure is attributed to a process of pathological cardiac remodeling that is initiated via molecular, cellular, and interstitial changes that structurally and functionally alter the myocardium [54]. Cardiac remodeling is initially a compensatory response to injury such as myocardial infarction or hypertension, but is maladaptive when these factors continue unabated, perpetuating the progression toward cardiac dysfunction and heart failure. The time course and extent of remodeling are influenced by several factors such as the severity of the pathological insult, secondary events including recurrent ischemia or infarction, elevated hemodynamic load, and neurohormonal activation.
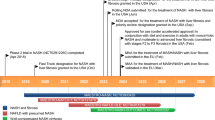
Heart failure manifests as a state of impaired pump function that results in inadequate cardiac output, and classification is based on left ventricular (LV) ejection fraction which is either reduced (HFrEF) or preserved (HFpEF) (Fig. 1) [46]. The dominant cause of HFrEF is coronary artery disease, and the underlying mechanisms that drive ventricular remodeling are the result of the ischemic injury caused by myocardial infarction. In the infarct zone, a fibrotic scar replaces loss of cardiomyocytes, whereas the remote myocardium undergoes eccentric remodeling that leads to LV dilatation, decreased contractility, and impaired systolic function. In contrast, HFpEF patients demonstrate evidence of diastolic dysfunction, including prolonged LV relaxation time, reduced LV filling, and increased myocardial stiffness [101], and often involves concentric remodeling of the myocardium.
Impact of systemic LXR signaling on co-morbidities associated with heart failure pathogenesis. The progression of atherosclerotic vascular disease increases the risk for myocardial infarction. Myocardial infarction causes eccentric remodeling of the myocardium and loss of systolic function; it is the predominant etiology underlying heart failure with reduced ejection fraction (HFrEF). The presence of co-morbidities such as hypertension, atrial fibrillation, diabetes, metabolic syndrome, renal disease, and aging, all impact the heart, which results in concentric hypertrophic remodeling and loss of diastolic function. This ultimately leads to the pathogenesis of heart failure with preserved ejection fraction (HFpEF). Cardiac remodeling is initially reversible, however, the prevalence of co-morbidities further aggravates the progression of both HFrEF and HFpEF such that adverse remodeling is accelerated and becomes largely irreversible. Consequently, death is inevitable. Liver X receptors (LXRs) are implicated as a protective target in the pathogenesis of heart failure for their beneficial effects in the development of atherosclerosis, insulin resistance and diabetes, nephropathy, and blood pressure modulation*
Most pharmacological therapies such as β-blockade and inhibitors of the renin-angiotensin-aldosterone system (RAAS) have proven efficacy in HFrEF by reducing morbidity and mortality [14]. However, this strategy has not been as successful for treating HFpEF [85], therefore diagnosing and treating HFpEF remains a challenge. In essence, the underlying pathophysiology of HFpEF is poorly understood largely owing to the presence of multiple co-morbidities such as hypertension, diabetes, metabolic syndrome, atrial fibrillation, and renal and vascular disease, which impact the pathogenesis of this syndrome and contribute to the complexity of mechanisms governing cardiac remodeling [86]. Lack of a clear understanding of these mechanisms thus poses several challenges in targeting and treating heart failure. Identification of novel pleiotropic targets that are integrative across multi-organ systems may therefore be effective therapeutic strategies in preventing or reversing heart failure.
Liver X receptors (LXR) α and β belong to the nuclear receptor superfamily of ligand-activated transcription factors. LXRs have emerged as important regulators of cholesterol homeostasis, lipid and glucose metabolism, and inflammation, and so have been regarded as promising therapeutic targets for intervention in atherosclerotic and metabolic disease [130]. They were originally discovered in the mid-1990s as “orphan receptors” because their natural ligands were yet unknown [4, 120, 137]. Shortly thereafter, oxysterols as well as cholesterol metabolites were identified as endogenous activators of LXRs, thus LXRs were “deorphanized” [60]. In the nucleus, LXRs form obligate heterodimers with the retinoid X receptor (RXR) and are bound to LXR response elements (LXREs) in regulatory regions of target genes. Binding of either their natural or synthetic ligands, such as T0901317 (T09) and GW3965, induces a conformational change in the LXR/RXR complex that facilitates activation of target gene transcription (Fig. 2). LXRβ is ubiquitously expressed, whereas LXRα features more abundantly in metabolically active systems such as the liver, adipose tissue, and macrophages, as well as in heart, skeletal muscle, kidney, and lung [102]. In the heart, expression levels of both LXRs are 10- to 15-fold higher in the non-myocytic compartment, consisting of fibroblasts and endothelial cells, compared to the myocyte compartment [79].
Mechanism of liver X receptor activation. In the nucleus, LXRs form an obligate heterodimer complex with the retinoid X receptor (RXR) that binds to an LXR response element (LXRE) in regulatory regions of target genes. Following ligand binding, the LXR/RXR complex undergoes a conformational change that leads to the release of co-repressors and the recruitment of co-activators, which activates target gene transcription
Here, we review recent evidence regarding the systemic effects of LXRs in relation to co-morbidities that are relevant in heart failure pathogenesis. Although studies of LXRs in the heart are few, they have generated clear evidence that LXR signaling exerts a potential cardioprotective role in cardiac remodeling and myocardial disease. Altogether, we provide a perspective on the potentiality of LXRs as an integrative target for the treatment of heart failure.
Systemic effects of LXR signaling in the development and progression of heart failure
Combined co-morbidities have a major impact on the pathogenesis of heart failure, which led to the supposition that myocardial dysfunction may not originate exclusively in the heart itself, but extrinsic factors that stem from these co-morbidities may perturb the heart [115]. Here, current knowledge on the role of LXRs in the pathogenesis of several of these co-morbidities, including atherosclerosis and vascular disease, hypertension, diabetes, metabolic syndrome, and chronic kidney disease, is summarized (Table 1). Given the widespread effects of LXRs, we postulate that systemic LXR activation may play an important role in conferring myocardial protection from these disorders that collectively contribute to the pathogenesis of HFrEF and HFpEF.
LXR and atherosclerosis
Atherosclerosis contributes to multi-organ dysfunction involving the kidney, brain, gut, and skeletal muscle, and is a major cause of HFrEF following myocardial infarction. LXRs have been extensively studied for their putative atheroprotective functions [15]. The initial stages of atherosclerosis involve the formation of foam cells by the uptake of oxidized low-density lipoprotein (LDL) in macrophages in the arterial wall. Mice deficient for both LXRα and LXRβ develop increased foam cell formation, implicating a basal role in cholesterol homeostasis [114]. LXRs limit pathogenic accumulation of cholesterol in macrophages by enhancing the rate of cholesterol efflux [94], which is mediated through upregulation of genes involved in all aspects of the reverse cholesterol transport (RCT) pathway, including Abca1, Abcg1, and ApoE in cellular cholesterol efflux, CETP and PLTP in plasma lipid transport, Abcg5 and Abcg8 for entero-hepatic sterol absorption and excretion, and Cyp7a1 for enhanced bile acid excretion [109]. In murine models, LXR agonist treatment significantly reduced atherosclerosis in both Ldlr −/− and apoE −/− mice [64], whereas selective loss of macrophage LXR activity through bone marrow transplantations markedly increased lesion development in these models [128]. Interestingly, liver-specific deletion of LXRα in mice leads to decreased RCT, cholesterol catabolism, and excretion while substantially increasing atherosclerosis, altogether underscoring their importance as whole-body cholesterol sensors [143].
In macrophages, the metabolic functions of LXRs are coupled to anti-inflammatory responses, which further contribute to the mechanism underlying their atheroprotective effects. LXR agonist activation inhibits the induction of pro-inflammatory cytokines through a mechanism involving transrepression [63]. In atherogenic Ldlr −/− mice, selectively increasing LXRα in macrophages leads to reductions in plasma inflammatory cytokines, IL6 and TNFα, and atherosclerotic lesion development [82]. Moreover, in the absence of cholesterol efflux pathways mediated by Abca1/g1-deficient macrophages, LXR agonism nonetheless decreased lesion area, complexity, and inflammatory cell infiltration, including plasma levels of the chemokine, MCP1 [67]. LXRs have also been shown to target the inflammatory process in atherogenesis at a critical step through the inhibition of chemokine-induced CD4-positive lymphocyte migration [133].
More recent evidence implicates additional atheroprotective properties of LXR agonists in the pathogenesis of atherosclerosis that extend beyond their capacity to promote peripheral cholesterol efflux and inhibit inflammation. A novel anti-atherosclerotic mechanism for LXRα through regulation of macrophage iron homeostasis has been identified. By increasing iron export, LXRα reduces iron loading which promotes formation of oxidized lipids, an inducer of cell death [12]. Other functions for LXRs within the vasculature are emerging. Endothelial dysfunction is the underlying cause of all vascular diseases and is a critical initiator of atherosclerosis. LXRs are expressed in endothelial cells [121], and their distribution in murine aortas reveals a greater degree of expression in the atheroprotective thoracic region than in atheroprone areas such as the aortic arch, supporting an anti-atherogenic function [145]. In atherosclerotic vessel walls, studies indicate that LXR activation decreases vascular expression of adhesion molecules such as E-selectin, ICAM-1, and CD44 [131], and improves arterial vasomotor function through enhanced endothelium-dependent vasorelaxation [22].
Also of relevance are the reparative effects of LXRs in vascular injury. The progression of atherosclerosis is accelerated via denuding of the endothelium and intimal injury, which are accompanied by platelet deposition, thrombus formation, and smooth muscle cell proliferation. In rodent models of carotid artery injury, LXR ligands repaired damaged vessel walls by advancing endothelial regeneration through increased proliferation and migration of endothelial progenitor cells and enhancing their secretion of vascular endothelial growth factor (VEGF) [140], as well as inhibiting vascular smooth muscle cell proliferation and neointima formation [11]. Also of note is the identification of a novel role for LXRs in thrombosis and platelet function. Although platelets are anuclear, they reportedly express LXRβ and GW3965 treatment has been shown to inhibit platelet accumulation and thrombi formation [122].
Taken together, evidence of an atheroprotective role for LXRs continues to broaden as studies reveal novel functions in cholesterol efflux, macrophage activity, and vascular protection. Preventing atherosclerotic lesion development is of paramount importance in offsetting coronary syndromes such as myocardial infarction, the major cause of systolic dysfunction leading to HFrEF. Thus, LXRs represent a promising target in the etiology underlying HFrEF and subsequent mortality.
LXR and hypertension
In HFpEF, hypertension is the most prevalent co-morbidity [89] and precedes heart failure in 60–90 % of all cases [81]. Besides being a risk factor for atherosclerosis and causing vascular injury, hypertension affects the cardiac muscle by invoking pathological hypertrophic growth through increased hemodynamic afterload.
The RAAS is a predominant hormonal signaling pathway in the regulation of blood pressure, fluid balance, and systemic vascular resistance. LXRs have been implicated in blood pressure control through modulation of the RAAS. Initial observations identified LXRα as a regulator of renin transcription [92, 127]. Acute administration of LXR agonists directly increased renin mRNA levels in vivo, whereas LXR-null mice lost their capacity to upregulate renin under β-adrenergic stress [92], suggesting a crosstalk between LXR signaling and the RAAS. In subsequent studies, chronic LXR activation inhibited isoproterenol-induced components of the RAAS, including renin, but also angiotensin converting enzyme (ACE) and angiotensin type I receptor (AT1R) expression in kidneys and heart [76]. Furthermore, in vivo investigation of the functional effects of LXRs on RAAS activation revealed that LXR agonism abolished angiotensin (Ang) II-induced increases in blood pressure in rats [80]. Although improved vasoreactivity was not unequivocally linked to the level of RAAS activation, these findings suggest that LXRs decrease peripheral vascular resistance and potentially lower blood pressure. In line with this, the LXR agonist T09 was found to reduce the elevation in blood pressure due to chronic pressure–volume overload in mice, whereas this effect was absent in mice lacking LXRα [75].
The RAAS is not only regulated by mechanisms that stimulate renin release, but is also modulated by natriuretic peptides, ANP and BNP, which are produced by the heart and antagonize the RAAS pathway. Recently, overexpressing cardiac LXRα has been shown to upregulate natriuretic peptide expression [16] (Cannon et al., unpublished data); therefore, LXRα modulation of natriuretic peptides may represent an indirect mechanism for RAAS suppression. Overall, existing evidence suggests that LXRs play a role in antagonizing RAAS activation and may be a viable target in alleviating the hemodynamic burden imposed on the heart.
LXR and diabetes
Disturbances in energy balance leads to impaired peripheral glucose utilization and the development of insulin resistance and type II diabetes, both of which increase the risk for cardiovascular disease [58]. Diabetes accelerates atherosclerosis, but also directly causes myocardial hypertrophy and diastolic dysfunction in the absence of hypertension or coronary artery disease [43].
LXR agonists have been recognized as a potential pharmacological strategy for the treatment of diabetes and associated metabolic disorders [45]. Multiple studies have established the importance of LXRs in glucose metabolism and in the adaptation to metabolic stress that triggers diabetes. In rodent models of type II diabetes and insulin resistance, LXR agonists have been shown to reduce plasma glucose [18, 84] and improve glucose tolerance and insulin sensitivity [18, 29, 48, 77, 84]. Mechanisms underlying the beneficial effects of LXRs on glucose homeostasis span several organ systems including the liver, adipose tissue, skeletal muscle, and pancreas. In the liver, LXR agonists suppress gluconeogenesis by downregulating Pgc1a, Pepck, and G6Pase genes, and induce glucokinase to promote hepatic glucose utilization [18, 77, 125]. In adipose tissue and skeletal muscle, LXRs directly regulate transcription of the glucose transporter, Glut4, and enhance peripheral glucose uptake both in the absence [33, 77] and presence of diabetes [6, 68]. In pancreatic islet cells, an important homeostatic role for LXRβ has been elucidated as Lxrβ −/− mice are intolerant to glucose due to impaired glucose-stimulated insulin secretion [44], whereas LXR ligands have been found to promote β-cell insulin secretion [39, 44, 48].
Although LXR agonists represent promising anti-diabetic agents given their insulin-sensitizing effects, the favorable effects on glucose metabolism need to be dissociated from their lipogenic effects for these compounds to be of potential clinical use (Table 1). LXR agonists enhance hepatic and skeletal muscle lipid accumulation and increase circulating triglycerides [30, 68], which worsens the lipogenic pathology in diabetes [26]. Chronic LXR activation may also impair insulin secretion by contributing to lipotoxicity-induced pancreatic β-cell apoptosis [27]. To circumvent these ramifications, alternative approaches are being initiated which include the development of partial LXR ligands or LXRβ-specific agonists since lipogenesis is mediated primarily via LXRα [59]. Interestingly, a recent study reported that administration of the LXR agonist T09 in combination with metformin, an established oral anti-diabetic drug, ameliorated the development of hepatic steatosis induced by LXR agonism in diabetic rats [49], suggesting that combinatorial therapies may also be viable.
Apart from metabolic dysregulation, diabetes is also characterized by low-grade inflammation that stems from macrophage infiltration in adipose tissue and secretion of pro-inflammatory cytokines [129]. By antagonizing NFκB signaling in the nucleus, LXRs have been shown to inhibit the induction of pro-inflammatory genes encoding iNOS, COX-2, IL6, and MCP1 [63]. To date, the impact of the anti-inflammatory functions of LXRs on diabetic pathophysiology is largely unknown. Since chronic systemic inflammation predisposes toward myocardial dysfunction and resultant HFpEF [100], we postulate that LXRs may protect the heart, amongst other susceptible organs, from diabetes- and obesity-induced inflammation.
In summary, LXRs are implicated in the protection against diabetes through modulation of glucose metabolism, β-cell insulin secretion, and inflammatory signaling, including recent developments indicating vasoprotection from hyperglycemia-induced endothelial dysfunction [50, 83]. Overall, LXRs mediate several pathways involved in diabetes, and as such, potentially affect the pathogenesis of HFpEF. These multiple effects are also linked to other co-morbidities contributing to heart failure development: atherosclerosis, the major cause of HFpEF, which is further aggravated by the presence of diabetes, as well as diabetes-induced kidney damage, which results in renal dysfunction, failure, and eventual HFpEF (discussed below).
LXR, obesity and metabolic syndrome
The metabolic syndrome is comprised of a cluster of metabolic abnormalities that include disturbances in glucose homeostasis, insulin resistance, obesity, dyslipidemia, and elevated blood pressure. These conditions increase the risk of developing cardiovascular disease and diabetes. Maintaining glucose homeostasis and improving insulin sensitivity are important effects of LXRs that potentially influence the development of insulin resistance and diabetes. However, the role of LXRs in modulating the molecular pathogenesis of the metabolic syndrome is less clear.
LXRs are critically involved in cholesterol homeostasis and lipid metabolism. In Lxrα −/− and Lxrα/β −/− mice, serum LDL is increased and HDL is decreased, but not in Lxrβ −/− mice, whereas serum and VLDL and LDL triglycerides are reduced in double-mutants [114]. Further, LXR agonism treatment lowers total and unesterified cholesterol levels in atherogenic Ldlr −/− mice [64]. In addition to promoting RCT [94], LXRs have also been shown to limit LDL receptor-dependent cholesterol uptake by transcriptionally inducing Idol, an E3 ubiquitin ligase that triggers ubiquitination of the LDL receptor, targeting it for degradation [141].
Apart from enhancing cholesterol catabolism and transport, LXRs are centrally involved in promoting hepatic lipogenesis. LXRs induce lipid synthesis by directly regulating the expression of Srebp1c and downstream target genes, Acc, Fas, and Scd1 [108]. Furthermore, functional LXREs have been identified in the promoter region of ChREBP, a glucose-activated transcription factor that converts excess carbohydrates into lipids [20]. LXRs are also implicated in regulating lipolysis within adipose tissue [124]. In rodents, LXR agonism has been shown to reduce adipocyte size [29], as well as increase serum levels of glycerol and nonesterified free fatty acids, indicative of increased triglyceride hydrolysis [111]. Altogether, dual effects of LXRs on hepatic lipogenesis and adipocyte lipolysis promote hyperlipidemia and insulin resistance, which are undesirable phenomena in the development of the metabolic syndrome.
The effect of LXRs on obesity has also been examined. LXR null mice are resistant to diet-induced obesity and exhibit significant reductions in adipocyte size [65, 74]. In an alternative model of genetic obesity, LXRα/β-deficient ob/ob mice remain obese and have increased adipose lipid storage, but display reduced hepatic lipid accumulation and improved insulin sensitivity compared to ob/ob mice [7]. Despite being more insulin sensitive, LXRα/β-deficient ob/ob mice are, however, glucose intolerant and have impaired pancreatic function. These data suggest that, although LXRs may not protect against obesity, their expression nevertheless influences lipid accumulation, insulin sensitivity, and glucose homeostasis in the setting of obesity [7]. Other studies have shown that LXRs may affect obesity through modulating pathways involved in nutrient status and energy expenditure. LXR agonism downregulated leptin expression in white adipose tissue in mice as well as decreased UCP1 expression, leading to increased energy intake and decreased energy expenditure, respectively [125].
Alternatively, LXRs may protect against obesity through anti-inflammatory functions that ameliorate the development of insulin resistance. LXR agonism has been shown to inhibit TNFα-stimulated release of inflammatory cytokines in fat cells, while re-establishing insulin sensitivity [41]. Thus overall, there is sufficient evidence to suggest that LXRs modulate key components of the metabolic syndrome.
LXR and chronic kidney disease
Nephropathy is a microvascular complication of diabetes mellitus and uncontrolled hypertension, leading to chronic kidney disease [112]. These, and other causes of chronic kidney disease, are major contributors to cardiac damage and are associated with an increased risk for cardiovascular disease [13, 117].
LXRs have been implicated as a renoprotective target, preserving intrinsic renal structure and function both basally and in diabetic nephropathy. A homeostatic role for LXRs in kidney function has been postulated. Lxrβ −/− mice exhibit polyuria and polydipsia, features of diabetes insipidus [42], and mice deficient for both LXRs display a renal phenotype analogous to diabetic nephropathy with elevations in albumin:creatinine ratio and glomerular lipid accumulation [99]. When challenged with diabetes, these mice demonstrated accelerated mesangial matrix expansion, increased glomerular lipid, and upregulation of inflammatory and oxidative stress markers [99].
In the kidney, expression levels of both LXRs are significantly decreased in animal models of type I diabetes [105] and in patients with diabetic nephropathy [87]. Studies conducted in several diabetic rodent models demonstrated that LXR activation with T09 and GW3965, as well as a new generation agonist, N,N-dimethyl-3β-hydroxycholenamide (DMHCA), prevented renal damage and dysfunction by reducing urinary albumin excretion and inhibiting macrophage infiltration, inflammation, and lipid accumulation [72, 99, 126]. Besides local renal effects, macrophage-derived LXR signaling is also pertinent in renal pathophysiology as transgenic LXRα overexpression in macrophages protected from hyperlipidemic-hyperglycemic nephropathy [72]. These findings suggest that LXRs play an important role in hyperglycemic-induced kidney disease. Whether LXRs affect hypertension-associated renal impairment remains to be established.
Local cardiac effects for LXRs
Relatively few studies have evaluated LXR signaling in the heart itself. Both LXRα and LXRβ are expressed in the heart where in comparison to the cardiomyocyte fraction, their expression levels are 10- to 15-fold higher in the non-myocytic fraction consisting of fibroblasts and endothelial cells [79]. In the heart, LXRs are induced and activated by myocardial infarction [51, 79], chronic pressure overload [17, 139], myocarditis [98], and diabetes [25, 52], indicating that LXRs are regulated in cardiac (patho)physiology. Here, we review current evidence regarding local cardiac effects for LXRs and the potential role of LXR signaling in the fundamental cellular processes governing cardiac remodeling, including cardiomyocyte hypertrophy and death, fibrosis, and metabolic and vascular remodeling (Fig. 3).
Cardiac effects of liver X receptor signaling. In the ischemic or hypertrophic myocardium, LXRs decrease cardiomyocyte hypertrophy and loss (death), as well as attenuate fibrotic remodeling. LXRs also modulate myocardial metabolism, and have regulatory functions in angiogenesis and neovascularization. LXRs are also expressed in macrophages, which can affect the myocardium through injury or disease. NFκB, nuclear factor kappa B; VEGF, vascular endothelial growth factor
Cardiomyocyte hypertrophy
Cardiomyocytes are non-proliferative, therefore they respond to pathophysiological stimuli through hypertrophic growth in order to reduce ventricular wall stress and augment contractile function. Increases in mechanical load as well as various neurohumoral signals such as catecholamines, growth factors, cytokines, and vasoactive peptides, activate a cascade of signal transduction pathways within the myocyte that orchestrates transcriptional reprogramming and posttranslational modification of protein synthesis and growth, as well as reactivation of fetal contractile and metabolic gene expression (fetal gene program). Initially, these adaptations are compensatory and considered protective, but with unremitted stress, become maladaptive and yield to pathological concentric or eccentric growth.
Several lines of evidence suggest an important role for LXRα in regulating hypertrophic cardiac remodeling. First, from in vitro experiments, LXR agonists have been shown to decrease cellular hypertrophy induced by diverse hypertrophic stimuli such as Ang II and lipopolysaccharides [139], endothelin-1 [75], and phenylephrine [17], whereas knockdown of LXRα in cardiomyocytes led to increased cellular growth [17]. Second, LXRα protein abundance is markedly upregulated in the pressure overloaded myocardium [17, 139]. Third, murine hearts deficient for LXRα demonstrate an exacerbated hypertrophic response to chronic pressure overload induced via transverse aortic constriction (TAC) [139], whereas the LXR agonists T09 and AZ876 attenuate hypertrophy in wild-type mice [17, 75], but not in LXRα-null mice [75]. Finally, the effect of LXRα on cardiac hypertrophy is heart-specific and independent of confounding systemic effects attributed to either T09 activation, which are lipogenic [102], anti-inflammatory [142], and blood pressure-lowering [75] effects, or residual effects from whole-body LXRα deletion [73]. Cardiac-specific LXRα overexpression in transgenic mice protected the heart from TAC-induced pressure overload and Ang II stimulation by attenuating LV hypertrophy and preventing cardiac dysfunction, in both the early and later phases of LV remodeling [16]. Taken together, these findings suggest a cell-specific role for LXRs in cardiomyocyte hypertrophy and are supported by pharmacological and genetic studies.
The molecular basis for the antagonistic actions of LXRα on pathological hypertrophic growth has been elucidated. In cardiomyocytes, suppressed pro-inflammatory NFκB signaling was found to be operative in T09-mediated decreases in cellular growth [139]. There are, however, various stages in the development of pathological cardiac hypertrophy, and the induction of an inflammatory response is only an early manifestation of this progression. Further evidence indicates that, in the intermediate phase of hypertrophy prior to decompensation and heart failure, the cardioprotective effects of LXRα may involve transcriptional regulation of myocardial glucose metabolism in the adaptation to hypertrophic stress. Mice with cardiac LXRα overexpression display an endogenous protective phenotype evidenced by enhanced myocardial glucose uptake that is linked to induction of potent anti-hypertrophic effectors, ANP and BNP. Specifically, increases in glucose flux activate the hexosamine biosynthetic pathway, which leads to downstream posttranslational O-GlcNAcylation of transcription factors of natriuretic peptides, GATA4 and Mef2c, potentiating their activities [16].
Cardiomyocyte death
Loss of cardiomyocytes is crucial in the pathogenesis of myocardial infarction, ischemia/reperfusion (I/R), and heart failure. Since cardiomyocytes are terminally differentiated and generally incapable of replicating in the adult heart, their survival is critical for maintaining myocardial viability. Cell death arises when blood supply to the myocardium is disrupted by coronary occlusion. Ensuing hypoxic and ischemic stimuli increase ROS production which triggers necrosis and apoptosis.
Recently, a role for LXR in apoptosis has been evaluated in the infarcted heart. LXR agonist treatment decreased infarct size and improved LV contractile function in murine hearts subjected to global I/R injury, and prevented hypoxia-reoxygenation-induced apoptosis by attenuating caspase 3 [79]. Furthermore, LXRα, but not LXRβ, was identified as the predominant isoform in the protection against acute and chronic I/R injury, which was associated with significant reductions in post-ischemic myocardial apoptosis. These infarct-sparing effects occurred via inhibition of endoplasmic reticulum stress- and mitochondria-mediated apoptotic pathways through targeting of caspases 12 and 9, respectively [51]. In an alternative therapeutic approach for cardiac repair following myocardial infarction, the combined therapy of the LXR agonist T09 and adipose-derived mesenchymal stem cells (AD-MSCs) transplanted into infarcted hearts inhibited host cardiomyocyte apoptosis and improved cardiac function, while T09 further improved the survival of AD-MSCs under hypoxic conditions [135]. Altogether, these findings are consistent with other studies demonstrating protective effects for LXRs in ischemic models of intestinal and brain injury, although the mechanisms underpinning LXR efficacy in these studies are linked to suppressed pro-inflammatory NFκB signaling [23, 31, 118].
LXRs have also been shown to regulate cell survival through inhibition of ROS production and oxidative stress [47, 121], as well as prevent apoptosis induced by hyperglycemia [24] and diabetes [52]. Interestingly, the anti-apoptotic factor AIM, also known as apoptosis inhibitor 6 or Spα, is a direct target gene for regulation by LXRα [62], which serves to protect macrophages from the apoptotic effects of oxidized lipids. Moreover, macrophages are essential for wound healing following myocardial infarction as they are the primary initiators of phagocytosis of the apoptotic cell. The inability to clear apoptotic cells is pro-inflammatory, and LXR signaling has been demonstrated to play an important role in apoptotic cell clearance and enhanced macrophage phagocytosis [1, 107]. In summary, LXRs may modulate critical facets of cellular death pathways in the ischemic and infarcted myocardium.
Fibrosis
Cardiac fibrosis is central in the pathogenesis of heart failure and is a major constituent in LV remodeling resulting from myocardial infarction and chronic pressure overload. With myocardial infarction, cardiomyocyte loss is resolved by cardiac fibroblasts, which initiate wound healing through replacement fibrosis to form a scar resilient in preventing ventricular rupture. Fibrosis that develops from pressure overload and in remote regions after myocardial infarction is termed reactive fibrosis. This form of fibrosis interferes not only with transduction of electrical impulses and contractile force in myocytes, but impedes diastolic relaxation through increased myocardial stiffness. In response to pathological stimuli, fibroblasts proliferate and differentiate into myofibroblasts, which contract and secrete collagens. Increased collagen deposition as well as changes in the balance of proteins regulating extracellular matrix turnover disrupt normal matricellular architecture. To date, there are no therapeutic strategies that specifically target fibrogenesis in the heart.
LXR agonists exhibit anti-proliferative properties as demonstrated in pancreatic β-cells [90], smooth muscle cells [11, 37], lymphocytes [9], and cancer cells [28]. Both LXRs are expressed in cardiac fibroblasts, and thus in the heart, they may potentially reduce expansion of the fibroblast population in LV remodeling. LXR activation with the novel agonist AZ876 resulted in both suppressed myofibroblast conversion and the prevention of Ang II- and transforming growth factor β (TGFβ)-induced collagen synthesis [17]. Further, in murine models of chronic pressure overload and diabetes, LXR agonism has been shown to oppose increases in myocardial fibrosis and pro-fibrotic gene expression in conjunction with improved diastolic function [17, 52]. Cardiac-specific LXRα overexpression also exerts anti-fibrotic effects and lowers fibrotic gene expression [16]. These observations are in accordance with other studies demonstrating anti-fibrotic effects of LXRs in liver injury [8], diabetic nephropathy [72, 126], and experimental skin fibrosis [10]. The latter two findings are associated with the interference of LXR ligands in macrophage infiltration and release of cytokines. Given that multiple co-morbidities contribute to a sustained pro-inflammatory state particularly evident in HFpEF [136], these effects on macrophage activity and fibrosis are of clinical relevance. Also of note, LXRs have been reported to downregulate matrix metallopeptidase MMP9 via repressed NFκB signaling [19], suggesting a role for macrophagic LXRs in regulation of extracellular matrix turnover.
LXRs may counteract pro-fibrotic signaling in the heart by affecting key intracellular pathways. For example, Ang II signaling promotes fibroblast proliferation and extracellular matrix formation through AT1 receptor-dependent activation. Several studies have demonstrated downregulation of AT1R by LXR agonism [57, 76, 80] through dephosphorylation of the transcription factor, Sp1 [57]. TGFβ is another central mediator of multiple inflammatory and fibrotic cellular responses in cardiac remodeling [38]. A crosstalk between LXRs and TGFβ signaling via interaction with the co-activator RAP250 and Smad2/3 has been determined [3]. Furthermore, LXR agonism has been shown to attenuate TGFβ and downstream Smad2/3 expression in hypertrophied murine hearts [17], which is consistent with their activation in other diseased states such as diabetes-induced renal fibrosis [126] and chronic asthma-induced airway remodeling [116]. These findings altogether implicate a role for LXRs in fibrogenesis, raising the possibility that they may serve as a protective target in the prevention of fibrosis in cardiac remodeling.
Metabolic remodeling
The heart is a highly metabolic organ requiring continuous replenishment of its cellular ATP stores to support sarcomeric contraction and relaxation as well as functioning of membrane transport systems. The demand for energy is supplied primarily through oxidation of fatty acids, but also glucose and to a lesser extent lactate, ketones, and amino acids. However, pathological states trigger alterations in myocardial substrate utilization in order to maximize energy efficiency through reciprocal downregulation of fatty acid oxidation and enhanced glucose reliance. As heart failure progresses, myocardial metabolism in maladaptive as oxygen and substrate supply are decreased and energy transfer is impaired, resulting in mitochondrial dysfunction and inefficient energy utilization. In essence, the failing heart becomes “an engine out of fuel” [95] as energy production is inadequate to support cardiac output.
Promoting the shift towards increased glucose reliance has been postulated to improve myocardial efficiency in heart failure, preventing energy depletion [5, 61]. LXRα has been implicated in the transcriptional regulation of cardiac glucose metabolism and orchestration of an adaptive metabolic response to hypertrophic stress. Constitutive LXRα overexpression in isolated cardiomyocytes and murine hearts induced Glut1 and Glut4 expression and increased the capacity for glucose uptake and utilization. Furthermore, mice deficient for LXRα display impaired myocardial glucose uptake in response to hypertrophic perturbation, whereas glucose levels are substantially enhanced with cardiac LXRα overexpression in the protection against cardiac dysfunction [16]. Interestingly, LXRα has also been shown to improve long-term cardiac performance following chronic I/R injury that is evidenced in part by preserved glucose uptake [51], an indicator of myocardial viability in this setting. Whether preservation of glucose uptake was a direct effect of LXRα on glucose metabolism, or secondary to reduced infarct size was not established herein. In contrast, lipid droplet accumulation has been observed following treatment with the LXR agonist GW3965, which associated with improved tolerance to acute myocardial ischemia [79]. At the onset of I/R there is increased availability and usage of fatty acids [66]. However, the role of lipids in the heart remains controversial as it may lead to lipotoxicity and dysfunction [97]. Glucose pathways were not assessed in this study and therefore cannot be precluded as a protective mechanism against acute myocardial infarction.
Targeting LXRα to promote cellular glucose uptake may indeed be advantageous under conditions where glucose uptake is compromised. For example, insulin resistance is highly prevalent in the diabetic and heart failure population and can impair the shift to glucose reliance [13, 93, 138]. LXRα may therefore serve as an important tool in sensitizing the heart to glucose under these conditions. Recently, LXR agonism has been shown to protect against diabetic cardiomyopathy in db/db mice, although the effects on cardiac metabolism were not investigated in this study [52]. An alternative investigation in mice overexpressing cardiac LXRα revealed that the elevated capacity for myocardial glucose uptake is sustained despite obesity-induced systemic insulin resistance and hypertriglyceridemia (Cannon et al., unpublished data), stimuli that impede the capacity for glucose uptake. Overall, LXRs represent a potential metabolic modulator for optimization of myocardial substrate utilization in cardiac pathophysiology.
Angiogenesis
Endothelial dysfunction involves a range of endothelial cell functions that become dysregulated, including impaired angiogenic responses that are crucial in salvaging the infarcted and hypertrophic myocardium [35]. In HFrEF, new microvascular networks are necessary for improving regional perfusion after ischemic injury. In HFpEF, muscle-to-capillary ratio is reduced in pathologically hypertrophied hearts, which causes myocardial hypoxia and contractile dysfunction through compromised oxygen and nutrient delivery that is necessary for growth. The aim of cardiovascular therapies is to stimulate angiogenesis within the myocardium to prevent or reverse heart failure.
The angiogenic potential of LXRs has been established in the ischemic rat brain [118] and following stroke [21]. LXRs promote angiogenesis by directly regulating VEGF [134]. Murine and human Vegfa genes harbor a functional LXRE in the promoter region, and regulation occurs independent of the hypoxia response element for HIF-1 [134]. However, several studies provide evidence for an anti-angiogenic (yet protective) role for LXRs in settings of uncontrolled angiogenesis such as in tumor growth [96] and cancer [36, 104]. Whether LXRs stimulate angiogenesis in either the ischemic or hypertrophic myocardium remains to be determined.
LXRs may also regulate angiogenesis through modulation of cholesterol. Cholesterol promotes lipid raft formation in the plasma membrane from where cell surface receptors initiate signaling events that lead to angiogenesis [40]. Since excess cholesterol or its removal determines the balance between either promoting or inhibiting angiogenesis, this balance may arguably be regulated by LXRs given their antagonistic actions on increasing HDL cholesterol [113] and stimulating cholesterol efflux via the RCT [94]. These data implicate a role for LXR in angiogenesis and suggest that LXRs may prevent tissue hypoxia, either through directly targeting VEGF or through modulation of cholesterol.
Conclusions
Heart failure is a complex clinical syndrome, and co-morbidities such as hypertension, diabetes, and kidney and vascular disease, including atherosclerosis, are increasingly recognized for their provocation of this disease. Left untreated, these co-morbidities accelerate the progression of adverse myocardial remodeling which results in impaired cardiac function, eventually leading to heart failure and death. The optimal window for therapeutic modulation likely occurs in the early phase when cardiac remodeling is largely reversible. Since systemic LXR activation may exert many roles in the pathogenesis of the aforementioned co-morbidities, targeting of LXRs during this phase may serve as a useful addendum in preventing remodeling progression. In addition, accumulating evidence implicates intracardiac LXR signaling in the protection against pathological processes involving myocyte hypertrophy and loss, fibrosis, and metabolism. However, translation of basic findings to clinical settings requires additional studies to further elucidate the role of LXRs in the heart. In the presence of multiple co-morbidities, the collective impact of systemic LXR activation on preserving myocardial integrity and function warrants further address.
Thus far, only few data exist on the role of LXR signaling in humans. In a human genetic study, analysis of the LXR gene sequence in patients afflicted with coronary artery disease revealed mutations in the ligand-binding domain of LXRα that altered its conformation, rendering LXRα inept in binding its ligands [34]. This suggests that humans having a mutated LXRα gene may develop a predisposition towards coronary artery disease. In further support of this, an LXRα gene polymorphism was found to be related with increased susceptibility of coronary artery disease in Chinese Han population [144]. Genetic variation in the LXRα-encoding gene NR1H3 has been associated with increased risk of ischemic vascular disease [123], as well as LV hypertrophy (Van der Harst et al., unpublished data), obesity [32, 110], longevity [91], and the metabolic syndrome [78], although another study was not able to validate the latter [110]. Polymorphisms in the NR1H2 gene encoding LXRβ mainly associated with obesity and type 2 diabetes [32, 70, 119]. Interestingly, the LXR signaling pathway was recently found to be highly enriched among pleiotropic genes that emerged from cardiovascular disease risk factor clustering, and for coronary artery disease [106], supporting the notion that the LXR pathway may affect many cardiometabolic traits.
Future perspectives
Testing of high affinity agonists specific for LXRs are needed to further evaluate the potential of LXR activation in human disease, and provide more appreciable insight into their therapeutic prospective [55]. To date, only one clinical study has been published for the LXR agonist, LXR-623, which activated LXRs without causing hepatic lipogenesis. However, this clinical trial was prematurely halted due to adverse neurological side effects in subjects tested [69]. Nevertheless, several other LXR agonists are in development and natural modulators of LXR activity are also being considered for their potential as nutraceuticals for therapy [56]. Recently, a novel partial, LXRβ-selective agonist, BMS-779788, has been shown to display an improved plasma lipid profile compared with a dual agonist in a cynomolgus monkey model, while inducing genes that enhance the RCT [71]. Indeed, much of the current interest in developing new generation compounds is channeled towards designing LXRβ-specific ligands that target induction of the RCT pathway and circumvent the hepatic lipogenic signaling pathways mediated by LXRα. However, in the heart, there is mounting evidence to suggest that LXRα is the predominant isoform in the protection against distinct myocardial pathologies related to ischemia [51], pathological hypertrophy [16, 17, 139], and diabetic cardiomyopathy [25]. Ideally, a tissue-selective LXR agonist with high affinities for cardiac LXRα may be more suitable for treating myocardial disease. A strategy to exclusively target LXRα pathways in a given cell, or tissue, such as in the heart, is to modulate the LXR co-regulatory transcriptional complex, which impacts its DNA-binding and transcriptional activity [2, 53, 132]. Hence, a greater understanding of the co-factor profile recruited to regulate LXRα in the normal and diseased heart may aid in this development.
In perspective, bridging the gap between preclinical studies and a clinically viable therapeutic strategy most likely lies in the development of highly specific and selective LXR ligands that minimize lipogenic and neurological side effects, and are well tolerated in clinical trials. Given the global salutary effects of LXR activation in cardiovascular disease and its precursors, atherosclerosis, hypertension, diabetes, and inflammation, we postulate that effective and successful targeting of LXRs holds promise for future therapies.
References
Agonzalez N, Bensinger SJ, Hong C, Beceiro S, Bradley MN, Zelcer N, Deniz J, Ramirez C, Diaz M, Gallardo G, de Galarreta CR, Salazar J, Lopez F, Edwards P, Parks J, Andujar M, Tontonoz P, Castrillo A (2009) Apoptotic cells promote their own clearance and immune tolerance through activation of the nuclear receptor LXR. Immunity 31:245–258. doi:10.1016/j.immuni.2009.06.018
Albers M, Blume B, Schlueter T, Wright MB, Kober I, Kremoser C, Deuschle U, Koegl M (2006) A novel principle for partial agonism of liver X receptor ligands. Competitive recruitment of activators and repressors. J Biol Chem 281:4920–4930 (M510101200 [pii])
Antonson P, Jakobsson T, Almlof T, Guldevall K, Steffensen KR, Gustafsson JA (2008) RAP250 is a coactivator in the transforming growth factor beta signaling pathway that interacts with Smad2 and Smad3. J Biol Chem 283:8995–9001. doi:10.1074/jbc.M707203200
Apfel R, Benbrook D, Lernhardt E, Ortiz MA, Salbert G, Pfahl M (1994) A novel orphan receptor specific for a subset of thyroid hormone-responsive elements and its interaction with the retinoid/thyroid hormone receptor subfamily. Mol Cell Biol 14:7025–7035
Ashrafian H, Frenneaux MP, Opie LH (2007) Metabolic mechanisms in heart failure. Circulation 116:434–448 (116/4/434 [pii])
Baranowski M, Zabielski P, Blachnio-Zabielska AU, Harasim E, Chabowski A, Gorski J (2014) Insulin-sensitizing effect of LXR agonist T0901317 in high-fat fed rats is associated with restored muscle GLUT4 expression and insulin-stimulated AS160 phosphorylation. Cell Physiol Biochem 33:1047–1057. doi:10.1159/000358675
Beaven SW, Matveyenko A, Wroblewski K, Chao L, Wilpitz D, Hsu TW, Lentz J, Drew B, Hevener AL, Tontonoz P (2013) Reciprocal regulation of hepatic and adipose lipogenesis by liver X receptors in obesity and insulin resistance. Cell Metab 18:106–117. doi:10.1016/j.cmet.2013.04.021
Beaven SW, Wroblewski K, Wang J, Hong C, Bensinger S, Tsukamoto H, Tontonoz P (2011) Liver X receptor signaling is a determinant of stellate cell activation and susceptibility to fibrotic liver disease. Gastroenterology 140:1052–1062. doi:10.1053/j.gastro.2010.11.053
Bensinger SJ, Bradley MN, Joseph SB, Zelcer N, Janssen EM, Hausner MA, Shih R, Parks JS, Edwards PA, Jamieson BD, Tontonoz P (2008) LXR signaling couples sterol metabolism to proliferation in the acquired immune response. Cell 134:97–111. doi:10.1016/j.cell.2008.04.052
Beyer C, Huang J, Beer J, Zhang Y, Palumbo-Zerr K, Zerr P, Distler A, Dees C, Maier C, Munoz L, Kronke G, Uderhardt S, Distler O, Jones S, Rose-John S, Oravecz T, Schett G, Distler JH (2014) Activation of liver X receptors inhibits experimental fibrosis by interfering with interleukin-6 release from macrophages. Ann Rheum Dis. doi:10.1136/annrheumdis-2013-204401
Blaschke F, Leppanen O, Takata Y, Caglayan E, Liu J, Fishbein MC, Kappert K, Nakayama KI, Collins AR, Fleck E, Hsueh WA, Law RE, Bruemmer D (2004) Liver X receptor agonists suppress vascular smooth muscle cell proliferation and inhibit neointima formation in balloon-injured rat carotid arteries. Circ Res 95:e110–e123 (01.RES.0000150368.56660.4f [pii])
Bories G, Colin S, Vanhoutte J, Derudas B, Copin C, Fanchon M, Daoudi M, Belloy L, Haulon S, Zawadzki C, Jude B, Staels B, Chinetti-Gbaguidi G (2013) Liver X receptor activation stimulates iron export in human alternative macrophages. Circ Res 113:1196–1205. doi:10.1161/CIRCRESAHA.113.301656
Brouwers FP, de Boer RA, van der Harst P, Voors AA, Gansevoort RT, Bakker SJ, Hillege HL, van Veldhuisen DJ, van Gilst WH (2013) Incidence and epidemiology of new onset heart failure with preserved vs. reduced ejection fraction in a community-based cohort: 11-year follow-up of PREVEND. Eur Heart J 34:1424–1431. doi:10.1093/eurheartj/eht066
Burchfield JS, Xie M, Hill JA (2013) Pathological ventricular remodeling: mechanisms: part 1 of 2. Circulation 128:388–400. doi:10.1161/CIRCULATIONAHA.113.001878
Calkin AC, Tontonoz P (2010) Liver x receptor signaling pathways and atherosclerosis. Arterioscler Thromb Vasc Biol 30:1513–1518. doi:10.1161/ATVBAHA.109.191197
Cannon MV, Sillje HH, Sijbesma JW, Vreeswijk-Baudoin I, Ciapaite J, van der Sluis B, van Deursen J, Silva GJ, de Windt LJ, Gustafsson JA, van der Harst P, van Gilst WH, de Boer RA (2015) Cardiac LXRalpha protects against pathological cardiac hypertrophy and dysfunction by enhancing glucose uptake and utilization. EMBO Mol Med 7:1229–1243. doi:10.15252/emmm.201404669
Cannon MV, Yu H, Candido WM, Dokter MM, Lindstedt EL, Sillje HH, van Gilst WH, de Boer RA (2015) The liver X receptor agonist AZ876 protects against pathological cardiac hypertrophy and fibrosis without lipogenic side effects. Eur J Heart Fail 17:273–282. doi:10.1002/ejhf.243
Cao G, Liang Y, Broderick CL, Oldham BA, Beyer TP, Schmidt RJ, Zhang Y, Stayrook KR, Suen C, Otto KA, Miller AR, Dai J, Foxworthy P, Gao H, Ryan TP, Jiang XC, Burris TP, Eacho PI, Etgen GJ (2003) Antidiabetic action of a liver x receptor agonist mediated by inhibition of hepatic gluconeogenesis. J Biol Chem 278:1131–1136. doi:10.1074/jbc.M210208200
Castrillo A, Joseph SB, Marathe C, Mangelsdorf DJ, Tontonoz P (2003) Liver X receptor-dependent repression of matrix metalloproteinase-9 expression in macrophages. J Biol Chem 278:10443–10449. doi:10.1074/jbc.M213071200
Cha JY, Repa JJ (2007) The liver X receptor (LXR) and hepatic lipogenesis. The carbohydrate-response element-binding protein is a target gene of LXR. J Biol Chem 282:743–751 (M605023200 [pii])
Chen J, Cui X, Zacharek A, Roberts C, Chopp M (2009) eNOS mediates TO90317 treatment-induced angiogenesis and functional outcome after stroke in mice. Stroke 40:2532–2538. doi:10.1161/STROKEAHA.108.545095
Chen J, Zhao L, Sun D, Narsinh K, Li C, Zhang Z, Qi S, Wei G, Li W, Guo W, Cao F (2012) Liver X receptor activation attenuates plaque formation and improves vasomotor function of the aortic artery in atherosclerotic ApoE(-/-) mice. Inflamm Res 61:1299–1307. doi:10.1007/s00011-012-0529-4
Cheng O, Ostrowski RP, Liu W, Zhang JH (2010) Activation of liver X receptor reduces global ischemic brain injury by reduction of nuclear factor-kappaB. Neuroscience 166:1101–1109. doi:10.1016/j.neuroscience.2010.01.024
Cheng Y, Feng Y, Zhu M, Yan B, Fu S, Guo J, Hu J, Song X, Guo S, Liu G (2014) Synthetic liver X receptor agonist T0901317 attenuates high glucose-induced oxidative stress, mitochondrial damage and apoptosis in cardiomyocytes. Acta Histochem 116:214–221. doi:10.1016/j.acthis.2013.07.007
Cheng Y, Liu G, Pan Q, Guo S, Yang X (2011) Elevated expression of liver X receptor alpha (LXRalpha) in myocardium of streptozotocin-induced diabetic rats. Inflammation 34:698–706. doi:10.1007/s10753-010-9281-5
Chisholm JW, Hong J, Mills SA, Lawn RM (2003) The LXR ligand T0901317 induces severe lipogenesis in the db/db diabetic mouse. J Lipid Res 44:2039–2048. doi:10.1194/jlr.M300135-JLR200
Choe SS, Choi AH, Lee JW, Kim KH, Chung JJ, Park J, Lee KM, Park KG, Lee IK, Kim JB (2007) Chronic activation of liver X receptor induces beta-cell apoptosis through hyperactivation of lipogenesis: liver X receptor-mediated lipotoxicity in pancreatic beta-cells. Diabetes 56:1534–1543 (db06-1059 [pii])
Chuu CP, Lin HP (2010) Antiproliferative effect of LXR agonists T0901317 and 22(R)-hydroxycholesterol on multiple human cancer cell lines. Anticancer Res 30:3643–3648 (30/9/3643 [pii])
Commerford SR, Vargas L, Dorfman SE, Mitro N, Rocheford EC, Mak PA, Li X, Kennedy P, Mullarkey TL, Saez E (2007) Dissection of the insulin-sensitizing effect of liver X receptor ligands. Mol Endocrinol 21:3002–3012 (me.2007-0156 [pii])
Cozzone D, Debard C, Dif N, Ricard N, Disse E, Vouillarmet J, Rabasa-Lhoret R, Laville M, Pruneau D, Rieusset J, Lefai E, Vidal H (2006) Activation of liver X receptors promotes lipid accumulation but does not alter insulin action in human skeletal muscle cells. Diabetologia 49:990–999. doi:10.1007/s00125-006-0140-8
Crisafulli C, Di Paola R, Mazzon E, Paterniti I, Galuppo M, Genovese T, Bramanti P, Cappellani A, Cuzzocrea S (2010) Liver X receptor agonist treatment reduced splanchnic ischemia and reperfusion injury. J Leukoc Biol 87:309–321. doi:10.1189/jlb.0609438
Dahlman I, Nilsson M, Jiao H, Hoffstedt J, Lindgren CM, Humphreys K, Kere J, Gustafsson JA, Arner P, Dahlman-Wright K (2006) Liver X receptor gene polymorphisms and adipose tissue expression levels in obesity. Pharmacogenet Genomics 16:881–889. doi:10.1097/01.fpc.0000236334.49422.48
Dalen KT, Ulven SM, Bamberg K, Gustafsson JA, Nebb HI (2003) Expression of the insulin-responsive glucose transporter GLUT4 in adipocytes is dependent on liver X receptor alpha. J Biol Chem 278:48283–48291. doi:10.1074/jbc.M302287200
Dave VP, Kaul D, Sharma Y, Bhattacharya R (2009) Functional genomics of blood cellular LXR-alpha gene in human coronary heart disease. J Mol Cell Cardiol 46:536–544. doi:10.1016/j.yjmcc.2008.12.020
De Boer RA, Pinto YM, Van Veldhuisen DJ (2003) The imbalance between oxygen demand and supply as a potential mechanism in the pathophysiology of heart failure: the role of microvascular growth and abnormalities. Microcirculation 10:113–126. doi:10.1038/sj.mn.7800188
De Boussac H, Alioui A, Viennois E, Dufour J, Trousson A, Vega A, Guy L, Volle DH, Lobaccaro JM, Baron S (2013) Oxysterol receptors and their therapeutic applications in cancer conditions. Expert Opin Ther Targets 17:1029–1038. doi:10.1517/14728222.2013.820708
Delvecchio CJ, Bilan P, Radford K, Stephen J, Trigatti BL, Cox G, Parameswaran K, Capone JP (2007) Liver X receptor stimulates cholesterol efflux and inhibits expression of proinflammatory mediators in human airway smooth muscle cells. Mol Endocrinol 21:1324–1334 (me.2007-0017 [pii])
Dobaczewski M, Chen W, Frangogiannis NG (2011) Transforming growth factor (TGF)-beta signaling in cardiac remodeling. J Mol Cell Cardiol 51:600–606. doi:10.1016/j.yjmcc.2010.10.033
Efanov AM, Sewing S, Bokvist K, Gromada J (2004) Liver X receptor activation stimulates insulin secretion via modulation of glucose and lipid metabolism in pancreatic beta-cells. Diabetes 53(Suppl 3):S75–S78 (53/suppl_3/S75 [pii])
Fang L, Choi SH, Baek JS, Liu C, Almazan F, Ulrich F, Wiesner P, Taleb A, Deer E, Pattison J, Torres-Vazquez J, Li AC, Miller YI (2013) Control of angiogenesis by AIBP-mediated cholesterol efflux. Nature 498:118–122. doi:10.1038/nature12166
Fernandez-Veledo S, Vila-Bedmar R, Nieto-Vazquez I, Lorenzo M (2009) c-Jun N-terminal kinase 1/2 activation by tumor necrosis factor-alpha induces insulin resistance in human visceral but not subcutaneous adipocytes: reversal by liver X receptor agonists. J Clin Endocrinol Metab 94:3583–3593. doi:10.1210/jc.2009-0558
Gabbi C, Kong X, Suzuki H, Kim HJ, Gao M, Jia X, Ohnishi H, Ueta Y, Warner M, Guan Y, Gustafsson JA (2012) Central diabetes insipidus associated with impaired renal aquaporin-1 expression in mice lacking liver X receptor beta. Proc Natl Acad Sci USA 109:3030–3034. doi:10.1073/pnas.1200588109
Galderisi M, Anderson KM, Wilson PW, Levy D (1991) Echocardiographic evidence for the existence of a distinct diabetic cardiomyopathy (the Framingham Heart Study). Am J Cardiol 68:85–89 (0002-9149(91)90716-X [pii])
Gerin I, Dolinsky VW, Shackman JG, Kennedy RT, Chiang SH, Burant CF, Steffensen KR, Gustafsson JA, MacDougald OA (2005) LXRbeta is required for adipocyte growth, glucose homeostasis, and beta cell function. J Biol Chem 280:23024–23031 (M412564200 [pii])
Geyeregger R, Zeyda M, Stulnig TM (2006) Liver X receptors in cardiovascular and metabolic disease. Cell Mol Life Sci 63:524–539. doi:10.1007/s00018-005-5398-3
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB, American Heart Association Statistics Committee and Stroke Statistics Subcommittee (2014) Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation 129:e28–e292. doi:10.1161/01.cir.0000441139.02102.80
Gong H, He J, Lee JH, Mallick E, Gao X, Li S, Homanics GE, Xie W (2009) Activation of the liver X receptor prevents lipopolysaccharide-induced lung injury. J Biol Chem 284:30113–30121. doi:10.1074/jbc.M109.047753
Grefhorst A, van Dijk TH, Hammer A, van der Sluijs FH, Havinga R, Havekes LM, Romijn JA, Groot PH, Reijngoud DJ, Kuipers F (2005) Differential effects of pharmacological liver X receptor activation on hepatic and peripheral insulin sensitivity in lean and ob/ob mice. Am J Physiol Endocrinol Metab 289:E829–E838 (00165.2005 [pii])
Hayashi T, Kotani H, Yamaguchi T, Taguchi K, Iida M, Ina K, Maeda M, Kuzuya M, Hattori Y, Ignarro LJ (2014) Endothelial cellular senescence is inhibited by liver X receptor activation with an additional mechanism for its atheroprotection in diabetes. Proc Natl Acad Sci USA 111:1168–1173. doi:10.1073/pnas.1322153111
Hazra S, Rasheed A, Bhatwadekar A, Wang X, Shaw LC, Patel M, Caballero S, Magomedova L, Solis N, Yan Y, Wang W, Thinschmidt JS, Verma A, Li Q, Levi M, Cummins CL, Grant MB (2012) Liver X receptor modulates diabetic retinopathy outcome in a mouse model of streptozotocin-induced diabetes. Diabetes 61:3270–3279. doi:10.2337/db11-1596
He Q, Pu J, Yuan A, Lau WB, Gao E, Koch WJ, Ma XL, He B (2014) Activation of liver-x-receptor alpha but not liver-x-receptor beta protects against myocardial ischemia/reperfusion injury. Circ Heart Fail 7:1032–1041. doi:10.1161/CIRCHEARTFAILURE.114.001260
He Q, Pu J, Yuan A, Yao T, Ying X, Zhao Y, Xu L, Tong H, He B (2014) Liver X receptor agonist treatment attenuates cardiac dysfunction in type 2 diabetic db/db mice. Cardiovasc Diabetol 13:149 (s12933-014-0149-0 [pii])
Herzog B, Hallberg M, Seth A, Woods A, White R, Parker MG (2007) The nuclear receptor cofactor, receptor-interacting protein 140, is required for the regulation of hepatic lipid and glucose metabolism by liver X receptor. Mol Endocrinol 21:2687–2697 (me.2007-0213 [pii])
Heusch G, Libby P, Gersh B, Yellon D, Bohm M, Lopaschuk G, Opie L (2014) Cardiovascular remodelling in coronary artery disease and heart failure. Lancet 383:1933–1943. doi:10.1016/S0140-6736(14)60107-0
Hong C, Tontonoz P (2014) Liver X receptors in lipid metabolism: opportunities for drug discovery. Nat Rev Drug Discov 13:433–444. doi:10.1038/nrd4280
Huang C (2014) Natural modulators of liver X receptors. J Integr Med 12:76–85 (S2095-4964(14)60013-3 [pii])
Imayama I, Ichiki T, Patton D, Inanaga K, Miyazaki R, Ohtsubo H, Tian Q, Yano K, Sunagawa K (2008) Liver X receptor activator downregulates angiotensin II type 1 receptor expression through dephosphorylation of Sp1. Hypertension 51:1631–1636. doi:10.1161/HYPERTENSIONAHA.107.106963
Ingelsson E, Sundstrom J, Arnlov J, Zethelius B, Lind L (2005) Insulin resistance and risk of congestive heart failure. JAMA 294:334–341 (294/3/334 [pii])
Jakobsson T, Treuter E, Gustafsson JA, Steffensen KR (2012) Liver X receptor biology and pharmacology: new pathways, challenges and opportunities. Trends Pharmacol Sci 33:394–404. doi:10.1016/j.tips.2012.03.013
Janowski BA, Willy PJ, Devi TR, Falck JR, Mangelsdorf DJ (1996) An oxysterol signalling pathway mediated by the nuclear receptor LXR alpha. Nature 383:728–731. doi:10.1038/383728a0
Jaswal JS, Keung W, Wang W, Ussher JR, Lopaschuk GD (2011) Targeting fatty acid and carbohydrate oxidation—a novel therapeutic intervention in the ischemic and failing heart. Biochim Biophys Acta 1813:1333–1350. doi:10.1016/j.bbamcr.2011.01.015
Joseph SB, Bradley MN, Castrillo A, Bruhn KW, Mak PA, Pei L, Hogenesch J, O’connell RM, Cheng G, Saez E, Miller JF, Tontonoz P (2004) LXR-dependent gene expression is important for macrophage survival and the innate immune response. Cell 119:299–309 (S0092867404009419 [pii])
Joseph SB, Castrillo A, Laffitte BA, Mangelsdorf DJ, Tontonoz P (2003) Reciprocal regulation of inflammation and lipid metabolism by liver X receptors. Nat Med 9:213–219. doi:10.1038/nm820
Joseph SB, McKilligin E, Pei L, Watson MA, Collins AR, Laffitte BA, Chen M, Noh G, Goodman J, Hagger GN, Tran J, Tippin TK, Wang X, Lusis AJ, Hsueh WA, Law RE, Collins JL, Willson TM, Tontonoz P (2002) Synthetic LXR ligand inhibits the development of atherosclerosis in mice. Proc Natl Acad Sci USA 99:7604–7609. doi:10.1073/pnas.112059299
Kalaany NY, Gauthier KC, Zavacki AM, Mammen PP, Kitazume T, Peterson JA, Horton JD, Garry DJ, Bianco AC, Mangelsdorf DJ (2005) LXRs regulate the balance between fat storage and oxidation. Cell Metab 1:231–244 (S1550-4131(05)00060-4 [pii])
Kantor PF, Dyck JR, Lopaschuk GD (1999) Fatty acid oxidation in the reperfused ischemic heart. Am J Med Sci 318:3–14
Kappus MS, Murphy AJ, Abramowicz S, Ntonga V, Welch CL, Tall AR, Westerterp M (2014) Activation of liver X receptor decreases atherosclerosis in Ldlr(-)/(-) mice in the absence of ATP-binding cassette transporters A1 and G1 in myeloid cells. Arterioscler Thromb Vasc Biol 34:279–284. doi:10.1161/ATVBAHA.113.302781
Kase ET, Wensaas AJ, Aas V, Hojlund K, Levin K, Thoresen GH, Beck-Nielsen H, Rustan AC, Gaster M (2005) Skeletal muscle lipid accumulation in type 2 diabetes may involve the liver X receptor pathway. Diabetes 54:1108–1115
Katz A, Udata C, Ott E, Hickey L, Burczynski ME, Burghart P, Vesterqvist O, Meng X (2009) Safety, pharmacokinetics, and pharmacodynamics of single doses of LXR-623, a novel liver X-receptor agonist, in healthy participants. J Clin Pharmacol 49:643–649. doi:10.1177/0091270009335768
Ketterer C, Mussig K, Machicao F, Stefan N, Fritsche A, Haring HU, Staiger H (2011) Genetic variation within the NR1H2 gene encoding liver X receptor beta associates with insulin secretion in subjects at increased risk for type 2 diabetes. J Mol Med (Berl) 89:75–81. doi:10.1007/s00109-010-0687-1
Kirchgessner TG, Martin R, Sleph P, Grimm D, Liu X, Lupisella J, Smalley J, Narayanan R, Xie Y, Ostrowski J, Cantor GH, Mohan R, Kick E (2015) Pharmacological Characterization of a Novel Liver X Receptor Agonist with Partial LXRalpha Activity and a Favorable Window in Nonhuman Primates. J Pharmacol Exp Ther 352:305–314. doi:10.1124/jpet.114.219923
Kiss E, Kranzlin B, Wagenblabeta K, Bonrouhi M, Thiery J, Grone E, Nordstrom V, Teupser D, Gretz N, Malle E, Grone HJ (2013) Lipid droplet accumulation is associated with an increase in hyperglycemia-induced renal damage: prevention by liver X receptors. Am J Pathol 182:727–741. doi:10.1016/j.ajpath.2012.11.033
Korach-Andre M, Archer A, Barros RP, Parini P, Gustafsson JA (2011) Both liver-X receptor (LXR) isoforms control energy expenditure by regulating brown adipose tissue activity. Proc Natl Acad Sci USA 108:403–408. doi:10.1073/pnas.1017884108
Korach-Andre M, Parini P, Larsson L, Arner A, Steffensen KR, Gustafsson JA (2010) Separate and overlapping metabolic functions of LXRalpha and LXRbeta in C57Bl/6 female mice. Am J Physiol Endocrinol Metab 298:E167–E178. doi:10.1152/ajpendo.00184.2009
Kuipers I, Li J, Vreeswijk-Baudoin I, Koster J, van der Harst P, Sillje HH, Kuipers F, van Veldhuisen DJ, van Gilst WH, de Boer RA (2010) Activation of liver X receptors with T0901317 attenuates cardiac hypertrophy in vivo. Eur J Heart Fail 12:1042–1050. doi:10.1093/eurjhf/hfq109;10.1093/eurjhf/hfq109
Kuipers I, van der Harst P, Kuipers F, van Genne L, Goris M, Lehtonen JY, van Veldhuisen DJ, van Gilst WH, de Boer RA (2010) Activation of liver X receptor-alpha reduces activation of the renal and cardiac renin-angiotensin-aldosterone system. Lab Invest 90:630–636. doi:10.1038/labinvest.2010.7
Laffitte BA, Chao LC, Li J, Walczak R, Hummasti S, Joseph SB, Castrillo A, Wilpitz DC, Mangelsdorf DJ, Collins JL, Saez E, Tontonoz P (2003) Activation of liver X receptor improves glucose tolerance through coordinate regulation of glucose metabolism in liver and adipose tissue. Proc Natl Acad Sci USA 100:5419–5424. doi:10.1073/pnas.0830671100
Legry V, Cottel D, Ferrieres J, Chinetti G, Deroide T, Staels B, Amouyel P, Meirhaeghe A (2008) Association between liver X receptor alpha gene polymorphisms and risk of metabolic syndrome in French populations. Int J Obes (Lond) 32:421–428. doi:10.1038/sj.ijo.0803705
Lei P, Baysa A, Nebb HI, Valen G, Skomedal T, Osnes JB, Yang Z, Haugen F (2013) Activation of Liver X receptors in the heart leads to accumulation of intracellular lipids and attenuation of ischemia-reperfusion injury. Basic Res Cardiol 108:323. doi:10.1007/s00395-012-0323-z
Leik CE, Carson NL, Hennan JK, Basso MD, Liu QY, Crandall DL, Nambi P (2007) GW3965, a synthetic liver X receptor (LXR) agonist, reduces angiotensin II-mediated pressor responses in Sprague-Dawley rats. Br J Pharmacol 151:450–456. doi:10.1038/sj.bjp.0707241
Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK (1996) The progression from hypertension to congestive heart failure. JAMA 275:1557–1562
Li G, Biju KC, Xu X, Zhou Q, Chen C, Valente AJ, He W, Reddick RL, Freeman GL, Ahuja SS, Clark RA, Li S (2011) Macrophage LXRalpha gene therapy ameliorates atherosclerosis as well as hypertriglyceridemia in LDLR(-/-) mice. Gene Ther 18:835–841. doi:10.1038/gt.2011.29
Li X, Song Y, Han Y, Wang D, Zhu Y (2012) Liver X receptor agonist alleviated high glucose-induced endothelial progenitor cell dysfunction via inhibition of reactive oxygen species and activation of AMP-activated protein kinase. Microcirculation 19:547–553. doi:10.1111/j.1549-8719.2012.00186.x
Liu Y, Yan C, Wang Y, Nakagawa Y, Nerio N, Anghel A, Lutfy K, Friedman TC (2006) Liver X receptor agonist T0901317 inhibition of glucocorticoid receptor expression in hepatocytes may contribute to the amelioration of diabetic syndrome in db/db mice. Endocrinology 147:5061–5068 (en.2006-0243 [pii])
Lund LH, Benson L, Dahlstrom U, Edner M (2012) Association between use of renin-angiotensin system antagonists and mortality in patients with heart failure and preserved ejection fraction. JAMA 308:2108–2117. doi:10.1001/jama.2012.14785
Lund LH, Benson L, Dahlstrom U, Edner M, Friberg L (2014) Association between use of beta-blockers and outcomes in patients with heart failure and preserved ejection fraction. JAMA 312:2008–2018. doi:10.1001/jama.2014.15241
Martini S, Eichinger F, Nair V, Kretzler M (2008) Defining human diabetic nephropathy on the molecular level: integration of transcriptomic profiles with biological knowledge. Rev Endocr Metab Disord 9:267–274. doi:10.1007/s11154-008-9103-3
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Bohm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez-Sanchez MA, Jaarsma T, Kober L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Ronnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A, ESC for Committee Practice Guidelines (2012) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 33:1787–1847. doi:10.1093/eurheartj/ehs104
McMurray JJ, Carson PE, Komajda M, McKelvie R, Zile MR, Ptaszynska A, Staiger C, Donovan JM, Massie BM (2008) Heart failure with preserved ejection fraction: clinical characteristics of 4133 patients enrolled in the I-PRESERVE trial. Eur J Heart Fail 10:149–156. doi:10.1016/j.ejheart.2007.12.010
Meng ZX, Nie J, Ling JJ, Sun JX, Zhu YX, Gao L, Lv JH, Zhu DY, Sun YJ, Han X (2009) Activation of liver X receptors inhibits pancreatic islet beta cell proliferation through cell cycle arrest. Diabetologia 52:125–135. doi:10.1007/s00125-008-1174-x
Mooijaart SP, Kuningas M, Westendorp RG, Houwing-Duistermaat JJ, Slagboom PE, Rensen PC, van Heemst D (2007) Liver X receptor alpha associates with human life span. J Gerontol A Biol Sci Med Sci 62:343–349 (62/4/343 [pii])
Morello F, de Boer RA, Steffensen KR, Gnecchi M, Chisholm JW, Boomsma F, Anderson LM, Lawn RM, Gustafsson JA, Lopez-Ilasaca M, Pratt RE, Dzau VJ (2005) Liver X receptors alpha and beta regulate renin expression in vivo. J Clin Invest 115:1913–1922. doi:10.1172/JCI24594
Nagoshi T, Yoshimura M, Rosano GM, Lopaschuk GD, Mochizuki S (2011) Optimization of cardiac metabolism in heart failure. Curr Pharm Des 17:3846–3853 (BSP/CPD/E-Pub/000724 [pii])
Naik SU, Wang X, Da Silva JS, Jaye M, Macphee CH, Reilly MP, Billheimer JT, Rothblat GH, Rader DJ (2006) Pharmacological activation of liver X receptors promotes reverse cholesterol transport in vivo. Circulation 113:90–97 (CIRCULATIONAHA.105.560177 [pii])
Neubauer S (2007) The failing heart—an engine out of fuel. N Engl J Med 356:1140–1151. doi:10.1056/NEJMra063052
Noghero A, Perino A, Seano G, Saglio E, Lo Sasso G, Veglio F, Primo L, Hirsch E, Bussolino F, Morello F (2012) Liver X receptor activation reduces angiogenesis by impairing lipid raft localization and signaling of vascular endothelial growth factor receptor-2. Arterioscler Thromb Vasc Biol 32:2280–2288. doi:10.1161/ATVBAHA.112.250621
Opie LH, Knuuti J (2009) The adrenergic-fatty acid load in heart failure. J Am Coll Cardiol 54:1637–1646. doi:10.1016/j.jacc.2009.07.024;10.1016/j.jacc.2009.07.024
Papageorgiou AP, Heggermont W, Rienks M, Carai P, Langouche L, Verhesen W, De Boer RA, Heymans S (2015) Liver X receptor activation enhances CVB3 viral replication during myocarditis by stimulating lipogenesis. Cardiovasc Res 107:78–88. doi:10.1093/cvr/cvv157
Patel M, Wang XX, Magomedova L, John R, Rasheed A, Santamaria H, Wang W, Tsai R, Qiu L, Orellana A, Advani A, Levi M, Cummins CL (2014) Liver X receptors preserve renal glomerular integrity under normoglycaemia and in diabetes in mice. Diabetologia 57:435–446. doi:10.1007/s00125-013-3095-6
Paulus WJ, Tschope C (2013) A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol 62:263–271. doi:10.1016/j.jacc.2013.02.092
Paulus WJ, Tschope C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE, Marino P, Smiseth OA, De Keulenaer G, Leite-Moreira AF, Borbely A, Edes I, Handoko ML, Heymans S, Pezzali N, Pieske B, Dickstein K, Fraser AG, Brutsaert DL (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J 28:2539–2550 (ehm037 [pii])
Peet DJ, Janowski BA, Mangelsdorf DJ (1998) The LXRs: a new class of oxysterol receptors. Curr Opin Genet Dev 8:571–575
Peet DJ, Turley SD, Ma W, Janowski BA, Lobaccaro JM, Hammer RE, Mangelsdorf DJ (1998) Cholesterol and bile acid metabolism are impaired in mice lacking the nuclear oxysterol receptor LXR alpha. Cell 93:693–704 (S0092-8674(00)81432-4 [pii])
Pencheva N, Buss CG, Posada J, Merghoub T, Tavazoie SF (2014) Broad-spectrum therapeutic suppression of metastatic melanoma through nuclear hormone receptor activation. Cell 156:986–1001. doi:10.1016/j.cell.2014.01.038
Proctor G, Jiang T, Iwahashi M, Wang Z, Li J, Levi M (2006) Regulation of renal fatty acid and cholesterol metabolism, inflammation, and fibrosis in Akita and OVE26 mice with type 1 diabetes. Diabetes 55:2502–2509 (55/9/2502 [pii])
Rankinen T, Sarzynski MA, Ghosh S, Bouchard C (2015) Are there genetic paths common to obesity, cardiovascular disease outcomes, and cardiovascular risk factors? Circ Res 116:909–922. doi:10.1161/CIRCRESAHA.116.302888
Rebe C, Raveneau M, Chevriaux A, Lakomy D, Sberna AL, Costa A, Bessede G, Athias A, Steinmetz E, Lobaccaro JM, Alves G, Menicacci A, Vachenc S, Solary E, Gambert P, Masson D (2009) Induction of transglutaminase 2 by a liver X receptor/retinoic acid receptor alpha pathway increases the clearance of apoptotic cells by human macrophages. Circ Res 105:393–401. doi:10.1161/CIRCRESAHA.109.201855
Repa JJ, Liang G, Ou J, Bashmakov Y, Lobaccaro JM, Shimomura I, Shan B, Brown MS, Goldstein JL, Mangelsdorf DJ (2000) Regulation of mouse sterol regulatory element-binding protein-1c gene (SREBP-1c) by oxysterol receptors, LXRalpha and LXRbeta. Genes Dev 14:2819–2830
Repa JJ, Mangelsdorf DJ (2002) The liver X receptor gene team: potential new players in atherosclerosis. Nat Med 8:1243–1248. doi:10.1038/nm1102-1243
Rooki H, Ghayour-Mobarhan M, Haerian MS, Ebrahimi M, Azimzadeh P, Heidari-Bakavoli A, Mirfakhraei R, Tavallaie S, Mirhafez R, Ferns G, Zali MR (2013) Lack of association between LXRalpha and LXRbeta gene polymorphisms and prevalence of metabolic syndrome: a case-control study of an Iranian population. Gene 532:288–293. doi:10.1016/j.gene.2013.09.107
Ross SE, Erickson RL, Gerin I, DeRose PM, Bajnok L, Longo KA, Misek DE, Kuick R, Hanash SM, Atkins KB, Andresen SM, Nebb HI, Madsen L, Kristiansen K, MacDougald OA (2002) Microarray analyses during adipogenesis: understanding the effects of Wnt signaling on adipogenesis and the roles of liver X receptor alpha in adipocyte metabolism. Mol Cell Biol 22:5989–5999
Ruggenenti P, Cravedi P, Remuzzi G (2012) Mechanisms and treatment of CKD. J Am Soc Nephrol 23:1917–1928. doi:10.1681/ASN.2012040390
Schultz JR, Tu H, Luk A, Repa JJ, Medina JC, Li L, Schwendner S, Wang S, Thoolen M, Mangelsdorf DJ, Lustig KD, Shan B (2000) Role of LXRs in control of lipogenesis. Genes Dev 14:2831–2838
Schuster GU, Parini P, Wang L, Alberti S, Steffensen KR, Hansson GK, Angelin B, Gustafsson JA (2002) Accumulation of foam cells in liver X receptor-deficient mice. Circulation 106:1147–1153
Sharma K, Kass DA (2014) Heart failure with preserved ejection fraction: mechanisms, clinical features, and therapies. Circ Res 115:79–96. doi:10.1161/CIRCRESAHA.115.302922
Shi Y, Xu X, Tan Y, Mao S, Fang S, Gu W (2014) A liver-X-receptor ligand, T0901317, attenuates IgE production and airway remodeling in chronic asthma model of mice. PLoS ONE 9:e92668. doi:10.1371/journal.pone.0092668
Silverberg D, Wexler D, Blum M, Schwartz D, Iaina A (2004) The association between congestive heart failure and chronic renal disease. Curr Opin Nephrol Hypertens 13:163–170
Sironi L, Mitro N, Cimino M, Gelosa P, Guerrini U, Tremoli E, Saez E (2008) Treatment with LXR agonists after focal cerebral ischemia prevents brain damage. FEBS Lett 582:3396–3400. doi:10.1016/j.febslet.2008.08.035
Solaas K, Legry V, Retterstol K, Berg PR, Holven KB, Ferrieres J, Amouyel P, Lien S, Romeo J, Valtuena J, Widhalm K, Ruiz JR, Dallongeville J, Tonstad S, Rootwelt H, Halvorsen B, Nenseter MS, Birkeland KI, Thorsby PM, Meirhaeghe A, Nebb HI (2010) Suggestive evidence of associations between liver X receptor beta polymorphisms with type 2 diabetes mellitus and obesity in three cohort studies: HUNT2 (Norway), MONICA (France) and HELENA (Europe). BMC Med Genet 11:144. doi:10.1186/1471-2350-11-144
Song C, Kokontis JM, Hiipakka RA, Liao S (1994) Ubiquitous receptor: a receptor that modulates gene activation by retinoic acid and thyroid hormone receptors. Proc Natl Acad Sci USA 91:10809–10813
Spillmann F, Van Linthout S, Miteva K, Lorenz M, Stangl V, Schultheiss HP, Tschope C (2014) LXR agonism improves TNF-alpha-induced endothelial dysfunction in the absence of its cholesterol-modulating effects. Atherosclerosis 232:1–9. doi:10.1016/j.atherosclerosis.2013.10.001
Spyridon M, Moraes LA, Jones CI, Sage T, Sasikumar P, Bucci G, Gibbins JM (2011) LXR as a novel antithrombotic target. Blood 117:5751–5761. doi:10.1182/blood-2010-09-306142
Stender S, Frikke-Schmidt R, Anestis A, Kardassis D, Sethi AA, Nordestgaard BG, Tybjaerg-Hansen A (2011) Genetic variation in liver X receptor alpha and risk of ischemic vascular disease in the general population. Arterioscler Thromb Vasc Biol 31:2990–2996. doi:10.1161/ATVBAHA.111.223867
Stenson BM, Ryden M, Venteclef N, Dahlman I, Pettersson AM, Mairal A, Astrom G, Blomqvist L, Wang V, Jocken JW, Clement K, Langin D, Arner P, Laurencikiene J (2011) Liver X receptor (LXR) regulates human adipocyte lipolysis. J Biol Chem 286:370–379. doi:10.1074/jbc.M110.179499
Stulnig TM, Steffensen KR, Gao H, Reimers M, Dahlman-Wright K, Schuster GU, Gustafsson JA (2002) Novel roles of liver X receptors exposed by gene expression profiling in liver and adipose tissue. Mol Pharmacol 62:1299–1305
Tachibana H, Ogawa D, Matsushita Y, Bruemmer D, Wada J, Teshigawara S, Eguchi J, Sato-Horiguchi C, Uchida HA, Shikata K, Makino H (2012) Activation of liver X receptor inhibits osteopontin and ameliorates diabetic nephropathy. J Am Soc Nephrol 23:1835–1846. doi:10.1681/ASN.2012010022;10.1681/ASN.2012010022
Tamura K, Chen YE, Horiuchi M, Chen Q, Daviet L, Yang Z, Lopez-Ilasaca M, Mu H, Pratt RE, Dzau VJ (2000) LXRalpha functions as a cAMP-responsive transcriptional regulator of gene expression. Proc Natl Acad Sci USA 97:8513–8518. doi:10.1073/pnas.100519097
Tangirala RK, Bischoff ED, Joseph SB, Wagner BL, Walczak R, Laffitte BA, Daige CL, Thomas D, Heyman RA, Mangelsdorf DJ, Wang X, Lusis AJ, Tontonoz P, Schulman IG (2002) Identification of macrophage liver X receptors as inhibitors of atherosclerosis. Proc Natl Acad Sci USA 99:11896–11901. doi:10.1073/pnas.182199799
Taube A, Schlich R, Sell H, Eckardt K, Eckel J (2012) Inflammation and metabolic dysfunction: links to cardiovascular diseases. Am J Physiol Heart Circ Physiol 302:H2148–H2165. doi:10.1152/ajpheart.00907.2011
Tontonoz P, Mangelsdorf DJ (2003) Liver X receptor signaling pathways in cardiovascular disease. Mol Endocrinol 17:985–993. doi:10.1210/me.2003-0061
Verschuren L, de Vries-van der Weij J, Zadelaar S, Kleemann R, Kooistra T (2009) LXR agonist suppresses atherosclerotic lesion growth and promotes lesion regression in apoE*3Leiden mice: time course and mechanisms. J Lipid Res 50:301–311. doi:10.1194/jlr.M800374-JLR200
Viennois E, Pommier AJ, Mouzat K, Oumeddour A, El Hajjaji FZ, Dufour J, Caira F, Volle DH, Baron S, Lobaccaro JM (2011) Targeting liver X receptors in human health: deadlock or promising trail? Expert Opin Ther Targets 15:219–232. doi:10.1517/14728222.2011.547853
Walcher D, Vasic D, Heinz P, Bach H, Durst R, Hausauer A, Hombach V, Marx N (2010) LXR activation inhibits chemokine-induced CD4-positive lymphocyte migration. Basic Res Cardiol 105:487–494. doi:10.1007/s00395-010-0092-5
Walczak R, Joseph SB, Laffitte BA, Castrillo A, Pei L, Tontonoz P (2004) Transcription of the vascular endothelial growth factor gene in macrophages is regulated by liver X receptors. J Biol Chem 279:9905–9911. doi:10.1074/jbc.M310587200
Wang Y, Li C, Cheng K, Zhang R, Narsinh K, Li S, Li X, Qin X, Zhang R, Li C, Su T, Chen J, Cao F (2014) Activation of liver X receptor improves viability of adipose-derived mesenchymal stem cells to attenuate myocardial ischemia injury through TLR4/NF-kappaB and Keap-1/Nrf-2 signaling pathways. Antioxid Redox Signal. doi:10.1089/ars.2013.5683
Westermann D, Lindner D, Kasner M, Zietsch C, Savvatis K, Escher F, von Schlippenbach J, Skurk C, Steendijk P, Riad A, Poller W, Schultheiss HP, Tschope C (2011) Cardiac inflammation contributes to changes in the extracellular matrix in patients with heart failure and normal ejection fraction. Circ Heart Fail 4:44–52. doi:10.1161/CIRCHEARTFAILURE.109.931451
Willy PJ, Umesono K, Ong ES, Evans RM, Heyman RA, Mangelsdorf DJ (1995) LXR, a nuclear receptor that defines a distinct retinoid response pathway. Genes Dev 9:1033–1045
Witteles RM, Fowler MB (2008) Insulin-resistant cardiomyopathy clinical evidence, mechanisms, and treatment options. J Am Coll Cardiol 51:93–102. doi:10.1016/j.jacc.2007.10.021;10.1016/j.jacc.2007.10.021
Wu S, Yin R, Ernest R, Li Y, Zhelyabovska O, Luo J, Yang Y, Yang Q (2009) Liver X receptors are negative regulators of cardiac hypertrophy via suppressing NF-kappaB signalling. Cardiovasc Res 84:119–126. doi:10.1093/cvr/cvp180;10.1093/cvr/cvp180
Yu J, Wang Q, Wang H, Lu W, Li W, Qin Z, Huang L (2014) Activation of liver X receptor enhances the proliferation and migration of endothelial progenitor cells and promotes vascular repair through PI3 K/Akt/eNOS signaling pathway activation. Vascul Pharmacol 62:150–161. doi:10.1016/j.vph.2014.05.010
Zelcer N, Hong C, Boyadjian R, Tontonoz P (2009) LXR regulates cholesterol uptake through Idol-dependent ubiquitination of the LDL receptor. Science 325:100–104. doi:10.1126/science.1168974
Zelcer N, Tontonoz P (2006) Liver X receptors as integrators of metabolic and inflammatory signaling. J Clin Invest 116:607–614. doi:10.1172/JCI27883
Zhang Y, Breevoort SR, Angdisen J, Fu M, Schmidt DR, Holmstrom SR, Kliewer SA, Mangelsdorf DJ, Schulman IG (2012) Liver LXRalpha expression is crucial for whole body cholesterol homeostasis and reverse cholesterol transport in mice. J Clin Invest 122:1688–1699. doi:10.1172/JCI59817;10.1172/JCI59817
Zhou YF, Zhang J, Li ZX, Miao JL, Yin QX, Li JJ, Zhang XY, Li YY, Luo HL (2014) Association of liver X receptor alpha (LXRalpha) gene polymorphism and coronary heart disease, serum lipids and glucose levels. Lipids Health Dis 13:34. doi:10.1186/1476-511X-13-34
Zhu M, Fu Y, Hou Y, Wang N, Guan Y, Tang C, Shyy JY, Zhu Y (2008) Laminar shear stress regulates liver X receptor in vascular endothelial cells. Arterioscler Thromb Vasc Biol 28:527–533 (ATVBAHA.107.143487 [pii])
Acknowledgments
This work was supported by the Netherlands Heart Foundation (grant no. 2007T046) and the Innovational Research Incentives Scheme program of the Netherlands Organization for Scientific Research (grants: VENI 916.10.117, VIDI 917.13.350).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Cannon, M.V., van Gilst, W.H. & de Boer, R.A. Emerging role of liver X receptors in cardiac pathophysiology and heart failure. Basic Res Cardiol 111, 3 (2016). https://doi.org/10.1007/s00395-015-0520-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00395-015-0520-7