Abstract
Purpose
We sought to determine the diagnostic ability of the end-expiratory inferior vena cava diameter (IVCEE) to predict fluid responsiveness (FR) and the potential confounding effect of intra-abdominal pressure (IAP).
Methods
In this multicenter study, 540 consecutive ventilated patients with shock of various origins underwent an echocardiographic assessment by experts. The IVCEE, velocity time integral (VTI) of the left ventricular outflow tract (LVOT) and intra-abdominal pressure (IAP) were measured. Passive leg raising (PLR) was then systematically used to perform a reversible central blood volume expansion. FR was defined by an increase in LVOT VTI ≥ 10% after 1 min of PLR.
Results
Since IVCEE was not obtained in 117 patients (22%), 423 were studied (septic shock: 56%), 129 of them (30%) having elevated IAP (≥ 12 mmHg) and 172 of them (41%) exhibiting FR. IVCEE ≤ 13 mm predicted FR with a specificity of at least 80% in 62 patients (15%), while IVCEE ≥ 25 mm predicted the absence of FR with a specificity of at least 80% in 61 patients (14%). In the remaining 300 patients (71%), the intermediate value of IVCEE did not allow predicting FR. An adjusted relationship between IVCEE and FR was observed while this relationship was less pronounced in patients with IAP ≥ 12 mmHg.
Conclusions
Measurement of IVCEE in ventilated patients is moderately feasible and poorly predicts FR, with IAP acting as a confounding factor. IVCEE might add some value to guide fluid therapy but should not be used alone for fluid prediction purposes.
Similar content being viewed by others
Introduction
Optimization of venous return to adjust oxygen delivery to metabolic needs is crucial in patients with acute circulatory failure, since excessive fluid loading may lead to interstitial edema and positive fluid balance has been shown to be detrimental [1]. Critical care echocardiography (CCE) is currently recommended as one of the first-line modalities to assess patients sustaining acute circulatory failure [2]. Various echocardiographic indices based on heart-lung interactions—such as respiratory variations of the inferior vena cava diameter (ΔIVC)—have been proposed to predict fluid responsiveness (FR) in ventilated patients, with suboptimal accuracy for the latter [3]. However, these parameters require a qualified operator with an advanced level of CCE experience [4], and their use is limited by numerous requirements, including the level of tidal volume [5] and the need to have a patient perfectly adapted to the ventilator [6]. In addition, the value of ΔIVC to predict FR has been suggested to be hampered by increased intra-abdominal pressure (IAP) [7].
Right atrial pressure (RAP) is a static parameter that is inaccurate in predicting FR [8]. Nevertheless, the correlation between the IVC diameter and RAP has been shown to be weak and inconsistent in mechanically ventilated patients [9], and we previously reported a large variability of RAP for a given IVC diameter [10]. A large overlap between the measured and estimated RAP based on IVC diameter measurement has also been reported in spontaneously breathing patients [11]. RAP measurement is highly influenced by the transmitted pressure (i.e., the pleural or pericardial pressure), and its measurement is altered by numerous technical factors [12]. In contrast, the end-expiratory IVC diameter (IVCEE) better reflects the transmural RAP and hence cardiac preload. In addition, IVCEE is expected to be easier and faster for measurements than ΔIVC by the front-line intensivist with competence in basic CCE in most critically ill patients [13]. It has recently been emphasized that IVCEE should be evaluated as a static index of FR in a large cohort of patients with acute circulatory failure [6]. Moreover, in the context of an increasing incidence of intra-abdominal hypertension in ICU patients [14], the potential influence of IAP on its diagnostic capacity should be addressed.
Accordingly, we sought to determine the diagnostic ability of IVCEE to predict FR in a multicenter cohort of ventilated patients with acute circulatory failure of various origins and to assess the potential confounding effect of IAP on its diagnostic accuracy.
Materials and methods
Patients
This multicenter descriptive study was prospectively conducted during a 2-year period in five intensive care units with expertise in CCE to initially assess the respective diagnostic value of echocardiographic dynamic parameters, including ΔIVC, for predicting FR [3]. We subsequently evaluated the clinical value of using IVCEE as a static parameter to identify patients with FR. All protocol aspects were approved by the local Ethics Committee, which waived the need for informed consent (no. 85-2012-09). Ventilated patients under sedation who required CCE assessment for an acute circulatory failure of any origin were eligible. Acute circulatory failure was defined as recommended [2]: sustained hypotension (systolic blood pressure < 90 mmHg or mean blood pressure < 65 mmHg) and/or the presence of clinical signs of hypoperfusion, metabolic acidosis (pH < 7.35 and base excess < − 5 mmol/l), elevated lactate (> 2 mmol/l) or decreased central venous oxygen saturation (ScvO2 < 70%). Hypotension may not have been present if previously corrected by ongoing vasopressor infusion. Exclusion criteria were: age < 18 years, pregnancy, amputation or severe lower limb ischemia and contraindication to the passive leg raising (PLR) maneuver (e.g., elevated intracranial pressure, tamponade, acute aortic dissection). Conventional hemodynamic parameters including RAP, respiratory parameters, bladder pressure used as a surrogate for IAP and ongoing therapy were recorded at the time of CCE assessment. Bladder pressure was measured as recommended at end-expiration through the patient’s indwelling bladder catheter after injecting 20 ml of normal saline, with the transducer zeroed on the mid-axillary line at the level of the iliac crest [15].
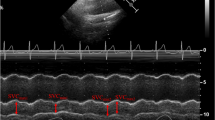
Critical care echocardiography
Patients were hemodynamically assessed within the first 24 h of admission in the semi-recumbent position by experienced intensivists trained in advanced CCE [4]. All echocardiographic measurements were performed in triplicate and averaged. IVCEE was measured in the subcostal longitudinal view of the vessel, using the inner edge technique, strictly perpendicular to IVC walls, approximately 2 cm from its junction with the right atrium and usually upstream of the take-off of the supra-hepatic vein [16]. Particular attention was directed to obtaining the largest vessel size at end-expiration with IVC walls strictly parallel to take into account a potential respiratory motion [17]. In addition, the left ventricular (LV) outflow tract velocity-time integral and diameter were measured to calculate LV stroke volume [18]. In our hands, the intraclass correlation coefficients used to assess intra- and interobserver reproducibility of measurements of IVCEE and LV stroke volume are 0.97 [95% confidence interval (CI) 0.96–0.99], 0.94 (95% CI 0.90–0.97), 0.98 (95% CI 0.97–0.99) and 0.93 (95% CI 0.89–0.96), respectively [3].
Systematic fluid loading was not performed because it could have been considered potentially harmful and unethical in our unselected consecutive patients sustaining any type of circulatory failure. Alternatively, PLR was systematically performed using a previously described technique allowing 90° tilting of the trunk [19]. This maneuver has been shown to mimic a blood volume expansion, with the advantage of being fully reversible, and to accurately identify FR in critically ill patients [20,21,22]. In practice, PLR was performed by elevating the patient’s legs and simultaneously transferring the trunk from a semi-recumbent to supine position [19]. At the end of the first minute of PLR corresponding to the maximal increase of venous return, the LV outflow tract velocity-time integral was measured and compared to the baseline value. FR was defined by an increase of the LV outflow tract velocity-time integral by at least 10% during PLR [23].
Statistical analysis
As continuous variables did not meet the normality distribution criteria (assessed by the Shapiro-Wilk and the Shapiro-Francia normality tests), descriptive statistics were provided as median and interquartile range for continuous variables and as numbers and percentages for categorical variables. To select factors associated with FR, we performed a multivariate logistic regression using FR as the dependent binary variable and IVCEE, age, gender, body surface area, septic shock, acute respiratory distress syndrome (ARDS), positive end-expiratory pressure level (as a binary variable: < or ≥ 8 cm H2O) and IAP. The latter was evaluated as a binary variable (IAP < or ≥ 12 mmHg) and a continuous variable. The interaction between IAP and IVCEE was specifically evaluated. The other relevant interactions were studied by including a cross-produced interaction term in the model. Adjusted probability of fluid responsiveness was then calculated from the model. The model's goodness of fit was checked using the Hosmer-Lemeshow test. For regression purposes, age, body surface area and IVCEE were centered on the minimal value (18 years, 1.24 m2 and 4 mm, respectively) observed in the data set. We a priori defined three targeted specificities for FR and for fluid unresponsiveness (95, 90 and 80%). We then calculated the respective sensitivity and determined the corresponding threshold values of IVCEE. Receiver-operating characteristic (ROC) curves were then plotted. p < 0.05 was considered significant except for interaction terms where we considered p < 0.1 nominally significant. All analyses were performed using Stata SE 14.1 (Stata Corp, College Station, TX).
Results
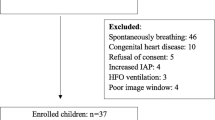
Among the 540 patients initially described [3], IVCEE was not obtained in 117 patients (22%) because of a poor subcostal view, and finally 423 patients were analyzed [median age: 65 years (IQR 56–76); 281 males; median SOFA score: 10 (8,9,10,11,12)], 172 of them being fluid responders (41%). One hundred twenty-nine patients (30%) had an IAP ≥ 12 mmHg. Acute circulatory failure was related to sepsis in 237 patients (56%) and ICU mortality reached 41% (Table 1). Differences between patients included in the study and the 117 excluded patients from the statistical analysis are reported in the eTable 1.
Correlation between IVCEE and RAP was significant, although weak, in the overall population and in the group of patients with an IAP < 12 mmHg, but not in the group of patients with an IAP ≥ 12 mmHg (eFigure 1). Median IVCEE was 19 (15–23) mm, significantly smaller in responders to fluid loading than in non-responders (18 [13–20] vs. 20 [18–23] mm: p = 0.000018) (Fig. 1). Distribution of individual IVCEE values is also reported in Fig. 1: 300 patients (71%) had an IVCEE diameter either > 13 mm or < 25 mm; 37% were fluid responders and 63% non-responders. To predict FR with a specificity of at least 95, 90 and 80%, the IVCEE threshold values were ≤ 8 mm (n = 16), ≤ 10 mm (n = 31) and ≤ 13 mm (n = 62), respectively. Conversely, to predict the absence of FR with a specificity of at least 95, 90 and 80%, IVCEE threshold values were ≥ 28 mm (n = 17), ≥ 27 mm (n = 28) and 25 mm (n = 61 patients), respectively (Table 2 and Fig. 2). As reported in the eFigure 2, the area under the ROC curve was not different for IVCEE and RAP in the overall population (0.620 and 0.573, respectively; p = 0.19), while the difference was significant in the subgroup of patients with an IAP < 12 mmHg (0.662 and 0.551, respectively; p = 0.018). No statistically significant difference in the IVCEE area under the ROC curve was observed between patients with and without elevated IAP (p = 0.1178).
Distribution of the end-expiratory inferior vena cava diameter measured in fluid responders and in non-responders. a Distribution in the overall population according to the different threshold values (dotted lines), as reported in the results. b Distribution according to the response to fluids (responders, green line; non-responders, blue line)
In multivariable analysis, IVCEE was independently associated with FR, and we observed a significant interaction between IVCEE and IAP (p for interaction = 0.069) (eTable 2). An adjusted relationship between IVCEE and FR in the subgroup of patients with an IAP < 12 mmHg was observed, while this relationship was less pronounced in patients with IAP ≥ 12 mmHg (Fig. 3).
Adjusted probability (and its 95% confidence intervals) of fluid responsiveness according to end-expiratory inferior vena cava diameter and intra-abdominal pressure. Probability was calculated using a multivariable logistic regression including an interaction term between inferior vena cava end-expiratory diameter and intra-abdominal pressure
Discussion
In ventilated patients assessed using CCE for an acute circulatory failure of any origin, the present study shows that: (1) the feasibility of measuring IVC is moderate since IVCEE could not be measured by experts in CCE in 22% of the cohort; (2) IVCEE was independently associated with FR, while its diagnostic value to predict FR remains globally low; (3) IVCEE predicted FR and fluid unresponsiveness in approximately 23% of patients (123/540) with a specificity of at least 80% based on two distinct threshold values, 13 (62 patients) and 25 mm (61 patients), respectively, while FR remained undetermined in 77% of the cases; (4) the relationship between FR and IVCEE was looser in the presence of elevated IAP (≥ 12 mmHg), a situation encountered in 30% of patients.
IVCEE was measured approximately 2 cm from the junction with the right atrium in the IVC long axis, as widely advocated [24], usually caudal to the hepatic vein inlet for the best accuracy [25]. However, the feasibility of such measurement reached only 78% in our cohort, a lower proportion than that reported in outpatients with only a 12% failure rate [26], presumably because of positive-pressure ventilation and the high prevalence of elevated IAP. Although previous studies have reported that two-dimensional measurement of IVCEE is accurate when performed by recently trained operators with a basic CCE level [27, 28], with a good interrater reliability [29], one may anticipate that the feasibility of IVCEE measurement could be even lower in less experienced hands.
Most studies assessing the ability of IVC ultrasound to predict FR used ΔIVC rather than IVCEE [6, 30]. ΔIVC, which is based on respirophasic variation of IVC, requires the use of M-mode tracing and an advanced level in CCE to be accurately measured [6, 13]. In ventilated patients it also probably requires that tidal volume exceeds 7 ml/kg [5] and that the patient is perfectly adapted to the ventilator [31]. Some authors also suggested that its accuracy could be altered in patients with elevated IAP [7]. In contrast, the subcostal view centered on the IVC is easily obtained [27, 28], and accuracy of IVCEE to predict FR is expected to be less dependent on respiratory settings.
In the present study, the overall diagnostic value of IVCEE for predicting FR was poor, as shown by the low area under the ROC curves. Nevertheless, markedly low or high IVCEE values may help the front-line intensivist guiding fluid therapy in certain patients. IVCEE ≤ 13 and ≤ 10 mm identified FR with a specificity of at least 80 and 90%, respectively. Similarly, all patients with IVCEE < 10 mm responded to a fluid loading in a previously published single-center study of 39 ventilated patients with septic shock [32]. Conversely, in our patients IVCEE ≥ 25 and ≥ 27 mm indicated the absence of FR with a specificity of at least 80 and 90%, respectively. These results are consistent with those of the same previous study reporting that all patients with IVCEE > 24 mm failed to respond to fluid loading [32]. Due to the large overlap of individual values of IVCEE, we purposely targeted high specificity to establish threshold values that could be used in the setting of a basic CCE assessment [13]. Although the proportion of patients exhibiting markedly low or high values of IVCEE is relatively small in the present cohort, using a specific and easy-to-obtain static index to guide the fluid requirement appears clinically relevant, especially during the basic CCE assessment of patients without advanced hemodynamic monitoring. If a reasonable specificity of 80% is considered clinically relevant by the physician to predict or eliminate FR, applying two distinct threshold values of 13 mm and 25 mm might allow discriminating 123 patients (22.7% of the 540 patients), 62 with a value ≤ 13 mm and 61 with a value ≥ 25 mm, while 71% of the 423 analyzed patients exhibited a value of IVCEE within an indeterminate range. A pragmatic approach that remains to be validated would be to administer fluids in patients with sustained acute circulatory failure and low risk of lung water overload when presenting with an indeterminate value of IVCEE, but to use highly specific threshold values of IVCEE to ascertain the benefit of fluid loading in patients at high risk of volume overload (e.g., ARDS), even though positive predictive values of such threshold values are not good.
One may consider that IVCEE has no additional value since it behaves as a static parameter and is related to RAP, which has widely been shown as inaccurate to predict FR [8]. Nevertheless, RAP suffers from numerous technical factors that limit its accuracy [12], whereas IVCEE measurement is straightforward and reproducible [3]. Moreover, RAP is very sensitive to any airway pressure transmission. Accordingly, it fails to accurately reflect right atrial transmural pressure, hence right ventricular preload. This may explain the weak correlation between RAP and IVCEE reported in many studies [9,10,11] and confirmed in the present cohort. Interestingly, the area under the ROC curve of IVCEE for predicting FR was significantly higher than that of RAP in the subgroup of patients with an IAP < 12 mmHg, which was not the case in patients with elevated IAP. As far as we know, our study first assessed the relationship between IAP and IVCEE in a large cohort of ventilated patients with acute circulatory failure of all causes. While IVCEE was independently associated with FR, a significant interaction with IAP was evidenced by a looser relationship in the presence of elevated IAP values (≥ 12 mmHg). Accordingly, elevated IAP appears to be a confounding factor and IVCEE should be used with caution to predict FR in patients with suspected or documented intra-abdominal hypertension. In our study, 30% of the patients had an elevated IAP, a similar proportion as that reported by Malbrain et al. (27.7%) in a large cohort of unselected critically ill patients [14]. Interestingly, the weak yet significant correlation between IVCEE and RAP observed in the overall study population was no longer present in the subgroup of patients with elevated IAP.
The present study has several limitations. First, PLR was performed to identify FR rather than systematic fluid loading because of the various origins of acute circulatory failure encountered in our cohort (e.g., cardiogenic shock, ARDS). However, in two recent meta-analyses, PLR had an area under the curve of 0.96 and 0.95, respectively, to predict FR in shocked patients and is well known to transiently mimic a blood volume expansion [20, 21]. Moreover, only 39 of our patients exhibited an IAP > 16 mmHg, a level known to reduce the effect of PLR on volume expansion [33]. Second, IVCEE was measured in ventilated patients who were sedated and perfectly adapted to the ventilator. Accordingly, our results cannot necessarily be extrapolated to the patient with spontaneous respiratory effort. This will require further study. Nevertheless, IVCEE measured in the long axis view of the vessel is neither influenced by respirophasic variation of the diameter of the vessel [5] nor by respiratory displacement of the vessel [17]. This offers an advantage compared to the measurement of ΔIVC. Third, we made the choice to study specificity instead of positive predictive value as the latter is dependent on the prevalence of fluid responsiveness in the study population and may not be therefore replicable in another ICU population with a different prevalence. However, we acknowledge that the positive predictive values were not good, even using low or high threshold values with high specificity. Finally, IVCEE was measured by an expert in CCE. Consequently, our results cannot be extrapolated to other clinical settings with less experienced operators.
In summary, even in expert hands, the measurement of IVCEE is moderately feasible in ventilated patients with acute circulatory failure of various origins and poorly predicts FR because of a broad range of uncertainty. Nevertheless, IVCEE might add some value to guide fluid therapy, but should not be used alone for fluid prediction purposes. This static parameter should be used with caution in patients with suspected or documented intra-abdominal hypertension because of the confounding effects of elevated IAP.
References
Boyd JH, Forbes J, Nakada TA et al (2011) Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med 39:259–265
Cecconi M, De Backer D, Antonelli M et al (2014) Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of intensive care medicine. Intensive Care Med 40:1795–1815
Vignon P, Repessé X, Bégot E et al (2017) Comparison of echocardiographic indices used to predict fluid responsiveness in ventilated patients. Am J Respir Crit Care Med 195:1022–1032
Experts round table on echocardiography in ICU (2014) International consensus statement on training standards for advanced critical care echocardiography. Intensive Care Med 40:654–666
De Backer D, Heenen S, Piagnerelli M, Koch M, Vincent JL (2005) Pulse pressure variations to predict fluid responsiveness: influence of tidal volume. Intensive Care Med 31:517–523
Bentzer P, Griesdale DE, Boyd J, MacLean K, Sirounis D, Ayas NT (2016) Will this hemodynamically unstable patient respond to a bolus of intravenous fluid? JAMA 316:1298–1309
Duperret S, Lhuillier F, Piriou V, Vivier E, Metton O, Branche P, Annat G, Bendjelid K, Viale JP (2007) Increased intra-abdominal pressure affects respiratory variations in arterial pressure in normovolaemic and hypovolaemic mechanically ventilated healthy pigs. Intensive Care Med 33:163–171
Osman D, Ridel C, Ray P, Monnet X, Anguel N, Richard C, Teboul JL (2007) Cardiac filling pressures are not appropriate to predict hemodynamic response to volume challenge. Crit Care Med 35:64–68
Ciozda W, Kedan I, Kehl D, Zimmer R, Khandwalla R, Kimchi A (2016) The efficacy of sonographic measurement of inferior vena cava diameter as an estimate of central venous pressure. Cardiovasc Ultrasound 14:33
Barbier C, Loubières Y, Jardin F, Vieillard-Baron A (2004) Author’s reply to the comment by Dr. Bendjelid. Intensive Care Med 30:1848
Seo Y, Iida N, Yamamoto M, Machino-Ohtsuka T, Ishizu T, Aonuma K (2017) Estimation of central venous pressure using the ratio of short to long diameter from cross-sectional images of the inferior vena cava. J Am Soc Echocardiogr 30:461–467
Magder S (2017) Right atrial pressure in the critically ill: how to measure, what is the value, what are the limitations? Chest 151:908–916
Mayo PH, Beaulieu Y, Doelken P et al (2009) American College of Chest Physicians/La SRLF. Statement on competence in critical care ultrasonography. Chest 135:1050–1060
Malbrain M, Chiumello D, Cesna B et al (2014) A systematic review and individual patient data meta-analysis on intra-abdominal hypertension in critically ill patients: the wake-up project. World initiative on abdominal hypertension epidemiology, a unifying project (Wake-up!). Minerva Anestesiol 80:293–306
Cheatham ML, Malbrain ML, Kirkpatrick A, Sugrue M et al (2007) Results from the international conference of experts on intra-abdominal hypertension and abdominal compartment syndrome II. Recommendations. Intensive Care Med 33:951–962
Stone MB, Huang JV (2013) Inferior vena cava assessment: correlation with CVP and plethora in tamponade. Glob Heart 8:323–327
Blehar DJ, Resop D, Chin B, Dayno M, Gaspari R (2012) Inferior vena cava displacement during respirophasic ultrasound imaging. Crit Ultrasound J 4:18
Zoghbi WA, Quinones MA (1986) Determination of cardiac output by Doppler echocardiography: a critical appraisal. Herz 11:258–268
Jabot J, Teboul JL, Richard C, Monnet X (2009) Passive leg raising for predicting fluid responsiveness: importance of the postural change. Intensive Care Med 35:85–90
Cavallaro F, Sandroni C, Marano C et al (2010) Diagnostic accuracy of passive leg raising for prediction of fluid responsiveness in adults: systematic review and meta-analysis of clinical studies. Intensive Care Med 36:1475–1483
Cherpanath TG, Hirsch A, Geerts BF et al (2016) Predicting fluid responsiveness by passive leg raising: a systematic review and meta-analysis of 23 clinical trials. Crit Care Med 44:981–991
Monnet X, Marik P, Teboul JL (2016) Passive leg raising for predicting fluid responsiveness: a systematic review and meta-analysis. Intensive Care Med 42:1935–1947
Monnet X, Rienzo M, Osman D et al (2006) Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med 34:1402–1407
Lang RM, Bierig M, Devereux RB et al (2015) Chamber quantification writing group; American Society of echocardiography’s guidelines and standards committee; European Association of echocardiography. Recommendations for chamber quantification. J Am Soc Echocardiogr 28:1–39
Wallace DJ, Allison M, Stone MB (2010) Inferior vena cava percentage collapse during respiration is affected by the sampling location: an ultrasound study in healthy volunteers. Acad Emerg Med 17:96–99
Brennan JM, Blair JE, Goonewardena S et al (2007) A comparison by medicine residents of physical examination versus and-carried ultrasound for estimation of right atrial pressure. Am J Cardiol 99:1614–1616
Vignon P, Dugard A, Abraham J et al (2007) Focused training for goal-oriented hand-held echocardiography performed by noncardiologist residents in the intensive care unit. Intensive Care Med 33:1795–1799
Vignon P, Mücke F, Bellec F et al (2011) Basic critical care echocardiography: validation of a curriculum dedicated to noncardiologist residents. Crit Care Med 39:636–642
Fields JM, Lee PA, Jenq KY, Mark DG, Panebianco NL, Dean AJ (2011) The interrater reliability of inferior vena cava ultrasound by bedside clinician sonographers in emergency department patients. Acad Emerg Med 18:98–101
Zhang Z, Xu X, Ye S, Xu L (2014) Ultrasonographic measurement of the respiratory variation in the inferior vena cava diameter is predictive of fluid responsiveness in critically ill patients: systematic review and meta-analysis. Ultrasound in Med and Biol 40:845–853
Via G, Tavazzi G, Price S (2016) Ten situations where inferior vena cava ultrasound may fail to accurately predict fluid responsiveness: a physiologically based point of view. Intensive Care Med 42:1164–1167
Feissel M, Michard F, Faller JP, Teboul JL (2004) The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med 30:1834–1837
Mahjoub Y, Touzeau J, Airapetian N, Lorne E, Hijazi M et al (2010) The passive leg raising maneuver cannot accurately predict fluid responsiveness in patients with intra-abdominal hypertension. Crit Care Med 38:1824–1829
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflict of interest relevant to this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vieillard-Baron, A., Evrard, B., Repessé, X. et al. Limited value of end-expiratory inferior vena cava diameter to predict fluid responsiveness impact of intra-abdominal pressure. Intensive Care Med 44, 197–203 (2018). https://doi.org/10.1007/s00134-018-5067-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-018-5067-2