Abstract
Objective
To evaluate the effect of increased intra-abdominal pressure (IAP) on the systolic and pulse pressure variations induced by positive pressure ventilation in a porcine model.
Design and setting
Experimental study in a research laboratory.
Subjects
Seven mechanically ventilated and instrumented pigs prone to normovolaemia and hypovolaemia by blood withdrawal.
Intervention
Abdominal banding gradually increased IAP in 5-mmHg steps up to 30 mmHg.
Measurements and main results
Variations in systolic pressure, pulse pressure, inferior vena cava flow, and pleural and transmural (LVEDPtm) left-ventricular end-diastolic pressure were recorded at each step. Systolic pressure variations were 6.1 ± 3.1%, 8.5 ± 3.6% and 16.0 ± 5.0% at 0, 10, and 30 mmHg IAP in normovolaemic animals (mean ± SD; p< 0.01 for IAP effect). They were 12.7 ± 4.6%, 13.4 ± 6.7%, and 23.4 ± 6.3% in hypovolaemic animals (p< 0.01 vs normovolaemic group) for the same IAP. Fluctuations of the inferior vena cava flow disappeared as the IAP increased. Breath cycle did not induce any variations of LVEDPtm for 0 and 30 mmHg IAP.
Conclusions
In this model, the systolic pressure and pulse pressure variations, and inferior vena cava flow fluctuations were dependent on IAP values which caused changes in pleural pressure swing, and this dependency was more marked during hypovolaemia. The present study suggests that dynamic indices are not exclusively related to volaemia in the presence of increased IAP. However, their fluid responsiveness predictive value could not be ascertained as no fluid challenge was performed.
Similar content being viewed by others
Introduction
The effects of positive-pressure ventilation on systolic pressure variations (SPV) have been intensively studied for several years but a clear understanding of the pathophysiology has not been established. Nevertheless, a pattern has emerged [1]. An increase in systolic arterial pressure during the inspiratory phase of mechanical ventilation is followed by a decrease during expiration [1, 2, 3]. Several publications described using the ventilation-induced cyclic fluctuations of systolic arterial pressure to assess volaemia [4] or detect fluid responsiveness in septic [5] or in postoperative patients [6]. Recently, special attention has been focused on variations in arterial pulse pressure [7] or aortic Doppler velocity [8] as predictors of preload dependency of the heart. Most of these studies have been performed in septic or postoperative patients without any mention of their intra-abdominal pressure (IAP),although the latter is often elevated in critically ill patients [9]. The increase in IAP is likely to modify some of the contributing factors to the cyclic circulatory changes induced by positive-pressure ventilation. As there is increasing interest in the use of respiratory-induced circulatory variations to assess the volaemia in ventilated critically ill patients, the effect of an increased IAP on the circulatory changes during positive-pressure ventilation should be evaluated. We hypothesized that the increased IAP induced an increase in pleural pressure swing contributing to the SPV increase. We therefore studied in an experimental pig model the circulatory changes induced by positive-pressure ventilation while the IAP was progressively increased.
Materials and methods
Animals and anaesthesia
The experimental protocol was conducted in seven pigs (weight 30–35 kg) according to the guidelines of the animal care committee of Claude Bernard University (Lyon, France). The animals were the same as those used in a previous paper describing the central effect of increased intra-abdominal pressure [10]. After premedication, the animals were anaesthetized with continuous infusion of propofol (Diprivan 1%, 100 μg·kg−1min−1) and sufentanil (1 μg·kg−1h−1). They underwent mechanical ventilation (Servo ventilator 900C-Siemens-Elema AB, Solna, Sweden) in a volume-controlled mode and a FIO2 of 0.4. Respiratory rate was 12 min−1, inspiratory:expiratory ratio was 1/2, end-expiratory pressure was 0 cmH2O, and tidal volume was set in order to maintain the end-expiratory partial pressure of CO2 at 0 mmHg IAP within the normal range. This tidal volume was not changed thereafter.
A fluid-filled catheter was placed in the carotid artery to monitor arterial pressure and an additional catheter was inserted into the contralateral internal jugular vein allowing administration of intravenous drugs and fluids. An 8-cm air-filled latex cylindrical balloon (Marquat, Boissy-St-Léger, France) was placed in the peritoneal cavity via a stab wound to measure abdominal pressure. Ultrasound transit-time flow probes were placed around the root of the aorta (14 mm A series; Transonic Systems, Ithaca, NY) and the inferior vena cava (16 mm S series; Transonic Systems) after median sternotomy and longitudinal pericardiotomy. The left ventricle was catheterized with a 20-cm fluid-filled catheter through a purse-string suture via the apex of the left ventricle (LV), allowing free movement of the heart. The pericardium was then partially closed and suspended in a pericardial cradle. Finally, the ultrasound transducer of a transoesophageal echocardiographic probe (5 MHz, Sonos 1500; Philips Medical Systems, Andover, MA) was placed on the epicardium in a position allowing a continuous monitoring of the LV in the midpapillary short axis plane. Before closing the chest cavity, drains were inserted in the pleural space and another air-filled balloon was placed in the mediastinal pleural cavity. All the signals of flows and pressures were recorded using a multichannel recording system (MP100; Biopac Systems, Santa Barbara, CA). In order to modify the IAP, the abdomen was banded with a Velcro belt maintained by three inextensible belts and a large extra-abdominal inflatable balloon was positioned underneath. During the normovolaemic measurements, a lactate Ringer's solution was infused, the amount infused before the measurements was intended to obtain an absolute end-expiratory right atrial pressure greater than 5 mmHg at 0 mmHg IAP.
Experimental protocol
After the surgical preparation, a 15 min stabilization period was allowed. Respiratory, circulatory and echocardiographic variables were recorded over 5 minutes under stable anaesthesia. Then the IAP was gradually increased by 5 mmHg increments up to 30 mmHg by inflating the balloon. Circulatory variables were recorded during the last 5 minutes of each step. At the end of each step, disconnection of the ventilator over two breaths allowed us to record the systolic arterial pressure during apnoea. At 30 mmHg IAP, in addition to circulatory variables, a new echocardiographic analysis was performed. IAP was then restored to the initial value by releasing the abdominal banding. Following this, blood was withdrawn until the mean arterial pressure stabilized at 60 mmHg. As most often the arterial pressure was partially restored, a new withdrawal of blood was necessary to stabilize the mean arterial pressure at 60 mmHg. Once a hypovolaemic steady state was obtained, a new progressive increase in IAP was realized, and the same recordings were obtained.
Measurements and calculations
All circulatory data were averaged over five breaths. Systolic and diastolic pressures were measured on a beat-by-beat basis, allowing us to calculate pulse pressure as the difference between systolic and diastolic pressure. The maximal and minimal systolic and pulse pressures within the breath were determined, and the SPV and pulse pressure variation (PPV) were calculated as the difference between the maximal and minimal values. Comparisons with the systolic pressure during apnoea allowed us to calculate a Δ up SPV, defined as the positive difference, and a Δ down SPV as the negative difference. From the aortic flow recordings, stroke volume was obtained by numerical integration. By using the same approach as mentioned above for the pressure, the stroke volume variations could be calculated. The pressure and volume variations are expressed in absolute values in Table 1 and in percent variation of their mean values in the figures. The same measurements were applied to the vena cava flow, allowing us to compute the inferior vena cava flow variations during positive-pressure ventilation.
By using the airway pressure signal displayed on the circulatory recordings, we selected eight specific beats to perform a within-breath analysis. The first and the second beats were before and after the onset of inspiration. The third and the fourth were at the end of the inspiration. The fifth and sixth beats were those at the onset of expiration. Finally, the last two analyzed beats were recorded at the end of the expiration. This method allowed us to synchronize the recordings performed in different animals with different heart rates. The dynamic compliance of the respiratory system was calculated by dividing the expiratory tidal volume by the maximal airway pressure.
Echocardiography
Echocardiographic study consisted of an epicardium short-axis view at the midpapillary level for analysis of left-ventricular end-diastolic area (LVEDA). End diastole was defined as the frame corresponding to the largest LV cross-sectional area immediately after the R-wake peak on the electrocardiogram. The LV end-diastolic cross-sectional area was measured by manual planimetry of the area circumscribed by the leading edge of the LV endocardial border. The anterolateral and posteromedial papillary muscles were included within the ventricular area. No further attempt was made in order to measure end-systolic area within the breath. Indeed, the inter-user variability of this area within the breath at 30 mmHg in normovolaemic animals exceeded 10%, the commonly held threshold value of reliable accuracy. The same was true for LVEDA and end-systolic areas in hypovolaemic animals. Indeed, in these animals, the areas of the left ventricle were very small or even virtual during the systole.
Statistical analysis
All results are expressed as mean ± SD. Data of cyclic changes induced by positive-pressure ventilation as a function of IAP were analysed using a two-way analysis of variance testing for volaemia and IAP effects. Data for circulatory changes within the breath were analysed by a three-way analysis of variance testing for volaemia, IAP, and heart beat effects. As there were several measurements for each effect, an interaction analysis was given by the same analysis of variance. Analysis of variance was followed by a Newman–Keuls post-hoc test when it showed significance for comparison of mean values. For all comparisons, the null hypothesis was rejected when the calculated probability p value was less than 0.05. The dependency of the SPV at 0 and 30 mmHg IAP was studied by a linear regression analysis with the pleural pressure and the stroke volume. Both 95% intervals of confidence were calculated after a Fischer Z transformation [11].
The statistical analyses were performed using SPSS 11.5 for Windows (SPSS, Chicago, IL, USA).
Results
Representative recording of pressures and flows over three breaths are reported in Fig. 1. The increase in IAP from baseline value to 30 mmHg induced significant changes in PaO2 only in normovolaemic animals, from 192 ± 77 to 101 ± 58 mmHg; the variation was from 151 ± 68 to 126 ± 46 in hypovolaemic animals. PaCO2 significantly increased from 47 ± 11 to 55 ± 8 and from 46 ± 8 to 57 ± 12 in normovolaemic and hypovolaemic animals, respectively. The dynamic compliance of the respiratory system significantly decreased in both groups: from 23 ± 6 to 11 ± 2 ml·cmH2O−1 in normovolaemic animals and from 22 ± 5 to 11 ± 2 ml·cmH2O−1 in hypovolaemic animals.
An illustrative example of recordings of arterial pressure (AP), inferior vena cava flow (IVC Flow), stroke volume (SV), pulse pressure (PP), left ventricular pressure (LVP), and pleural pressure (Ppl) over three breaths at baseline IAP (left column) and at 30 mmHg IAP (right column). Increase in systolic arterial pressure and pulse pressure occurred during inspiration with a parallel evolution of the stroke volume at baseline IAP. At 30 mmHg IAP, the amplitudes of pressure variations were greater than at baseline IAP. The SAP fluctuations were not strictly parallel to the stroke volume and pulse pressure variations. This is the case at the end of the inspiration during which the stroke volume and pulse pressure decreased whereas the systolic arterial pressure still increased. Whatever the IAP, the evolution of LV end-diastolic pressure and Ppl were parallel
Cyclic circulatory changes induced by positive-pressure ventilation as a function of IAP
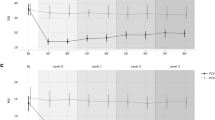
In normovolaemic animals, the SPV steadily increased with the IAP. In hypovolaemic animals, the SPV was higher and remained unchanged for values of IAP lower than 15 mmHg. Beyond this level the SPV increased in a parallel manner to the other group. In both groups of animals, this increase was ascribed to the Δ up variation, as no Δ down increase with the IAP was noted. The PPV followed a pattern similar to that of the SPV, and the stroke volume variations were parallel to those of the pulse pressure. Contrary to other circulatory data, the values for inferior vena cava flow were lower during inspiration than expiration. The inferior vena cava flow fluctuations were cancelled as soon as the IAP was beyond 15 mmHg and 10 mmHg in the normovolaemic and hypovolaemic groups respectively. The pleural pressure variations were similar between the two groups, whereas the transmural left-ventricular end-diastolic pressure was consistently higher in the normovolaemic group (Fig. 2, Table 1).
Evolution of the cyclic circulatory changes induced by positive-pressure ventilation as a function of intra-abdominal pressure (IAP): systolic arterial pressure (SAP), systolic pressure variations (SPV), pulse pressure variations (PPV), stroke volume variations (SVV), pleural pressure variations ( Δ Ppl), stroke volume (SV), negative systolic pressure variations ( Δ down), positive systolic pressure variations ( Δ up), inferior vena cava flow variations ( Δ IVC Flow), and trans mural left ventricular end-diastolic (LVEDPtm) for normovolaemic group (closed circles) and hypovolaemic group (open circles). Analysis of variance testing for the effect of volaemia showed significance for all the variables except for Δ Ppl and Δ up. There was a significant interaction between the two factors for PPV (p = 0.03) and Δ IVC Flow (p = 0.005) variations. *p < 0.05 versus baseline IAP for all variables; #p < 0.05 versus normovolaemic group
Cyclic circulatory changes in systolic arterial pressure within breath at 0 and 30 mmHg IAP.
Systolic arterial pressure increased during inspiration and decreased during expiration (Fig. 3). The amplitude of the increase depended on the IAP for the two groups of animals: it was low at an IAP of 0 mmHg and higher at an IAP of 30 mmHg. The Δ up was 1.0 ± 1.7 and 1.7 ± 1.2 mmHg at 0 mmHg IAP for the normovolaemic and hypovolaemic groups, respectively. It was 8.8 ± 3.6 and 9.4 ± 3.2 mmHg at 30 mmHg IAP, respectively. The Δ down was –3.8 ± 2.3 and –8.9 ± 1.3 mmHg at 0 mmHg IAP, and –4.1 ± 3.5 and –5.5 ± 2.8 at 30 mmHg IAP, for normovolaemic and hypovolaemic animals respectively. The behaviour of pulse pressure was different. There was no significant increase during inspiration, whatever the IAP or the volaemia. Conversely, a decrease was noted during expiration at the highest level of IAP, whatever the volaemia. The results observed for stroke volume were parallel to those for pulse pressure, except for the dependency on volaemia of stroke volume at high IAP, which was not observed for the pulse pressure. SPV correlated better with pleural pressure (r = 0.65, 95% CI [0.56, 0.72]) than with stroke volume (r = 0.12, 95% CI [–0.05, 0.20]).
Evolution of the systolic pressure variations from the pressure recorded during apnoea ( Δ SAP), pulse pressure (PP), and stroke volume (SV) within the breath cycle at 0 and 30 mmHg for normovolaemic animals (closed circles) and hypovolaemic animals (open circles), at low IAP (0 mmHg – left column) and high IAP (30 mmHg – right column). The heart beat numbers have been synchronized by selection among animals of specific beats as shown in Fig. 1. Transition from insufflation to expiration is represented as a dotted vertical line. The level of SAP during apnoea is indicated by the horizontal dotted line. Analysis of variance testing for the effect of volaemia showed significance for SV but not for Δ SAP (p = 0.08) and PP (p = 0.08). The same analysis confirmed an IAP effect for all variables. An interaction was observed between the heart beat number and the IAP for Δ SAP. *p < 0.05 versus baseline IAP for all variables
Cyclic circulatory changes in inferior vena cava flow and left ventricular size within breath at 0 and 30 mmHg IAP
Besides the dependency of the inferior vena cava flow on the volaemia and the IAP, a clear contrast was observed regarding the effect of the breath cycle between the two levels of IAP (Fig. 4). At low IAP the inferior vena cava flow fluctuated within the breath, whereas no fluctuation was observed at 30 mmHg IAP. Whereas the transmural left-ventricular end-diastolic pressure was dependent on the volaemia, it was not dependent on the phase of the breath, whatever the IAP level (Fig. 4). The same pattern was observed for the LVEDA.
Evolution of inferior vena cava flow (IVC Flow), transmural left-ventricular end-diastolic pressure (LVEDPtm), left-ventricular end-diastolic area (LVEDA), and pleural pressure (Ppl) within the breath cycle at 0 mmHg (left column) and 30 mmHg (right column) for normovolaemic animals (closed circles) and hypovolaemic animals (open circles). The heart beat numbers have been synchronized by selection among animals of specific beats as shown in Fig. 1. Transition from inspiration to expiration is the dotted vertical line. Analysis of variance testing for the effect of volaemia showed significance for IVC Flow and LVEDPtm but not for Ppl. The same analysis confirmed an IAP effect for all variables. An interaction was observed between the heart beat number and the IAP for IVC Flow and Ppl. Analysis of variance testing for heart beat number effect did not show any significance for LVEDA and LVEDPtm. *p < 0.05 versus baseline IAP for all variables
Discussion
The main finding of this study is that the cyclic circulatory changes induced by positive-pressure ventilation were dependent on the IAP. The cyclic circulatory changes of SPV, PPV and stroke volume variations increased as the pleural pressure swing induced by the progressive change in IAP was enhanced. However, these increases were more marked in hypovolaemic than in normovolaemic animals.
Numerous previous publications have studied the cyclic changes induced by mechanical ventilation [1, 3, 4, 5, 7]. The mechanisms of these variations involve the increases in thoracic pressure and thoracic volume on the right and left ventricular functions. The major effect of mechanical ventilation on the venous return may explain the sensitivity of the pressure-induced variations on the volaemia. This dependency has led to the commonly held assertion that patients experiencing large pressure fluctuations during mechanical ventilation are preload-dependent and that, if needed, they should respond to a fluid loading challenge with an increase in cardiac output [5, 12]. This interpretation relies on the principles of heart–lung interactions developed in physiological conditions or in specific critically ill patients with sepsis or in the postoperative period. Other pathological conditions may limit the routine assessment of preload by using cyclic circulatory change monitoring. One such condition is the increase in the abdominal pressure that is commonly observed in the general population admitted to adult ICUs [9, 13]. This high IAP could interfere with the interactions linking the positive-pressure ventilation to the observed cyclic circulatory changes by at least two mechanisms. First, the IAP is the pressure around the inferior vena cava and thus is likely to modify the vena cava transmural pressure and flow. Second, an increase in IAP is likely to alter chest wall compliance and thus, for a given tidal volume, to increase the tidal pressure swing. This positive-pressure variation represents the forcing function applied to the circulatory system and any change in its amplitude is likely to modify the pressure-induced variations of arterial pressures.
The inferior vena cava flow fluctuations actually decreased with the progressive modification of the IAP. This finding is in agreement with the concept of abdominal vascular zone conditions as reported by Takata et al. [14]. At low IAP, the driving pressure for the inferior vena cava flow is the hydrostatic pressure gradient between the inferior vena cava and the right atrium. Any increase in pleural pressure induced by positive-pressure ventilation led to an increase in right atrial pressure. The inferior vena cava pressure remained fairly stable as the pleural pressure was only partially transmitted to the abdomen [15]. As a consequence, the pressure gradient for venous return and thus the inferior vena cava flow decreased. The situation was quite different at high levels of IAP. In this condition, a phenomenon termed vascular waterfall has been described to develop as the IAP is superior to the right atrial pressure [14]. The gradient pressure for the venous return became the difference between the intravascular venous cava pressure and the IAP. Any fluctuation of the pleural pressure and thus of the right atrial pressure had no more influence on the backward driving pressure and therefore on the vena cava flow. In the present study, the disappearance of the vena cava flow fluctuations with the increasing IAP is in agreement with this abdominal zone concept [14]. From a practical point of view, this observation should caution against fluid responsiveness interpretation of respiratory changes in inferior vena cava diameter in the case of IAP greater than right atrial pressure [16].
The tidal pleural pressure swing increased with the IAP changes. Increasing the IAP led to a marked decrease in the respiratory system compliance as evidenced by the increase in airway pressure needed to insufflate the tidal volume. This resulted in marked increase in pleural pressure during inspiration at high IAP, whereas the end-expiratory pressure was not modified, as the respiratory system is open to the atmosphere. This respiratory mechanical modifications were in line with a previous publication reporting a decreased respiratory system compliance with an unchanged end-expiratory pleural pressure as the IAP was increased to 20 cmH2O [17]. The increase in positive pressure-induced arterial fluctuations associated with the increase in the pleural pressure swing may have at least three explanations: (1) The increase in the IAP induced a progressive increase in intrathoracic pressure, as indicated by the increased pleural pressure swings, and therefore a relative hypovolaemia owing to a redistribution of blood volume. Although this factor is likely to play a role at the highest values of IAP as a decrease in LVEDA was observed, a moderate value of IAP was, on the contrary, associated with an increase in thoracic blood volume [10]. This was observed in our experiments as manifested by the increase in the LVEDA [10] and in the transmural left-ventricular end-diastolic pressure. Moreover, this finding was in line with previous papers reporting an increase in heart volume secondary to a moderate increase in IAP at 20 cmH2O [17]. (2) The second explanation could be related to the increased pleural pressure swing itself. Indeed, it has been already reported that for the same volaemia, stroke volume variations [18] or PPV [19, 20] were dependent on the insufflated tidal volume and therefore on the induced variation in pleural pressure. In fact, induced pressure variations depend not only on the part of the left-ventricular Starling curve the forcing function is operating, in other words the volaemia, but also on the amplitude of this forcing function. However, this mechanism would have induced a progressive increase in the left-ventricular preload fluctuations which was not observed in the beat by beat analysis. Similarly, this would have induced a preferential increase in Δ down with the increase in IAP, whereas we observed a more marked increase in the Δ up. This results are in agreement with a previous study investigating the determinants of pressure variation during positive-pressure ventilation in anaesthetized cardiac surgery patients [21]. The authors found no consistent relationship between the arterial pressure variations and the left-ventricular areas estimated by transoesophageal echocardiography. Moreover, in the present study there was no clear-cut difference in the LVEDA pattern between 0 and 30 mmHg IAP. (3) Finally, the role of the end-inspiratory pleural pressure variations should be considered. The pleural pressure was transmitted to the left ventricle and the aorta inducing an increase in LVEDP and diastolic arterial pressure during inspiration, as shown in Fig. 1. The transmission of the pleural pressure to the aortic pressure could explain why, during inspiration, the systolic pressure increased at the end-inspiratory period whereas the stroke volume was stable or even decreased. The magnified inspiratory Δ up we observed should be ascribed to the increase in diastolic pressure induced by the pleural pressure increase. The mechanism of pleural pressure transmission may further explain the higher coefficient of correlation between the systolic arterial pressure variation, taken as the dependent variable, and the pleural pressure compared with the stroke volume.
This experimental study suffers some limitations that preclude any extension to clinical situations without caution. First, our animals had normal pulmonary and cardiac functions before the IAP increase, whereas it was reported, at least in experimental conditions, that an increase in IAP induced a worsening of oedema in previously injured lungs [17]. Our study confirmed that an increase in IAP could deteriorate pulmonary gas exchange in previously healthy lungs; in this respect, the putative protective role of positive end-expiratory pressure was not evaluated. Second, the sequences of IAP increases and of the volaemic periods were not randomized. The increase in IAP as well as the volaemic status is likely to modify the systemic vascular resistance by catecholamine activation [10] or by modification of pulmonary gas exchange. The relationship between stroke volume variations and PPV depends on the vascular tone: for the same stroke volume, the higher the vascular tone, the higher the pulse pressure. However, in our study, the stroke volume variations and PPV changed in the same direction, and therefore the variation in arterial tone could have only amplified the increase in PPV in respect of the increase in stroke volume variations, or could have magnified the observed difference between the normovolaemic and hypovolaemic animals. Third, although the IAP dependency of respiratory variations in arterial pressure was evidenced, we may expect that the animals would have been fluid responsive if a fluid challenge had been performed as a relative redistribution of intravascular volume might have occurred.
In conclusion, the present animal studies showed that the changes in arterial pressure and inferior vena cava flow induced by positive-pressure ventilation are dependent on the IAP. This dependency was more pronounced in the case of hypovolaemia. This finding does not preclude any direct assessment of fluid responsiveness by SPV in the case of increased IAP, as a relative redistribution of intravascular volume might have occurred.
References
Pinsky M (1998) Hemodynamic effects of ventilation and ventilatory maneuvers, In: Marini J, Slutsky A (eds) Respiratory–circulation interactions in health and disease. Edited by. Dekker, New York, pp 183–218
Morgan BC, Martin WE, Hornbein TF, Crawford EW, Guntheroth WG (1966) Hemodynamic effects of intermittent positive pressure respiration. Anesthesiology 27:584–590
Jardin F, Farcot JC, Gueret P, Prost JF, Ozier Y, Bourdarias JP (1983) Cyclic changes in arterial pulse during respiratory support. Circulation 68:266–274
Perel A, Pizov R, Cotev S (1987) Systolic blood pressure variation is a sensitive indicator of hypovolemia in ventilated dogs subjected to graded hemorrhage. Anesthesiology 67:498–502
Tavernier B, Makhotine O, Lebuffe G, Dupont J, Scherpereel P (1998) Systolic pressure variation as a guide to fluid therapy in patients with sepsis-induced hypotension. Anesthesiology 89:1313–1321
Coriat P, Vrillon M, Perel A, Baron JF, Le Bret F, Saada M, Viars P (1994) A comparison of systolic blood pressure variations and echocardiographic estimates of end-diastolic left ventricular size in patients after aortic surgery. Anesth Analg 78:46–53
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky MR, Teboul JL (2000) Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 162:134–138
Feissel M, Michard F, Mangin I, Ruyer O, Faller JP, Teboul JL (2001) Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest 119:867–873
Malbrain ML, Chiumello D, Pelosi P, Wilmer A, Brienza N, Malcangi V, Bihari D, Innes R, Cohen J, Singer P, Japiassu A, Kurtop E, De Keulenaer BL, Daelemans R, Del Turco M, Cosimini P, Ranieri M, Jacquet L, Laterre PF, Gattinoni L (2004) Prevalence of intra-abdominal hypertension in critically ill patients: a multicentre epidemiological study. Intensive Care Med 30:822–829
Vivier E, Metton O, Piriou V, Lhuillier F, Cottet-Emard JM, Branche P, Duperret S, Viale JP (2006) Effects of increased intra-abdominal pressure on central circulation. Br J Anaesth 96:701–707
Fischer L, Van Belle G (1993) Biostatistics: a methodology for the health sciences. Wiley, New York
Perel A (1998) Assessing fluid responsiveness by the systolic pressure variation in mechanically ventilated patients. Systolic pressure variation as a guide to fluid therapy in patients with sepsis-induced hypotension. Anesthesiology 89:1309–1310
Magder S (2004) Clinical usefulness of respiratory variations in arterial pressure. Am J Respir Crit Care Med 169:151–155
Takata M, Wise RA, Robotham JL (1990) Effects of abdominal pressure on venous return: abdominal vascular zone conditions. J Appl Physiol 69:1961–1972
Theres H, Binkau J, Laule M, Heinze R, Hundertmark J, Blobner M, Erhardt W, Baumann G, Stangl K (1999) Phase-related changes in right ventricular cardiac output under volume-controlled mechanical ventilation with positive end-expiratory pressure. Crit Care Med 27:953–958
Barbier C, Loubieres Y, Schmit C, Hayon J, Ricome JL, Jardin F, Vieillard-Baron A (2004) Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med 30:1740–1746
Quintel M, Pelosi P, Caironi P, Meinhardt JP, Luecke T, Herrmann P, Taccone P, Rylander C, Valenza F, Carlesso E, Gattinoni L (2004) An increase of abdominal pressure increases pulmonary edema in oleic acid-induced lung injury. Am J Respir Crit Care Med 169:534–541
Reuter DA, Bayerlein J, Goepfert MS, Weis FC, Kilger E, Lamm P, Goetz AE (2003) Influence of tidal volume on left ventricular stroke volume variation measured by pulse contour analysis in mechanically ventilated patients. Intensive Care Med 29:476–480
Michard F, Teboul JL, Richard C (2003) Influence of tidal volume on stroke volume variation. Does it really matter? Intensive Care Med 29:1613
De Backer D, Heenen S, Piagnerelli M, Koch M, Vincent JL (2005) Pulse pressure variations to predict fluid responsiveness: influence of tidal volume. Intensive Care Med 31:517–523
Denault AY, Gasior TA, Gorcsan J 3rd, Mandarino WA, Deneault LG, Pinsky MR (1999) Determinants of aortic pressure variation during positive-pressure ventilation in man. Chest 116:176–186
Acknowledgements
The authors thank Florence Arnal and Sylviane Conti, research technicians, UPRES EA 1896, Faculté de médecine, Rockefeller, Lyon, France for excellent technical assistance, and A. Vieillard Baron for his helpful comments.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-006-0413-1
Rights and permissions
About this article
Cite this article
Duperret, S., Lhuillier, F., Piriou, V. et al. Increased intra-abdominal pressure affects respiratory variations in arterial pressure in normovolaemic and hypovolaemic mechanically ventilated healthy pigs. Intensive Care Med 33, 163–171 (2007). https://doi.org/10.1007/s00134-006-0412-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0412-2