Abstract
Objective
We sought to evaluate the efficacy of a limited training dedicated to residents without knowledge in ultrasound for performing goal-oriented echocardiography in ICU patients.
Design
Prospective pilot observational study.
Setting
Medical-surgical ICU of a teaching hospital.
Patients
61 consecutive adult ICU patients (SAPS II score: 38 ± 17; 46 ventilated patients) requiring a transthoracic echocardiography were studied.
Interventions
After a curriculum including a 3-h training course and 5 h of hands-on training, one of four noncardiologist residents and an intensivist experienced in ultrasound subsequently performed hand-held echocardiography (HHE), independently and in random order. Assessable “rule in, rule out” clinical questions were purposely limited to easily identifiable conditions by the sole use of two-dimensional imaging.
Measurements and results
When compared with residents, the experienced intensivist performed shorter examinations (4 ± 1 vs. 11 ± 4 min: p < 0.0001) and had significantly less unsolved clinical questions [3 (0.8%) vs. 27 (7.4%) of 366 clinical questions: p < 0.0001]. When addressed, clinical questions were adequately appraised by residents: left ventricular systolic dysfunction [Kappa: 0.76 ± 0.09 (95% CI: 0.59–0.93)], left ventricular dilatation [Kappa: 0.66 ± 0.12 (95% CI: 0.43–0.90)], right ventricular dilatation [Kappa: 0.71 ± 0.12 (95% CI: 0.46–0.95)], pericardial effusion [Kappa: 0.68 ± 0.18 (95 CI: 0.33–1.03)], and pleural effusion [Kappa: 0.71 ± 0.09 (95% CI: 0.53–0.88)]. The only case of tamponade was accurately diagnosed by the resident.
Conclusions
Limited training of noncardiologist ICU residents without previous knowledge in ultrasound appears feasible and efficient to address simple clinical questions using point-of-care echography. Influence of the learning curve on diagnostic accuracy and potential therapeutic impact remain to be determined.
Similar content being viewed by others
Introduction
Echocardiography constitutes an unparalleled imaging modality that provides structural and functional information on the heart and great vessels at patient bedside. Ease of use, portability, and accuracy account for the diffusion of this diagnostic tool in intensive care units (ICUs) [1]. Continuous progress in electronics allowed the recent emergence of small, battery-operated, low-cost, and highly portable devices. Hand-held echocardiography (HHE) has been recently validated in the ICU for simple diagnoses based on two-dimensional imaging [2, 3].
Leading academic teams in cardiology have recently reported their successful experience in developing focused training in echocardiography for medical residents without previous experience in ultrasound [4], but this approach has yet been scarcely evaluated in adult ICU patients [5]. Accordingly, we sought to evaluate the efficacy of a limited training dedicated to residents without previous knowledge in ultrasound for performing goal-oriented echocardiography in critically ill patients using a hand-held system.
Materials and methods
This study was approved by our regional Ethics Committee that waived the need for informed consent.
Focused training
Under the supervision of an experienced intensivist with level-III competence in echocardiography [6], four noncardiologist residents (anesthesiologists, n = 2; internal medicine, n = 2) without previous experience in ultrasound underwent a 3-h training course and 5 h of hands-on training. This focused training was adapted from a previously validated curriculum [7]. The number of assessable clinical questions was purposely limited to easily identifiable conditions by the sole use of two-dimensional imaging (Table 1). Courses were focused on the description of standard echocardiographic views and normal anatomy, and on the identification of gross pathologic changes (e. g., dilated hypokinetic left ventricle, dilated right ventricle, pericardial effusion and tamponade, pleural effusion) using digital loops. Hands-on sessions were performed on sedated patients under ventilator (10–12 examinations per resident) and particular attention was directed toward: (a) obtaining adequate windows and proper orientation in the subcostal, apical four-chamber, and parasternal long and short axis views; (b) identifying correctly anatomic landmarks in corresponding echocardiographic views; and (c) diagnosing accurately all pathologic features covered during courses.
Patients
After completion of the focused training and during a 2-month period, all patients who required a transthoracic echocardiography were examined subsequently by one of the residents and by same trained level-III intensivist, in random order depending on respective availability, but within a 1-h time frame. Indication for echocardiography was left to the discretion of the attending physician, according to standard care in our ICU. In each patient, operators attempted to answer the following “rule in, rule out” clinical questions: presence of a left ventricular (LV) systolic dysfunction (eye-ball evaluated ejection fraction ≤ 50%), LV dilatation, right ventricular (RV) dilatation (cor pulmonale), uncomplicated pericardial effusion or tamponade, and presence of pleural effusion. In case of undetermined interpretation due to suboptimal imaging quality (i. e., absence of clear visualization of all anatomical structures), the corresponding clinical question was considered not addressed. Both the residents and experienced intensivist had access to the same information regarding the medical history and clinical status of patients but performed HHE and fulfilled the case report forms independently.
Point-of-care echocardiography
Examinations were performed using a hand-held device with two-dimensional capability (Optigo, Philips, France). Color Doppler mapping was purposely not used. Each patient was systematically screened for the four studied echocardiographic windows. The number of acoustic windows obtained was recorded and global imaging quality was graded as follows: 0, no image; 1, poor imaging quality (identification of < 50% of left endocardial borders); 2, good imaging quality (identification of > 50% of LV endocardial borders); 3, excellent imaging quality (identification of the entire LV endocardial borders). In the presence of a pleural effusion, the maximal interpleural distance was measured, as previously described [8]. Values greater than 45 mm and 50 mm for right- and left-sided effusions, respectively, were indicative for large pleural effusions [8]. Since the Optigo system does not allow video or digital loop recording, interpretation of HHE and two-dimensional measurements were performed on-line by operators at bedside. The time required to perform the examination was noted.
Statistics
The number of acoustic windows and proportion of addressed questions were compared between residents and the experienced intensivist using the MacNemar test. Imaging quality graded by these operators and duration of HHE study were compared using a Wilcoxon test. Agreement between responses to clinical questions provided by the residents and the experienced intensivist was assessed using the Cohen's Kappa coefficient [9]. Agreement between echocardiographic measurements performed by investigators was assessed by the intraclass correlation coefficient [10]. In both cases, 95% confidence intervals (95% CI) were also calculated.
Results
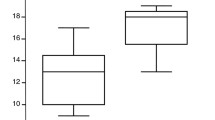
Sixty-one patients underwent a point-of-care examination [age (mean ± SD): 64 ± 14 years; SAPS II score: 38 ± 17; 46 ventilated patients]. Patients were admitted to the ICU for a medical condition (n = 51), complicated surgery (n = 7), or a multisystem trauma (n = 3). Residents performed a mean of 15 HHE studies (range: 11–20). When compared with residents, the experienced intensivist performed shorter examinations (4 ± 1 vs. 11 ± 4 min: p < 0.0001) with more acoustic windows (200 vs. 221 of 244 potential windows: p = 0.0018) and better imaging quality (mean grade, 1.95 ± 0.76 vs. 1.75 ± 0.66: p < 0.0001). The trained intensivist had significantly less unaddressed clinical questions than residents [3 (0.8%) vs. 27 (7.4%) of 366 clinical questions: p < 0.0001].
When addressed, clinical questions were adequately appraised by residents as reflected by the agreement of their qualitative diagnoses with those of the experienced intensivist (Table 2). Residents assessed inadequately LV systolic function in 7 of 58 patients (12%). In all discrepant cases, LV systolic function was considered moderately depressed instead of normal by either the resident or the experienced intensivist. The RV dilatation was not accurately identified by residents in 5 of 56 patients (9%). A single resident accounted for three of the four discrepant negative results. Pericardial effusions were correctly diagnosed by residents (Table 2). The two discrepant positive results were attributable to the presence of fat along the free wall of the RV in the subcostal view which was erroneously interpreted as a mild pericardial effusion, whereas a trivial effusion without clinical relevance was only identified by the experienced intensivist in a hemodynamically stable patient. The only case of tamponade encountered in this study was accurately diagnosed by the resident. Similarly, residents correctly diagnosed pleural effusions using pleural ultrasonography (Table 2) and adequately identified large volumes of effusion [Kappa: 0.67 ± 0.18 (95% CI: 0.33–1.02)]. Intraclass correlation coefficient was 0.89 (95% CI: 0.67–0.97) and 0.81 (95% CI: 0.60–0.92) for the measurement of left and right maximal interpleural distances, respectively.
Discussion
The present pilot study shows that an 8-h focused training program allowed noncardiologist residents to efficiently use HHE for the identification of gross cardiac changes and pleural effusions. In the current study, eye-ball identification of global LV systolic dysfunction by residents was fairly accurate, as previously reported in adult patients [11–15] and in pediatric patients [16, 17]. In keeping with previous results [17], a focused training program allowed the identification of dilated LV cavity by residents in our ICU patients. Similarly, residents adequately identified the presence of a RV dilatation, as recently shown when using transesophageal echocardiography by novice intensivists [18]. As previously reported [14, 17], residents correctly identified the presence of pericardial effusion and the single case of tamponade diagnosed in the present study. In the specific setting of patients sustaining life-threatening tamponade, HHE appears ideally suited for prompt recognition and to guide rapid pericardiocentesis [19]. In the present study, residents identified satisfactorily the presence of large pleural effusion [8], as reflected by fairly high intraclass coefficient correlations for the measurement of interpleural distance.
The training curriculum proposed to medical residents without previous experience in ultrasound for goal-oriented point-of-care echocardiography varied widely among studies [4]. The beneficial effect of a tailored training program on the diagnostic accuracy of HHE users has been documented [7, 15]. With a mean of 15 HHE examinations performed in the current study, the residents were presumably on the ascending part of their learning curve. Accordingly, improvement of the promising results reported in this pilot study is anticipated with accumulated experience by noncardiologist residents. Importantly, the present results cannot be extended to other indications of echocardiography (e. g., evaluation of complex shock) which require a higher level of training [20] and frequently a transesophageal examination [1].
The present study has several limitations. Firstly, the relatively low number of enrolled patients and participating trainees did not allow for evaluating the effect of the learning curve on individual diagnostic accuracy among trained residents. Secondly, two-dimensional measurements of ventricular end-diastolic diameters were not performed to help operators to more objectively identify left or right ventricular dilatation. Thirdly, the potential impact of point-of-care echocardiography on therapy was not evaluated. Fourthly, we used HHE with no spectral Doppler capability and limited setting possibilities (depth of image and gain) to facilitate ultrasound instrument settings. Nevertheless, the present data can presumably be extended to two-dimensional imaging obtained by conventional equipment.
Conclusion
In the ICU environment, limited training of noncardiologist residents without previous knowledge in ultrasound appears feasible and efficient to address simple limited clinical questions using point-of-care echography. The influence of the learning curve on diagnostic accuracy and the potential therapeutic impact of focused echocardiography performed by noncardiologist residents remain to be determined by further studies.
References
Vignon P (2005) Hemodynamic assessment of critically ill patients using echocardiography Doppler. Curr Opin Crit Care 11:227–234
Vignon P, Chastagner C, François B, Normand S, Bonnivard M, Gastinne H (2003) Diagnostic ability of hand-held echocardiography in ventilated critically ill patients. Crit Care 7:R84–R91
Vignon P, Frank MBJ, Lesage J, Mucke F, François B, Normand S, Bonnivard M, Clavel M, Gastinne H (2004) Hand-held echocardiography with spectral Doppler capability for the assessment of critically ill patients: Is it reliable? Intensive Care Med 30:718–723
Duvall WL, Croft LB, Goldman ME (2003) Can hand-carried ultrasound devices be extended for use by the noncardiology medical community? Echocardiography 20:471–476
Manasia AR, Nagaraj HM, Kodali RB, Croft LB, Oropello JM, Kohli-Seth R, Leibowitz AB, DelGiudice R, Hufanda JF, Benjamin E, Goldman ME (2005) Feasibility and potential clinical utility of goal-directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand-carried device (SonoHeart) in critically ill patients. J Cardiothoracic Vasc Anesth 19:155–159
Pearlman AS, Gardin JM, Martin RP, Parisi AF, Popp RL, Quinones MA, Stevenson JG (1987) Guidelines for optimal physician training in echocardiography: recommendations of the American Society of Echocardiography Committee for Physician Training in Echocardiography. Am J Cardiol 60:158–163
Jones AE, Tayal VS, Kline JA (2003) Focused training of emergency medicine residents in goal-directed echocardiography: a prospective study. Acad Emerg Med 10:1054–1058
Vignon P, Chastagner C, Berkane V, Chardac E, François B, Normand S, Bonnivard M, Clavel M, Pichon N, Preux PM, Maubon A, Gastinne H (2005) Quantitative assessment of pleural effusion in critically-ill patients by means of ultrasonography. Crit Care Med 33:1757–1763
Fermanian J (1984) Mesure de l'accord entre deux juges. Cas qualitatif. Rev Epidemiol Santé Publique 32:140–147
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
Kimura BJ, Amundson SA, Willis CL, Gilpin EA, DeMaria AN (2002) Usefulness of hand-held ultrasound device for bedside examination of left ventricular function. Am J Cardiol 90:1038–1039
Rugulotto M, Schnittger I, Liang D (2001) The new generation hand-carried echocardiographs: the Stanford view. Thoraxcentre J 13:100–102
Lemola K, Yamada E, Jagasia D, Kerber RE (2003) A hand-carried personal ultrasound device for rapid evaluation of left ventricular function: use after limited echo training. Echocardiography 20:309–312
Alexander JH, Peterson ED, Chen AY, Harding TM, Adams DB, Kisslo JA (2004) Feasibility of point-of-care echocardiography by internal medicine house staff. Am Heart J 147:476–481
DeCara JM, Lang RM, Koch R, Bala R, Penzotti J, Spencer KT (2003) The use of small personal ultrasound devices by internists without formal training in echocardiography. Eur J Echocardiogr 4:141–147
Pershad J, Myers S, Plouman C, Rosson C, Elam K, Wan J, Chin T (2004) Bedside limited echocardiography by the emergency physician is accurate during evaluation of the critically ill patient. Pediatrics 114:e667–e671
Spurney CF, Sable CA, Berger JT, Martin GR (2005) Use of hand-carried ultrasound device by critical care physicians for the diagnosis of pericardial effusions, decreased cardiac function, and left ventricular enlargement in pediatric patients. J Am Soc Echocardiogr 18:313–319
Vieillard-Baron A, Charron C, Chergui K, Peyrouset O, Jardin F (2006) Bedside echocardiographic evaluation of hemodynamics in sepsis: Is a qualitative evaluation sufficient? Intensive Care Med 32:1547–1552
Osranek M, Bursi F, O'Leary PW, Bruce CJ, Sinak LJ, Chandrasekaran K, Seward JB (2003) Hand-carried ultrasound-guided pericardiocentesis and thoracentesis. J Am Soc Echocardiogr 16:480–484
Vignon P, Guéret P (2004) Formation des réanimateurs à l'échographie cardiaque. Réanimation 13:126–130
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vignon, P., Dugard, A., Abraham, J. et al. Focused training for goal-oriented hand-held echocardiography performed by noncardiologist residents in the intensive care unit. Intensive Care Med 33, 1795–1799 (2007). https://doi.org/10.1007/s00134-007-0742-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0742-8