Abstract
Purpose
The optimal target blood glucose concentration for acute glycemic control remains unclear because few studies have directly compared 144–180 with 110–144 or >180 mg/dL. Accordingly, we performed a network meta-analysis to compare four different target blood glucose levels (<110, 110–144, 144–180, and >180 mg/dL) in terms of the benefit and risk of insulin therapy.
Methods
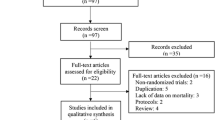
We included all of the studies from three systematic reviews and searched the PubMed and Cochrane databases for other studies investigating glucose targets among critically ill patients. The primary outcome was hospital mortality, and the secondary outcomes were sepsis or bloodstream infection and the risk of hypoglycemia. Network meta-analysis to identify an optimal target glucose concentration.
Results
The network meta-analysis included 18,098 patients from 35 studies. There were no significant differences in the risk of mortality and infection among the four blood glucose ranges overall or in subgroup analysis. Conversely, target concentrations of <110 and 110–144 mg/dL were associated with a four to ninefold increase in the risk of hypoglycemia compared with 144–180 and >180 mg/dL. However, there were no significant differences between the target concentrations of 144–180 and >180 mg/dL.
Conclusions
This network meta-analysis found no significant difference in the risk of mortality and infection among four target blood glucose ranges in critically ill patients, but indicated that target blood glucose levels of <110 and 110–144 mg/dL were associated with a higher risk of hypoglycemia than target levels of 144–180 and >180 mg/dL. Further studies are required to refute or confirm our findings.



Similar content being viewed by others
References
Egi M, Finfer S, Bellomo R (2011) Glycemic control in the ICU. Chest 140:212–220. doi:10.1378/chest.10-1478
van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R (2001) Intensive insulin therapy in critically ill patients. N Engl J Med 345:1359–1367
Krinsley JS (2004) Effect of an intensive glucose management protocol on the mortality of critically ill adult patients. Mayo Clin Proc 79:992–1000
Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, Van Wijngaerden E, Bobbaers H, Bouillon R (2006) Intensive insulin therapy in the medical ICU. N Engl J Med 354:449–461
Wiener RS, Wiener DC, Larson RJ (2008) Benefits and risks of tight glucose control in critically ill adults: a meta-analysis. JAMA 300:933–944. doi:10.1001/jama.300.8.933
Friedrich JO, Chant C, Adhikari NK (2010) Does intensive insulin therapy really reduce mortality in critically ill surgical patients? A reanalysis of meta-analytic data. Crit Care 14:324. doi:10.1186/cc9240
Hermans G, Van den Berghe G (2015) Clinical review: intensive care unit acquired weakness. Crit Care 19:274. doi:10.1186/s13054-015-0993-7
NICE-SUGAR Study Investigators, Finfer S, Liu B, Chittock DR et al (2012) Hypoglycemia and risk of death in critically ill patients. N Engl J Med 367:1108–1118
NICE-SUGAR Study Investigators, Finfer S, Chittock DR, Su SY et al (2009) Intensive versus conventional glucose control in critically ill patients. N Engl J Med 360:1283–1297. doi:10.1056/NEJMoa0810625
Dellinger RP, Levy MM, Rhodes A et al (2013) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 41:580–637. doi:10.1097/CCM.0b013e31827e83af
Jacobi J, Bircher N, Krinsley J et al (2012) Guidelines for the use of an insulin infusion for the management of hyperglycemia in critically ill patients. Crit Care Med 40:3251–3276. doi:10.1097/CCM.0b013e3182653269
Song F, Zhong LJ, Han L, Xie GH, Xiao C, Zhao B, Hu YQ, Wang SY, Qin CJ, Zhang Y, Lai DM, Cui P, Fang XM (2014) Intensive insulin therapy for septic patients: a meta-analysis of randomized controlled trials. Biomed Res Int 2014:698265. doi:10.1155/2014/698265
Skapinakis P, Caldwell DM, Hollingworth W, Bryden P, Fineberg NA, Salkovskis P, Welton NJ, Baxter H, Kessler D, Churchill R, Lewis G (2016) Pharmacological and psychotherapeutic interventions for management of obsessive–compulsive disorder in adults: a systematic review and network meta-analysis. Lancet Psychiatry. doi:10.1016/S2215-0366(16)30069-4
Singh JA, Hossain A, Tanjong Ghogomu E, Kotb A, Christensen R, Mudano AS, Maxwell LJ, Shah NP, Tugwell P, Wells G (2016) Biologics or tofacitinib for rheumatoid arthritis in incomplete responders to methotrexate or other traditional disease-modifying anti-rheumatic drugs: a systematic review and network meta-analysis. Cochrane Database Syst Rev 13:CD012183. doi:10.1002/14651858.CD012183
Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G (2013) Graphical tools for network meta-analysis in STATA. PLoS One 8:e76654. doi:10.1371/journal.pone.0076654.eCollection
Higgins JPT, Green S (eds) (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration, 2011. http://www.cochrane-handbook.org. Accessed March 2011
Plummer M (2016) rjags: Bayesian graphical models using MCMC. R package version 4–6. http://CRAN.R-project.org/package=rjags
van Valkenhoef G, Kuiper J (2016) gemtc: network meta-analysis using Bayesian methods. R package version 0.8. http://CRAN.R-project.org/package=gemtc
Shyangdan DS, Uthman OA, Waugh N (2016) SGLT-2 receptor inhibitors for treating patients with type 2 diabetes mellitus: a systematic review and network meta-analysis. BMJ Open 6:e009417. doi:10.1136/bmjopen-2015-009417
Li T, Puhan MA, Vedula SS, Singh S, Dickersin K, Ad Hoc Network Meta-analysis Methods Meeting Working Group (2011) Network meta-analysis-highly attractive but more methodological research is needed. BMC Med 9:79. doi:10.1186/1741-7015-9-79
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Yin S, Zhang D, Du H, Du H, Yin Z, Qiu Y (2015) Is there any difference in survivorship of total hip arthroplasty with different bearing surfaces? A systematic review and network meta-analysis. Int J Clin Exp Med 8:21871–21885
Grey NJ, Perdrizet GA (2004) Reduction of nosocomial infections in the surgical intensive-care unit by strict glycemic control. Endocr Pract 10(Suppl 2):46–52
Bilotta F, Spinelli A, Giovannini F, Doronzio A, Delfini R, Rosa G (2007) The effect of intensive insulin therapy on infection rate, vasospasm, neurologic outcome, and mortality in neurointensive care unit after intracranial aneurysm clipping in patients with acute subarachnoid hemorrhage: a randomized prospective pilot trial. J Neurosurg Anesthesiol 19:156–160
Bilotta F, Caramia R, Cernak I, Paoloni FP, Doronzio A, Cuzzone V, Santoro A, Rosa G (2008) Intensive insulin therapy after severe traumatic brain injury: a randomized clinical trial. Neurocrit Care 9:159–166. doi:10.1007/s12028-008-9084-9
Bland DK, Fankhanel Y, Langford E, Lee M, Lee SW, Maloney C, Rogers M, Zimmerman G (2005) Intensive versus modified conventional control of blood glucose level in medical intensive care patients: a pilot study. Am J Crit Care 14:370–376
Walters MR, Weir CJ, Lees KR (2006) A randomised, controlled pilot study to investigate the potential benefit of intervention with insulin in hyperglycaemic acute ischaemic stroke patients. Cerebrovasc Dis 22:116–122
Bruno A, Kent TA, Coull BM, Shankar RR, Saha C, Becker KJ, Kissela BM, Williams LS (2008) Treatment of hyperglycemia in ischemic stroke (THIS): a randomized pilot trial. Stroke 39:384–389
Mitchell I, Knight E, Gissane J, Tamhane R, Kolli R, Leditschke IA, Bellomo R, Finfer S (2006) Australian and New Zealand Intensive Care Society Clinical Trials Group. A phase II randomised controlled trial of intensive insulin therapy in general intensive care patients. Crit Care Resusc 8:289–293
Brunkhorst FM, Engel C, Bloos F et al (2008) Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 358:125–139. doi:10.1056/NEJMoa070716
Iapichino G, Albicini M, Umbrello M, Sacconi F, Fermo I, Pavlovich R, Paroni R, Bellani G, Mistraletti G, Cugno M, Pesenti A, Gattinoni L (2008) Tight glycemic control does not affect asymmetric-dimethylarginine in septic patients. Intensive Care Med 34:1843–1850. doi:10.1007/s00134-008-1158-9
De La Rosa Gdel C, Donado JH, Restrepo AH et al (2008) Strict glycaemic control in patients hospitalised in a mixed medical and surgical intensive care unit: a randomised clinical trial. Crit Care 12:R120. doi:10.1186/cc7017
Arabi YM, Dabbagh OC, Tamim HM, Al-Shimemeri AA, Memish ZA, Haddad SH, Syed SJ, Giridhar HR, Rishu AH, Al-Daker MO, Kahoul SH, Britts RJ, Sakkijha MH (2008) Intensive versus conventional insulin therapy: a randomized controlled trial in medical and surgical critically ill patients. Crit Care Med 36:3190–3197. doi:10.1097/CCM.0b013e31818f21aa
Chan RP, Galas FR, Hajjar LA, Bello CN, Piccioni MA, Auler JO Jr (2009) Intensive perioperative glucose control does not improve outcomes of patients submitted to open-heart surgery: a randomized controlled trial. Clinics (Sao Paulo) 64:51–60
Farah R, Samokhvalov A, Zviebel F, Makhoul N (2007) Insulin therapy of hyperglycemia in intensive care. Isr Med Assoc J 9:140–142
Henderson WR, Dhingra V, Chittock D, Foster D, Hebert P, Cook D, Heyland D, Dodek P, Griesdale D, Schulzer M, Ronco JJ, Canadian Critical Trials Group (2009) The efficacy and safety of glucose control algorithms in intensive care: a pilot study of the Survival Using Glucose Algorithm Regulation (SUGAR) trial. Pol Arch Med Wewn 119:439–446
COIITSS Study Investigators, Annane D, Cariou A, Maxime V et al (2010) Corticosteroid treatment and intensive insulin therapy for septic shock in adults: a randomized controlled trial. JAMA 303:341–348. doi:10.1001/jama.2010.2
Savioli M, Cugno M, Polli F, Taccone P, Bellani G, Spanu P, Pesenti A, Iapichino G, Gattinoni L (2009) Tight glycemic control may favor fibrinolysis in patients with sepsis. Crit Care Med 37:424–431. doi:10.1097/CCM.0b013e31819542da
Cappi SB, Noritomi DT, Velasco IT, Curi R, Loureiro TC, Soriano FG (2012) Dyslipidemia: a prospective controlled randomized trial of intensive glycemic control in sepsis. Intensive Care Med 38:634–641. doi:10.1007/s00134-011-2458-z
Preiser JC, Devos P, Ruiz-Santana S, Mélot C, Annane D, Groeneveld J, Iapichino G, Leverve X, Nitenberg G, Singer P, Wernerman J, Joannidis M, Stecher A, Chioléro R (2009) A prospective randomised multi-centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med 35:1738–1748. doi:10.1007/s00134-009-1585-2
McMullin J, Brozek J, McDonald E, Clarke F, Jaeschke R, Heels-Ansdell D, Leppert R, Foss A, Cook D (2007) Lowering of glucose in critical care: a randomized pilot trial. J Crit Care 22:112–118 (discussion 118–119)
Oksanen T, Skrifvars MB, Varpula T, Kuitunen A, Pettilä V, Nurmi J, Castrén M (2007) Strict versus moderate glucose control after resuscitation from ventricular fibrillation. Intensive Care Med 33:2093–2100
de Azevedo JR, de Araujo LO, da Silva WS, de Azevedo RP (2010) A carbohydrate-restrictive strategy is safer and as efficient as intensive insulin therapy in critically ill patients. J Crit Care 25:84–89. doi:10.1016/j.jcrc.2008.10.011
Mackenzie IM, Ercole A, Ingle S, Palmer CR (2008) Glycaemic control and outcome in general intensive care: the East Anglian GLYCOGENIC study. Br J Intensive Care 18:121–126
Davies RR, Newton RW, McNeill GP, Fisher BM, Kesson CM, Pearson D (1991) Metabolic control in diabetic subjects following myocardial infarction: difficulties in improving blood glucose levels by intravenous insulin infusion. Scott Med J 36:74–76
Arabi YM, Tamim HM, Dhar GS, Al-Dawood A, Al-Sultan M, Sakkijha MH, Kahoul SH, Brits R (2011) Permissive underfeeding and intensive insulin therapy in critically ill patients: a randomized controlled trial. Am J Clin Nutr 93:569–577. doi:10.3945/ajcn.110.005074
Bilotta F, Caramia R, Paoloni FP, Delfini R, Rosa G (2009) Safety and efficacy of intensive insulin therapy in critical neurosurgical patients. Anesthesiology 110:611–619. doi:10.1097/ALN.0b013e318198004b
Kalfon P, Giraudeau B, Ichai C, Guerrini A, Brechot N, Cinotti R, Dequin PF, Riu-Poulenc B, Montravers P, Annane D, Dupont H, Sorine M, Riou B, CGAO-REA Study Group (2014) Tight computerized versus conventional glucose control in the ICU: a randomized controlled trial. Intensive Care Med 40:171–181. doi:10.1007/s00134-013-3189-0
Hsu CW, Sun SF, Lin SL, Huang HH, Wong KF (2012) Moderate glucose control results in less negative nitrogen balances in medical intensive care unit patients: a randomized, controlled study. Crit Care 16:R56. doi:10.1186/cc11299
Coester A, Neumann CR, Schmidt MI (2010) Intensive insulin therapy in severe traumatic brain injury: a randomized trial. J Trauma 68:904–911. doi:10.1097/TA.0b013e3181c9afc2
Mahmoodpoor A, Ali-Asgharzadeh A, Parish M, Amir-Aslanzadeh Z, Abedini A (2011) A comparative study of efficacy of intensive insulin therapy versus conventional method on mortality and morbidity of critically ill patients. Pak J Med Sci 27:496–499
Green DM, O’Phelan KH, Bassin SL, Chang CW, Stern TS, Asai SM (2010) Intensive versus conventional insulin therapy in critically ill neurologic patients. Neurocrit Care 13:299–306. doi:10.1007/s12028-010-9417-3
Giakoumidakis K, Eltheni R, Patelarou E, Theologou S, Patris V, Michopanou N, Mikropoulos T, Brokalaki H (2013) Effects of intensive glycemic control on outcomes of cardiac surgery. Heart Lung 42:146–151. doi:10.1016/j.hrtlng.2012.12.007
Okabayashi T, Shima Y, Sumiyoshi T, Kozuki A, Tokumaru T, Iiyama T, Sugimoto T, Kobayashi M, Yokoyama M, Hanazaki K (2014) Intensive versus intermediate glucose control in surgical intensive care unit patients. Diabetes Care 37:1516–1524. doi:10.2337/dc13-1771
American Diabetes Association (2012) Standards of medical care in diabetes–2012. Diabetes Care 35(Suppl 1):S11–S63. doi:10.2337/dc12-s011
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Take-home message: This network meta-analysis suggested (a) that there was no significant difference in the risk of mortality and infection among the four blood glucose ranges evaluated and (b) that targets of <110 and 110–144 mg/dL were associated with a four to ninefold increase in the risk of hypoglycemia compared with 144–180 and >180 mg/dL. There were no significant differences in the risk of hypoglycemia between the 144–180 and >180 mg/dL target blood glucose levels.
Electronic supplementary material
Below is the link to the electronic supplementary material.
134_2016_4558_MOESM3_ESM.tiff
Supplementary material 3 Risk of bias in the included randomized controlled trials. The Cochrane Collaboration tool was used to assess the risk of bias. The authors’ judgments were used to assign the risk of bias for each included study. +, low risk of bias; −, high risk of bias; empty space, unclear risk of bias. Eight studies with a high risk of “other bias” did not provide financial support and/or conflict of interest statements (TIFF 2456 kb)
134_2016_4558_MOESM4_ESM.tiff
Supplementary material 4 The network of all eligible comparisons for the meta-analysis. a In-hospital mortality, b incidences of sepsis or bloodstream infection and c incidences of hypoglycemia. Each node (circle) corresponds to a target blood glucose range. Each line represents a direct comparison between the target ranges, and the width of the line is proportional to the number of studies that compared each target pair. N number of studies (TIFF 3199 kb)
134_2016_4558_MOESM6_ESM.tif
Supplementary material 6 Forest plot for network meta-analysis based on the actual achieved mean glycemic levels. The upper row indicates the pairwise meta-analysis result (blue) and the lower row indicates the network meta-analysis result (black) (TIFF 1541 kb)
134_2016_4558_MOESM7_ESM.tiff
Supplementary material 7 Results of the network analysis comparing the 110–144 and 144–180 mg/dL target blood glucose levels. The circles correspond to the odds ratio and the black horizontal lines correspond to the 95 % credible intervals (TIFF 984 kb)
Rights and permissions
About this article
Cite this article
Yatabe, T., Inoue, S., Sakaguchi, M. et al. The optimal target for acute glycemic control in critically ill patients: a network meta-analysis. Intensive Care Med 43, 16–28 (2017). https://doi.org/10.1007/s00134-016-4558-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-016-4558-2