Abstract
Purpose
Central venous pressure (CVP) has been shown to have poor predictive value for fluid responsiveness in critically ill patients. We aimed to re-evaluate this in a larger sample subgrouped by baseline CVP values.
Methods
In April 2015, we systematically searched and included all clinical studies evaluating the value of CVP in predicting fluid responsiveness. We contacted investigators for patient data sets. We subgrouped data as lower (<8 mmHg), intermediate (8–12 mmHg) and higher (>12 mmHg) baseline CVP.
Results
We included 51 studies; in the majority, mean/median CVP values were in the intermediate range (8–12 mmHg) in both fluid responders and non-responders. In an analysis of patient data sets (n = 1148) from 22 studies, the area under the receiver operating curve was above 0.50 in the <8 mmHg CVP group [0.57 (95 % CI 0.52–0.62)] in contrast to the 8–12 mmHg and >12 mmHg CVP groups in which the lower 95 % CI crossed 0.50. We identified some positive and negative predictive value for fluid responsiveness for specific low and high values of CVP, respectively, but none of the predictive values were above 66 % for any CVPs from 0 to 20 mmHg. There were less data on higher CVPs, in particular >15 mmHg, making the estimates on predictive values less precise for higher CVP.
Conclusions
Most studies evaluating fluid responsiveness reported mean/median CVP values in the intermediate range of 8–12 mmHg both in responders and non-responders. In a re-analysis of 1148 patient data sets, specific lower and higher CVP values had some positive and negative predictive value for fluid responsiveness, respectively, but predictive values were low for all specific CVP values assessed.
Similar content being viewed by others
Introduction
Fluid therapy is a key intervention in optimizing the cardiovascular status in critically ill patients [1]. Previous studies have shown that only 50 % of patients respond to fluid administration with an increase in stroke volume (SV) or cardiac output (CO), so-called fluid responsiveness [2]. The ability to discriminate between fluid responders and non-responders is important, as fluid overload may be associated with increased mortality in critically ill patients [3].
Central venous pressure (CVP) continues to be widely used in guiding fluid therapy [4, 5] and is recommended to guide fluid therapy in patients with septic shock [6]. However, systematic reviews of the literature have concluded that CVP has no predictive value for fluid responsiveness in critically ill patients [7, 8]. The latter observations may be in conflict with the physiological rationale according to which extreme values of CVP would be expected to have some predictive value even if CVP may be considered the downstream pressure of venous return rather than a measure of preload [5]. Along this line, a recent consensus statement recommended immediate fluid resuscitation in shock states associated with very low levels of preload parameters (e.g. CVP) [9].
In the study reports on fluid responsiveness it is often difficult to read the number of patients having extreme values of CVP, because overall median or average values are presented. Given the context of clinical research in critically ill patients, it may be that patients who were obviously hypo- or hypervolaemic were less likely to be included in the studies assessing fluid responsiveness. A number of studies, and in particular the smaller ones, may therefore have included few patients with extreme values. If so this may have contributed to the observed poor predictive values of CVP for fluid responsiveness.
The aim of our systematic review was to re-evaluate the predictive value of CVP for fluid responsiveness by reassessing and reanalysing the reported data and individual patient data on the basis of baseline values of CVP.
Methods
Two authors (T.G.E. and M.W.) searched PubMed and Embase individually to identify all relevant studies investigating fluid responsiveness including CVP as a parameter. The following search string was used:
-
1.
CVP OR central venous pressure OR CVC OR central venous cath*
-
2.
Fluid responsiveness OR fluid OR fluid status OR fluid therapy OR volume OR volume status OR responsiveness OR resuscitation OR PLR OR passive leg raising
-
3.
#1 AND #2
Study selection
The search was restricted to hospitalised patients. No restrictions were made regarding language, patient categories or study settings. The search was done in December 2014 and updated in April 2015. Identified studies were screened on title, abstract or both by two authors (T.G.E. and M.W.). All potentially relevant studies were evaluated in full text. Bibliographies of included studies were reviewed for further relevant studies. The inclusion criteria of studies were (1) clinical setting, (2) adult patients, (3) performance of at least one fluid loading, (4) baseline CVP values reported, (5) evaluation of fluid responsiveness and (6) CVP data presented discriminating fluid responders from non-responders. Doubts regarding inclusion or exclusion of studies were resolved with the senior author (A.P.).
Data extraction
Two authors (T.G.E. and M.W.) extracted the data independently using a standardised form (Tables 2 and 3 in the supplementary material). The extracted data included (1) patient population, (2) number of patients, (3) potential exclusion criterion based on a certain CVP value, (4) the technique used to define fluid responsiveness, (5) definition of fluid responsiveness, (6) method used to induce a change in preload, (7) potential type of fluid and fluid volume, (8) body position, (9) use of ventilation and (10) key results. The corresponding authors of all included studies were contacted by e-mail requesting the individual patient’s baseline CVP data grouped by fluid responders and non-responders.
From the studies from which we received individual patient data we extracted the following quality indicators of CVP measurements: levelling, zeroing, dealing with respiratory variations, CVP measured at end expiration, excluding patients recruiting expiratory muscles or giving muscle relaxants, and if CVP was a measured value of the trace rather than a registered value of a monitor.
Statistical analyses
We subgrouped studies and individual patient data sets on the basis of baseline CVP values (mean/median for the studies) as lower (<8 mmHg), intermediate (8–12 mmHg) and higher (>12 mmHg) CVP groups (these cut-off points have been used to guide fluid therapy [10]) and on the basis of setting [operating room patients or intensive care unit (ICU) or other patients].
We compared the area under the receiver operating characteristics curves (AUC-ROC) for the individual patient data sets grouped as lower, intermediate and higher CVP values using GraphPad Prism 6 (GraphPad Software Inc.). We calculated positive and negative predictive values and likelihood ratios with 95 % confidence intervals (CI) for specific CVP cut-off points in the range 0–20 mmHg.
We performed sensitivity analyses of studies including ICU patients, studies including solely mechanically ventilated patients, studies reporting to have included observations on changes in CVP due to the fluid challenge, studies reporting the timing of the CO/SV measurement after the fluid challenge, studies reporting three or more of the quality indicators for CVP measurements and studies using thermo- or lithium dilution or oesophageal Doppler to define fluid responsiveness as these methods may be considered clinical reference methods for detecting changes in SV and CO during fluid loading [11].
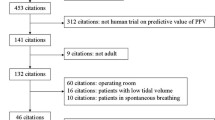
Results
The search resulted in 4767 unique citations: 135 studies were reviewed in full text and 51 studies were included, the majority of which were done in the ICU and in the operating room (Fig. 1; Table 1 and Tables 1–3 in the supplementary material).
In the majority of studies, the patients were mechanically ventilated [12–50] with tidal volumes varying from 5 to 12 ml/kg. In nine studies mixed populations of mechanically ventilated and non-ventilated patients were included [51–59], and in one study non-ventilated patients were included [60]. In two studies (4 %) patients were excluded if they had high CVP values or other signs of hypervolaemia, and in two studies (4 %) patients were excluded if they had low CVP values.
In most of the studies colloid solutions were used to induce the change in preload, and 500 ml was given [18, 19, 23, 24, 27–31, 34, 35, 37–41, 43, 44, 52, 57, 58, 60]; in the remaining studies fluid volumes varied between 100 and 1500 ml [14, 21, 47, 51, 53, 54, 56, 61], 6–10 ml/kg [12, 13, 22, 32, 33, 36, 42, 45, 48, 50, 55, 62] or 10–20 ml × BMI [15, 26]. A few studies used passive leg raising [16, 17, 25, 59] to induce the change in preload.
In most studies fluid responsiveness was defined as a change in SV or CO as measured by thermodilution, but a variety of methods were used as reference technique (Table 1).
Analyses of CVP subgroups of reported data
The majority of reported mean/median baseline CVP values in the 51 studies were in the intermediate CVP range (8–12 mmHg) both in ICU and operating room patient groups and in fluid responders and non-responders (Table 1). There were more responders than non-responders in the lower CVP subgroup of studies (<8 mmHg), whereas the opposite was observed in the higher CVP subgroup (>12 mmHg) (Fig. 1 in the supplementary material). Comparable results were observed in the 37 studies using thermo- or lithium dilution or oesophageal Doppler to define fluid responsiveness (Fig. 2 in the supplementary material).
Analyses of individual patient CVP data sets
Investigators of 22 studies including 982 patients [15, 16, 24, 25, 28, 31, 34, 35, 38–40, 43, 44, 47, 48, 52, 54, 55, 59–62] submitted raw baseline CVP data on fluid responders and non-responders resulting in 1148 patient data sets. The 22 studies differed in patient population, reference technique, definition of fluid responsiveness, and fluid type and volume to induce a preload challenge (Table 1).
In ten studies ICU patients were investigated (451 data sets), and in 13 studies (687 data sets) [16, 24, 25, 28, 31, 38, 40, 43, 47, 48, 54, 55, 61] thermo- or lithium dilution or oesophageal Doppler was used to define fluid responsiveness. In 15 studies (727 data sets) mechanically ventilated patients were included, in four studies both mechanically ventilated and spontaneously breathing patients were included, and in one study spontaneously breathing patients were included. No information was provided on mode of ventilation in two studies. Eighteen (938 data sets) out of the 22 studies reported to include observations on changes in CVP due to the fluid challenge, and in 12 studies (845 data sets) the timing of the CO/SV measurement after the fluid challenge was reported. Nineteen studies reported quality indicators for CVP measurements (Table 4 in supplementary material); in eight studies (603 data sets), three or more indicators were reported to have been used.
The median CVP value was 9 mmHg (interquartile range 6–12 mmHg) in the full data set (n = 1148), and 47 % of the CVP values were in the lower CVP subgroup, 30 % in the intermediate subgroup (8–12 mmHg) and 23 % in the higher CVP subgroup. Overall 48 % of the assessments were in fluid responders (551/1148) and 52 % in non-responders (597/1148), and the ratios between responders and non-responders varied depending on baseline CVP subgroup (Fig. 2 and Fig. 3 in the supplementary material).
The AUC-ROCs were 0.57 (95 % CI 0.52–0.62) for the lower CVP subgroup, 0.54 (0.48–0.60) for the intermediate CVP subgroup and 0.56 (0.48–0.63) for the higher CVP subgroup (Fig. 3 and Fig. 4 in the supplementary material). Comparable results were observed using the individual patient data sets from the studies including only patients who were mechanically ventilated, the studies of ICU patients only, the studies using thermo- or lithium dilution or oesophageal Doppler to define fluid responsiveness, the studies reporting the timing of the CO/SV measurement after the fluid challenge, and those reporting the use of three or more quality indicators for CVP measurements (Fig. 3 and Figs. 5–9 in the supplementary material). In exploratory analyses the highest positive and negative predictive values were at CVP cut-off points of 2 mmHg (65 % (95 % CI 54–76)) and 14 mmHg [66 % (58–73)], respectively (Table 2). The highest positive and negative likelihood ratios were also at CVP cut-off points of 2 mmHg [2.04 (1.27–3.26)] and 14 mmHg [0.56 (0.41–0.77)], respectively (Table 2).
Forest plot including AUC-ROC with 95 % CIs for the lower, intermediate and higher CVP groups of the individual patient data sets (n = 1148) and the sensitivity analyses of the five subgroups (use of mechanical ventilation, use of thermo- or lithium-dilution or oesophageal Doppler to define fluid responsiveness, ICU patients, timing of CO/SV measurement reported, and three or more quality indicators for CVP measurements). AUC area under the curve, ROC receiver operating characteristic
Discussion
The main finding of this systematic review was that most of the reported mean/median CVP values in studies were in the intermediate range (8–12 mmHg) for both operating room and ICU/other patient groups and for fluid responders and non-responders. For the studies with available individual patient data sets 47 % of the CVP values were in the lower (<8 mmHg) range. In this lower CVP subgroup the AUC-ROC was different from 0.50 (no overall predictive value), but the observed value of 0.57 indicated that CVP was a poor test for fluid responsiveness even in the lower range of CVP values. This was supported by the low positive predictive values and likelihood ratios of specific CVP cut-off points (6, 4, 2 and 0 mmHg). However, our estimates were less precise the lower the CVP cut-off point as the 95 % CIs widened, because of lower numbers of individual patient data sets with very low CVP values. For the intermediate and higher CVP subgroup, the AUC-ROC did not differ from 0.50 and no specific CVP cut-off points had negative predictive value for fluid responsiveness above 66 %. Our estimates of the predictive values were less certain at CVP cut-off points >15 mmHg because of lower numbers of individual patient data sets with CVP values above this level.
Our main finding, that CVP is of limited value in the prediction of fluid responsiveness, is in agreement with previous systematic reviews [7, 8]. Our analyses of a large number of individual patient data sets are novel and include a reasonable number of extreme CVP values, in particular in the lower end. These analyses also indicate low predictive values for fluid responsiveness even at extreme values of CVP, at least in the average way CVP is used in the included studies. However, it does appear that patients with higher CVP levels were less likely to be included in the original studies even though only few studies had specific exclusion criteria driving this. If this was a systematic error, it may have happened because clinicians follow the general physiological principle and the observations supporting that the higher the baseline CVP, the less the response to fluid [54]. In any case, it represents a potential selection bias, which is difficult to quantify. Because we observed fewer individual patient data sets with CVP values above 15 mmHg, the negative predictive values above this CVP cut-off point should be interpreted with some caution.
There are alternative methods to CVP for the prediction of fluid responsiveness, but a number of prerequisites have to be fulfilled for these to be valid (continuous SV or CO measurement for passive leg raising test and sinus rhythm, controlled ventilation with tidal volumes >7 ml/kg and sedation for the use of pulse pressure variation and stroke volume variation), which limits their use [63, 64].
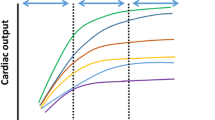
Measuring CVP in the clinical setting is not an easy task and there are several confounders that may reduce CVP’s predictive value for fluid responsiveness. CVP measurements are sensitive to both the zeroing and the levelling of the transducer, where small differences can result in significant measurement differences [5]. Being an intramural pressure CVP is sensitive to several factors influencing both the vessel distensibility and the transmural pressure. Effective circulating volume and diastolic and systolic cardiac function, pericardial, intrathoracic and intra-abdominal pressures all influence CVP [5]. The intra-thoracic pressure increases when applying positive pressure ventilation and higher positive end expiratory pressure (PEEP), which will increase CVP. And the Frank–Starling curve describing the relationship between venous return (preload) and SV is a very simplified approach because the curve is influenced by several factors. Pathophysiological conditions such as heart failure and cardiogenic shock affect the contractile state of the heart, which may reduce the increase of SV due to an increase in preload [65]. Also, CVP is the downstream pressure for mean systemic filling pressure to deliver venous return to the right side of the heart [5, 66].
Before we can conclude that CVP is of limited value in guiding fluid therapy, we need larger studies that control for the confounding factors and studies where the use of CVP is integrated with estimates of mean systemic filling pressure. Preferably, these studies should be performed in patient populations at higher risk of hypo- or hypervolaemia [67].
The strengths of this study include those of a systematic review in general. The search for studies was done systematically using a wide search string in multiple databases without limitations. The inclusion and exclusion of studies were predefined and done systematically by two independent investigators. The collection of data was structured using a standardised form. In addition, we predefined the subgroup and sensitivity analyses including the cut-off points of the three CVP subgroups. We obtained a large sample of individual patient data sets enabling us to perform pooled analyses with better statistical power than in the individual studies.
The limitations of the study include the weaknesses of systematic reviews in general. It is possible that we did not identify all the relevant studies. The included studies were heterogeneous in both setting and design. In particular the studies differed in the amount of fluids given and in their cut-off points for fluid responsiveness. This limits our analyses of both reported and individual CVP values. The clinical translation of our results is also hampered by the definition of fluid responsiveness. The cut-off values for fluid responsiveness are chosen because of the cut-off points of the methods for measurement of SV or CO; this is somewhat artificial. On the other hand, there are limited data supporting alternative ‘outcome measures’ for a fluid challenge. We obtained individual patient data from less than half of the studies and several included more data sets from some patients, which may have affected the results of our re-analyses. Also, we did not obtain more detailed patient data, excluding the possibility for explorative analyses based on differences in clinical setting, cardiopulmonary status and/or ventilator settings. Finally, it may be that the pooling of results in studies and systematic reviews of clinicians’ complex assessments of potential fluid responsiveness including CVP and other characteristics represents too rough a reduction of these complex data, so that the signals are lost.
Conclusions
Most studies on fluid responsiveness reported mean/median CVP values in the intermediate range of 8–12 mmHg in both responders and non-responders. In our re-analyses of a large sample of individual patient data sets, lower CVP values (<8 mmHg) predicted fluid responsiveness and had some positive predictive value at 2 and 4 mmHg. Overall, the intermediate (8–12 mmHg) and higher (>12 mmHg) ranges of CVP values did not predict fluid responsiveness, though we found some negative predictive value using 14 and 16 mmHg as cut-off points. However, there were fewer data on higher CVP values, in particular >15 mmHg, resulting in less certain estimates of predictive values of higher CVP values. In any case, the predictive values, both positive and negative, were generally low for all the specific CVP values assessed in the range 0–20 mmHg.
References
Perner A, De Backer D (2014) Understanding hypovolaemia. Intensive Care Med 40:613–615
Marik PE, Cavallazzi R, Vasu T, Hirani A (2009) Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med 37:2642–2647
Boyd JH, Forbes J, Nakada TA, Walley KR, Russell JA (2011) Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med 39:259–265
Cecconi M, Hofer C, Teboul JL, Pettila V, Wilkman E, Molnar Z, Della Rocca G, Aldecoa C, Artigas A, Jog S, Sander M, Spies C, Lefrant JY, De Backer D (2015) Fluid challenges in intensive care: the FENICE study: a global inception cohort study. Intensive Care Med 41:1529–1537
Sondergaard S, Parkin G, Aneman A (2015) Central venous pressure: we need to bring clinical use into physiological context. Acta Anaesthesiol Scand 59:552–560
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R (2013) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39:165–228
Marik PE, Baram M, Vahid B (2008) Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest 134:172–178
Marik PE, Cavallazzi R (2013) Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med 41:1774–1781
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Jaeschke R, Mebazaa A, Pinsky MR, Teboul JL, Vincent JL, Rhodes A (2014) Consensus on circulatory shock and hemodynamic monitoring. Task Force of the European Society of Intensive Care Medicine. Intensive Care Med 40:1795–1815
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
Wetterslev M, Haase N, Johansen RR, Perner A (2013) Predicting fluid responsiveness with transthoracic echocardiography is not yet evidence based. Acta Anaesthesiol Scand 57:692–697
Barbier C, Loubieres Y, Schmit C, Hayon J, Ricome JL, Jardin F, Vieillard-Baron A (2004) Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med 30:1740–1746
Belloni L, Pisano A, Natale A, Piccirillo MR, Piazza L, Ismeno G, De Martino G (2008) Assessment of fluid-responsiveness parameters for off-pump coronary artery bypass surgery: a comparison among LiDCO, transesophageal echochardiography, and pulmonary artery catheter. J Cardiothorac Vasc Anesth 22:243–248
Berkenstadt H, Margalit N, Hadani M, Friedman Z, Segal E, Villa Y, Perel A (2001) Stroke volume variation as a predictor of fluid responsiveness in patients undergoing brain surgery. Anesth Analg 92:984–989
Biais M, Nouette-Gaulain K, Cottenceau V, Revel P, Sztark F (2008) Uncalibrated pulse contour-derived stroke volume variation predicts fluid responsiveness in mechanically ventilated patients undergoing liver transplantation. Br J Anaesth 101:761–768
Broch O, Bein B, Gruenewald M, Hocker J, Schottler J, Meybohm P, Steinfath M, Renner J (2011) Accuracy of the pleth variability index to predict fluid responsiveness depends on the perfusion index. Acta Anaesthesiol Scand 55:686–693
Broch O, Renner J, Gruenewald M, Meybohm P, Hocker J, Schottler J, Steinfath M, Bein B (2012) Variation of left ventricular outflow tract velocity and global end-diastolic volume index reliably predict fluid responsiveness in cardiac surgery patients. J Crit Care 27:325.e7–325.e13
Cannesson M, Attof Y, Rosamel P, Desebbe O, Joseph P, Metton O, Bastien O, Lehot JJ (2007) Respiratory variations in pulse oximetry plethysmographic waveform amplitude to predict fluid responsiveness in the operating room. Anesthesiology 106:1105–1111
Cannesson M, Le Manach Y, Hofer CK, Goarin JP, Lehot JJ, Vallet B, Tavernier B (2011) Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness: a “gray zone” approach. Anesthesiology 115:231–241
Cannesson M, Musard H, Desebbe O, Boucau C, Simon R, Henaine R, Lehot JJ (2009) The ability of stroke volume variations obtained with Vigileo/FloTrac system to monitor fluid responsiveness in mechanically ventilated patients. Anesth Analg 108:513–517
Cecconi M, Monti G, Hamilton MA, Puntis M, Dawson D, Tuccillo ML, Della Rocca G, Grounds RM, Rhodes A (2012) Efficacy of functional hemodynamic parameters in predicting fluid responsiveness with pulse power analysis in surgical patients. Minerva Anestesiol 78:527–533
de Waal EE, Rex S, Kruitwagen CL, Kalkman CJ, Buhre WF (2009) Dynamic preload indicators fail to predict fluid responsiveness in open-chest conditions. Crit Care Med 37:510–515
Desgranges FP, Desebbe O, Ghazouani A, Gilbert K, Keller G, Chiari P, Robin J, Bastien O, Lehot JJ, Cannesson M (2011) Influence of the site of measurement on the ability of plethysmographic variability index to predict fluid responsiveness. Br J Anaesth 107:329–335
Fischer MO, Pelissier A, Bohadana D, Gerard JL, Hanouz JL, Fellahi JL (2013) Prediction of responsiveness to an intravenous fluid challenge in patients after cardiac surgery with cardiopulmonary bypass: a comparison between arterial pulse pressure variation and digital plethysmographic variability index. J Cardiothorac Vasc Anesth 27:1087–1093
Geerts BF, Aarts LP, Groeneveld AB, Jansen JR (2011) Predicting cardiac output responses to passive leg raising by a PEEP-induced increase in central venous pressure, in cardiac surgery patients. Br J Anaesth 107:150–156
Heijmans JH, Ganushak YM, Theunissen MS, Maessen JG, Roekaerts PJ (2010) Predictors of cardiac responsiveness to fluid therapy after cardiac surgery. Acta Anaesthesiol Belg 61:151–158
Huang CC, Fu JY, Hu HC, Kao KC, Chen NH, Hsieh MJ, Tsai YH (2008) Prediction of fluid responsiveness in acute respiratory distress syndrome patients ventilated with low tidal volume and high positive end-expiratory pressure. Crit Care Med 36:2810–2816
Keller G, Sinavsky K, Desebbe O, Lehot JJ (2012) Combination of continuous pulse pressure variation monitoring and cardiac filling pressure to predict fluid responsiveness. J Clin Monit Comput 26:401–405
Kramer A, Zygun D, Hawes H, Easton P, Ferland A (2004) Pulse pressure variation predicts fluid responsiveness following coronary artery bypass surgery. Chest 126:1563–1568
Lakhal K, Ehrmann S, Benzekri-Lefevre D, Runge I, Legras A, Dequin PF, Mercier E, Wolff M, Regnier B, Boulain T (2011) Respiratory pulse pressure variation fails to predict fluid responsiveness in acute respiratory distress syndrome. Crit Care 15:R85
Lakhal K, Ehrmann S, Runge I, Benzekri-Lefevre D, Legras A, Dequin PF, Mercier E, Wolff M, Regnier B, Boulain T (2010) Central venous pressure measurements improve the accuracy of leg raising-induced change in pulse pressure to predict fluid responsiveness. Intensive Care Med 36:940–948
Lee JH, Jeon Y, Bahk JH, Gil NS, Kim KB, Hong DM, Kim HJ (2011) Pulse-pressure variation predicts fluid responsiveness during heart displacement for off-pump coronary artery bypass surgery. J Cardiothorac Vasc Anesth 25:1056–1062
Lee JH, Kim JT, Yoon SZ, Lim YJ, Jeon Y, Bahk JH, Kim CS (2007) Evaluation of corrected flow time in oesophageal Doppler as a predictor of fluid responsiveness. Br J Anaesth 99:343–348
Mahjoub Y, Benoit-Fallet H, Airapetian N, Lorne E, Levrard M, Seydi AA, Amennouche N, Slama M, Dupont H (2012) Improvement of left ventricular relaxation as assessed by tissue Doppler imaging in fluid-responsive critically ill septic patients. Intensive Care Med 38:1461–1470
Monge Garcia MI, Gil Cano A, Diaz Monrove JC (2009) Brachial artery peak velocity variation to predict fluid responsiveness in mechanically ventilated patients. Crit Care 13:R142
Moretti R, Pizzi B (2010) Inferior vena cava distensibility as a predictor of fluid responsiveness in patients with subarachnoid hemorrhage. Neurocrit Care 13:3–9
Muller L, Louart G, Bengler C, Fabbro-Peray P, Carr J, Ripart J, de La Coussaye JE, Lefrant JY (2008) The intrathoracic blood volume index as an indicator of fluid responsiveness in critically ill patients with acute circulatory failure: a comparison with central venous pressure. Anesth Analg 107:607–613
Muller L, Louart G, Bousquet PJ, Candela D, Zoric L, de La Coussaye JE, Jaber S, Lefrant JY (2010) The influence of the airway driving pressure on pulsed pressure variation as a predictor of fluid responsiveness. Intensive Care Med 36:496–503
Muller L, Toumi M, Bousquet PJ, Riu-Poulenc B, Louart G, Candela D, Zoric L, Suehs C, de La Coussaye JE, Molinari N, Lefrant JY (2011) An increase in aortic blood flow after an infusion of 100 ml colloid over 1 minute can predict fluid responsiveness: the mini-fluid challenge study. Anesthesiology 115:541–547
Oliveira-Costa CD, Friedman G, Vieira SR, Fialkow L (2012) Pulse pressure variation and prediction of fluid responsiveness in patients ventilated with low tidal volumes. Clinics (Sao Paulo) 67:773–778
Osman D, Ridel C, Ray P, Monnet X, Anguel N, Richard C, Teboul JL (2007) Cardiac filling pressures are not appropriate to predict hemodynamic response to volume challenge. Crit Care Med 35:64–68
Perel A, Minkovich L, Preisman S, Abiad M, Segal E, Coriat P (2005) Assessing fluid-responsiveness by a standardized ventilatory maneuver: the respiratory systolic variation test. Anesth Analg 100:942–945
Preisman S, Kogan S, Berkenstadt H, Perel A (2005) Predicting fluid responsiveness in patients undergoing cardiac surgery: functional haemodynamic parameters including the respiratory systolic variation test and static preload indicators. Br J Anaesth 95:746–755
Roy S, Couture P, Qizilbash B, Toupin F, Levesque S, Carrier M, Lambert J, Denault AY (2013) Hemodynamic pressure waveform analysis in predicting fluid responsiveness. J Cardiothorac Vasc Anesth 27:676–680
Shin YH, Ko JS, Gwak MS, Kim GS, Lee JH, Lee SK (2011) Utility of uncalibrated femoral stroke volume variation as a predictor of fluid responsiveness during the anhepatic phase of liver transplantation. Liver Transpl 17:53–59
Trof RJ, Danad I, Groeneveld AJ (2013) Global end-diastolic volume increases to maintain fluid responsiveness in sepsis-induced systolic dysfunction. BMC Anesthesiol 13:12
Trof RJ, Danad I, Reilingh MW, Breukers RM, Groeneveld AB (2011) Cardiac filling volumes versus pressures for predicting fluid responsiveness after cardiovascular surgery: the role of systolic cardiac function. Crit Care 15:R73
Wilkman E, Kuitunen A, Pettila V, Varpula M (2014) Fluid responsiveness predicted by elevation of PEEP in patients with septic shock. Acta Anaesthesiol Scand 58:27–35
Wyffels PA, Durnez PJ, Helderweirt J, Stockman WM, De Kegel D (2007) Ventilation-induced plethysmographic variations predict fluid responsiveness in ventilated postoperative cardiac surgery patients. Anesth Analg 105:448–452
Yazigi A, Khoury E, Hlais S, Madi-Jebara S, Haddad F, Hayek G, Jabbour K (2012) Pulse pressure variation predicts fluid responsiveness in elderly patients after coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth 26:387–390
Calvin JE, Driedger AA, Sibbald WJ (1981) The hemodynamic effect of rapid fluid infusion in critically ill patients. Surgery 90:61–76
Fischer MO, Balaire X, Mauff Le, de Kergal C, Boisselier C, Gerard JL, Hanouz JL, Fellahi JL (2014) The diagnostic accuracy of estimated continuous cardiac output compared with transthoracic echocardiography. Can J Anaesth 61:19–26
Hu B, Xiang H, Liang H, Yu L, Xu T, Yang JH, Du ZH, Li JG (2013) Assessment effect of central venous pressure in fluid resuscitation in the patients with shock: a multi-center retrospective research. Chin Med J (Engl) 126:1844–1849
Magder S, Bafaqeeh F (2007) The clinical role of central venous pressure measurements. J Intensive Care Med 22:44–51
Saugel B, Kirsche SV, Hapfelmeier A, Phillip V, Schultheiss C, Schmid RM, Huber W (2013) Prediction of fluid responsiveness in patients admitted to the medical intensive care unit. J Crit Care 28:537.e531–537.e539
Sturgess DJ, Pascoe RL, Scalia G, Venkatesh B (2010) A comparison of transcutaneous Doppler corrected flow time, b-type natriuretic peptide and central venous pressure as predictors of fluid responsiveness in septic shock: a preliminary evaluation. Anaesth Intensive Care 38:336–341
Thiel SW, Kollef MH, Isakow W (2009) Non-invasive stroke volume measurement and passive leg raising predict volume responsiveness in medical ICU patients: an observational cohort study. Crit Care 13:R111
Velissaris D, Pierrakos C, Scolletta S, De Backer D, Vincent JL (2011) High mixed venous oxygen saturation levels do not exclude fluid responsiveness in critically ill septic patients. Crit Care 15:R177
Yu T, Pan C, Guo FM, Yang Y, Qiu HB (2013) Changes in arterial blood pressure induced by passive leg raising predict hypotension during the induction of sedation in critically ill patients without severe cardiac dysfunction. Chin Med J (Engl) 126:2445–2450
Monge Garcia MI, Gil Cano A, Diaz Monrove JC (2009) Arterial pressure changes during the valsalva maneuver to predict fluid responsiveness in spontaneously breathing patients. Intensive Care Med 35:77–84
Cecconi M, Aya HD, Geisen M, Ebm C, Fletcher N, Grounds RM, Rhodes A (2013) Changes in the mean systemic filling pressure during a fluid challenge in postsurgical intensive care patients. Intensive Care Med 39:1299–1305
Lanspa MJ, Brown SM, Hirshberg EL, Jones JP, Grissom CK (2012) Central venous pressure and shock index predict lack of hemodynamic response to volume expansion in septic shock: a prospective, observational study. J Crit Care 27:609–615
Hamzaoui O, Monnet X, Teboul JL (2015) Evolving concepts of hemodynamic monitoring for critically ill patients. Indian J Crit Care Med 19:220–226
Mahjoub Y, Lejeune V, Muller L, Perbet S, Zieleskiewicz L, Bart F, Veber B, Paugam-Burtz C, Jaber S, Ayham A, Zogheib E, Lasocki S, Vieillard-Baron A, Quintard H, Joannes-Boyau O, Plantefeve G, Montravers P, Duperret S, Lakhdari M, Ammenouche N, Lorne E, Slama M, Dupont H (2014) Evaluation of pulse pressure variation validity criteria in critically ill patients: a prospective observational multicentre point-prevalence study. Br J Anaesth 112:681–685
Marik PE, Lemson J (2014) Fluid responsiveness: an evolution of our understanding. Br J Anaesth 112:617–620
Berlin DA, Bakker J (2014) Understanding venous return. Intensive Care Med 40:1564–1566
Perner A, Vieillard-Baron A, Bakker J (2015) Fluid resuscitation in ICU patients: quo vadis? Intensive Care Med 41:1667–1669
Acknowledgments
We warmly thank Drs. M. Biais, O. Broch, M. Cecconi, M.O. Fischer, M.I. Monge Garcia, B.F. Geerts, G. Keller, K. Lakhal, M.J. Lanspa, S. Magder, Y. Mahjoub, L. Muller, C.D. Oliveira-Costa, S. Preisman, S. Roy, B. Saugel, R.J. Trof, E. Wilkman and T. Yu for sharing their original data. Without their altruistic help the results of this study would have been less conclusive.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None of the authors have potential conflicts of interest.
Funding
None of the authors receive funding or financial support.
Additional information
Take-home message: In the re-analysis of 1148 individual data sets lower CVP values had low predictive power for fluid responsiveness.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Eskesen, T.G., Wetterslev, M. & Perner, A. Systematic review including re-analyses of 1148 individual data sets of central venous pressure as a predictor of fluid responsiveness. Intensive Care Med 42, 324–332 (2016). https://doi.org/10.1007/s00134-015-4168-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-4168-4