Abstract
Purpose
The aim of this retrospective clinical quality assessment was to evaluate the efficacy of low-dose radiotherapy (RT) for painful benign skeletal disorders.
Methods
Patients with different painful benign skeletal disorders (arthrosis and enthesopathies) were recruited for this retrospective clinical quality assessment between January 2014 and December 2015. RT was applied with a linear accelerator. Single doses of 0.5 Gy (total dose 3.0–5.0 Gy) were used. Pain was measured before and immediately after RT (early response) by a 10-point visual analogue scale (VAS). We defined a VAS score of 0–2 as a good response. Pain relief was measured during follow-up.
Results
A total of 598 evaluable patients (394 females, 204 males) with a mean age of 61.4 years (range 33–81 years) were recruited. The median VAS score was 7.0 (interquartile range [IQR] 2) before treatment and 5.0 (IQR 4) upon completion of RT (p < 0.001). A good response was achieved upon completion of RT in 83 patients (13.9%), with a median follow-up of 38 months (range 29–47 months) in 373 patients (62.4%; p < 0.001). In general, RT had a better effect on enthesopathies than on arthrosis.
Conclusion
Low-dose RT is a very effective treatment for the management of painful benign skeletal disorders. Due to the delayed onset of analgesic effects, low-dose RT results in significantly improved long-term efficacy compared to the results immediately after RT. These findings confirm the results of other retrospective, prospective, and randomized trials.
Zusammenfassung
Hintergrund
Ziel dieser retrospektiven klinischen Qualitätskontrolle war es, die Wirksamkeit der niedrigdosierten Radiotherapie (RT) bei schmerzhaften benignen muskuloskeletalen Erkrankungen zu bewerten.
Methoden
Zwischen Januar 2014 und Dezember 2015 wurden Patienten mit schmerzhaften muskuloskeletalen Erkrankungen (Arthrosen und Enthesiopathien) für die Studie rekrutiert. Für die RT wurde ein Linearbeschleuniger verwendet. Die RT erfolgte mit Einzeldosen von 0,5 Gy und Gesamtdosen von 3,0 bis 5,0 Gy. Der Schmerz wurde vor und direkt nach der RT (frühes Ansprechen) mithilfe einer 10 Punkte umfassenden visuellen Analogskala (VAS) bewertet. VAS-Werte von 0–2 wurden als gutes Ansprechen definiert. Das Ansprechen der RT gemäß VAS wurde zur Nachsorge erneut bewertet.
Ergebnisse
Insgesamt wurden 598 auswertbare Fälle von Patienten (394 Frauen, 204 Männer) mit einem Durchschnittsalter von 61,4 Jahren (Spanne: 33–81) in die Auswertung einbezogen. Der mediane VAS-Wert betrug 7,0 (Interquartilsabstand, IQR: 2) vor der Behandlung und 5,0 (IQR: 4) unmittelbar nach Beendigung der RT (p < 0,001). Bei 83 Patienten (13,9%) wurde sofort nach Abschluss der RT ein gutes Ansprechen erzielt, nach einer medianen Nachbeobachtungszeit von 38 Monaten (29–47) zeigte sich ein gutes Ansprechen bei 373 Patienten (62,4%; p < 0,001). Die RT führte bei den Enthesiopathien zu signifikant besseren Ergebnissen im Vergleich zu den Arthrosen.
Schlussfolgerungen
Die niedrig dosierte RT ist wirksam in der Behandlung von schmerzhaften benignen muskuloskeletalen Erkrankungen. Durch die zeitlich verzögert ablaufenden radiobiologischen Effekte führt die niedrig dosierte RT zu einer signifikant besseren Langzeitwirkung im Vergleich zu den Ergebnissen unmittelbar direkt nach der RT. Die Resultate sind vergleichbar mit denen aus publizierten retrospektiven, prospektiven und randomisierten Studien.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Unchanged low-dose radiotherapy (RT) for benign diseases accounts for 8–10% of all RT procedures in Germany. As many as 70% of these indications represent painful disorders in the locomotor system [1].
Previous radiobiological studies have shown that low doses of radiation can favorably influence various inflammatory pathways and immune components, such as endothelial cells, mononuclear and polynuclear leukocytes, and macrophages [2].
In clinical practice, single doses of 0.5 to 1.0 Gy and total doses of 3.0 to 6.0 Gy per series are used. The aims of this retrospective clinical quality assessment were to analyze the therapeutic effect of low-dose irradiation immediately after completion of RT and during follow-up, and to identify possible prognostic factors in patients with painful arthrosis and enthesopathies.
Methods
Patients and treatment
Between January 2014 and December 2015, patients with painful arthrosis and enthesopathies were recruited for this retrospective clinical quality assessment. All patients provided informed consent regarding radiotherapy and participation in this clinical quality assessment prior to enrollment. RT was applied with a linear accelerator using 6 and 15 MV photon fields. Single doses of 0.5 Gy were administered five times a week, for a total dose of 3.0–5.0 Gy.
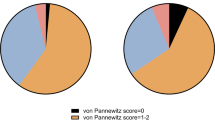
Pain was measured before and immediately after RT (early response) using a 10-point visual analogue scale (VAS; 0, no pain to 10, strongest pain) [3]. A VAS score of 0–2 is comparable to the “von Pannewitz” score pain-free and significantly improved; therefore, we defined a VAS score of 0–2 as a good response following RT. Pain relief was measured during follow-up.
The assessment of long-term efficacy was carried out by telephone survey. All 598 patients were available by phone. All results were recorded in an Excel (Microsoft Corporation, Redmond, WA, USA) spreadsheet and then transferred to SPSS (IBM Corporation, Armonk, NY, USA) for evaluation after completion of the survey.
Statistical analysis
All data were stored and analyzed using the SPSS statistical package 23.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics were computed for continuous and categorical variables, including median and interquartile ranges (IQR) of ordinal variables, mean and standard deviations of continuous variables, and frequencies and relative frequencies of categorical factors. The Wilcoxon signed-rank test was used to test for differences in continuous and categorical variables within the groups. To test for between-group differences, the Mann–Whitney U test was used for continuous variables and Fisher’s exact test for categorical variables, as appropriate. All P-values were two-sided statistical tests, and P < 0.05 was considered significant. A Cox proportional hazards model was used for multivariate analysis to assess the independence of pain on prognostic factors for a good response at follow-up.
Results
Patients
A total of 598 evaluable patients (394 women, 204 men) with a mean age of 61.4 years (range 33–81 years) were recruited for the study. The following diagnoses were given: calcaneodynia (n = 194), shoulder syndrome (n = 135), arthrosis of the hand including rhizarthritis (n = 95), elbow syndrome (n = 60), trochanteric syndrome (n = 54), gonarthrosis (n = 30), and coxarthrosis (n = 30). A total of 507 patients were pre-treated prior to RT, including local injections, physiotherapy, NSAIDs, and shoe insoles. Ninety-one patients were irradiated without previous treatment. Patient characteristics are summarized in Table 1.
Treatment and series
RT was fractionated into 6 × 0.5 Gy in 34 patients and with 10 × 0.5 Gy in 564 patients. The standard was fractionation of 10 × 0.5 Gy. In 34 cases, due to individual reasons, RT was fractionated as 6 × 0.5 Gy. RT was performed as one series in 339 patients, two series in 229 patients, and three series in 40 patients based on insufficient remission of pain. RT of shoulder, hip, knee joints, and trochanteric syndrome was performed with opposing photon fields, and RT of the heels, hands, and elbows was performed with single photon fields.
VAS before and immediately upon completion of RT
The median VAS score was 7.0 (IQR 2) before treatment and 5.0 (IQR 4) immediately upon completion of RT (p < 0.001). The results of RT for patients with different diagnoses are summarized in Table 2.
VAS follow-up
Twelve weeks after radiotherapy (n = 339), the median VAS score was 4.0 (IQR 4). After a median follow-up of 38 months (range 29–47 months), the median VAS score was 1.0 (IQR 4; p = 0.001).
Good response immediately upon completion of RT
A good response was achieved immediately upon completion of RT in 83/598 patients (13.9%) and 12 weeks after radiotherapy in 119/339 patients (35.1%; p < 0.001).
Good response at follow-up
A good response was achieved within a median follow-up of 38 months in 373/598 patients (62.4%). This is a significant improvement over the results immediately upon completion of RT and 12 weeks after RT (p < 0.001). Results for the different diagnoses are given in Table 3.
Rate of recurrence after a good response during follow-up
Compared to immediately after RT, 15 of the 83 patients (18.1%) with a good response 12 weeks after the onset of RT exhibited pain recurrence. Compared to 12 weeks after the onset of RT, 25 of the 119 patients (21%) with a good response within the 38-month follow-up exhibited pain recurrence.
Comparison of results for enthesopathies and arthrosis
Treatment results comparing enthesopathies and arthrosis are given in Table 4. In general, RT had a better effect on enthesopathies than on arthrosis.
Comparison of sex
Results regarding biological sex are given in Table 5. Efficacy immediately after RT (early response) was better in men than in women, but no significant difference was found at follow-up.
Multivariate analysis
The multivariate Cox regression analysis including sex, age, pre-treatment, disease group (enthesopathies or arthrosis), and number of treatment series revealed male gender (p = 0.031) and patients with enthesopathies (p < 0.001) as significant prognostic factors for a good response at follow-up (Table 6).
Comparison of fractionation
With regard to fractionation, we found no significant differences between 6 × 0.5 Gy and 10 × 0.5 Gy.
No side effects were observed.
Discussion
The results of our retrospective clinical quality assessment confirmed the results of recently published retrospective and prospective randomized studies showing a good analgesic effect of low-dose RT in patients with enthesopathies or arthrosis [4,5,6,7,8,9,10,11,12,13]. The pathophysiological mechanisms of pain relief after RT are most likely multifactorial. Radiobiological experiments clearly indicate that low-dose RT has an anti-inflammatory effect due to the modulation of a variety of inflammatory pathways and the influence on cellular components, such as endothelial cells, mononuclear and polynuclear leukocytes, and macrophages. An influence of the vascular endothelium, with improved tissue perfusion, destruction of inflammatory cells (especially lymphocytes) and release of cytokines and proteolytic enzymes, modulation of the autonomic nervous system, a change in tissue pH, and increased membrane permeability, has been demonstrated previously in experimental studies [2].
Compared to the results immediately after RT, we observed a significant improvement in efficacy in the long term, confirming the results of other comparable studies. The relevant radiobiological mechanisms could cause the delayed clinical onset [2, 12, 13].
Similar to recently published results, our data show a significantly better response to RT in patients with enthesopathies than in patients with arthritis [12, 13]. Arthroses reflect irreversible pathological processes in which cartilaginous and bony destruction occurs that cannot be reversed by radiotherapy. This irreversible destruction can trigger inflammatory processes, which then appear clinically as activated osteoarthritis with pain and swelling. During these episodes of pain, low-dose RT may be helpful due to known radiobiological mechanisms. The arthrosis itself remains, despite the improvement in pain. Therefore, the analgesic effect on arthrosis is only moderate compared to the analgesic effect on enthesopathies.
Furthermore, the significantly better response to RT in men compared to women confirms the well-known evidence of general differences between men and women in terms of pain perception and pain assessment [14].
With regard to the number of treatment series in the same treatment region, the results of the patients who received two or three series are worse. Therefore, in the future, we will make the indication for low-dose radiotherapy strict in the case of repeated treatment series, because non-responders do not substantially benefit from additional treatment series.
A possible placebo effect of low-dose RT for the treatment of pain cannot be completely ruled out. Two randomized, blinded, and sham-controlled trials on knee and hand joint osteoarthritis were published recently and showed no significant difference in remission for RT groups compared to placebo groups [15, 16]. Despite the good study design, both studies are open to critique because of low patient numbers, short follow-up (3 months), and presumption of a very optimistic prognosis for the assessment of success. In addition, approximately 50% of the included patients had experienced pain ≥5 years before RT. In the future, randomized trials should include more patients, include patients with less advanced arthrosis and shorter duration of pain, and have a longer follow-up [17].
Side effects did not occur in any of our patients. This confirms the relevant results in the literature [4,5,6,7,8,9,10,11,12,13].
With respect to the comparison of 6 × 0.5 Gy (n = 34) and 10 × 0.5 Gy (n = 564), we found no significant advantages of any of the fractionation schemes. Therefore, in the future, for radiation protection, irradiation should be performed according to the recommended German guidelines: enthesopathies and trochanteric syndrome with single doses of 0.5 to 1.0 Gy up to a total dose of 3.0 Gy, and arthrosis with single doses of 0.5 to 1.0 Gy up to a total dose of 3.0 to 6.0 Gy [4].
Due to the known cancer risk, the indication for irradiation in patients younger than 40 years should be very critical. However, in older patients, the cancer risk can be neglected because it is low compared to the improvement in quality of life.
The limitations of our evaluation are the lack of randomization and blinding. Nevertheless, the crucial strength of the analysis is the long follow-up. Importantly, our analysis shows that low-dose RT of benign musculoskeletal diseases plays a very important, tendentially increasing, role in the context of health care in Germany in view of the aging population.
Conclusion
Low-dose RT is a very effective treatment for the management of painful benign skeletal disorders. In the present study, 62.4% of patients achieved a longer-lasting significant improvement in their quality of life. Due to the delayed onset of analgesic effects, low-dose RT results in significantly improved long-term efficacy compared to the results immediately after RT. In general, RT had a better effect on enthesopathies than on arthrosis. The results of our retrospective clinical quality assessment confirm the results of other retrospective, prospective, and randomized trials.
References
Seegenschmiedt MH, Micke O, Muecke R, German Cooperative Group on Radiotherapy for Non-malignant Diseases (GCG-BD) (2015) Radiotherapy for nonmalignant disorders: state of the art and update of the evidence-based practice guidelines. Br J Radiol 88:20150080
Reichl B, Block A, Schaefer U, Bert C, Mueller R, Jung H, Roedel F, German Working Group on Radiotherapy in Germany(GCG-BD) (2015) DEGRO practical guidelines for radiotherapy of non-malignant disorders: part I: physical principles, radiobiological mechanisms, and radiogenic risk. Strahlenther Onkol 191:701–709
Bortz J, Doering N (2006) Forschungsmethoden und Evaluation für Human- und Sozialwissenschaftler. Springer, Heidelberg, p 177. ISBN 3‑540-33305‑3
Ott OJ, Niewald M, Weitmann HD, Jacob I, Adamietz IA, Schaefer U, Keilholz L, Heyd R, Muecke R, German Cooperative Group on Radiotherapy for Benign Diseases (GCG-BD) (2015) DEGRO guidelines for the radiotherapy of non-malignant disorders: part II: painful degenerative skeletal disorders. Strahlenther Onkol 191:1–6
Ott OJ, Jeremias C, Gaipl US, Frey B, Schmidt M, Fietkau R (2015) Radiotherapy for benign achillodynia: long-term results of the Erlangen dose optimization trial. Strahlenther Onkol 191:979–984
Ott OJ, Jeremias C, Gaipl US, Frey B, Schmidt M, Fietkau R (2014) Radiotherapy for benign calcaneodynia: long-term results of the Erlangen dose optimization (EDO) trial. Strahlenther Onkol 190:671–675
Niewald M, Seegenschmiedt MH, Micke O, Graeber S, Muecke R, Schaefer V, Scheid C, Fleckenstein J, Licht N, Ruebe C, German Cooperative Group on Radiotherapy for Benign Diseases (2012) Randomized, multicenter trial on the effect of radiation therapy on plantar fasciitis (painful heel spur) comparing a standard dose with a very low dose: mature results after 12 months’ followup. Int J Radiat Oncol Biol Phys 84:e455–462
Muecke R, Seegenschmiedt MH, Heyd R, Schaefer U, Prott FJ, Glatzel M, Micke O, German Cooperative Group on Radiotherapy for Benign Diseases (GCG-BD) (2010) Radiotherapy in painful gonarthrosis. Results of a national patterns-of-care study. Strahlenther Onkol 186:7–17
Muecke R, Micke O, Reichl B, Heyder R, Prott FJ, Seegenschmiedt MH, Glatzel M, Schneider O, Schaefer U, Kundt G (2007) Demographic, clinical and treatment related predictors for event-free probability following low-dose radiotherapy for painful heel spurs—a retrospective multicenter study of 502 patients. Acta Oncol 46:239–246
Kaltenborn A, Carl UM, Hinsche T, Nitsche M, Herrmann RM (2017) Low-dose external beam radiotherapy for greater trochanteric pain syndrome-target volume definition and treatment outcome. Strahlenther Onkol 193:260–268
Ott OJ, Hertel S, Gaipl US, Frey B, Schmidt M, Fietkau R (2014) The Erlangen dose optimization trial for radiotherapy of benign painful shoulder syndrome. Long-term results. Strahlenther Onkol 190:394–398
Micke O, Seegenschmiedt MH, Adamietz IA, Fakhrian K, Schaefer U, Muecke R (2017) Low-dose radiation therapy for benign painful skeletal disorders: the typical treatment for the elderly patient? Int J Radiat Oncol Biol Phys 98:958–963
Micke O, Ugrak E, Bartmann S, Adamietz IA, Schaefer U, Bücker R, Kisters K, Seegenschmiedt MH, Fakhrian K, Muecke R (2018) Radiotherapy for calcaneodynia, achillodynia, painful gonarthrosis, bursitis trochanterica, and painful shoulder syndrome—Early and late results of a prospective clinical quality assessment. Radiat Oncol 13:71
Pieretti S, Di Giannuario A, Di Giovannandrea R, Marzoli F, Piccaro G, Minosi P, Aloisi AM (2016) Gender differences in pain and its relief. Ann Ist Super Sanita 52:184–189
Mahler EAM, Minten MJ, Leseman-Hoogenboom MM, Poortmans PMP, Leer JWH, Boks SS, van den Hoogen FHJ, den Broeder AA, van den Ende CHM (2019) Effectiveness of low-dose radiation therapy on symptoms in patients with knee osteoarthritis: a randomised, double-blinded, sham-controlled trial. Ann Rheum Dis 78:83–90
Minten MJM, Leseman-Hoogenboom MM, Kloppenburg M, Kortekaas MC, Leer JW, Poortmans PMP, van den Hoogen FHJ, den Broeder AA, van den Ende CHM (2018) Lack of beneficial effects of low-dose radiation therapy on hand osteoarthritis symptoms and inflammation: a randomised, blinded, sham-controlled trial. Osteoarthritis Cartilage 26:1283–1290
Ott OJ, Micke O, Mücke R, Niewald M, Rödel F, Schäfer U, Seegenschmiedt MH, Arenas M, Frey B, Gaipl US, German Cooperative Group on Radiotherapy for Benign Diseases (GCG-BD) (2018) Low-dose radiotherapy: Mayday, mayday. We’ve been hit! Strahlenther Onkol 195:285–288
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
NJ was the principle investigator of the retrospective clinical quality assessment. NJ, OM, MHS, and RM participated in the design of the retrospective clinical quality assessment, its coordination, and performed a part of the statistical analysis. NJ participated in patient accrual and the follow-up examinations. NJ, OM, and RM drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
N. Juniku, O. Micke, M. H. Seegenschmiedt, and R. Muecke declare that they have no competing interests.
Ethical standards
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case. The Ethics Committee of the Medical Association of the State of Bavaria decided that no formal ethical approval for this analysis was required, as only retrospective data from anonymized subjects were processed (telephone call from March 3, 2019, and website http://ethikkommission.blaek.de/studien/sonstige-studien-15-bo).
Additional information
Availability of data and materials
Please contact the corresponding author for data requests.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Juniku, N., Micke, O., Seegenschmiedt, M.H. et al. Radiotherapy for painful benign skeletal disorders. Strahlenther Onkol 195, 1068–1073 (2019). https://doi.org/10.1007/s00066-019-01514-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-019-01514-w