Abstract
Purpose
Evaluation of postoperative fractionated local 3D-conformal radiotherapy (3DRT) of the resection cavity in brain metastases.
Patients and methods
Between 2011 and 2016, 57 patients underwent resection of a single, previously untreated (37/57, 65%) or recurrent (20/57, 35%) brain metastasis (median maximal diameter 3.5 cm [1.1–6.5 cm]) followed by 3DRT. For definition of the gross tumor volume (GTV), the resection cavity was used and for the clinical target volume (CTV), margins of 1.0–1.5 cm were added. Median dose was 48.0 Gy (30.0–50.4 Gy) in 25 (10–28) fractions; most patients had 36.0–42.0 Gy in 3.0 Gy fractions (n = 16, EQD210Gy 39.0–45.5 Gy) or 40.0–50.4 Gy in 1.8–2.0 Gy fractions (n = 37, EQD210Gy 39.3–50.0 Gy).
Results
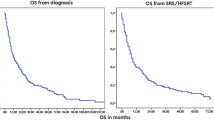
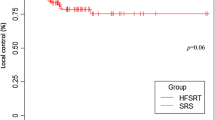
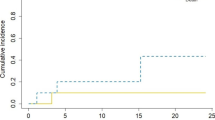
Median follow-up was 18 months. Local control rates were 83% at 1 year and 78% at 2 years and were significantly influenced by histology (breast cancer 100%, non-small lung cancer 87%, melanoma 80%, colorectal cancer 26% at 2 years, p = 0.006) and resection status (p < 0.0001), but not by EQD210Gy or size of the planning target volume (median 96.7 ml [16.7–282.8 ml]). At 1 and 2 years, 74% and 52% of the patients were free from distant brain metastases. Salvage procedures were applied in 25/27 (93%) of recurrent patients. Survival was 68% at 1 year and 41% at 2 years and was significantly improved in younger patients (p = 0.006) with higher Karnofsky performance score (p < 0.0001) and without prior radiotherapy (54% vs. 9% at 2 years, p = 0.006). No cases of radiographic or symptomatic radionecrosis were observed.
Conclusion
Adjuvant fractionated local 3DRT is highly effective in radiosensitive, completely resected metastases and should be considered for treating large resection cavities as an alternative to postoperative stereotactic single dose or hypofractionated radiosurgery.
Zusammenfassung
Ziel
Untersuchung der Wirksamkeit einer postoperativen fraktionierten, lokalen 3‑D-konformalen Strahlentherapie (3DRT) der Resektionshöhle bei Hirnmetastasen.
Patienten und Methoden
Von 2011–2016 wurde bei 57 Patienten eine unbehandelte (37/57, 65 %) oder rezidivierte (20/57, 35 %) Hirnmetastase (medianer maximaler Durchmesser 3,5 cm [1,1–6,5 cm]) reseziert und postoperativ lokal bestrahlt. Für das klinische Zielvolumen (CTV) wurden Säume von 1,0–1,5 cm um die Resektionshöhle verwendet. Die mediane Dosis betrug 48,0 Gy (30,0–50,4 Gy) in 25 (10–28) Fraktionen (meistens 36,0–42,0 Gy/3,0 Gy [n = 16, EQD210Gy 39,0–45,5 Gy] oder 40,0–50,4 Gy/1,8–2,0 Gy [n = 37, EQD210Gy 39,3–50,0 Gy]).
Ergebnisse
Die lokalen Kontrollraten von 83 % nach 1 Jahr und 78 % nach 2 Jahren wurden signifikant durch den Primärtumor (Mammakarzinom 100 %, nichtkleinzelliges Lungenkarzinom 87 %, Melanom 80 %, kolorektale Tumoren 26 % nach 2 Jahren, p = 0,006) und den Resektionsstatus (p < 0,0001), nicht aber durch die EQD210Gy oder die Größe des Planungszielvolumens (Median 96,7 ml [16,7–282,8 ml]) beeinflusst. Nach 1(2) Jahren waren 74 % (52 %) frei von neuen Hirnmetastasen. Salvage-Verfahren wurden bei 25/27 (93 %) angewendet. Das Überleben lag nach 1(2) Jahren bei 68 % (41 %) und war bei jüngeren Patienten (p = 0,006), bei höherem Karnofsky-Score (p < 0,0001) und ohne Vorbestrahlung (54 % vs. 9 % nach 2 Jahren, p = 0,006) signifikant verbessert. Es wurden keine radiologischen oder symptomatischen Radionekrosen beobachtet.
Schlussfolgerung
Die adjuvante fraktionierte, lokale 3DRT ist bei strahlensensiblen, vollständig resezierten Metastasen hoch wirksam und sollte zur Behandlung großer Resektionshöhlen als Alternative zur postoperativen stereotaktischen Einzeldosis- oder hypofraktionierten Radiochirurgie in Betracht gezogen werden.


Similar content being viewed by others
References
Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE (2004) Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol 22:2865–2872
Gavrilovic IT, Posner JB (2005) Brain metastases: epidemiology and pathophysiology. J Neurooncol 75:5–14
Chamberlain MC, Baik CS, Gadi VK, Bhatia S, Chow LQ (2017) Systemic therapy of brain metastases: non-small cell lung cancer, breast cancer, and melanoma. Neuro-Oncology 19(i1):i24
Shen CJ, Lim M, Kleinberg LR (2016) Controversies in the therapy of brain metastases: shifting paradigms in an era of effective systemic therapy and longer-term survivorship. Curr Treat Options Oncol 17:46
Patchell RA, Tibbs PA, Walsh JW et al (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322:494–500
Kocher M, Soffietti R, Abacioglu U et al (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol 29:134–141
Soffietti R, Kocher M, Abacioglu UM et al (2013) A European Organisation for Research and Treatment of Cancer phase III trial of adjuvant whole-brain radiotherapy versus observation in patients with one to three brain metastases from solid tumors after surgical resection or radiosurgery: quality-of-life results. J Clin Oncol 31:65–72
Brown PD, Ballman KV, Cerhan JH et al (2017) Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC.3): a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol 18:1049–1060
Aoyama H, Shirato H, Tago M et al (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295:2483–2491
Aoyama H, Tago M, Kato N et al (2007) Neurocognitive function of patients with brain metastasis who received either whole brain radiotherapy plus stereotactic radiosurgery or radiosurgery alone. Int J Radiat Oncol Biol Phys 68:1388–1395
Aoyama H, Tago M, Shirato H, Japanese Radiation Oncology Study Group I (2015) Stereotactic radiosurgery with or without whole-brain radiotherapy for brain metastases: secondary analysis of the JROSG 99-1 randomized clinical trial. Jama Oncol 1:457–464
Gans JH, Raper DM, Shah AH et al (2013) The role of radiosurgery to the tumor bed after resection of brain metastases. Neurosurgery 72:317–325 (discussion 325–316)
Mahajan A, Ahmed S, McAleer MF et al (2017) Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomised, controlled, phase 3 trial. Lancet Oncol 18:1040–1048
Jensen CA, Chan MD, McCoy TP et al (2011) Cavity-directed radiosurgery as adjuvant therapy after resection of a brain metastasis. J Neurosurg 114:1585–1591
Brennan C, Yang TJ, Hilden P et al (2014) A phase 2 trial of stereotactic radiosurgery boost after surgical resection for brain metastases. Int J Radiat Oncol Biol Phys 88:130–136
Narita Y, Shibui S (2009) Strategy of surgery and radiation therapy for brain metastases. Int J Clin Oncol 14:275–280
Thomas SS, Dunbar EM (2010) Modern multidisciplinary management of brain metastases. Curr Oncol Rep 12:34–40
Ueki K, Matsutani M, Nakamura O, Tanaka Y (1996) Comparison of whole brain radiation therapy and locally limited radiation therapy in the treatment of solitary brain metastases from non-small cell lung cancer. Neurol Med Chir (Tokyo) 36:364–369
Coucke PA, Zouhair A, Ozsahin M, De Tribolet N, Mirimanoff RO (1998) Focalized external radiotherapy for resected solitary brain metastasis: does the dogma stand? Radiother Oncol 47:99–101
Hashimoto K, Narita Y, Miyakita Y et al (2011) Comparison of clinical outcomes of surgery followed by local brain radiotherapy and surgery followed by whole brain radiotherapy in patients with single brain metastasis: single-center retrospective analysis. Int J Radiat Oncol Biol Phys 81:e475–480
Connolly EP, Mathew M, Tam M et al (2013) Involved field radiation therapy after surgical resection of solitary brain metastases—mature results. Neuro-Oncology 15:589–594
Shin SM, Vatner RE, Tam M et al (2015) Resection followed by involved-field fractionated radiotherapy in the management of single brain metastasis. Front Oncol 5:206
Igaki H, Harada K, Umezawa R et al (2017) Outcomes of surgery followed by local brain radiotherapy compared with surgery followed by whole brain radiotherapy for single brain metastasis. Tumori 103:367–373
Ahmed S, Hamilton J, Colen R et al (2014) Change in postsurgical cavity size within the first 30 days correlates with extent of surrounding edema: consequences for postoperative radiosurgery. J Comput Assist Tomogr 38:457–460
Jarvis LA, Simmons NE, Bellerive M et al (2012) Tumor bed dynamics after surgical resection of brain metastases: implications for postoperative radiosurgery. Int J Radiat Oncol Biol Phys 84:943–948
Patchell RA, Tibbs PA, Regine WF et al (1998) Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA 280:1485–1489
Chang EL, Wefel JS, Hess KR et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044
Brown PD, Jaeckle K, Ballman KV et al (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 316:401–409
Choi CY, Chang SD, Gibbs IC et al (2012) Stereotactic radiosurgery of the postoperative resection cavity for brain metastases: prospective evaluation of target margin on tumor control. Int J Radiat Oncol Biol Phys 84:336–342
Hartford AC, Paravati AJ, Spire WJ et al (2013) Postoperative stereotactic radiosurgery without whole-brain radiation therapy for brain metastases: potential role of preoperative tumor size. Int J Radiat Oncol Biol Phys 85:650–655
Prabhu R, Shu HK, Hadjipanayis C et al (2012) Current dosing paradigm for stereotactic radiosurgery alone after surgical resection of brain metastases needs to be optimized for improved local control. Int J Radiat Oncol Biol Phys 83:e61–66
Ojerholm E, Lee JY, Thawani JP et al (2014) Stereotactic radiosurgery to the resection bed for intracranial metastases and risk of leptomeningeal carcinomatosis. J Neurosurg 121(Suppl):75–83
Kondziolka D, Shin SM, Brunswick A, Kim I, Silverman JS (2015) The biology of radiosurgery and its clinical applications for brain tumors. Neuro-Oncology 17:29–44
Toma-Dasu I, Sandstrom H, Barsoum P, Dasu A (2014) To fractionate or not to fractionate? That is the question for the radiosurgery of hypoxic tumors. J Neurosurg 121(Suppl):110–115
Ishihara T, Yamada K, Harada A et al (2016) Hypofractionated stereotactic radiotherapy for brain metastases from lung cancer: evaluation of indications and predictors of local control. Strahlenther Onkol 192:386–393
Zindler JD, Schiffelers J, Lambin P, Hoffmann AL (2018) Improved effectiveness of stereotactic radiosurgery in large brain metastases by individualized isotoxic dose prescription: an in silico study. Strahlenther Onkol 194:560–569
Eaton BR, LaRiviere MJ, Kim S et al (2015) Hypofractionated radiosurgery has a better safety profile than single fraction radiosurgery for large resected brain metastases. J Neurooncol 123:103–111
Ahmed KA, Freilich JM, Abuodeh Y et al (2014) Fractionated stereotactic radiotherapy to the post-operative cavity for radioresistant and radiosensitive brain metastases. J Neurooncol 118:179–186
Minniti G, Esposito V, Clarke E et al (2013) Multidose stereotactic radiosurgery (9 Gy x 3) of the postoperative resection cavity for treatment of large brain metastases. Int J Radiat Oncol Biol Phys 86:623–629
Specht HM, Kessel KA, Oechsner M, Meyer B, Zimmer C, Combs SE (2016) HFSRT of the resection cavity in patients with brain metastases. Strahlenther Onkol 192:368–376
Blonigen BJ, Steinmetz RD, Levin L, Lamba MA, Warnick RE, Breneman JC (2010) Irradiated volume as a predictor of brain radionecrosis after linear accelerator stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 77:996–1001
Bilger A, Milanovic D, Lorenz H et al (2016) Stereotactic fractionated radiotherapy of the resection cavity in patients with one to three brain metastases. Clin Neurol Neurosurg 142:81–86
Combs SE, Bilger A, Diehl C et al (2018) Multicenter analysis of stereotactic radiotherapy of the resection cavity in patients with brain metastases. Cancer Med 7:2319–2327
Baumert BG, Rutten I, Dehing-Oberije C et al (2006) A pathology-based substrate for target definition in radiosurgery of brain metastases. Int J Radiat Oncol Biol Phys 66:187–194
Berghoff AS, Rajky O, Winkler F et al (2013) Invasion patterns in brain metastases of solid cancers. Neuro-Oncology 15:1664–1672
Raore B, Schniederjan M, Prabhu R, Brat DJ, Shu HK, Olson JJ (2011) Metastasis infiltration: an investigation of the postoperative brain-tumor interface. Int J Radiat Oncol Biol Phys 81:1075–1080
Siam L, Bleckmann A, Chaung HN et al (2015) The metastatic infiltration at the metastasis/brain parenchyma-interface is very heterogeneous and has a significant impact on survival in a prospective study. Oncotarget 6:29254–29267
Kamp MA, Grosser P, Felsberg J et al (2012) 5‑aminolevulinic acid (5-ALA)-induced fluorescence in intracerebral metastases: a retrospective study. Acta Neurochir (Wien) 154:223–228 (discussion 228)
Kamp MA, Slotty PJ, Cornelius JF, Steiger HJ, Rapp M, Sabel M (2018) The impact of cerebral metastases growth pattern on neurosurgical treatment. Neurosurg Rev 41:77–86
Yoo H, Kim YZ, Nam BH et al (2009) Reduced local recurrence of a single brain metastasis through microscopic total resection. J Neurosurg 110:730–736
Soliman H, Ruschin M, Angelov L et al (2018) Consensus contouring guidelines for postoperative completely resected cavity stereotactic radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys 100:436–442
Williams JR, Zhang Y, Zhou H et al (2008) A quantitative overview of radiosensitivity of human tumor cells across histological type and TP53 status. Int J Radiat Biol 84:253–264
Dore M, Martin S, Delpon G, Clement K, Campion L, Thillays F (2017) Stereotactic radiotherapy following surgery for brain metastasis: predictive factors for local control and radionecrosis. Cancer Radiother 21:4–9
Agboola O, Benoit B, Cross P et al (1998) Prognostic factors derived from recursive partition analysis (RPA) of Radiation Therapy Oncology Group (RTOG) brain metastases trials applied to surgically resected and irradiated brain metastatic cases. Int J Radiat Oncol Biol Phys 42:155–159
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. W. Ayas, S. Grau, K. Jablonska, D. Ruess, M. Ruge, S. Marnitz, R. Goldbrunner and M. Kocher declare that they have no competing interests.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors. For images or other information within the manuscript which identify patients, consent was obtained from them and/or their legal guardians.
Additional information
Ahmad Walid Ayas and Stefan Grau share first authorship.
Rights and permissions
About this article
Cite this article
Ayas, A.W., Grau, S., Jablonska, K. et al. Postoperative local fractionated radiotherapy for resected single brain metastases. Strahlenther Onkol 194, 1163–1170 (2018). https://doi.org/10.1007/s00066-018-1368-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-018-1368-1