Abstract
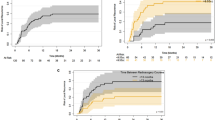
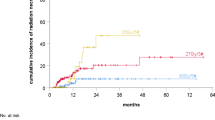
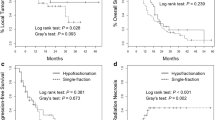
The purpose of this study is to compare the safety and efficacy of single fraction radiosurgery (SFR) with hypofractionated radiosurgery (HR) for the adjuvant treatment of large, surgically resected brain metastases. Seventy-five patients with 76 resection cavities ≥ 3 cm received 15 Gray (Gy) × 1 SFR (n = 40) or 5–8 Gy × 3–5 HR (n = 36). Cumulative incidence of local failure (LF) and radiation necrosis (RN) was estimated accounting for death as a competing risk and compared with Gray’s test. The effect of multiple covariates was evaluated with the Fine-Gray proportional hazards model. The most common HR dose-fractionation schedules were 6 Gy × 5 (44 %), 7–8 Gy × 3 (36 %), and 6 Gy × 4 (8 %). The median follow-up was 11 months (range 2–71). HR patients had larger median resection cavity volumes (24.0 vs. 13.3 cc, p < 0.001), planning target volumes (PTV) (37.7 vs. 20.5 cc, p < 0.001), and cavity to PTV expansion margins (2 vs. 1.5 mm, p = 0.002) than SFR patients. Cumulative incidence of LF (95 % CI) at 6 and 12-months for HR versus SFR was 18.9 % (0.07–0.34) versus 15.9 % (0.06–0.29), and 25.6 % (0.12–0.42) versus 27.2 % (0.14–0.42), p = 0.80. Cumulative incidence of RN (95 % CI) at 6 and 12 months for HR vs. SFR was 3.3 % (0.00–0.15) versus 10.7 % (0.03–0.23), and 10.3 % (0.02–0.25) versus 19.2 % (0.08–0.34), p = 0.28. On multivariable analysis, SFR was significantly associated with an increased risk of RN, with a HR of 3.81 (95 % CI 1.04–13.93, p = 0.043). Hypofractionated radiosurgery may be the more favorable treatment approach for radiosurgery of cavities 3–4 cm in size and greater.


Similar content being viewed by others
References
Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, Markesbery WR, Macdonald JS, Young B (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322(8):494–500. doi:10.1056/NEJM199002223220802
Kocher M, Soffietti R, Abacioglu U, Villa S, Fauchon F, Baumert BG, Fariselli L, Tzuk-Shina T, Kortmann RD, Carrie C, Ben Hassel M, Kouri M, Valeinis E, Van Den Berge D, Collette S, Collette L, Mueller RP (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the eortc 22952-26001 study. J Clin Oncol 29 (2):134–141. doi:10.1200/JCO.2010.30.1655
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, Arbuckle RB, Swint JM, Shiu AS, Maor MH, Meyers CA (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10(11):1037–1044. doi:10.1016/S1470-2045(09)70263-3
Roberge D, Parney I, Brown PD (2012) Radiosurgery to the postoperative surgical cavity: who needs evidence? Int J Radiat Oncol Biol Phys 83(2):486–493. doi:10.1016/J.IJROBP.2011.09.032
Prabhu R, Shu HK, Hadjipanayis C, Dhabaan A, Hall W, Raore B, Olson J, Curran W, Oyesiku N, Crocker I (2012) Current dosing paradigm for stereotactic radiosurgery alone after surgical resection of brain metastases needs to be optimized for improved local control. Int J Radiat Oncol Biol Phys 83(1):E61–66. doi:10.1016/J.IJROBP.2011.12.017
Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J, Farnan N (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of rtog protocol 90-05. Int J Radiat Oncol Biol Phys 47(2):291–298
Linskey ME, Andrews DW, Asher AL, Burri SH, Kondziolka D, Robinson PD, Ammirati M, Cobbs CS, Gaspar LE, Loeffler JS, McDermott M, Mehta MP, Mikkelsen T, Olson JJ, Paleologos NA, Patchell RA, Ryken TC, Kalkanis SN (2010) The role of stereotactic radiosurgery in the management of patients with newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neuro-oncol 96(1):45–68. doi:10.1007/S11060-009-0073-4
Adler JR, Cox RS, Kaplan I, Martin DP (1992) Stereotactic radiosurgical treatment of brain metastases. J Neurosurg 76(3):444–449. doi:10.3171/JNS.1992.76.3.0444
Alexander E 3rd, Moriarty TM, Davis RB, Wen PY, Fine HA, Black PM, Kooy HM, Loeffler JS (1995) Stereotactic radiosurgery for the definitive, noninvasive treatment of brain metastases. J Natl Cancer Inst 87 (1):34–40
Eaton BR, Gebhardt B, Prabhu R, Shu HK, Curran WJ, Jr., Crocker I (2013) Hypofractionated radiosurgery for intact or resected brain metastases: defining the optimal dose and fractionation. Radiat Oncol 8:135. doi:10.1186/1748-717X-8-135
Wang CC, Floyd SR, Chang CH, Warnke PC, Chio CC, Kasper EM, Mahadevan A, Wong ET, Chen CC (2012) Cyberknife hypofractionated stereotactic radiosurgery (hsrs) of resection cavity after excision of large cerebral metastasis: efficacy and safety of an 800 cgy × 3 daily fractions regimen. J Neuro-oncol 106(3):601–610. doi:10.1007/S11060-011-0697-Z
Soltys SG, Adler JR, Lipani JD, Jackson PS, Choi CY, Puataweepong P, White S, Gibbs IC, Chang SD (2008) Stereotactic radiosurgery of the postoperative resection cavity for brain metastases. Int J Radiat Oncol Biol Phys 70(1):187–193. doi:10.1016/J.IJROBP.2007.06.068
Minniti G, Esposito V, Clarke E, Scaringi C, Lanzetta G, Salvati M, Raco A, Bozzao A, MAURIZI ENRICI R (2013) Multidose stereotactic radiosurgery (9 gy × 3) of the postoperative resection cavity for treatment of large brain metastases. Int J Radiat Oncol Biol Phys 86(4):623–629. doi:10.1016/J.IJROBP.2013.03.037
Choi CY, Chang SD, Gibbs IC, Adler JR, Harsh GRT, Atalar B, Lieberson RE, Soltys SG (2012) What is the optimal treatment of large brain metastases? An argument for a multidisciplinary approach. Int J Radiat Oncol Biol Phys 84(3):688–693. doi:10.1016/J.IJROBP.2012.01.028
Gaspar L, Scott C, Rotman M, Asbell S, Phillips T, Wasserman T, McKenna WG, Byhardt R (1997) Recursive partitioning analysis (Rpa) of prognostic factors in three radiation therapy oncology group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 37(4):745–751
Dhabaan A, Schreibmann E, Siddiqi A, Elder E, Fox T, Ogunleye T, Esiashvili N, Curran W, Crocker I, Shu HK (2012) Six degrees of freedom cbct-based positioning for intracranial targets treated with frameless stereotactic radiosurgery. J Appl Clin Med Phys 13(6):3916. doi:10.1120/JACMP.V13I6.3916
Prabhu RS, Dhabaan A, Hall WA, Ogunleye T, Crocker I, Curran WJ, Shu HK (2013) Clinical outcomes for a novel 6 degrees of freedom image guided localization method for frameless radiosurgery for intracranial brain metastases. J Neurooncol 113(1):93–99. doi:10.1007/S11060-013-1093-7
Hall EJ, Giaccia AJ (2006) Radiobiology for the radiologist, 6th edn. Lippincott Williams & Wilkins, Philadelphia
Park C, Papiez L, Zhang S, Story M, Timmerman RD (2008) Universal survival curve and single fraction equivalent dose: useful tools in understanding potency of ablative radiotherapy. Int J Radiat Oncol Biol Phys 70(3):847–852. doi:10.1016/J.IJROBP.2007.10.059
Cancer Therapy Evaluation Program. Common terminology criteria for adverse events, version 3.0. DCTD, NCI, NIH, DHHS
Kalbfleisch JD, Prentice RL (1980) The statistical analysis of failure time data. wiley series in probability and mathematical statistics, Wiley, New York
Gray R (1988) A class of k-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16:1141–1154
Cox DR (1972) Regression models and life tables. J R Stat Soc B34:187–220
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Kwon AK, Dibiase SJ, Wang B, Hughes SL, Milcarek B, Zhu Y (2009) Hypofractionated stereotactic radiotherapy for the treatment of brain metastases. Cancer 115(4):890–898. doi:10.1002/CNCR.24082
Broemme J, Abu-Isa J, Kottke R, Beck J, Wiest R, Malthaner M, Schmidhalter D, Raabe A, Aebersold DM, Pica A (2013) Adjuvant therapy after resection of brain metastases. Frameless image-guided linac-based radiosurgery and stereotactic hypofractionated radiotherapy. Strahlentherapie und Onkologie: Organ der Deutschen Rontgengesellschaft [et al] 189 (9):765–770. doi:10.1007/S00066-013-0409-Z.
Brennan C, Yang TJ, Hilden P, Zhang Z, Chan K, Yamada Y, Chan TA, Lymberis SC, Narayana A, Tabar V, Gutin PH, Ballangrud A, Lis E, Beal K (2014) A phase 2 trial of stereotactic radiosurgery boost after surgical resection for brain metastases. Int J Radiat Oncol Biol Phys 88(1):130–136. doi:10.1016/J.IJROBP.2013.09.051
Hartford AC, Paravati AJ, Spire WJ, Li Z, Jarvis LA, Fadul CE, Rhodes CH, Erkmen K, Friedman J, Gladstone DJ, Hug EB, Roberts DW, Simmons NE (2013) Postoperative stereotactic radiosurgery without whole-brain radiation therapy for brain metastases: potential role of preoperative tumor size. Int J Radiat Oncol Biol Phys 85(3):650–655. doi:10.1016/J.IJROBP.2012.05.027
Ahmed KA, Freilich JM, Abuodeh Y, Figura N, Patel N, Sarangkasiri S, Chinnaiyan P, Yu HH, Etame AB, Rao NG (2014) Fractionated stereotactic radiotherapy to the post-operative cavity for radioresistant and radiosensitive brain metastases. J Neuro-oncol 118(1):179–186. doi:10.1007/S11060-014-1417-2
Steinmann D, Maertens B, Janssen S, Werner M, Fruhauf J, Nakamura M, Christiansen H, Bremer M (2012) Hypofractionated stereotactic radiotherapy (hfsrt) after tumour resection of a single brain metastasis: report of a single-centre individualized treatment approach. J Cancer Res Clin Oncol 138(9):1523–1529. doi:10.1007/S00432-012-1227-X
Conflict of interest
Ian Crocker serves as a consultant for Varian Medical Systems (Varian, Palo Alto, CA).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eaton, B.R., La Riviere, M.J., Kim, S. et al. Hypofractionated radiosurgery has a better safety profile than single fraction radiosurgery for large resected brain metastases. J Neurooncol 123, 103–111 (2015). https://doi.org/10.1007/s11060-015-1767-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1767-4