Abstract
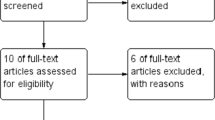
Laparoscopic sleeve gastrectomy with omentopexy (O-LSG) has been compared to laparoscopic sleeve gastrectomy with no-omentopexy (NO-LSG) in terms of postoperative outcomes and one-year anthropometric results. This systematic review with meta-analysis aimed to compare the utility of omentopexy in sleeve gastrectomy. We performed a systematic review with meta-analysis according to PRISMA 2020 and AMSTAR 2 guidelines. We included studies that systematically searched electronic databases and compared the O-LSG with the NO-LSG conducted through 1st March 2023. The bibliographic research yielded 13 eligible studies. These studies included 5514 patients. The O-LSG is associated with lower leakage (OR = 0.22; 95% CI [0.08, 0.55], p = 0.001), bleeding (OR = 0.33; 95% CI [0.19, 0.57], p < 0.0001), vomiting (OR = 0.50; 95% CI [0.28, 0.89], p = 0.02), twist (OR = 0.09; 95% CI [0.02, 0.39], p = 0.001), and shorter hospital stay (MD = − 0.33; 95% CI [− 0.61, − 0.05], p = 0.02) compared with NO-LSG. The O-LSG is associated with longer operative time (MD = 8.15; 95% CI [3.65, 12.64], p = 0.0004) than the NO-LSG. There were no differences between the two groups in terms of postoperative GERD (OR = 0.53; 95% CI [0.27, 1.02], p = 0.06), readmission (OR = 0.60; 95% CI [0.27, 1.37], p = 0.23), and one-year total weight loss (MD = 2.06; 95% CI [− 1.53, 5.65], p = 0.26). In the subgroup analysis including only RCTs, postoperative GERD was lower in the O-LSG (OR = 0.26; 95% CI [0.11, 0.63], p = 0.003). Our systematic review and meta-analysis concluded that omentopexy in sleeve gastrectomy is feasible and safe It reduced leakage, bleeding, and twist. It probably increased the operative time. It may reduce vomiting, GERD, and hospital stay. We don't know if it led to an additional readmission rate or one-year total weight loss.
Registration The protocol was registered in PROSPERO with the ID CRD42022336790.








Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article.
References
Welbourn R, Hollyman M, Kinsman R, Dixon J, Liem R, Ottosson J et al (2019) Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the fourth IFSO global registry report 2018. Obes Surg mars 29(3):782–795
Aurora AR, Khaitan L, Saber AA (2012) Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg Endosc juin 26(6):1509–1515
Jossart GH (2010) Complications of sleeve gastrectomy: bleeding and prevention. Surg Laparosc Endosc Percutan Tech juin 20(3):146–147
Bransen J, Gilissen LPL, van Rutte PWJ, Nienhuijs SW (2015) Costs of leaks and bleeding after sleeve gastrectomies. Obes Surg 25(10):1767–1771
Oweira H, Mazotta A, Mehrabi A, Reissfelder C, Rahbari N, Betzler A et al (2022) Using a reinforced stapler decreases the incidence of postoperative pancreatic fistula after distal pancreatectomy: a systematic review and meta-analysis. World J Surg 46:1–11
Dziri C, Paquet JC, Hay JM, Fingerhut A, Msika S, Zeitoun G et al (1999) Omentoplasty in the prevention of deep abdominal complications after surgery for hydatid disease of the liver: a multicenter, prospective, randomized trial. French associations for surgical research. J Am Coll Surg 188(3):281–289
Lin BC, Liao CH, Wang SY, Hwang TL (2017) Laparoscopic repair of perforated peptic ulcer: simple closure versus omentopexy. J Surg Res 220:341–345
D’Ugo S, Gentileschi P, Benavoli D, Cerci M, Gaspari A, Berta RD et al (2014) Comparative use of different techniques for leak and bleeding prevention during laparoscopic sleeve gastrectomy: a multicenter study. Surg Obes Related Dis 10(3):450–454
Zarzycki P, Kulawik J, Małczak P, Rubinkiewicz M, Wierdak M, Major P (2021) Laparoscopic sleeve gastrectomy with omentopexy: is it really a promising method?—A systematic review with meta-analysis. Obes Surg 31(6):2709–2716
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372:n160
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg sept 73(9):712–716
Campbell MK, Elbourne DR, Altman DG (2004) CONSORT statement: extension to cluster randomised trials. BMJ 328(7441):702–708
Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:14898
Peterson J, Welch V, Losos M, Tugwell P (2011) The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hosp Res Ins 2(1):1–12
Higgins JP (2008) Cochrane handbook for systematic reviews of interventions version 5.0. 1. The Cochrane Collaboration. http://www.cochrane-handbook.org
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5(1):1–10
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J et al (2011) GRADE guidelines: 3 rating the quality of evidence. J Clin Epidemiol 64(4):401–406
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions: Cochrane book series.
Abdallah E, Zakaria M, Fikry M, Abdelnaby M, Gado W, Elbaz SA et al (2020) Laparoscopic sleeve gastrectomy with T-shaped omentoplasty: impact on the early postoperative outcomes. Obes Surg 30(10):3735–3741
Abosayed AK, Mostafa MS (2022) Omentopexy effect on the upper gastrointestinal symptoms and the esophagogastroduodenoscopy findings in patients undergoing sleeve gastrectomy. Obes Surg 32(6):1864–1871
Abou-Ashour HS (2022) Impact of gastropexy/omentopexy on gastrointestinal symptoms after laparoscopic sleeve gastrectomy. Obes Surg 32(3):729–736
Afaneh C, Costa R, Pomp A, Dakin G (2015) A prospective randomized controlled trial assessing the efficacy of omentopexy during laparoscopic sleeve gastrectomy in reducing postoperative gastrointestinal symptoms. Surg Endosc 29(1):41–47
AlHaddad M, AlAtwan AA, AlKhadher T, AlJewaied A, Qadhi I, AlSabah SK (2021) Omentopexy during laparoscopic sleeve gastrectomy: is it effective in reducing postoperative gastrointestinal symptoms. A retrospective cohort study. Ann Med Surg (Lond) 65:102369
Fouad MMB, Ibraheim SMN, Ibraheim P, Maurice KK, Saber AT (2022) Assessment of the role of omentopexy in laparoscopic sleeve gastrectomy: a tertiary center experience. J Laparoendosc Adv Surg Tech A 32(9):962–968
Khalifa I, Balamoun H, Lasheen O, Ibrahim M, Mashhour A, Kandeel A (2018) Effect of omental reattachment on food tolerance and gastric emptying in laparoscopic sleeve gastrectomy. Bariatr Surg Pract Patient Care 13:68
Lale A, Aygen E, Kirkil C, Artas H, Yur M (2020) Efficacy of staple line reinforcement with omentopexy during laparoscopic sleeve gastrectomy on postoperative complications: experience of a single center. Surg Laparosc Endosc Percutan Tech 31(2):181–187
Nosrati SS, Pazouki A, Sabzikarian M, Pakaneh M, Kabir A, Kermansaravi M (2021) Can omentopexy reduce the incidence of gastroesophageal reflux disease after laparoscopic sleeve gastrectomy. Obes Surg 31(1):274–281
Pilone V, Tramontano S, Renzulli M, Romano M, Monda A, Albanese A et al (2019) Omentopexy with Glubran®2 for reducing complications after laparoscopic sleeve gastrectomy: results of a randomized controlled study. BMC Surg 19(Suppl 1):56
Sharma N, Chau WY (2020) Remodifying omentopexy technique used with laparoscopic sleeve gastrectomy: does it change any outcomes? Obes Surg avr 30(4):1527–1535
Våge V, Behme J, Jossart G, Andersen JR (2020) Gastropexy predicts lower use of acid-reducing medication after laparoscopic sleeve gastrectomy. A prospective cohort study. Int J Surg 74:113–117
Yapalak Y, Yigman S, Gonultas C, Coskun H, Yardimci E (2023) The effects of the staple line reinforcement procedures on gastrointestinal symptoms and its early results in sleeve gastrectomy. J Laparoendosc Adv Surg Tech A 33(2):162–170
Chaouch MA, Kellil T, Taieb SK, Zouari K (2021) Barbed versus conventional thread used in laparoscopic gastric bypass: a systematic review and meta-analysis. Langenbecks Arch Surg 406(4):1015–1022
Parikh M, Issa R, McCrillis A, Saunders JK, Ude-Welcome A, Gagner M (2013) Surgical strategies that may decrease leak after laparoscopic sleeve gastrectomy: a systematic review and meta-analysis of 9991 cases. Ann Surg févr 257(2):231–237
Shoar S, Poliakin L, Khorgami Z, Rubenstein R, El-Matbouly M, Levin JL et al (2017) Efficacy and safety of the over-the-scope clip (OTSC) system in the management of leak and fistula after laparoscopic sleeve gastrectomy: a systematic review. Obes Surg 27(9):2410–2418
Gagner M, Buchwald JN (2014) Comparison of laparoscopic sleeve gastrectomy leak rates in four staple-line reinforcement options: a systematic review. Surg Obes Related Dis 10(4):713–723
Knapps J, Ghanem M, Clements J, Merchant AM (2013) A systematic review of staple-line reinforcement in laparoscopic sleeve gastrectomy. JSLS J Soc Laparoendosc Surg 17(3):390
Dogra P, Kaushik R, Singh S, Bhardwaj S (2023) Risk factors for leak after omentopexy for duodenal ulcer perforations. Eur J Trauma Emerg Surg 49(2):1163–1167
Litbarg NO, Gudehithlu KP, Sethupathi P, Arruda JAL, Dunea G, Singh AK (2007) Activated omentum becomes rich in factors that promote healing and tissue regeneration. Cell Tissue Res 328(3):487–497
Deitel M, Gagner M, Erickson AL, Crosby RD (2011) Third international summit: current status of sleeve gastrectomy. Surg Obes Related Dis 7(6):749–759
Halliday TA, Sundqvist J, Hultin M, Walldén J (2017) Post-operative nausea and vomiting in bariatric surgery patients: an observational study. Acta Anaesthesiol Scand mai 61(5):471–479
Slater BJ, Collings A, Dirks R, Gould JC, Qureshi AP, Juza R et al (2022) Multi-society consensus conference and guideline on the treatment of gastroesophageal reflux disease (GERD). Surg Endosc. https://doi.org/10.1007/s00464-022-09817-3
Filho AMM, Silva LB, Godoy ES, Falcão AM, de Quadros LG, Zotarelli Filho IJ et al (2019) Omentopexy in sleeve gastrectomy reduces early gastroesophageal reflux symptoms. Surg Laparosc Endosc Percutan Techiques. 29(3):155–161
Abd Ellatif ME, Abbas A, El Nakeeb A, Magdy A, Salama AF, Bashah MM et al (2017) Management options for twisted gastric tube after laparoscopic sleeve gastrectomy. Obes Surg 27(9):2404–2409
Burgos AM, Csendes A, Braghetto I (2013) Gastric stenosis after laparoscopic sleeve gastrectomy in morbidly obese patients. Obes Surg 23(9):1481–1486
Elbalshy MA, Fayed AM, Abdelshahid MA, Alkhateep YM (2017) Role of staple line fixation during laparoscopic sleeve gastrectomy. Int Surg J 5(1):156
Arslan E, Banli O, Sipahi M, Yagci G (2018) Effects and results of omentopexy during laparoscopic sleeve gastrectomy. Surg Laparosc Endosc Percutan Tech 28(3):174–177
Kermansaravi M, Parmar C, Chiappetta S, Shikora S, Aminian A, Abbas SI et al (2023) Best practice approach for redo-surgeries after sleeve gastrectomy, an expert’s modified Delphi consensus. Surg Endosc 37(3):1617–1628
Labib MF (2020) The omentopexy role in the prevention of post-operative gastric sleeve surgery complications. Egypt J Hosp Med 81(6):2199–2204
Acknowledgements
None
Funding
The authors have no conflicts of interest or financial ties to disclose for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors participated in the study on the conception, design of the research, and data acquisition. All the authors validated the final version of the article.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest or support to disclose.
Ethical approval
Ethics approval and consent to participate in this retrospective research involving human participants are not applicable in this review. Provenance and peer review: Not commissioned, externally peer-reviewed.
Human or animal rights
This research involves Human participants. It is a retrospective analysis of published cases and did not require informed consent. Ethics approval and consent to participate were not applicable in this review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chaouch, M.A., Khalfallah, M., Jabra, S.B. et al. Omentopexy versus no omentopexy in sleeve gastrectomy: an updated systematic review and meta-analysis. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01794-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01794-7