Abstract
Purpose
Osteoporosis is one of the most common conditions among adults worldwide. It also presents a challenge among patients undergoing spinal surgery. Use of Teriparatide and bisphosphonates in such patients has been shown to improve outcomes after fusion surgery, including successful fusion, decreased risk of instrumentation failure, and patient-reported outcomes. Herein, we performed a systematic review and indirect meta-analysis of available literature on outcomes of fusion surgery after use of bisphosphonates or Teriparatide.
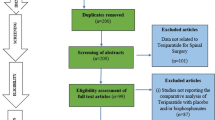
Methods
We conducted a comprehensive search of all databases (Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid Embase, Ovid Cochrane Central Register of Controlled Trials, Ovid Cochrane Database of Systematic Reviews, and Scopus) to identify studies assessing outcomes of spinal fusion among osteoporotic patients after use of Teriparatide or bisphosphonate. Four authors independently screened electronic search results, and all four authors independently performed study selection. Two authors performed independent data extraction and assessed the studies’ risk of bias assessment using standardized forms of Revised Cochrane risk-of-bias tool for randomized trials (RoB 2) and Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I).
Results
Nineteen studies were included in the final analysis. A total of 13 studies evaluated the difference in fusion rate between bisphosphonates and Teriparatide or control group. Fusion rate was higher for bisphosphonates (effect size (ES) 83%, 95% CI 77–89%) compared with Teriparatide (ES 71%, 95% CI 57–85%), with the p value for heterogeneity between groups without statistical significance (p = 0.123). Five studies assessed the impact of using bisphosphonate or Teriparatide on screw loosening. The rate of screw loosening was higher for bisphosphonates (ES 19%, 95% CI 13–25%) compared with Teriparatide (ES 13%, 95% CI 9–16%) without statistical significance (p = 0.52).
Conclusion
Our results indicate that while both agents may be associated with positive outcomes, bisphosphonates may be associated with a higher fusion rate, while Teriparatide may be associated with lower screw loosening. The decision to treat with either agent should be tailored individually for each patient keeping in consideration the adverse effect and pharmacokinetic profiles.







Similar content being viewed by others
References
Reginster J-Y, Burlet N (2006) Osteoporosis: a still increasing prevalence. Bone 38:S4–S9
Farmer RP, Herbert B, Cuellar DO, Hao J, Stahel PF, Yasui R et al (2014) Osteoporosis and the orthopaedic surgeon: basic concepts for successful co-management of patients’ bone health. Int Orthop 38:1731–1738
Bjerke BT, Zarrabian M, Aleem IS, Fogelson JL, Currier BL, Freedman BA et al (2018) Incidence of osteoporosis-related complications following posterior lumbar fusion. Global Spine J 8:563–569
Park SB, Chung CK (2011) Strategies of spinal fusion on osteoporotic spine. J Korean Neurosurg Soc 49:317–322
Eastell R, Walsh JS (2017) Anabolic treatment for osteoporosis: teriparatide. Clin Cases Miner Bone Metab 14:173–178
Lewiecki EM (2010) Bisphosphonates for the treatment of osteoporosis: insights for clinicians. Ther Adv Chronic Dis 1:115–128
Liu W-B, Zhao W-T, Shen P, Zhang F-J (2018) The effects of bisphosphonates on osteoporotic patients after lumbar fusion: a meta-analysis. Drug Des Devel Ther 12:2233–2240
Wanderman N, Alvi M, Yolcu Y, Carlson B, Sebastian A, Bydon M et al (2019) Is Teriparatide beneficial to spinal fusion surgery in the older patient?: a narrative review. Clin Spine Surg 32:182–190
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 350:g7647
Wilson EB (1927) Probable inference, the law of succession, and statistical inference. J Am Stat Assoc Taylor & Francis 22:209–212
Freeman MF, Tukey JW (1950) Transformations related to the angular and the square root. Ann Math Stat. Institute of Mathematical Statistics 21:607–611
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ. 327:557–560
Higgins JPT (2008) Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. Int. J. Epidemiol 1158–60
Sterne JA, Egger M (2001) Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol 54:1046–1055
Kim S-M, Rhee W, Ha S, Lim JH, Jang IT (2014) Influence of alendronate and endplate degeneration to single level posterior lumbar spinal interbody fusion. Korean J Spine 11:221–226
Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, Ochiai N et al (2012) Teriparatide accelerates lumbar posterolateral fusion in women with postmenopausal osteoporosis: prospective study. Spine 37:E1464–E1468
Ohtori S, Orita S, Yamauchi K, Eguchi Y, Aoki Y, Nakamura J et al (2017) Does discontinuing Teriparatide treatment and replacing it with bisphosphonate maintain the volume of the bone fusion mass after lumbar posterolateral fusion in women with postmenopausal osteoporosis? Asian Spine J 11:272–277
Wang M, Meng X, Li Y, Feng Y, Chang Z, Hai Y (2016) Effects of anti-osteoporosis treatment in the elderly with anterior cervical discectomy and fusion. Acta Orthop Traumatol Turc 50:186–190
Chen F, Dai Z, Kang Y, Lv G, Keller ET, Jiang Y (2016) Effects of zoledronic acid on bone fusion in osteoporotic patients after lumbar fusion. Osteoporos Int 27:1469–1476
Cho PG, Ji GY, Shin DA, Ha Y, Yoon DH, Kim KN (2017) An effect comparison of teriparatide and bisphosphonate on posterior lumbar interbody fusion in patients with osteoporosis: a prospective cohort study and preliminary data. Eur Spine J 26:691–697
Ding Q, Chen J, Fan J, Li Q, Yin G, Yu L (2017) Effect of zoledronic acid on lumbar spinal fusion in osteoporotic patients. Eur Spine J 26:2969–2977
Jespersen AB, Andresen ADK, Jacobsen MK, Andersen MØ, Carreon LY (2019) Does systemic administration of parathyroid hormone after noninstrumented spinal fusion surgery improve fusion rates and fusion mass in elderly patients compared to placebo in patients with degenerative lumbar spondylolisthesis? Spine 44:157–162
Kaliya-Perumal A-K, Lu M-L, Luo C-A, Tsai T-T, Lai P-L, Chen L-H et al (2017) Retrospective radiological outcome analysis following teriparatide use in elderly patients undergoing multilevel instrumented lumbar fusion surgery. Medicine 96:e5996
Kim JW, Park SW, Kim YB, Ko MJ (2018) The effect of postoperative use of teriparatide reducing screw loosening in osteoporotic patients. J Korean Neurosurg Soc 61:494–502
Li C, Wang H-R, Li X-L, Zhou X-G, Dong J (2012) The relation between zoledronic acid infusion and interbody fusion in patients undergoing transforaminal lumbar interbody fusion surgery. Acta Neurochir 154:731–738
Nagahama K, Kanayama M, Togawa D, Hashimoto T, Minami A (2011) Does alendronate disturb the healing process of posterior lumbar interbody fusion? A prospective randomized trial. J Neurosurg Spine 14:500–507
Ushirozako H, Hasegawa T, Ebata S, Oba H, Ohba T, Mukaiyama K et al (2019) Weekly teriparatide administration and preoperative anterior slippage of the cranial vertebra next to fusion segment < 2 mm promote osseous union after posterior lumbar interbody fusion. Spine 44:E288–E297
Ebata S, Takahashi J, Hasegawa T, Mukaiyama K, Isogai Y, Ohba T et al (2017) Role of weekly teriparatide administration in osseous union enhancement within six months after posterior or transforaminal lumbar interbody fusion for osteoporosis-associated lumbar degenerative disorders: a multicenter, prospective randomized study. J Bone Joint Surg Am 99:365–372
Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kuniyoshi K et al (2015) More than 6 months of teriparatide treatment was more effective for bone union than shorter treatment following lumbar posterolateral fusion surgery. Asian Spine J 9:573–580
Park Y-S, Kim H-S, Baek S-W, Kong D-Y, Ryu J-A (2013) The effect of zoledronic acid on the volume of the fusion-mass in lumbar spinal fusion. Clin Orthop Surg 5:292–297
Seki S, Hirano N, Kawaguchi Y, Nakano M, Yasuda T, Suzuki K et al (2017) Teriparatide versus low-dose bisphosphonates before and after surgery for adult spinal deformity in female Japanese patients with osteoporosis. Eur Spine J 26:2121–2127
Tu C-W, Huang K-F, Hsu H-T, Li H-Y, Yang SS-D, Chen Y-C (2014) Zoledronic acid infusion for lumbar interbody fusion in osteoporosis. J Surg Res 192:112–116
Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, Ochiai N et al (2013) Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine 38:E487–E492
Chin DK, Park JY, Yoon YS, Kuh SU, Jin BH, Kim KS et al (2007) Prevalence of osteoporosis in patients requiring spine surgery: incidence and significance of osteoporosis in spine disease. Osteoporos Int 18:1219–1224
Lehman RA Jr, Polly DW Jr, Kuklo TR, Cunningham B, Kirk KL, Belmont PJ Jr (2003) Straight-forward versus anatomic trajectory technique of thoracic pedicle screw fixation: a biomechanical analysis. Spine 28:2058–2065
Lee JH, Lee J-H, Park JW, Shin YH (2012) The insertional torque of a pedicle screw has a positive correlation with bone mineral density in posterior lumbar pedicle screw fixation. J Bone Joint Surg (Br) 94:93–97
DeWald CJ, Stanley T (2006) Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65: surgical considerations and treatment options in patients with poor bone quality. Spine 31:S144–S151
Buerba RA, Sharma A, Ziino C, Arzeno A, Ajiboye RM (2018) Bisphosphonate and teriparatide use in thoracolumbar spinal fusion: a systematic review and meta-analysis of comparative studies. Spine 43:E1014–E1023
Fretes N, Vellios E, Sharma A, Ajiboye RM (2019) Radiographic and functional outcomes of bisphosphonate use in lumbar fusion: a systematic review and meta-analysis of comparative studies. Eur Spine J. https://doi.org/10.1007/s00586-019-06090-2
Huang RC, Khan SN, Sandhu HS, Metzl JA, Cammisa FP Jr, Zheng F et al (2005) Alendronate inhibits spine fusion in a rat model. Spine 30:2516–2522
Xue Q, Li H, Zou X, Dalstra M, Lind M, Christensen FB et al (2010) Alendronate treatment improves bone-pedicle screw interface fixation in posterior lateral spine fusion: an experimental study in a porcine model. Int Orthop 34:447–451
Hirsch BP, Unnanuntana A, Cunningham ME, Lane JM (2013) The effect of therapies for osteoporosis on spine fusion: a systematic review. Spine J 13:190–199
Inoue G, Ueno M, Nakazawa T, Imura T, Saito W, Uchida K et al (2014) Teriparatide increases the insertional torque of pedicle screws during fusion surgery in patients with postmenopausal osteoporosis. J Neurosurg Spine 21:425–431
O’Loughlin PF, Cunningham ME, Bukata SV, Tomin E, Poynton AR, Doty SB et al (2009) Parathyroid hormone (1-34) augments spinal fusion, fusion mass volume, and fusion mass quality in a rabbit spinal fusion model. Spine 34:121–130
Sugiura T, Kashii M, Matsuo Y, Morimoto T, Honda H, Kaito T et al (2015) Intermittent administration of teriparatide enhances graft bone healing and accelerates spinal fusion in rats with glucocorticoid-induced osteoporosis. Spine J 15:298–306
Ming N, Cheng JT-Y, Rui Y-F, Chan K-M, Kuhstoss S, Ma YL et al (2012) Dose-dependent enhancement of spinal fusion in rats with teriparatide (PTH[1-34]). Spine 37:1275–1282
Seeman E (2003) Reduced bone formation and increased bone resorption: rational targets for the treatment of osteoporosis. Osteoporos Int 14(Suppl 3):S2–S8
Heaney RP (2003) Remodeling and skeletal fragility. Osteoporos Int 14(Suppl 5):S12–S15
Russell RGG, Watts NB, Ebetino FH, Rogers MJ (2008) Mechanisms of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacy. Osteoporos Int 19:733–759
Zhou J, Ma X, Wang T, Zhai S (2016) Comparative efficacy of bisphosphonates in short-term fracture prevention for primary osteoporosis: a systematic review with network meta-analyses. Osteoporos Int 27:3289–3300
Santos ERG, Goss DG, Morcom RK, Fraser RD (2003) Radiologic assessment of interbody fusion using carbon fiber cages. Spine 28:997–1001
Ito Z, Imagama S, Kanemura T, Hachiya Y, Miura Y, Kamiya M et al (2013) Bone union rate with autologous iliac bone versus local bone graft in posterior lumbar interbody fusion (PLIF): a multicenter study. Eur Spine J 22:1158–1163
Lenke LG, Bridwell KH, Bullis D, Betz RR, Baldus C, Schoenecker PL (1992) Results of in situ fusion for isthmic spondylolisthesis. J Spinal Disord 5:433–442
Glassman SD, Dimar JR, Carreon LY, Campbell MJ, Puno RM, Johnson JR (2005) Initial fusion rates with recombinant human bone morphogenetic protein-2/compression resistant matrix and a hydroxyapatite and tricalcium phosphate/collagen carrier in posterolateral spinal fusion. Spine 30:1694–1698
Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K (1995) Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine 20:1410–1418
Sandén B, Olerud C, Petrén-Mallmin M, Johansson C, Larsson S (2004) The significance of radiolucent zones surrounding pedicle screws. Definition of screw loosening in spinal instrumentation. J Bone Joint Surg (Br) 86:457–461
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presented as a poster at the Orthopedic Research Society Annual Meeting February 8–11, 2020, at Phoenix, Arizona
Rights and permissions
About this article
Cite this article
Tsai, S.H.L., Chien, RS., Lichter, K. et al. Teriparatide and bisphosphonate use in osteoporotic spinal fusion patients: a systematic review and meta-analysis. Arch Osteoporos 15, 158 (2020). https://doi.org/10.1007/s11657-020-00738-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-020-00738-z