Abstract
Purpose
In patients undergoing lumbar fusion, osteoporosis has been shown to lead to poorer outcomes and greater incidence of fusion-related complications. Given the undesirable effect of osteoporosis on lumbar fusion surgery, a number of medications have been proposed for use in the peri- and postoperative period to mitigate risks and enhance outcomes. The purpose of this review was to summarize and synthesize the current literature regarding medical management of osteoporosis in the context of lumbar fusion surgery.
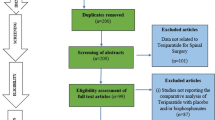
Methods
A literature search of PubMed, Embase, and Web of Science was conducted in October 2016, using permutations of various search terms related to osteoporosis, medications, and lumbar fusion.
Results
Teriparatide injections may lead to faster, more successful fusion, and may reduce fusion-related complications. Bisphosphonate therapy likely does not hinder fusion outcomes and may be useful in reducing certain complications of fusion in osteoporotic patients. Calcitonin and selective estrogen receptor modulator therapy show mixed results, but more research is necessary to make a recommendation. Vitamin D deficiency is associated with poor fusion outcomes, but evidence for supplementation in patients with normal serum levels is weak.
Conclusions
Overall, the current body of research appears to support the use of teriparatide therapy to enhance lumbar fusion outcomes in the osteoporotic patient, although the extent of research on this topic is limited. Additionally, very little evidence exists to cease any of the mentioned osteoporosis treatments prior to lumbar fusion.

Similar content being viewed by others
References
Centers for Disease Control. Percentage of adults aged 65 and over with osteoporosis or low bone mass at the femur neck or lumbar spine: United States, 2005–2010 [Centers for Disease Control web site]. August 2015. Available at: http://www.cdc.gov/nchs/data/hestat/osteoporsis/osteoporosis2005_2010.htm Accessed October 13th, 2016
Office of the Surgeon General (US). Bone health and osteoporosis: a report of the surgeon general. Rockville (MD): Office of the Surgeon General (US); 2004. Reports of the Surgeon General
Siris ES, Brenneman SK, Barrett-Connor E, Miller PD, Sajjan S, Berger ML, Chen YT (2006) The effect of age and bone mineral density on the absolute, excess, and relative risk of fracture in postmenopausal women aged 50–99: results from the National Osteoporosis Risk Assessment (NORA). Osteoporos Int 17:565–574
Vogt MT, Rubin DA, San Valentin R et al (1999) Degenerative lumbar listhesis and bone mineral density in elderly women. The study of osteoporotic fractures. Spine 24(23):2536–2541
Dipaola CP, Bible JE, Biswas D, Dipaola M, Grauer JN, Rechtine GR (2009) Survey of spine surgeons on attitudes regarding osteoporosis and osteomalacia screening and treatment for fractures, fusion surgery, and pseudoarthrosis. Spine J 9(7):537–544
Moazzaz P, Gupta MC, Gilotra MM, Gilotra MN, Maitra S, Theerajunyaporn T, Chen JL, Reddi AH, Martin RB (2005) Estrogen-dependent actions of bone morphogenetic protein-7 on spine fusion in rats. Spine 30(15):1706–1711
Nakao S, Minamide A, Kawakami M, Boden SD, Yoshida M (2011) The influence of alendronate on spine fusion in an osteoporotic animal model. Spine 36(18):1446–1452
Park SB, Park SH, Kim NH, Chung CK (2013) BMP-2 induced early bone formation in spine fusion using rat ovariectomy osteoporosis model. Spine J 13(10):1273–1280
Park SB, Park SH, Kang YK, Chung CK (2014) The time-dependent effect of ibandronate on bone graft remodeling in an ovariectomized rat spinal arthrodesis model. Spine J 14(8):1748–1757
Park SB, Kim CH, Hong M, Yang HJ, Chung CK (2016) Effect of a selective estrogen receptor modulator on bone formation in osteoporotic spine fusion using an ovariectomized rat model. Spine J 16(1):72–81
Zhou Z, Tian FM, Wang P et al (2015) Alendronate prevents intervertebral disc degeneration adjacent to a lumbar fusion in ovariectomized rats. Spine 40(20):1073–1083
Zhou Z, Tian FM, Gou Y, Wang P, Zhang H, Song HP, Shen Y, Zhang YZ, Zhang L (2016) Enhancement of lumbar fusion and alleviation of adjacent segment disc degeneration by intermittent PTH(1-34) in ovariectomized rats. J Bone Miner Res 31(4):828–838
Andersen T, Christensen FB, Langdahl BL, Ernst C, Fruensgaard S, Østergaard J, Andersen JL, Rasmussen S, Niedermann B, Høy K, Helmig P, Holm R, Lindblad BE, Hansen ES, Egund N, Bünger C (2010) Fusion mass bone quality after uninstrumented spinal fusion in older patients. Eur Spine J 19(12):2200–2208
Schreiber JJ, Hughes AP, Taher F et al (2014) An association can be found between Hounsfield units and success of lumbar spine fusion. Hospital Spec Surg 10(1):25–29
Hou Y, Yuan W (2012) Influences of disc degeneration and bone mineral density on the structural properties of lumbar end plates. Spine J 12(3):249–256
Kim SM, Rhee W, Ha S, Lim JH, Jang IT (2014) Influence of alendronate and endplate degeneration to single level posterior lumbar spinal interbody fusion. Korean J Spine 11(4):221–226
Kwon BK, Elgafy H, Keynan O, Fisher CG, Boyd MC, Paquette SJ, Dvorak MF (2006) Progressive junctional kyphosis at the caudal end of lumbar instrumented fusion: etiology, predictors, and treatment. Spine 31(17):1943–1951
Li YC, Yang SC, Chen HS, Kao YH, Tu YK (2015) Impact of lumbar instrumented circumferential fusion on the development of adjacent vertebral compression fracture. Bone Joint J 97-B(10):1411–1416
Meredith DS, Taher F, Cammisa FP Jr et al (2013) Incidence, diagnosis, and management of sacral fractures following multilevel spinal arthrodesis. Spine J 13(11):1464–1469
Meredith DS, Schreiber JJ, Taher F, Cammisa FP Jr, Girardi FP (2013) Lower preoperative Hounsfield unit measurements are associated with adjacent segment fracture after spinal fusion. Spine 38(5):415–418
Oh KW, Lee JH, Lee JH, et al (2016) The correlation between cage subsidence, bone mineral density, and clinical results in posterior lumbar interbody fusion. Clin Spine Surg
Park SJ, Lee CS, Chung SS, et al (2016) Different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: survivorship analysis of 160 patients. Neurosurgery
Tempel ZJ, Gandhoke GS, Okonkwo DO, Kanter AS (2015) Impaired bone mineral density as a predictor of graft subsidence following minimally invasive transpsoas lateral lumbar interbody fusion. Eur Spine J 24(3):414–419
Toyone T, Ozawa T, Kamikawa K, Watanabe A, Matsuki K, Yamashita T, Shiboi R, Takeuchi M, Wada Y, Inada K, Aoki Y, Inoue G, Ohtori S, Tanaka T (2010) Subsequent vertebral fractures following spinal fusion surgery for degenerative lumbar disease: a mean ten-year follow-up. Spine 35(21):1915–1918
Babat LB, McLain R, Milks R, Ferrara L, Sohn MJ (2005) The effects of the antiresorptive agents calcitonin and pamidronate on spine fusion in a rabbit model. Spine J 5(5):542–547
Huang RC, Khan SN, Sandhu HS, Metzl JA, Cammisa FP Jr, Zheng F, Sama AA, Lane JM (2005) Alendronate inhibits spine fusion in a rat model. Spine 30(22):2516–2522
Lehman RA Jr, Kuklo TR, Freedman BA et al (2004) The effect of alendronate sodium on spinal fusion: a rabbit model. Spine J 4(1):36–43
Xue Q, Li H, Zou X, Bünger M, Egund N, Lind M, Christensen FB, Bünger C (2005) The influence of alendronate treatment and bone graft volume on posterior lateral spine fusion in a porcine model. Spine 30(10):1116–1121
Takahata M, Ito M, Abe Y, Abumi K, Minami A (2008) The effect of anti-resorptive therapies on bone graft healing in an ovariectomized rat spinal arthrodesis model. Bone 43(6):1057–1066
Yasen M, Li X, Jiang L, Yuan W, Che W, Dong J (2015) Effect of zoledronic acid on spinal fusion outcomes in an ovariectomized rat model of osteoporosis. J Orthop Res 33(9):1297–1304
Nagahama K, Kanayama M, Togawa D, Hashimoto T, Minami A (2011) Does alendronate disturb the healing process of posterior lumbar interbody fusion? A prospective randomized trial. J Neurosurg Spine 14(4):500–507
Chen F, Dai Z, Kang Y, Lv G, Keller ET, Jiang Y (2016) Effects of zoledronic acid on bone fusion in osteoporotic patients after lumbar fusion. Osteoporos Int 27(4):1469–1476
Park YS, Kim HS, Baek SW, Kong DY, Ryu JA (2013) The effect of zoledronic acid on the volume of the fusion-mass in lumbar spinal fusion. Clin Orthop Surg 5(4):292–297
Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kuniyoshi K, Aoki Y, Nakamura J, Miyagi M, Suzuki M, Kubota G, Inage K, Sainoh T, Sato J, Shiga Y, Abe K, Fujimoto K, Kanamoto H, Inoue G, Takahashi K (2015) More than 6 months of teriparatide treatment was more effective for bone union than shorter treatment following lumbar posterolateral fusion surgery. Asian Spine J 9(4):573–580
Ohtori S, Inoue G, Orita S et al (2012) Teriparatide accelerates lumbar posterolateral fusion in women with postmenopausal osteoporosis: prospective study. Spine 37(23):1464–1468
Cho PG, Ji GY, Shin DA, Ha Y, Yoon DH, Kim KN (2015) An effect comparison of teriparatide and bisphosphonate on posterior lumbar interbody fusion in patients with osteoporosis: a prospective cohort study and preliminary data. Eur Spine J 26:691–697. https://doi.org/10.1007/s00586-015-4342-y
Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kishida S, Kuniyoshi K, Aoki Y, Nakamura J, Ishikawa T, Miyagi M, Kamoda H, Suzuki M, Kubota G, Sakuma Y, Oikawa Y, Inage K, Sainoh T, Takaso M, Toyone T, Takahashi K (2013) Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine 38(8):E487–E492
Inoue G, Ueno M, Nakazawa T, Imura T, Saito W, Uchida K, Ohtori S, Toyone T, Takahira N, Takaso M (2014) Teriparatide increases the insertional torque of pedicle screws during fusion surgery in patients with postmenopausal osteoporosis. J Neurosurg Spine 21(3):425–431
Xu Y, Zhou M, Liu H, Zhang Q, Hu Z, Zhang N, Ren Y (2014) Effect of 1,25-dihydroxyvitamin D3 on posterior transforaminal lumbar interbody fusion in patients with osteoporosis and lumbar disc degenerative disease. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 28(8):969–972
Tu CW, Huang KF, Hsu HT, Li HY, Yang SSD, Chen YC (2014) Zoledronic acid infusion for lumbar interbody fusion in osteoporosis. J Surg Res 192(1):112–116
Ebata S, Takahashi J, Hasegawa T, Mukaiyama K, Isogai Y, Ohba T, Shibata Y, Ojima T, Yamagata Z, Matsuyama Y, Haro H (2017 Mar 1) Role of weekly teriparatide administration in osseous union enhancement within six months after posterior or transforaminal lumbar interbody fusion for osteoporosis-associated lumbar degenerative disorders: a multicenter, prospective randomized study. J Bone Joint Surg 99(5):365–372. https://doi.org/10.2106/JBJS.16.00230
Ding Q, Chen J, Fan J, Li Q, Yin G, Yu L (2017 Sep 1) Effect of zoledronic acid on lumbar spinal fusion in osteoporotic patients. Eur Spine J 26:2969–2977. https://doi.org/10.1007/s00586-017-5286-1
Body JJ, Gaich GA, Scheele WH, Kulkarni PM, Miller PD, Peretz A, Dore RK, Correa-Rotter R, Papaioannou A, Cumming DC, Hodsman AB (2002) A randomized double-blind trial to compare the efficacy of teriparatide [recombinant human parathyroid hormone (1-34)] with alendronate in postmenopausal women with osteoporosis. J Clin Endocrinol Metab 87(10):4528–4535
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, Wang O, Mellström D, Oefjord ES, Marcinowska-Suchowierska E, Salmi J, Mulder H, Halse J, Sawicki AZ, Mitlak BH (2001) Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344(19):1434–1441
Saag KG, Shane E, Boonen S, Marín F, Donley DW, Taylor KA, Dalsky GP, Marcus R (2007) Teriparatide or alendronate in glucocorticoid-induced osteoporosis. N Engl J Med 357(20):2028–2039
Abe Y, Takahata M, Ito M, Irie K, Abumi K, Minami A (2007) Enhancement of graft bone healing by intermittent administration of human parathyroid hormone (1-34) in a rat spinal arthrodesis model. Bone 41(5):775–785
Lehman RA Jr, Dmitriev AE, Cardoso MJ et al (2010) Effect of teriparatide [rhPTH(1,34)] and calcitonin on intertransverse process fusion in a rabbit model. Spine 35(2):146–152
Morimoto T, Kaito T, Kashii M et al (2014) Effect of intermittent administration of teriparatide (parathyroid hormone 1-34) on bone morphogenetic protein-induced bone formation in a rat model of spinal fusion. J Bone Joint Surg (Am Vol) 96(13):107
Sugiura T, Kashii M, Matsuo Y, Morimoto T, Honda H, Kaito T, Iwasaki M, Yoshikawa H (2015) Intermittent administration of teriparatide enhances graft bone healing and accelerates spinal fusion in rats with glucocorticoid-induced osteoporosis. Spine J 15(2):298–306
Yishake M, Yasen M, Jiang L, Liu W, Xing R, Chen Q, Lin H, Dong J (2017 Aug 10) Effects of combined teriparatide and zoledronic acid on posterior lumbar vertebral fusion in an aged ovariectomized rat model of osteopenia. J Orthop Res. https://doi.org/10.1002/jor.23682
Lee JH, Lee JH, Park JW et al (2012) The insertional torque of a pedicle screw has a positive correlation with bone mineral density in posterior lumbar pedicle screw fixation. J Bone Joint Surg Br Vol 94:93–97
Andrews EB, Gilsenan AW, Midkiff K, Sherrill B, Wu Y, Mann BH, Masica D (2012) The US postmarketing surveillance study of adult osteosarcoma and teriparatide: study design and findings from the first 7 years. J Bone Miner Res 27(12):2429–2437
Cho JH, Cho DC, Yu SH, Jeon YH, Sung JK, Kim KT (2012) Effect of dietary calcium on spinal bone fusion in an ovariectomized rat model. J Korean Neurosurg Soc 52(4):281–287
Metzger MF, Kanim LE, Zhao L et al (2015) The relationship between serum vitamin D levels and spinal fusion success: a quantitative analysis. Spine 40(8):E458–E468
Ravindra VM, Godzik J, Dailey AT, Schmidt MH, Bisson EF, Hood RS, Cutler A, Ray WZ (2015) Vitamin D levels and 1-year fusion outcomes in elective spine surgery: a prospective observational study. Spine 40(19):1536–1541
Liu Y, Fan Y, Cao D, Zhang J, Wu Z, Qiu G (2012) Calcitonin enhanced lumbar spinal fusion in a New Zealand rabbit model: a study with morphologic and molecular analysis. Spine 37(3):E139–E146
Liu CC, Tian FM, Zhou Z, Wang P, Gou Y, Zhang H, Wang WY, Shen Y, Zhang YZ, Zhang L (2015) Protective effect of calcitonin on lumbar fusion-induced adjacent-segment disc degeneration in ovariectomized rat. BMC Musculoskelet Disord 16:342
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Morris, M.T., Tarpada, S.P., Tabatabaie, V. et al. Medical optimization of lumbar fusion in the osteoporotic patient. Arch Osteoporos 13, 26 (2018). https://doi.org/10.1007/s11657-018-0427-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-018-0427-7