Abstract
Wound healing presents a complex physiological process that involves a sequence of events orchestrated by various cellular and molecular mechanisms. In recent years, there has been growing interest in leveraging nanomaterials and peptides to enhance wound healing outcomes. Nanocarriers offer unique properties such as high surface area-to-volume ratio, tunable physicochemical characteristics, and the ability to deliver therapeutic agents in a controlled manner. Similarly, peptides, with their diverse biological activities and low immunogenicity, hold great promise as therapeutics in wound healing applications. In this review, authors explore the potential of peptides as bioactive components in wound healing formulations, focusing on their antimicrobial, anti-inflammatory, and pro-regenerative properties. Despite the significant progress made in this field, several challenges remain, including the need for standardized characterization methods, optimization of biocompatibility and safety profiles, and translation from bench to bedside. Furthermore, developing multifunctional nanomaterial-peptide hybrid systems represents promising avenues for future research. Overall, the integration of nanomaterials made up of natural or synthetic polymers with peptide-based formulations holds tremendous therapeutic potential in advancing the field of wound healing and improving clinical outcomes for patients with acute and chronic wounds.
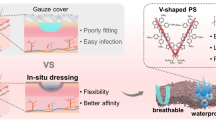
Graphical Abstract











Similar content being viewed by others
References
Kumar M, Mandal UK, Mahmood S. Dermatological formulations. 1st ed. 2024;613–42.
Honari G. Skin structure and function. Sensitive Ski Syndr. CRC Press; 2017. p. 16–22.
Xu R, Fang Y, Zhang Z, Cao Y, Yan Y, Gan L, et al. Recent advances in biodegradable and biocompatible synthetic polymers used in skin wound healing. Materials (Basel). 2023;16:5459.
Yousef H, Alhajj M, Sharma S. Anatomy, skin (integument), epidermis. 2017.
Norahan MH, Pedroza-González SC, Sánchez-Salazar MG, Álvarez MM, de Santiago GT. Structural and biological engineering of 3D hydrogels for wound healing. Bioact Mater. 2023;24:197–235.
Kumar M, Mandal UK. Asiaticoside: A Wonderful Herbal Component of Versatile Therapeutic benefits with Special Reference to Wound Healing Activity. J Clin Exp Dermatol Res. 2021;12:1–7.
Kumar M, Kumar D, Mahmood S, Singh V, Chopra S, Hilles AR, et al. Nanotechnology-driven wound healing potential of asiaticoside: a comprehensive review. RSC Pharm. 2024;1:9-36.
Rodrigues M, Kosaric N, Bonham CA, Gurtner GC. Wound healing: a cellular perspective. Physiol Rev. 2019;99:665–706.
Kumar M, Mahmood S, Mandal UK. An updated account on formulations and strategies for the treatment of burn infection-a review. Curr Pharm Des. 2022;28:1480–92.
Kumar M, Keshwania P, Chopra S, Mahmood S, Bhatia A. Correction: Therapeutic Potential of Nanocarrier-Mediated Delivery of Phytoconstituents for Wound Healing: Their Current Status and Future Perspective. AAPS PharmSciTech. 2023;24:206.
Percival S, Cutting K. Microbiology of wounds. CrC press; 2010.
Boateng J, Catanzano O. Advanced therapeutic dressings for effective wound healing—a review. J Pharm Sci. 2015;104:3653–80.
Rezvani Ghomi E, Khalili S, Nouri Khorasani S, Esmaeely Neisiany R, Ramakrishna S. Wound dressings: Current advances and future directions. J Appl Polym Sci. 2019;136:47738.
Andreu V, Mendoza G, Arruebo M, Irusta S. Smart dressings based on nanostructured fibers containing natural origin antimicrobial, anti-inflammatory, and regenerative compounds. Materials (Basel). 2015;8:5154–93.
Zahid AA, Chakraborty A, Shamiya Y, Ravi SP, Paul A. Leveraging the advancements in functional biomaterials and scaffold fabrication technologies for chronic wound healing applications. Mater Horizons. 2022;9:1850–65.
Saghazadeh S, Rinoldi C, Schot M, Kashaf SS, Sharifi F, Jalilian E, et al. Drug delivery systems and materials for wound healing applications. Adv Drug Deliv Rev. 2018;127:138–66.
Nandhini J, Karthikeyan E, Rajeshkumar S. Nanomaterials for wound healing: Current status and futuristic frontier. Biomed Technol. 2024;6:26–45.
Das S, Baker AB. Biomaterials and nanotherapeutics for enhancing skin wound healing. Front Bioeng Biotechnol. 2016;4:82.
Mangoni ML, McDermott AM, Zasloff M. Antimicrobial peptides and wound healing: biological and therapeutic considerations. Exp Dermatol. 2016;25:167–73.
Nasseri S, Sharifi M. Therapeutic potential of antimicrobial peptides for wound healing. Int J Pept Res Ther. 2022;28:38.
Chen CH, Lu TK. Development and challenges of antimicrobial peptides for therapeutic applications. Antibiotics. 2020;9:24.
Torchilin VP. Cell penetrating peptide-modified pharmaceutical nanocarriers for intracellular drug and gene delivery. Pept Sci. 2008;90:604–10.
Aramwit P. Introduction to biomaterials for wound healing. Wound Heal Biomater. Elsevier; 2016;2:3–38.
Naimer SA, Chemla F. Elastic adhesive dressing treatment of bleeding wounds in trauma victims. Am J Emerg Med. 2000;18:816–9.
Pereira RF, Bartolo PJ. Traditional therapies for skin wound healing. Adv wound care. 2016;5:208–29.
Sheridan RL, Morgan JR, Mohammad R. Biomaterials in burn and wound dressings. Polym Biomater Revis Expand. CRC Press; 2001. p. 465–72.
Xiang J, Shen L, Hong Y. Status and future scope of hydrogels in wound healing: Synthesis, materials and evaluation. Eur Polym J. 2020;130: 109609.
Moura LIF, Dias AMA, Carvalho E, de Sousa HC. Recent advances on the development of wound dressings for diabetic foot ulcer treatment—A review. Acta Biomater. 2013;9:7093–114.
Augustine R, Kalarikkal N, Thomas S. Advancement of wound care from grafts to bioengineered smart skin substitutes. Prog Biomater. 2014;3:103–13.
Josephson CD, Kuehnert MJ. Human tissue allografts: responsibilities in understanding the path from donor to recipient. Ross Princ Transfus Med. 2022;660–73.
Hermans MHE. Porcine xenografts vs. (cryopreserved) allografts in the management of partial thickness burns: is there a clinical difference? Burns. 2014;40:408–15.
Bahaj MS, Maki MAA, Rao KRSS, Kumar PV. Progressive exploration on the influence of natural polymers and emerging biomaterials in advanced wound care strategies. Indian J Biochem Biophys. 2024;61:127–44.
Moreira TD, Martins VB, da Silva Júnior AH, Sayer C, de Araújo PHH, Immich APS. New insights into biomaterials for wound dressings and care: Challenges and trends. Prog Org Coatings. 2024;187: 108118.
Liu Y, Ouyang Y, Yu L, Wang P, Peng Z, Liu H, et al. Novel approach for enhancing skin allograft survival by bioadhesive nanoparticles loaded with rapamycin. Int J Pharm. 2024;651: 123742.
Sommerfeld SD, Zhou X, Mejías JC, Oh BC, Maestas DR, Furtmüller GJ, et al. Biomaterials-based immunomodulation enhances survival of murine vascularized composite allografts. Biomater Sci. 2023;11:4022–31.
Irilouzadian R, Khalaji A, Baghsheikhi H, Sarmadian R, Hoveidamanesh S, Ghadimi T, et al. The clinical outcomes of xenografts in the treatment of burn patients: a systematic review and meta-analysis. Eur J Med Res. 2023;28:524.
Jang Y, Kim T, Kim D. Clinical and radiological outcomes between superior capsule reconstruction using allografts or xenografts: a 2-year retrospective comparison study. J Shoulder Elb Surg. 2023. https://doi.org/10.1016/j.jse.2023.10.032.
Yu R, Zhang H, Guo B. Conductive biomaterials as bioactive wound dressing for wound healing and skin tissue engineering. Nano-micro Lett. 2022;14:1–46.
Kumar M, Thakur A, Mandal UK, Thakur A, Bhatia A. Foam-Based Drug Delivery: A Newer Approach for Pharmaceutical Dosage Form. AAPS PharmSciTech. 2022;23:244.
Gomes I, Dale CS, Casten K, Geigner MA, Gozzo FC, Ferro ES, et al. Hemoglobin-derived peptides as novel type of bioactive signaling molecules. AAPS J. 2010;12:658–69.
Kim HS, Sun X, Lee J-H, Kim H-W, Fu X, Leong KW. Advanced drug delivery systems and artificial skin grafts for skin wound healing. Adv Drug Deliv Rev. 2019;146:209–39.
Zheng Y, Wu J, Zhu Y, Wu C. Inorganic-based biomaterials for rapid hemostasis and wound healing. Chem Sci. 2023;14:29–53.
Zhang X, Qin M, Xu M, Miao F, Merzougui C, Zhang X, et al. The fabrication of antibacterial hydrogels for wound healing. Eur Polym J. 2021;146: 110268.
Deng X, Gould M, Ali MA. A review of current advancements for wound healing: Biomaterial applications and medical devices. J Biomed Mater Res Part B Appl Biomater. 2022;110:2542–73.
Wang F, Hu S, Jia Q, Zhang L. Advances in electrospinning of natural biomaterials for wound dressing. J Nanomater. 2020;2020:1–20.
Chatterjee R, Maity M, Hasnain MS, Nayak AK. Chitosan: source, chemistry, and properties. Chitosan Drug Deliv. Elsevier; 2022. p. 1–22.
Baharlouei P, Rahman A. Chitin and chitosan: prospective biomedical applications in drug delivery, cancer treatment, and wound healing. Mar Drugs. 2022;20:460.
Soubhagya AS, Moorthi A, Prabaharan M. Preparation and characterization of chitosan/pectin/ZnO porous films for wound healing. Int J Biol Macromol. 2020;157:135–45.
Bombin ADJ, Dunne NJ, McCarthy HO. Electrospinning of natural polymers for the production of nanofibres for wound healing applications. Mater Sci Eng C. 2020;114: 110994.
Akakuru OU, Louis H, Amos PI, Akakuru OC, Nosike EI, Ogulewe EF. The chemistry of chitin and chitosan justifying their nanomedical utilities. Biochem Pharmacol (Los Angel). 2018;7:501–2167.
Garg Y, Kumar M, Sharma G, Katare OP, Chopra S, Bhatia A. Systematic designing and optimization of polymeric nanoparticles using central composite design: a novel approach for nose-to-brain delivery of donepezil hydrochloride. J Clust Sci. 2023;1–13. https://doi.org/10.1007/s10876-023-02528-2.
Yadav TC, Srivastava AK, Raghuwanshi N, Kumar N, Prasad R, Pruthi V. Wound healing potential of natural polymer: chitosan “A Wonder Molecule.” Integr Green Chem Sustain Eng. Hoboken: John Wiley Sons, Ltd.; 2019. p. 527–79.
Liu H, Wang C, Li C, Qin Y, Wang Z, Yang F, et al. A functional chitosan-based hydrogel as a wound dressing and drug delivery system in the treatment of wound healing. RSC Adv. 2018;8:7533–49.
Iacob AT, Lupascu FG, Apotrosoaei M, Vasincu IM, Tauser RG, Lupascu D, et al. Recent biomedical approaches for chitosan based materials as drug delivery nanocarriers. Pharmaceutics. 2021;13:587.
Ramya R, Venkatesan J, Kim SK, Sudha PN. Biomedical applications of chitosan: an overview. J Biomater Tissue Eng. 2012;2:100–11.
Abourehab MAS, Rajendran RR, Singh A, Pramanik S, Shrivastav P, Ansari MJ, et al. Alginate as a promising biopolymer in drug delivery and wound healing: A review of the state-of-the-art. Int J Mol Sci. 2022;23:9035.
Kumar M, Kumar D, Garg Y, Mahmood S, Chopra S, Bhatia A. Marine-derived polysaccharides and their therapeutic potential in wound healing application-A review. Int J Biol Macromol. 2023;253:127331.
Lin Z, Wu T, Wang W, Li B, Wang M, Chen L, et al. Biofunctions of antimicrobial peptide-conjugated alginate/hyaluronic acid/collagen wound dressings promote wound healing of a mixed-bacteria-infected wound. Int J Biol Macromol. 2019;140:330–42.
Hegde V, Uthappa UT, Altalhi T, Jung H-Y, Han SS, Kurkuri MD. Alginate based polymeric systems for drug delivery, antibacterial/microbial, and wound dressing applications. Mater Today Commun. 2022;33:104813.
Varaprasad K, Jayaramudu T, Kanikireddy V, Toro C, Sadiku ER. Alginate-based composite materials for wound dressing application: A mini review. Carbohydr Polym. 2020;236: 116025.
Saraiva MM, Campelo M da S, Camara Neto JF, Lima ABN, Silva G de A, Dias AT de FF, et al. Alginate/polyvinyl alcohol films for wound healing: Advantages and challenges. J Biomed Mater Res Part B Appl Biomater. 2023;111:220–33.
Jing X, Sun Y, Liu Y, Ma X, Hu H. Alginate/chitosan-based hydrogel loaded with gene vectors to deliver polydeoxyribonucleotide for effective wound healing. Biomater Sci. 2021;9:5533–41.
Barbu A, Neamtu B, Zăhan M, Iancu GM, Bacila C, Mireșan V. Current trends in advanced alginate-based wound dressings for chronic wounds. J Pers Med. 2021;11:890.
Mao G, Tian S, Shi Y, Yang J, Li H, Tang H, et al. Preparation and evaluation of a novel alginate-arginine-zinc ion hydrogel film for skin wound healing. Carbohydr Polym. 2023;311: 120757.
Feng X, Zhang X, Li S, Zheng Y, Shi X, Li F, et al. Preparation of aminated fish scale collagen and oxidized sodium alginate hybrid hydrogel for enhanced full-thickness wound healing. Int J Biol Macromol. 2020;164:626–37.
Naomi R, Bahari H, Ridzuan PM, Othman F. Natural-based biomaterial for skin wound healing (Gelatin vs. collagen): Expert review. Polymers (Basel). 2021;13:2319.
Ebhodaghe SO. A short review on chitosan and gelatin-based hydrogel composite polymers for wound healing. J Biomater Sci Polym Ed. 2022;33:1595–622.
Li T, Sun M, Wu S. State-of-the-art review of electrospun gelatin-based nanofiber dressings for wound healing applications. Nanomaterials. 2022;12:784.
Garcia-Orue I, Santos-Vizcaino E, Etxabide A, Uranga J, Bayat A, Guerrero P, et al. Development of bioinspired gelatin and gelatin/chitosan bilayer hydrofilms for wound healing. Pharmaceutics. 2019;11:314.
Kushibiki T, Mayumi Y, Nakayama E, Azuma R, Ojima K, Horiguchi A, et al. Photocrosslinked gelatin hydrogel improves wound healing and skin flap survival by the sustained release of basic fibroblast growth factor. Sci Rep. 2021;11:23094.
Stubbe B, Mignon A, Van Damme L, Claes K, Hoeksema H, Monstrey S, et al. Photo-crosslinked gelatin-based hydrogel films to support wound healing. Macromol Biosci. 2021;21:2100246.
Lu Y, Zhu X, Hu C, Li P, Zhao M, Lu J, et al. A fucoidan-gelatin wound dressing accelerates wound healing by enhancing antibacterial and anti-inflammatory activities. Int J Biol Macromol. 2022;223:36–48.
Taheri P, Jahanmardi R, Koosha M, Abdi S. Physical, mechanical and wound healing properties of chitosan/gelatin blend films containing tannic acid and/or bacterial nanocellulose. Int J Biol Macromol. 2020;154:421–32.
Kamoun EA, Chen X, Eldin MSM, Kenawy E-RS. Crosslinked poly (vinyl alcohol) hydrogels for wound dressing applications: A review of remarkably blended polymers. Arab J Chem. 2015;8:1–14.
Gajra B, Pandya SS, Vidyasagar G, Rabari H, Dedania RR, Rao S. Poly vinyl alcohol hydrogel and its pharmaceutical and biomedical applications: A review. Int J Pharm Res. 2012;4:2026.
Baghaie S, Khorasani MT, Zarrabi A, Moshtaghian J. Wound healing properties of PVA/starch/chitosan hydrogel membranes with nano Zinc oxide as antibacterial wound dressing material. J Biomater Sci Polym Ed. 2017;28:2220–41.
Alven S, Aderibigbe BA. Fabrication of Hybrid Nanofibers from Biopolymers and Poly (Vinyl Alcohol)/Poly (ε-Caprolactone) for Wound Dressing Applications. Polymers (Basel). 2021;13:2104.
Mir M, Ali MN, Barakullah A, Gulzar A, Arshad M, Fatima S, et al. Synthetic polymeric biomaterials for wound healing: a review. Prog Biomater. 2018;7:1–21.
Masud RA, Islam MS, Haque P, Khan MNI, Shahruzzaman M, Khan M, et al. Preparation of novel chitosan/poly (ethylene glycol)/ZnO bionanocomposite for wound healing application: effect of gentamicin loading. Materialia. 2020;12: 100785.
Farzaei MH, Derayat P, Pourmanouchehri Z, Kahrarian M, Samimi Z, Hajialyani M, et al. Characterization and evaluation of antibacterial and wound healing activity of naringenin-loaded polyethylene glycol/polycaprolactone electrospun nanofibers. J Drug Deliv Sci Technol. 2023;81: 104182.
Wang Z, Zhao Z, Khan NR, Hua Z, Huo J, Li Y. Microwave assisted chitosan-polyethylene glycol hydrogel membrane synthesis of curcumin for open incision wound healing. Die Pharm Int J Pharm Sci. 2020;75:118–23.
Minhas MU, Ahmad S, Khan KU, Sohail M, Abdullah O, Khalid I, et al. Synthesis and evaluation of polyethylene glycol-4000-co-poly (AMPS) based hydrogel membranes for controlled release of mupirocin for efficient wound healing. Curr Drug Deliv. 2022;19:1102–15.
Del Olmo JA, Alonso JM, Sáez-Martínez V, Benito-Cid S, Moreno-Benítez I, Bengoa-Larrauri M, et al. Self-healing, antibacterial and anti-inflammatory chitosan-PEG hydrogels for ulcerated skin wound healing and drug delivery. Biomater Adv. 2022;139: 212992.
Zhang H, Lin X, Cao X, Wang Y, Wang J, Zhao Y. Developing natural polymers for skin wound healing. Bioact Mater. 2024;33:355–76.
Zitzmann S, Ehemann V, Schwab M. Arginine-glycine-aspartic acid (RGD)-peptide binds to both tumor and tumor-endothelial cells in vivo. Cancer Res. 2002;62:5139–43.
Yin L, Li X, Wang R, Zeng Y, Zeng Z, Xie T. Recent Research Progress of RGD Peptide-Modified Nanodrug Delivery Systems in Tumor Therapy. Int J Pept Res Ther. 2023;29:53.
Mertz PM, Davis SC, Franzen L, Uchima F-D, Pickett MP, Pierschbacher MD, et al. Effects of an arginine-glycine-aspartic acid peptide-containing artificial matrix on epithelial migration in vitro and experimental second-degree burn wound healing in vivo. J Burn Care Rehabil. 1996;17:199–206.
Cui FZ, Tian WM, Hou SP, Xu QY, Lee I-S. Hyaluronic acid hydrogel immobilized with RGD peptides for brain tissue engineering. J Mater Sci Mater Med. 2006;17:1393–401.
Chen J, Li H, Chen J. Human epidermal growth factor coupled to different structural classes of cell penetrating peptides: A comparative study. Int J Biol Macromol. 2017;105:336–45.
Ying H, Zhou J, Wang M, Su D, Ma Q, Lv G, et al. In situ formed collagen-hyaluronic acid hydrogel as biomimetic dressing for promoting spontaneous wound healing. Mater Sci Eng C. 2019;101:487–98.
Hazrati R, Davaran S, Omidi Y. Bioactive functional scaffolds for stem cells delivery in wound healing and skin regeneration. React Funct Polym. 2022;174: 105233.
Pakyari M, Farrokhi A, Maharlooei MK, Ghahary A. Critical role of transforming growth factor beta in different phases of wound healing. Adv wound care. 2013;2:215–24.
Sharma S, Rai VK, Narang RK, Markandeywar TS. Collagen-based formulations for wound healing: A literature review. Life Sci. 2022;290: 120096.
Zhang S, Uludağ H. Nanoparticulate systems for growth factor delivery. Pharm Res. 2009;26:1561–80.
Del Gaudio P, De Cicco F, Aquino RP, Picerno P, Russo P, Dal Piaz F, et al. Evaluation of in situ injectable hydrogels as controlled release device for ANXA1 derived peptide in wound healing. Carbohydr Polym. 2015;115:629–35.
Chen F, Zhao Y, Wu H, Deng Z, Wang Q, Zhou W, et al. Enhancement of periodontal tissue regeneration by locally controlled delivery of insulin-like growth factor-I from dextran–co-gelatin microspheres. J Control release. 2006;114:209–22.
Lee K, Silva EA, Mooney DJ. Growth factor delivery-based tissue engineering: general approaches and a review of recent developments. J R Soc Interface. 2011;8:153–70.
John JV, McCarthy A, Wang H, Chen S, Su Y, Davis E, et al. Engineering biomimetic nanofiber microspheres with tailored size, predesigned structure, and desired composition via gas bubble–mediated coaxial electrospray. Small. 2020;16:1907393.
Haney EF, Hancock REW. Peptide design for antimicrobial and immunomodulatory applications. Pept Sci. 2013;100:572–83.
Wei Q, Duan J, Ma G, Zhang W, Wang Q, Hu Z. Enzymatic crosslinking to fabricate antioxidant peptide-based supramolecular hydrogel for improving cutaneous wound healing. J Mater Chem B. 2019;7:2220–5.
Tesauro D, Accardo A, Diaferia C, Milano V, Guillon J, Ronga L, et al. Peptide-based drug-delivery systems in biotechnological applications: recent advances and perspectives. Molecules. 2019;24:351.
Verma S, Goand UK, Husain A, Katekar RA, Garg R, Gayen JR. Challenges of peptide and protein drug delivery by oral route: Current strategies to improve the bioavailability. Drug Dev Res. 2021;82:927–44.
Lee Y-CJ, Javdan B, Cowan A, Smith K. More than skin deep: cyclic peptides as wound healing and cytoprotective compounds. Front Cell Dev Biol. 2023;11:1195600.
Wang X, Duan H, Li M, Xu W, Wei L. Characterization and mechanism of action of amphibian-derived wound-healing-promoting peptides. Front Cell Dev Biol. 2023;11:1219427.
Ebrahimi A, Farahpour MR, Amjadi S, Mohammadi M, Hamishehkar H. Nanoliposomal peptides derived from Spirulina platensis protein accelerate full-thickness wound healing. Int J Pharm. 2023;630: 122457.
John JV, Sharma NS, Tang G, Luo Z, Su Y, Weihs S, et al. Nanofiber aerogels with precision macrochannels and LL-37-mimic peptides synergistically promote diabetic wound healing. Adv Funct Mater. 2023;33:2206936.
Rai A, Ferrão R, Palma P, Patricio T, Parreira P, Anes E, et al. Antimicrobial peptide-based materials: Opportunities and challenges. J Mater Chem B. 2022;10:2384–429.
Peczuh MW, Hamilton AD. Peptide and protein recognition by designed molecules. Chem Rev. 2000;100:2479–94.
Yin S, Wang Y, Yang X. Amphibian-derived wound healing peptides: chemical molecular treasure trove for skin wound treatment. Front Pharmacol. 2023;14:1120228.
Pfalzgraff A, Brandenburg K, Weindl G. Antimicrobial peptides and their therapeutic potential for bacterial skin infections and wounds. Front Pharmacol. 2018;9:281.
Xu L, Xu S, Xiang T, Liu H, Chen L, Jiang B, et al. Multifunctional building elements for the construction of peptide drug conjugates. Eng Regen. 2022;3:92–109.
Sewald N, Jakubke H-D. Peptides: chemistry and biology. John Wiley & Sons; 2015.
Savale SK. Protein and peptide drug delivery system. World J Pharm Pharm Sci. 2016;5:1–19.
Mei F, Liu J, Wu J, Duan Z, Chen M, Meng K, et al. Collagen peptides isolated from salmo salar and tilapia nilotica skin accelerate wound healing by altering cutaneous microbiome colonization via upregulated NOD2 and BD14. J Agric Food Chem. 2020;68:1621–33.
Yang Q, Xie Z, Hu J, Liu Y. Hyaluronic acid nanofiber mats loaded with antimicrobial peptide towards wound dressing applications. Mater Sci Eng C. 2021;128: 112319.
Deng A, Yang Y, Du S, Yang X, Pang S, Wang X, et al. Preparation of a recombinant collagen-peptide (RHC)-conjugated chitosan thermosensitive hydrogel for wound healing. Mater Sci Eng C. 2021;119: 111555.
Chereddy KK, Her C-H, Comune M, Moia C, Lopes A, Porporato PE, et al. PLGA nanoparticles loaded with host defense peptide LL37 promote wound healing. J Control Release. 2014;194:138–47.
Sultana A, Luo H, Ramakrishna S. Antimicrobial peptides and their applications in biomedical sector. Antibiotics. 2021;10:1094.
Otvos L Jr, Ostorhazi E. Therapeutic utility of antibacterial peptides in wound healing. Expert Rev Anti Infect Ther. 2015;13:871–81.
Zhao C-C, Zhu L, Wu Z, Yang R, Xu N, Liang L. Resveratrol-loaded peptide-hydrogels inhibit scar formation in wound healing through suppressing inflammation. Regen Biomater. 2020;7:99–107.
Kaspar AA, Reichert JM. Future directions for peptide therapeutics development. Drug Discov Today. 2013;18:807–17.
Luong HX, Thanh TT, Tran TH. Antimicrobial peptides–Advances in development of therapeutic applications. Life Sci. 2020;260: 118407.
Zhang L, Tai Y, Liu X, Liu Y, Dong Y, Liu Y, et al. Natural polymeric and peptide-loaded composite wound dressings for scar prevention. Appl Mater Today. 2021;25: 101186.
d’Orlyé F, Trapiella-Alfonso L, Lescot C, Pinvidic M, Doan B-T, Varenne A. Synthesis, characterization and evaluation of peptide nanostructures for biomedical applications. Molecules. 2021;26:4587.
Deshayes S, Morris M, Heitz F, Divita G. Delivery of proteins and nucleic acids using a non-covalent peptide-based strategy. Adv Drug Deliv Rev. 2008;60:537–47.
Berillo D, Yeskendir A, Zharkinbekov Z, Raziyeva K, Saparov A. Peptide-based drug delivery systems. Medicina (B Aires). 2021;57:1209.
Bolatchiev A, Baturin V, Bazikov I, Maltsev A, Kunitsina E. Effect of antimicrobial peptides HNP-1 and hBD-1 on Staphylococcus aureus strains in vitro and in vivo. Fundam Clin Pharmacol. 2020;34:102–8.
Shi R, Li H, Jin X, Huang X, Ou Z, Zhang X, et al. Promoting Re-epithelialization in an oxidative diabetic wound microenvironment using self-assembly of a ROS-responsive polymer and P311 peptide micelles. Acta Biomater. 2022;152:425–39.
Lin Y, Zhang Y, Cai X, He H, Yang C, Ban J, et al. Design and self-assembly of peptide-copolymer conjugates into nanoparticle hydrogel for wound healing in diabetes. Int J Nanomedicine. 2024;574:2487–506.
Nayab S, Aslam MA, Rahman S ur, Sindhu Z ud D, Sajid S, Zafar N, et al. A review of antimicrobial peptides: its function, mode of action and therapeutic potential. Int J Pept Res Ther. 2022;28:46.
Guidotti G, Brambilla L, Rossi D. Cell-penetrating peptides: from basic research to clinics. Trends Pharmacol Sci. 2017;38:406–24.
El-Andaloussi S, Holm T, Langel U. Cell-penetrating peptides: mechanisms and applications. Curr Pharm Des. 2005;11:3597–611.
Desale K, Kuche K, Jain S. Cell-penetrating peptides (CPPs): An overview of applications for improving the potential of nanotherapeutics. Biomater Sci. 2021;9:1153–88.
Hällbrink M, Kilk K, Elmquist A, Lundberg P, Lindgren M, Jiang Y, et al. Prediction of cell-penetrating peptides. Int J Pept Res Ther. 2005;11:249–59.
Pescina S, Ostacolo C, Gomez-Monterrey IM, Sala M, Bertamino A, Sonvico F, et al. Cell penetrating peptides in ocular drug delivery: State of the art. J Control Release. 2018;284:84–102.
Fonseca SB, Pereira MP, Kelley SO. Recent advances in the use of cell-penetrating peptides for medical and biological applications. Adv Drug Deliv Rev. 2009;61:953–64.
Kim GC, Cheon DH, Lee Y. Challenge to overcome current limitations of cell-penetrating peptides. Biochim Biophys Acta (BBA)-Proteins Proteomics. 2021;1869:140604.
Zhao Z, Ukidve A, Kim J, Mitragotri S. Targeting strategies for tissue-specific drug delivery. Cell. 2020;181:151–67.
Van NT, Lee K-H, Huang Y, Shin MC, Park YS, Kim H, et al. Topical Delivery of Cell-penetrating peptide-modified human growth hormone for enhanced wound healing. Pharmaceuticals. 2023;16:394.
Gori A, Lodigiani G, Colombarolli SG, Bergamaschi G, Vitali A. Cell Penetrating Peptides: Classification, Mechanisms, Methods of Study, and Applications. ChemMedChem. 2023;18: e202300236.
Sajid MI, Moazzam M, Stueber R, Park SE, Cho Y, Tiwari RK. Applications of amphipathic and cationic cyclic cell-penetrating peptides: Significant therapeutic delivery tool. Peptides. 2021;141: 170542.
Zhang R, Qin X, Kong F, Chen P, Pan G. Improving cellular uptake of therapeutic entities through interaction with components of cell membrane. Drug Deliv. 2019;26:328–42.
Xu J, Khan AR, Fu M, Wang R, Ji J, Zhai G. Cell-penetrating peptide: a means of breaking through the physiological barriers of different tissues and organs. J Control Release. 2019;309:106–24.
Ruczynski J, Wierzbicki PM, Kogut-Wierzbicka M, Mucha P, Siedlecka-Kroplewska K, Rekowski P. Cell-penetrating peptides as a promising tool for delivery of various molecules into the cells. Folia Histochem Cytobiol. 2014;52:257–69.
Langel Ü. CPP, cell-penetrating peptides. Springer; 2019.
Epand RM, Shai Y, Segrest JP, Anantharamiah GM. Mechanisms for the modulation of membrane bilayer properties by amphipathic helical peptides. Biopolym Orig Res Biomol. 1995;37:319–38.
Kalafatovic D, Giralt E. Cell-penetrating peptides: Design strategies beyond primary structure and amphipathicity. Molecules. 2017;22:1929.
Milletti F. Cell-penetrating peptides: classes, origin, and current landscape. Drug Discov Today. 2012;17:850–60.
Cruz J, Ortiz C, Guzman F, Fernández-Lafuente R, Torres R. Antimicrobial peptides: promising compounds against pathogenic microorganisms. Curr Med Chem. 2014;21:2299–321.
Bahar AA, Ren D. Antimicrobial peptides Pharmaceuticals. 2013;6:1543–75.
Pasupuleti M, Schmidtchen A, Malmsten M. Antimicrobial peptides: key components of the innate immune system. Crit Rev Biotechnol. 2012;32:143–71.
Moravej H, Moravej Z, Yazdanparast M, Heiat M, Mirhosseini A, Moosazadeh Moghaddam M, et al. Antimicrobial peptides: features, action, and their resistance mechanisms in bacteria. Microb Drug Resist. 2018;24:747–67.
Seyfi R, Kahaki FA, Ebrahimi T, Montazersaheb S, Eyvazi S, Babaeipour V, et al. Antimicrobial peptides (AMPs): roles, functions and mechanism of action. Int J Pept Res Ther. 2020;26:1451–63.
Yu SM, Li Y, Kim D. Collagen mimetic peptides: progress towards functional applications. Soft Matter. 2011;7:7927–38.
Malcor J-D, Mallein-Gerin F. Biomaterial functionalization with triple-helical peptides for tissue engineering. Acta Biomater. 2022;148:1–21.
Xu Y, Kirchner M. Collagen mimetic peptides. Bioengineering. 2021;8:5.
Chan TR, Stahl PJ, Li Y, Yu SM. Collagen–gelatin mixtures as wound model, and substrates for VEGF-mimetic peptide binding and endothelial cell activation. Acta Biomater. 2015;15:164–72.
Hao Z, Li H, Wang Y, Hu Y, Chen T, Zhang S, et al. Supramolecular peptide nanofiber hydrogels for bone tissue engineering: from multihierarchical fabrications to comprehensive applications. Adv Sci. 2022;9:2103820.
de Torre IG, García-Arévalo C, Alonso M, Cabello JCR. Stimuli-responsive protein fibers for advanced applications. Smart Polym their Appl. Elsevier; 2019. p. 323–77.
de Castro Brás LE, Frangogiannis NG. Extracellular matrix-derived peptides in tissue remodeling and fibrosis. Matrix Biol. 2020;91:176–87.
Rowley AT, Nagalla RR, Wang S, Liu WF. Extracellular matrix-based strategies for immunomodulatory biomaterials engineering. Adv Healthc Mater. 2019;8:1801578.
Song J, Zhang Q, Li G, Zhang Y. Constructing ECM-like Structure on the Plasma Membrane via Peptide Assembly to Regulate the Cellular Response. Langmuir. 2022;38:8733–47.
Fang H, Chen W, Gao Y, Shen Y, Luo M. Molecular mechanisms associated with Angiotensin-converting enzyme-inhibitory peptide activity on vascular extracellular matrix remodeling. Cardiology. 2014;127:247–55.
Cardoso F, Lewis R, Vetter I, Inserra M, King G. Does nature do ion channel drug discovery better than us? RSC Drug Discov Ser. 2014;2015:297–319.
Gelain F, Luo Z, Zhang S. Self-assembling peptide EAK16 and RADA16 nanofiber scaffold hydrogel. Chem Rev. 2020;120:13434–60.
Park SI, An GM, Kim MG, Heo SH, Shin MS. Enhancement of skin permeation of anti-wrinkle peptide GHKs using cell penetrating peptides. Korean Chem Eng Res. 2020;58:29–35.
Pickart L, Vasquez-Soltero JM, Margolina A. The effect of the human peptide GHK on gene expression relevant to nervous system function and cognitive decline. Brain Sci. 2017;7:20.
Schussler O, Falcoz PE, Chachques JC, Alifano M, Lecarpentier Y. Possible treatment of myocardial infarct based on tissue engineering using a cellularized solid collagen scaffold functionalized with Arg-Glyc-Asp (RGD) peptide. Int J Mol Sci. 2021;22:12563.
König N. Structure and exchange kinetics of nanocrystalline micelles, telechelic hydrogels and self-assembling antimicrobial peptides. 2020.
Xu D, Chen W, Tobin-Miyaji YJ, Sturge CR, Yang S, Elmore B, et al. Fabrication and microscopic and spectroscopic characterization of cytocompatible self-assembling antimicrobial nanofibers. ACS Infect Dis. 2018;4:1327–35.
Sant’Ana EMC. Estudo do efeito da Alternagina-C, uma desintegrina do veneno de Bothrops alternatus e de um peptídeo sintético derivado de sua estrutura, sobre a expressão de fatores de crescimento, angiogênese e cicatrização de lesão em pele de rato. 2008.
Torchilin VP. Tat peptide-mediated intracellular delivery of pharmaceutical nanocarriers. Adv Drug Deliv Rev. 2008;60:548–58.
Kumar VB, Tiwari OS, Finkelstein-Zuta G, Rencus-Lazar S, Gazit E. Design of functional RGD peptide-based biomaterials for tissue engineering. Pharmaceutics. 2023;15:345.
Guan T, Li J, Chen C, Liu Y. Self-assembling peptide-based hydrogels for wound tissue repair. Adv Sci. 2022;9:2104165.
Vaz ER, Fujimura PT, Araujo GR, da Silva CAT, Silva RL, Cunha TM, et al. A short peptide that mimics the binding domain of TGF-β1 presents potent anti-inflammatory activity. PLoS ONE. 2015;10: e0136116.
Kiveliö A-SJ. Tissue engineering for prenatal applications. EPFL; 2015.
Puthia M, Butrym M, Petrlova J, Strömdahl A-C, Andersson MÅ, Kjellström S, et al. A dual-action peptide-containing hydrogel targets wound infection and inflammation. Sci Transl Med. 2020;12:eaax6601.
Petruk G, Petrlova J, Samsudin F, Del GR, Bond PJ, Schmidtchen A. Concentration-and pH-dependent oligomerization of the thrombin-derived C-terminal peptide TCP-25. Biomolecules. 2020;10:1572.
Yang S, Wang C, Zhu J, Lu C, Li H, Chen F, et al. Self-assembling peptide hydrogels functionalized with LN-and BDNF-mimicking epitopes synergistically enhance peripheral nerve regeneration. Theranostics. 2020;10:8227.
Tałałaj U, Uścinowicz P, Bruzgo I, Surażyński A, Zaręba I, Markowska A. The effects of a novel series of KTTKS analogues on cytotoxicity and proteolytic activity. Molecules. 2019;24:3698.
Lee JY, Cho KH, Kim JW, Nam SD, Kim HY, Shin JS, et al. Synthesis and biological screening of small molecule peptides based on the amino acid sequence of thymosin β4. J Korean Soc Appl Biol Chem. 2015;58:651–8.
Memdouh S, Gavrilović I, Ng K, Cowan D, Abbate V. Advances in the detection of growth hormone releasing hormone synthetic analogs. Drug Test Anal. 2021;13:1871–87.
Pawar K, Kolli CS, Rangari VK, Babu RJ. Transdermal iontophoretic delivery of lysine-proline-valine (KPV) peptide across microporated human skin. J Pharm Sci. 2017;106:1814–20.
Medina-Cruz D, Saleh B, Vernet-Crua A, Ajo A, Roy AK, Webster TJ. Drug-delivery nanocarriers for skin wound-healing applications. Wound Heal Tissue Repair, Regen Diabetes. Elsevier; 2020. p. 439–88.
Farasati Far B, Naimi-Jamal MR, Sedaghat M, Hoseini A, Mohammadi N, Bodaghi M. Combinational system of lipid-based nanocarriers and biodegradable polymers for wound healing: an updated review. J Funct Biomater. 2023;14:115.
Kumar M, Mahmood S, Chopra S, Bhatia A. Biopolymer based nanoparticles and their therapeutic potential in wound healing–a review. int J Biol Macromol. 2024;267:131335.
Krishnaswami V, Raju NS, Alagarsamy S, Kandasamy R. Novel Nanocarriers for the Treatment of Wound Healing. Curr Pharm Des. 2020;26:4591–600.
Kumar M, Hilles AR, Almurisi SHA, Bhatia A, Mahmood S. Micro and nano-carriers-based pulmonary drug delivery system: their current updates, challenges, and limitations–A review. JCIS Open. 2023;12:100095.
Yu N, Wang X, Qiu L, Cai T, Jiang C, Sun Y, et al. Bacteria-triggered hyaluronan/AgNPs/gentamicin nanocarrier for synergistic bacteria disinfection and wound healing application. Chem Eng J. 2020;380: 122582.
Kumar M, Kumar D, Chopra S, Mahmood S, Bhatia A. Microbubbles: Revolutionizing Biomedical Applications with Tailored Therapeutic Precision. Curr Pharm Des. 2023;29:3532–45.
Kumar M, Dogra R, Mandal UK. Nanomaterial-based delivery of vaccine through nasal route: opportunities, challenges, advantages, and limitations. J Drug Deliv Sci Technol. 2022;74:103533.
Kumar M, Kumar D, Kumar S, Kumar A, Mandal UK. A Recent Review on Bio-availability Enhancement of Poorly Water-soluble Drugs by using Bioenhancer and Nanoparticulate Drug Delivery System. Curr Pharm Des. 2022;28:3212–24.
Majumdar M, Shivalkar S, Pal A, Verma ML, Sahoo AK, Roy DN. Nanotechnology for enhanced bioactivity of bioactive compounds. Biotechnol Prod Bioact Compd. Elsevier; 2020. p. 433–66.
Zhang Z, Tsai P, Ramezanli T, Michniak-Kohn BB. Polymeric nanoparticles-based topical delivery systems for the treatment of dermatological diseases. Wiley Interdiscip Rev Nanomedicine Nanobiotechnology. 2013;5:205–18.
Chatterjee S, Ghosal K, Kumar M, Mahmood S, Thomas S. A detailed discussion on interpenetrating polymer network (IPN) based drug delivery system for the advancement of health care system. J Drug Deliv Sci Technol. 2022;79:104095.
Puri A, Loomis K, Smith B, Lee J-H, Yavlovich A, Heldman E, et al. Lipid-based nanoparticles as pharmaceutical drug carriers: from concepts to clinic. Crit Rev Ther Drug Carr Syst. 2009;26:523–80.
Lombardo D, Kiselev MA, Caccamo MT. Smart nanoparticles for drug delivery application: development of versatile nanocarrier platforms in biotechnology and nanomedicine. J Nanomater. 2019;2019. https://doi.org/10.1155/2019/3702518.
Chauhan N, Kumar M, Chaurasia S, Garg Y, Chopra S, Bhatia A. A comprehensive review on drug therapies and nanomaterials used in orthodontic treatment. Curr Pharm Des. 2023;29:154–3165.
Matei A-M, Caruntu C, Tampa M, Georgescu SR, Matei C, Constantin MM, et al. Applications of nanosized-lipid-based drug delivery systems in wound care. Appl Sci. 2021;11:4915.
Kumar M, Mandal UK, Mahmood S. Novel drug delivery system. Adv Mod Approaches Drug Deliv [Internet]. 2023 [cited 2023 Aug 8];1–32. Available from: https://linkinghub.elsevier.com/retrieve/pii/B9780323916684000125.
Çağdaş M, Sezer AD, Bucak S. Liposomes as potential drug carrier systems for drug delivery. Appl Nanotechnol drug Deliv. 2014;1:1–50.
Wang W, Lu K, Yu C, Huang Q, Du Y-Z. Nano-drug delivery systems in wound treatment and skin regeneration. J Nanobiotechnology. 2019;17:1–15.
Kumar M, Dogra R, Mandal UK. Novel Formulation Approaches Used for the Management of Osteoarthritis: A Recent Review. Curr Drug Deliv. 2023;20:841–56.
Ahmed KS, Hussein SA, Ali AH, Korma SA, Lipeng Q, Jinghua C. Liposome: Composition, characterisation, preparation, and recent innovation in clinical applications. J Drug Target. 2019;27:742–61.
Koppa Raghu P, Bansal KK, Thakor P, Bhavana V, Madan J, Rosenholm JM, et al. Evolution of nanotechnology in delivering drugs to eyes, skin and wounds via topical route. Pharmaceuticals. 2020;13:167.
Gera S, Kankuri E, Kogermann K. Antimicrobial peptides–unleashing their therapeutic potential using nanotechnology. Pharmacol Ther. 2022;232: 107990.
Tuncer Degim I, Celebi N. Controlled delivery of peptides and proteins. Curr Pharm Des. 2007;13:99–117.
Cheng R, Liu L, Xiang Y, Lu Y, Deng L, Zhang H, et al. Advanced liposome-loaded scaffolds for therapeutic and tissue engineering applications. Biomaterials. 2020;232: 119706.
Dawoud MHS, Yassin GE, Ghorab DM, Morsi NM. Insulin mucoadhesive liposomal gel for wound healing: a formulation with sustained release and extended stability using quality by design approach. AAPS PharmSciTech. 2019;20:1–15.
Berry-Kilgour C, Cabral J, Wise L. Advancements in the delivery of growth factors and cytokines for the treatment of cutaneous wound indications. Adv wound care. 2021;10:596–622.
Abdelfattah S, Nasr M, Ali A, Geneidi A. Vesicular systems used for wound healing. Arch Pharm Sci Ain Shams Univ. 2021;5:184–203.
Mishra DK, Shandilya R, Mishra PK. Lipid based nanocarriers: a translational perspective. Nanomedicine Nanotechnology, Biol Med. 2018;14:2023–50.
Allaw M, Pleguezuelos-Villa M, Manca ML, Caddeo C, Aroffu M, Nacher A, et al. Innovative strategies to treat skin wounds with mangiferin: Fabrication of transfersomes modified with glycols and mucin. Nanomedicine. 2020;15:1671–85.
Ag Seleci D. Design and application of niosomal drug delivery systems. 2017.
Feng C, Lu G, Li Y, Huang X. Self-assembly of amphiphilic homopolymers bearing ferrocene and carboxyl functionalities: effect of polymer concentration, β-cyclodextrin, and length of alkyl linker. Langmuir. 2013;29:10922–31.
Marianecci C, Di Marzio L, Rinaldi F, Celia C, Paolino D, Alhaique F, et al. Niosomes from 80s to present: the state of the art. Adv Colloid Interface Sci. 2014;205:187–206.
Chen S, Hanning S, Falconer J, Locke M, Wen J. Recent advances in non-ionic surfactant vesicles (niosomes): Fabrication, characterization, pharmaceutical and cosmetic applications. Eur J Pharm Biopharm. 2019;144:18–39.
Barani M, Sangiovanni E, Angarano M, Rajizadeh MA, Mehrabani M, Piazza S, et al. Phytosomes as innovative delivery systems for phytochemicals: A comprehensive review of literature. Int J Nanomedicine. 2021;16:6983.
Chen S. Dermal delivery of Centella asiatica using hyaluronic acid niosomal system for wound healing. ResearchSpace@ Auckland; 2022.
Uchegbu IF, Florence AT. Non-ionic surfactant vesicles (niosomes): physical and pharmaceutical chemistry. Adv Colloid Interface Sci. 1995;58:1–55.
Kashapov R, Gaynanova G, Gabdrakhmanov D, Kuznetsov D, Pavlov R, Petrov K, et al. Self-assembly of amphiphilic compounds as a versatile tool for construction of nanoscale drug carriers. Int J Mol Sci. 2020;21:6961.
Witika BA, Bassey KE, Demana PH, Siwe-Noundou X, Poka MS. Current advances in specialised niosomal drug delivery: Manufacture, characterization and drug delivery applications. Int J Mol Sci. 2022;23:9668.
Elmowafy M. Skin penetration/permeation success determinants of nanocarriers: Pursuit of a perfect formulation. Colloids Surfaces B Biointerfaces. 2021;203: 111748.
Prabha J, Kumar M, Kumar D, Chopra S, Bhatia A. Nano-platform strategies of herbal components for the management of rheumatoid arthritis: a review on the battle for next-generation formulations. Curr Drug Deliv. 2023.
Godin B, Touitou E. Ethosomes: new prospects in transdermal delivery. Crit Rev Ther drug Carr Syst. 2003;20:63–102.
Mbah CC, Builders PF, Attama AA. Nanovesicular carriers as alternative drug delivery systems: ethosomes in focus. Expert Opin Drug Deliv. 2014;11:45–59.
Verma P, Pathak K. Therapeutic and cosmeceutical potential of ethosomes: An overview. J Adv Pharm Technol Res. 2010;1:274.
Singh D, Pradhan M, Nag M, Singh MR. Vesicular system: Versatile carrier for transdermal delivery of bioactives. Artif cells, nanomedicine, Biotechnol. 2015;43:282–90.
Kandregula B, Narisepalli S, Chitkara D, Mittal A. Exploration of lipid-based nanocarriers as drug delivery systems in diabetic foot ulcer. Mol Pharm. 2022;19:1977–98.
Dahri M, Beheshtizadeh N, Seyedpour N, Nakhostin-Ansari A, Aghajani F, Seyedpour S, et al. Biomaterial-based delivery platforms for transdermal immunotherapy. Biomed Pharmacother. 2023;165: 115048.
Tapeinos C, Battaglini M, Ciofani G. Advances in the design of solid lipid nanoparticles and nanostructured lipid carriers for targeting brain diseases. J Control Release. 2017;264:306–32.
Ramezanpour S, Tavatoni P, Akrami M, Navaei-Nigjeh M, Shiri P. Potential wound healing of PLGA nanoparticles containing a novel L-Carnitine–GHK peptide conjugate. J Nanomater. 2022;2022. https://doi.org/10.1155/2022/6165759.
Yeboah A, Cohen RI, Faulknor R, Schloss R, Yarmush ML, Berthiaume F. The development and characterization of SDF1α-elastin-like-peptide nanoparticles for wound healing. J Control release. 2016;232:238–47.
Papaioannou A, Liakopoulou A, Papoulis D, Gianni E, Gkolfi P, Zygouri E, et al. Effect of Peptides on the Synthesis, Properties and Wound Healing Capacity of Silver Nanoparticles. Pharmaceutics. 2023;15:2471.
Sun L, Li A, Hu Y, Li Y, Shang L, Zhang L. Self-assembled fluorescent and antibacterial GHK-Cu nanoparticles for wound healing applications. Part Part Syst Charact. 2019;36:1800420.
Wu L, Chen Y, Zeng G, Mao N, Li N, Li L, et al. Supramolecular peptide hydrogel doped with nanoparticles for local siRNA delivery and diabetic wound healing. Chem Eng J. 2023;457: 141244.
Teng R, Yang Y, Zhang Z, Yang K, Sun M, Li C, et al. In situ enzyme‐induced self‐assembly of antimicrobial‐antioxidative peptides to promote wound healing. Adv Funct Mater. 2023;33:2214454.
Arab WT, Niyas AM, Seferji K, Susapto HH, Hauser CAE. Evaluation of peptide nanogels for accelerated wound healing in normal micropigs. Front Nanosci Nanotech. 2018;4:1–9.
Li X, Fan R, Tong A, Yang M, Deng J, Zhou L, et al. In situ gel-forming AP-57 peptide delivery system for cutaneous wound healing. Int J Pharm. 2015;495:560–71.
Qin P, Meng Y, Yang Y, Gou X, Liu N, Yin S, et al. Mesoporous polydopamine nanoparticles carrying peptide RL-QN15 show potential for skin wound therapy. J Nanobiotechnology. 2021;19:1–18.
Nanditha CK, Kumar GSV. Bioactive peptides laden nano and micro-sized particles enriched ECM inspired dressing for skin regeneration in diabetic wounds. Mater Today Bio. 2022;14: 100235.
Santhini E, Parthasarathy R, Shalini M, Dhivya S, Mary LA, Padma VV. Bio inspired growth factor loaded self assembling peptide nano hydrogel for chronic wound healing. Int J Biol Macromol. 2022;197:77–87.
Li Y, Xu T, Tu Z, Dai W, Xue Y, Tang C, et al. Bioactive antibacterial silica-based nanocomposites hydrogel scaffolds with high angiogenesis for promoting diabetic wound healing and skin repair. Theranostics. 2020;10:4929.
Fu C, Qi Z, Zhao C, Kong W, Li H, Guo W, et al. Enhanced wound repair ability of arginine-chitosan nanocomposite membrane through the antimicrobial peptides-loaded polydopamine-modified graphene oxide. J Biol Eng. 2021;15:17.
Sun T, Zhan B, Zhang W, Qin D, Xia G, Zhang H, et al. Carboxymethyl chitosan nanoparticles loaded with bioactive peptide OH-CATH30 benefit nonscar wound healing. Int J Nanomedicine. 2018;13:5771–86.
Sun H, Wang Y, He T, He D, Hu Y, Fu Z, et al. Hollow polydopamine nanoparticles loading with peptide RL-QN15: a new pro-regenerative therapeutic agent for skin wounds. J Nanobiotechnology. 2021;19:1–20.
Mueller LK, Baumruck AC, Zhdanova H, Tietze AA. Challenges and perspectives in chemical synthesis of highly hydrophobic peptides. Front Bioeng Biotechnol. 2020;8:162.
Isidro-Llobet A, Kenworthy MN, Mukherjee S, Kopach ME, Wegner K, Gallou F, et al. Sustainability challenges in peptide synthesis and purification: from R&D to production. J Org Chem. 2019;84:4615–28.
Svenson J, Stensen W, Brandsdal B-O, Haug BE, Monrad J, Svendsen JS. Antimicrobial peptides with stability toward tryptic degradation. Biochemistry. 2008;47:3777–88.
Palm C, Jayamanne M, Kjellander M, Hällbrink M. Peptide degradation is a critical determinant for cell-penetrating peptide uptake. Biochim Biophys Acta (BBA)-Biomembranes. 2007;1768:1769–76.
Moncla BJ, Pryke K, Rohan LC, Graebing PW. Degradation of naturally occurring and engineered antimicrobial peptides by proteases. Adv Biosci Biotechnol. 2011;2:404.
Starr CG, Wimley WC. Antimicrobial peptides are degraded by the cytosolic proteases of human erythrocytes. Biochim Biophys Acta (BBA)-Biomembranes. 2017;1859:2319–26.
Zhang X, Li X, Zhao Y, Zheng Q, Wu Q, Yu Y. Nanocarrier system: An emerging strategy for bioactive peptide delivery. Front Nutr. 2022;9:1050647.
Zhang T, Luo X, Xu K, Zhong W. Peptide-containing nanoformulations: Skin barrier penetration and activity contribution. Adv Drug Deliv Rev. 2023;203:115139.
Dunshee LC, Sullivan MO, Kiick KL. Therapeutic nanocarriers comprising extracellular matrix-inspired peptides and polysaccharides. Expert Opin Drug Deliv. 2021;18:1723–40.
Hwang J, Kiick KL, Sullivan MO. Collagen-mimetic peptides for delivery of therapeutics in chronic wounds healing application. 2022.
Yadav SC, Kumari A, Yadav R. Development of peptide and protein nanotherapeutics by nanoencapsulation and nanobioconjugation. Peptides. 2011;32:173–87.
Han H, Li S, Xu M, Zhong Y, Fan W, Xu J, et al. Polymer-and lipid-based nanocarriers for ocular drug delivery: Current status and future perspectives. Adv Drug Deliv Rev. 2023;196: 114770.
Kanaujia KA, Mishra N, Rajinikanth PS, Saraf SA. Antimicrobial peptides as antimicrobials for wound care management: a comprehensive review. J Drug Deliv Sci Technol. 2024;95:105570.
Mu R, Zhu D, Abdulmalik S, Wijekoon S, Wei G, Kumbar SG. Stimuli-responsive peptide assemblies: Design, self-assembly, modulation, and biomedical applications. Bioact Mater. 2024;35:181–207.
Deptuła M, Zawrzykraj M, Sawicka J, Banach-Kopeć A, Tylingo R, Pikuła M. Application of 3D-printed hydrogels in wound healing and regenerative medicine. Biomed Pharmacother. 2023;167: 115416.
Qin M, Guo Y, Su F, Huang X, Qian Q, Zhou Y, et al. High-strength, fatigue-resistant, and fast self-healing antibacterial nanocomposite hydrogels for wound healing. Chem Eng J. 2023;455: 140854.
Yi X, He J, Wei X, Li H, Liu X, Cheng F. A polyphenol and ε-polylysine functionalized bacterial cellulose/PVA multifunctional hydrogel for wound healing. Int J Biol Macromol. 2023;247: 125663.
Chen X, Zhang M, Chen S, Wang X, Tian Z, Chen Y, et al. Peptide-modified chitosan hydrogels accelerate skin wound healing by promoting fibroblast proliferation, migration, and secretion. Cell Transplant. 2017;26:1331–40.
Zhu J, Han H, Li F, Wang X, Yu J, Qin X, et al. Peptide-functionalized amino acid-derived pseudoprotein-based hydrogel with hemorrhage control and antibacterial activity for wound healing. Chem Mater. 2019;31:4436–50.
Xu T, Tian Y, Zhang R, Yu B, Cong H, Shen Y. Hydrogel vectors based on peptide and peptide-like substances: For treating bacterial infections and promoting wound healing. Appl Mater Today. 2021;25: 101224.
Acknowledgements
The authors would like to thank the Maharaja Ranjit Singh Punjab Technical University (MRSPTU), Bathinda, India, for providing the research facilities. The authors also thank the Indian Council of Medical Research, New Delhi, India.
Funding
Research grant (5/8–4/5/Env/2020-NCD-II Dated 22/12/2021) Under Indian Council of Medical Research (ICMR), New Delhi, India.
Author information
Authors and Affiliations
Contributions
Dikshant and Mohit Kumar: Writing-Original draft preparation, collecting information, methodology, Devesh Kumar and Yogesh Garg: Conceptualization, collecting information, revising draft, Amit Bhatia and Shruti Chopra: Revising draft, finalizing the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The author declares no conflict of interest, financial or otherwise.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kumar, M., Kumar, D., Kumar, D. et al. Therapeutic Potential of Nanocarrier Mediated Delivery of Peptides for Wound Healing: Current Status, Challenges and Future Prospective. AAPS PharmSciTech 25, 108 (2024). https://doi.org/10.1208/s12249-024-02827-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-024-02827-5