Abstract
The microneedles have attracted great interests for a wide range of transdermal biomedical applications, such as biosensing and drug delivery, due to the advantages of being painless, semi-invasive, and sustainable. The ongoing challenges are the materials and fabrication methods of the microneedles in order to obtain a specific shape, configuration and function of the microneedles to achieve a target biomedical application. Here, this review would introduce the types of materials of the microneedles firstly. The hardness, Young's modulus, geometric structure, processability, biocompatibility and degradability of the microneedles are explored as well. Then, the fabrication methods for the solid and hollow microneedles in recent years are reviewed in detail, and the advantages and disadvantages of each process are analyzed and compared. Finally, the biomedical applications of the microneedles are reviewed, including biosensing, drug delivery, body fluid extraction, and nerve stimulation. It is expected that this work provides the fundamental knowledge for developing new microneedle devices, as well as the applications in a variety of biomedical fields.
Similar content being viewed by others
1 Introduction
Microneedles have attracted increasing interest in recent years in biomedical areas, such as drug delivery, biosensing, and fluid extraction (Chen et al. 2017). The tips of the microneedles can penetrate the epidermis layer of skin to arrive at the top layer of the dermis that is above the blood capillaries. Thus, the microneedles would not touch the nerve endings to further avoid bleeding and pain (Arai et al. 2015). The microchannels can be formed on the skin by the microneedles where the molecules can pass through, or the microneedles can bring the devices, such as the electrodes to get the biomedical signals (Kalluri and Banga 2009). For drug administration, the microneedle approach has the advantages of avoiding the effect of the gastrointestinal digestion, accelerating the drug absorption, prolonging the effective time, and patient self-administered without needing doctors (Prausnitz and Langer 2008). For biosensing, the microneedle approach provides possible continuous monitoring of the biomarkers in interstitial fluid (Liu et al. 2004).
A microneedle usually has a microscale height and width, in the shape of a cone or a pyramid, and usually, a patch of microneedle arrays sticks to the skin. The concept of transdermal delivery by using microneedles was first proposed by Zhao et al. in 2020, but due to the limitations of micromachining technology, it was not until the 1990s that microneedles were mass produced. The earliest use of hollow needles was by Mcallister et al., 150 μm micron needles made of silicon in the 1980s (Chen et al. 2017).
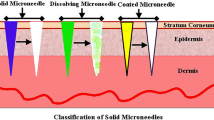
Several types of microneedles have been fabricated, including solid microneedles, coated microneedles, soluble microneedles, and hollow microneedles. The microneedle materials can be silicon (Park et al. 2005), metals, biomaterials, and polymers (Lee et al. 2016a; van der Maaden et al. 2012). A variety of fabrication methods have been explored, including photolithography with selective etching, machining with chemical etching, machining with micro-milling, laser cutter, 3d printing, soft lithography, micro-injection molding, hot embossing, electrohydrodynamic atomization, laser machining, electric-discharge machining with laser machining, soft lithography, drawing lithography, centrifugal lithography, and droplet-borne air blowing (Jung and Jin 2021).
This review would focus particularly on the recent progress of the materials, fabrication methods, and biomedical applications of microneedles. The study would introduce the types of materials for constructing the microneedles, their fabrication, and related biomedical applications in drug delivery, biosensing, and body fluid extraction. Most of the published reviews on microneedles mainly reviewed the application of microneedles in drug delivery (Ita 2015; Yang et al. 2019, 2021). In recent years, the potential of microneedles in the field of biosensors has attracted great attention because of its painless and slightly invasive, such as the sensor based on microneedles for biomarkers of human tissue fluid. This paper also summarizes other applications on body fluid extraction and nerves. In addition, due to the high precision of the structure of the microneedle, there are great difficulties in the preparation of the microneedle. At present, other reviews lacked discussion about the fabrication methods of the microneedle (Yang et al. 2019; Ma and Wu 2017). This study summarized almost all the existing processing technologies of the microneedle that can serve as the fundamentals for future study of the microneedle devices.
2 Materials for microneedles
FDA has strict regulatory requirements for the safety and effectiveness of medical devices and products. When selecting microneedle materials, it is necessary to ensure that their biocompatibility, safety, and stability meet the clinical requirements of the FDA. Therefore, the following describes the microneedle materials that meet FDA requirements.
2.1 Inorganic non-metallic materials
2.1.1 Silicon
Silicon and silicon-based materials have a excellent mechanical strength and chemical and thermal stability. The processing technologies of the silicon and silicon-based materials have been very mature, such as laser technology, etching technology, and laser cutting (Jung and Jin 2021) (Howells et al. 2022). These technologies have expanded the preparation of complex silicon structures for medical device applications, such as joint implants, the infusion tube materials, the microfluidic systems, and the contact lenses (Khanna et al. 2011; Abla et al. 2013). The silicon and silicon-based materials are also widely used in the microneedle drug delivery systems, which are mainly prepared by a combination of isotropic and anisotropic corrosion processes (Vinayakumar et al. 2014; Khanna et al. 2010).
However, when being punctured into the skin, the fractures easily occur on the silicon microneedle, and the fragmented needle stays in the body and the biocompatibility of silicon is poor, which leads to the adverse reactions such as inflammation in the human body. Therefore, improving the mechanical strength of silicon is one of the research directions of the silicon microneedles (Yan et al. 2011). Narayanan et al. coated a layer of gold on the silicon material by metal sputtering to improve the mechanical strength and biocompatibility of the microneedle array. The calculated mechanical strength is 37.27 GPa, which is higher than the skin's resistance (Narayanan and Raghavan 2019).
Another way to improve the hardness of silicon is to optimize its etching process. S. Raghavan et al. optimized the etching factor of tetramethylammonium hydroxide to make slender silicon tapered microneedles, and the microhardness of the manufactured Si microneedles was 44.4 (HRC), which was 52.2 times the ultimate tensile strength of the skin. This would make the microneedles safer through the skin and easier to be inserted without breaking. In addition, optimizing the structure and size of silicon microneedles is also a very important way to improve their hardness. The general length of silicon microneedles is 150~1700 μm and the needle pitch is 260~2000 μm (Pradeep Narayanan and Raghavan 2017).
In addition to silicon, inorganic materials that can be used for microneedles include glass, glassy carbon (Mishra et al. 2018a), and ceramics (Bystrova and Luttge 2011; Hartmann et al. 2015; Verhoeven et al. 2012; Gholami et al. 2019), as shown in Fig. 1.
2.1.2 Ceramics
The biocompatible ceramics have higher mechanical strength and high temperature and moisture stability than most polymers. At the same time, the surface of the ceramics can also interact with biomolecules electrostatically to enhance molecular penetration. The preparation of ceramic microneedles generally uses dual-replicated PDMS production molds and ceramic micro-molding technology, while ceramic micro-molding technology includes uniform filling of the mold and drying steps, during which the solvent evaporates and forms a raw tape, resulting in microstructure defects.
Bystrova et al. produced alumina ceramic microneedle arrays through micro-forming and ceramic sintering. In order to degas to prevent the formation of raw tape, they inserted a PDMS mold filled with slurry into a petri dish and sealed it with paraffin film, and then placed it under ultrasound for 30 min. The prepared ceramic microneedles were tested at the micro-indentation station and there was no damage (Bystrova and Luttge 2011). Since alumina is sintered at a higher temperature, it has thermal instability, the hybridization of ceramics and polymers can introduce strong covalent bonds, and the cross-linking of organic and inorganic components forms a three-dimensional network, thereby improving the chemical and thermal stability. Currently commonly used microneedle ceramic materials mainly include alumina and zirconia.
2.2 Metal
The metal materials have several advantages for being constructed as the structural materials for the microneedles, such as the excellent mechanical and physical properties, being not easy to break, low cost, and excellent biocompatibility.
The metal microneedles can be used for the hollow microneedles, coated microneedles, solid-state microneedles, etc. The metal microneedles include stainless steel (Cahill et al. 2018), titanium (Skoog et al. 2015), aluminum, and Ni (Chen et al. 2019). However, the disadvantages of the metal microneedles are non-degradable and inflexible.
2.2.1 Stainless steel
Stainless steel is a kind of special steel material with an excellent biocompatibility, mechanical property, and corrosion resistance. It is the most commonly used surgical implant material, especially AISI316L and AISI317L ultra-low carbon stainless steel. Therefore, stainless steel become the most widely used material in the metal microneedles. Stainless steel microneedles can be prepared by excimer and infrared laser Processing, femtosecond laser processing, electric-discharge machining and electro-hydraulic atomization. Cahill et al. used an electrolytic polishing process to produce the stainless steel microneedles that maintain a mechanical integrity and have a high specific surface area and associated porosity. These can greatly improve the drug-loading capacity of the stainless steel microneedles (Cahill et al. 2018). Ullah et al. covered the surface of the stainless steel microneedles with a porous polymer to increase its drug delivery rate. For lidocaine drug delivery, the drug release of porous coating MNs was 25 times that of uncoated MNs (Ullah et al. 2018).
2.2.2 Titanium
Titanium, as a silver-white transition metal is widely used for medical applications. It has many excellent properties, such as lightweight, high strength, stable chemical properties, excellent temperature resistance, strong resistances to acid and alkaline, and low density. Li, JY introduced a titanium porous microneedle array prepared by an improved metal injection molding (MIM) technology, which guarantees the biocompatibility of microneedles and can easily penetrate human forearm skin without fractures (Li et al. 2017). Khandan et al. used a titanium deep reactive ion etching technology to prepare the Ti microneedles with the complex through holes and applied them to the ocular drug delivery devices (Khandan et al. 2016).
2.2.3 Aluminum
Aluminum, as a silver-white light metal, is the most economical and applicable medical material with the outstanding features such as ductility, lightweight, and corrosion resistance. Chen et al. proposed a combination of micromachining, electrolyte polishing, and anodizing methods to prepare an aluminum microneedle array with the nanochannels on the surface, which had hundreds of times the specific surface area of a traditional template. By incorporating a dense network of needle-like nanotube thin film channels, which cover a large surface area, the drug-carrying capacity of aluminum microneedles can be increased while simultaneously improving their mechanical properties (Chen et al. 2013). Le Thanh et al. prepared a microneedle of aluminum sample processed by computer numerical control. The process was characterized by low cost and scalability for a mass production (Hoa Le et al. 2015).
2.3 Polymers
Due to the polymer's easy formability, short processing cycle, low cost, rich material variety, it is easy to achieve a large-scale production, and the needle has a good toughness. At the same time, the polymer material can be biocompatible and biodegradable, and the polymer material molding process has become important research in the field of medical microneedle preparation. Table 1 summarizes the typical polymers for constructing the microneedles.
2.3.1 Polycarbonate (PC)
PC is a high molecular polymer containing carbonate groups in the molecular chain. It is a tough thermoplastic resin, resistant to weak acids and alkalis, with high strength and elasticity, excellent electrical properties, dimensional stability, and fatigue resistance. Due to the thermodynamic properties of polycarbonate (PC), the PC microneedles can be prepared with a hot embossing. McConville et al. used the palladium nanopowders in PC adhesive to prepare microneedles with a high mechanical strength (McConville and Davis 2016). Nair et al. used a plasma technology and a micro-injection molding to prepare the surface-modified PC microneedles, which improved the surface energy and roughness of the PC materials (Nair et al. 2015).
2.3.2 Polyvinylpyrrolidone (PVP)
PVP is a thermoplastic resin made by polymerization of ethylene. It has the advantages of non-toxicity, resistance to most acids and alkalis, and a high electrical insulation. Liu's work was to prepare soluble PVP microneedles loaded with insulin by a two-step centrifugation and molding process. Compared with pure PVP microneedles, CaCO3 doped PVP microneedles show a high mechanical strength (Liu et al. 2018). In addition, its mechanical stability can also be enhanced by changing its geometry.
2.3.3 Polylactide (PLA)
PLA, a polymer obtained by polymerization of lactic acid, is made from starch raw materials proposed (e.g. corn). It has a good thermal stability, biocompatibility, good degradability, good gloss and transparency, and the best tensile strength and ductility.
Kim, MJ, et al. obtained the sharp PLA microneedles by an oxygen plasma etching, and the mechanical tests showed that the microneedles with an obelisk-shape were mechanically stronger than those with a pyramid-shape (Kim et al. 2018).
2.3.4 Acrylate
Acrylic polymers have a series of common characteristics, such as transparency, low toxicity, easy preparation, wide adhesion, water resistance, and durability. Therefore, the acrylic resin can be widely used for medical applications. Acrylate microneedles can be prepared by melt extrusion and mold methods. Gittard et al. used the microneedles made from acrylate-based polymer e-shell 200 and tested their geometry to study the microneedle mechanical failure mode and the mechanism of penetrating pigskin (Gittard et al. 2013). It is verified that the increase in aspect ratio and the decrease in tip diameter are related to the lower failure force.
2.3.5 Hydrogels
Hydrogels have good mechanical properties and material permeabilities. When the hydrogel is in a dry state, it is very hard to have a sufficient mechanical strength to penetrate the skin. After it penetrates into the skin, it would quickly absorbs a small amount of tissue fluid, then the swelling becomes soft, and the internal network structure opens, becoming a channel for the material transportation. At the same time, small molecule substances would circulate and diffuse freely under the action of an osmotic pressure between tissue fluid and the hydrogel. Therefore, the inflatable microneedles are mostly made of the crosslinked hydrogel. Hydrogels microneedles can be prepared by soft lithography. Kim et al. used the X-linked HA nanoparticles to prepare the microneedles. The addition of hydrogel enables the microneedles to have the continuous drug delivery capabilities and can be used in various applications that require the sustained release of drugs for several days (Kim et al. 2020b). Bok et al. studied to enhance the permeability of hydrogels and drugs by a ultrasonic sound pressure and an AC iontophoresis with the hyaluronic acid microneedles (Bok et al. 2020).
2.3.6 Polyvinylalcohol (PVA)
PVA has excellent thermal degradation characteristics and can be used as the main material for constructing the dissolving microneedles (Yun et al. 2020). PVA microneedles can be prepared by means of 3D printing (Uddin et al. 2020). Rongyan et al. developed a PVA microneedle patch for the point-of-care testing (He et al. 2020). First, interstitial fluid was extracted from the high pore microstructure of the hydrogel, and then the PVA was heated and dissolved in the water bath. The target biomarker was recovered from the microneedle patch quickly and effectively, and the concentration of the target in the solution was detected.
2.3.7 Polycaprolactone (PCL)
PCL has been widely used in the fields of drug carrier, plasticizer, degradable plastics, nanofiber spinning, and forming and processing materials because of its good biocompatibility, good organic homopolymer compatibility, and good biodegradability. PCL microneedles can be prepared by melt extrusion, mold method, laser cutting method, 3D printing method, etc.
PCL has excellent thermal ablation changes and a low melting point. In the soluble microneedles, it can be used as a material that is triggered by light and heat to release the model drugs (Andersen et al. 2018; Zhang et al. 2019). Zhang et al. used lauric acid and PCL as arrows, polyethylene and PCL as a support base, and Cu7S4 nanoparticles as light-to-heat conversion factors. After inserting the microneedles into the skin, the support base was dissolved and the detachable microneedle arrow were embedded in the skin. Then, under near-infrared light, PCL was triggered by photothermal to ablate and release the loaded metformin drug (Zhang et al. 2018).
2.3.8 Carboxymethylcellulose (CMC)
It is a carboxymethylated derivative of cellulose, usually an anionic polymer compound prepared by reacting natural cellulose with caustic alkali and monochloroacetic acid. It is non-toxic, hygroscopic, and easy-to-disperse in water. CMC can improve the mechanical strength of dissolving microneedles with the excellent biodegradability and biocompatibility (Kamal et al. 2020). The CMC microneedles can be prepared by mold method. Jeong et al. designed a soluble microneedle composed of CMC and trehalose, in which CMC provides a mechanical strength, and trehalose increases the dissolution rate of the microneedle. Human growth hormone is administered in the form of embedding microneedle with a good tolerance (Lee et al. 2011). Prepared CMC with gelatin copolymer hydrogel microneedles by Nayak et al., and combined with ultrasound for delivery of lidocaine. Microneedles application increased permeability up to 17 fold at 0.5 h, averaging up to fourfold. The time required to reach therapeutic levels of lidocaine was reduced to less than 7 min (Nayak et al. 2014).
2.3.9 Cellulose acetate phthalate (CAP)
CAP, as a modified natural porous polymer, can be acquired by esterifying the hydroxyl groups in the cellulose acetate molecule with acetic acid. CAP is selective, water permeable, and simple-to-process. It is non-toxic, harmless, and non-allergic to a skin contact for a long time. However, it is easy to deteriorate in the alkaline solutions and strong oxidants. CAP is pH sensitive and can be used for the electrochemical control of the drug release based on a pH sensitivity. It can swell or dissolve when the local pH changes caused by an appropriate reduction potential (Seddiqi et al. 2021). Anderson et al. used nano-particle carbon as a conductive material, and CAP as a polymer binder, and prepared conductive microneedles by mold method. When electricity was applied to the microneedle, a hydrogen evolution reaction occurs, causing the local pH on the electrode to increase. The increase of pH would cause the swelling of the CAP polymer that constitutes the needle structure, thereby achieving the effect of controlling the drug release (Anderson et al. 2019).
3 Fabrication methods of solid microneedles
The structure includes cones, quadrangular pyramids, and triangular pyramid (Das et al. 2019). The main microneedle preparation processes include the conventional micromachine, the microelectronic integrated manufacturing technology (MEMS), and the 3D printing technology. In the manufacturing process, the shape, length and width of the needle tip need to be optimized for an easy insertion into the skin. Therefore, according to the characteristics of the preparation material and the requirements of the application, the preparation process need to be selected and improved accordingly.
3.1 Fabrication without mould
3.1.1 Lithography/machining with selective etching
Photolithography with etching
A combination of photolithography, metal deposition, and selective etching was used for the fabrication of the microneedles. The manufacturing process is by using photolithography to obtain a microsized pattern, followed by the deposition of metals, such as chromium as a mask material layer (Henry et al. 1998). A dry etching and/or wet etching process is used to etch the patterned wafer, which can vertically etch the unmasked silicon portion and a slight lateral under-etched masked portion to obtain a series of sharp silicon spikes, as shown in Fig. 2a (Held et al. 2010).
Silicon solid microneedles are prepared by the selective etching method. a A schematic diagram of isotropic etching using the type I and type II process and the profiles as a function of the process parameters. b A schematic diagram of the combination of isotropic and anisotropic etching using the type II process (Held et al. 2010). c A lithography process sketch (not to scale) for manufacturing micro needles (MNS) by method 1 and method 2 (Dardano et al. 2015)
X-ray lithography with etching
In the manufacture of the semiconductor devices, the light source used for photolithography has been reduced from visible time ultraviolet (UV) lamps to soft X-rays. Short-wavelength X-rays have been successfully used and need to leak deeper microneedle gully structures. Generally, there is a close relationship between the X-ray dose energy and the microneedle exposure depth, as well as between dose energy and size transition.
The positive and negative photoresists for X-ray lithography are generally PMMA and SU-8 respectively. UV-LIGA exposure photoresist is often used to obtain the needle structure of the microneedle, but it is easy to overreach during the preparation and etching of the bevel of the needle tip, resulting in the collapse of the needle tip structure. Bai et al. adjusted the X ray exposure direction and performed two exposures. In the second exposure, there was a certain deviation from the vertical direction and finally formed a three-dimensional microneedle structure with a single beveled side wall. And using the mobile photolithography process, a complete three-dimensional PMMA pyramid structure with multiple inclined surfaces is prepared, which is more conducive to piercing the skin and reducing pain. However, due to the expensive X-ray equipment, this process is difficult to popularize (Bai et al. 2012).
Machining with chemical etching
Machining with chemical etching has been studied as well. For example, the micropillars were fabricated on stainless steel or silicon wafers using a cutting machine, and a chemical etching or an electrochemical etching was used for adjusting the shape of the microneedles, as illustrated in Fig. 3a (Lee et al. 2016b; Yan et al. 2018).
Fabrication sequences of 3D steel microneedle array by machining. a a machining with chemical etching and FE-SEM image of the 3D micro-needle array with Au/Pt black on stainless steel (Lee et al. 2016b). b a micro-milling method for CAM strategy for the needle geometry (left) and experimental setup (right) (Garcia-Lopez et al. 2018). c a laser ablation for fabricating the microneedles on metal surfaces that uses distorted light to rotate (Omatsu et al. 2010)
3.1.2 Laser engraving
Laser ablation, as a top-down process for material processing, has been widely used in micro drilling and cutting applications. The 3D microneedle structure with a certain height and pitch can be fabricated by laser processing directly, and its height can be adjusted as needed by adjusting the power and scanning speed of the laser. The laser process can manufacture the microneedles array in a variety of materials, including metals, PDMS, and PMMA.
However, the melting point of PDMS is low, a laser processing would cause the burning and resolidification problems, and the depth is not uniform. Tu et al. used CO2 direct writing laser to process the microneedle mold structure in PMMA and fabricated the PLGA microneedles ranging from 700 μm to 1100 μm through the secondary casting PDMS process, but the disadvantage was that the surface of the prepared PMMA microneedles was relatively rough. Omatsu et al. used a circularly polarized optical vortex process to prepare the metal solid microneedles. As the laser-induced plasma rotated along the light intensity curve, a smoother microneedle surface was produced during the ablation process. They used this method to prepare a metal microneedle array with a uniform height and needle shape (Omatsu et al. 2010), as shown in Fig. 3c. Aydin Sadeq introduced a method for manufacturing hollow and solid chitosan microneedles a commercial CO2 laser cutting machine (Sadeqi et al. 2018).
3.1.3 Micro-milling
Micro-milling was another method for manufacturing microneedles. A stainless-steel needle array with a conical geometry was manufactured by a ball-end micro-end milling cutter, as shown in Fig. 3b. However, this method would wear or even break the tool, and the production time is too long, making it economically unsuitable, and it is difficult to convert multi-step batch processing to high-throughput manufacturing scalability (Garcia-Lopez et al. 2018).
3.1.4 3D printing
3D printing is a rapid approach for constructing microneedles. Without machining or any molds, the microneedle structure can be directly generated from computer graphics data, which shortens the product development cycle significantly, reduces the material waste, improves the productivity, and reduces the production costs. In Fig. 4a, the 3D printing for the microneedles is generally divided into several steps. First, a software, such as SolidWorks, is used to design the microneedle structure based on a few parameters. Then, from the perspective of stress, pressure and force, a simulation analysis is used to design and determine the appropriate parameters and materials processed by a 3D printer (Saroia et al. 2020). Generally, three types of 3D printing have been studied, including stereolithography (SLA), fused deposition modeling (FDM), and digital light processing (DLP). The accuracy of FDM printing technology is affected by several factors, such as temperature and the size of the release nozzle, and the minimum feature size for these two methods can be 100 µm. The DLP system has a high printing accuracy and can meet the manufacturing accuracy of the microneedle. In Fig. 4b, Kevinkrieger et al. developed a low-cost, simple, and customizable method for manufacturing microneedle molds through the common, commercial, and reasonably priced SLA 3D printers, which can print the needles with a good NIB definition, and can quickly produce microneedle molds with easy to customize needle parameters (Krieger et al. 2019).
Stereolithography
A 3D printer with SLA has been studied for constructing the microneedles. The process is to irradiate selected materials with ultraviolet rays, and use polyvinyl alcohol to cure each layer. Because SLA is a nozzle-less process, there will be no material clogging and high resolution. The printing speed is slow. The quality of the final product depends on the laser intensity, laser exposure and curing time, scanning speed, and printing resolution. However, the photoinitiator required for the SLA printing process is toxic, the machine is more expensive, and less biocompatible materials can be printed. The materials can be acrylonitrile-butadiene styrene (ABS), polyester resin, PLA, PVA, and biocompatible resin. The microneedles have been used in several healthcare applications, such as the treatment of cancer, human squamous cell carcinoma Zenoraft tumors, and inhibition and elimination (Uddin et al. 2020). Economidou used SLA technology to prepare an MN array of pyramids and spears, and applied a thin layer of insulin sugar to the surface of MNs uniformly and accurately by inkjet printing, successfully achieving rapid hypoglycemia in mice. Compared with metal MN, 3D printed polymer MN requires less force to penetrate pig skin (Economidou et al. 2019).
Fused deposition modeling
FDM is another method for the construction of microneedles. The method has a low cost, a rapid prototyping, and a simple process. Two nozzles can be used to print different materials at the same time. The disadvantage is that the extrusion process of filler particles is difficult to uniformly disperse. The disadvantage is poor resolution. The materials generally are thermoplastic materials, such as PLA and ABS. To solve the problem of low resolution, Luzuriaga et al. first used FDM to print the degradable PLA solid microneedles, and then etched the microneedles in KOH solution, reducing the thickness and width to 200-300 μm, and the tip size was Between 1-55 μm, it improves the feature size resolution of FDM printed materials and has considerable mechanical strength (Luzuriaga et al. 2018).
Digital light processing
The method with DLP is that after the image signal is digitally processed, the light is projected and the photosensitive resin is molded. It can project and aggregate a whole layer during printing, and the printing speed is fast, which is especially obvious when compared with SLA technology. The resolution is high, and the molding accuracy can reach up to 25 microns. Several types of materials have been studied, such as resin, nylon, ABS, and PLA. Han et al. used DLP technology to create a biologically heuristic microneedle with the backward curved barbs. Since the curing light intensity attenuated as the light propagates through the precursor solution, a cross-link density gradient was formed, and triangular barbs were formed after curing. The barb thickness was 100 µm, and the maximum bending curvature was 0.0033 µm−1. The tissue adhesion of barbed microneedle was 18 times that of non-barbed microneedle, and the tissue adhesion of biologically inspired microneedle had been improved (Han et al. 2020). Wei Yao et al. proposed the hydrogel MNs based on DLP 3D printing, studied the mechanical properties of MNs in detail at different exposure times, and performed artificial skin microneedle puncture simulation, MNs injection, and extraction drug simulation experiments, and it shows that the microneedles prepared by DLP have good mechanical properties (Yao et al. 2019).
3.2 Fabrication with with mould
3.2.1 Soft Lithography
Soft lithography is a widely used method for a pattern transfer. The transfer procedure is normally by pouring polymeric materials onto a mold, and after hardening and demolding, the microneedles in the desired material are obtained. The original structures of microneedles or cavities were fabricated by conventional machining, microfabrication, or 3D printing. The original mold can be microneedles or their negative patter, the cavities. For the microneedle structure-based mold, a two-step transfer was used, the microneedles are transferred into the cavities, and the cavities were further used to transfer to obtain the microneedles in the desired material. For the cavity-structure-based mold, the microneedles are obtained directly with a one-step transfer. The materials of the obtained microneedles can be PMMA, SU-8, Si, and PDMS.
3.2.2 Micro-injection molding
Similarly, micro-injection molding and hot embossing are used for the pattern transfer to obtain the microneedles in the desired material. For the micro-injection, the solution was injected into the cavities of the mold with a micro-injector by a compression process (Sammoura et al. 2007; O'Mahony et al. 2019; Mirza et al. (2017)). The injection speed, melt temperature and secondary clamping pressure have a significant effect on the quality of microneedles during the injection process (Zhuang et al. 2018).
3.2.3 Hot Embossing
For hot embossing, the process is to heat the material to the molding temperature, control the displacement and strength for embossing isothermal forming, and then keep the force constant to cool, and finally, the pattern is demolded, as shown the Fig. 5c (Worgull et al. 2008). The embossing temperature, pressure and time affected the quality of the microneedles, as illustrated in Fig. 5a (Abubaker and Zhang 2019), and the coupling of the gradient thermal field and the pressure field is the key to the process, as indicated in Fig. 5b (Li et al. 2019a).
a A hot embossing machine and video measurement system (Abubaker and Zhang 2019). b The schematic (left) of the modified hot embossing setup for the GMPA microneedle fabrication and its photo (right) (Li et al. 2019a). c Three-dimensional structure diagram of microneedle mould using micro injection compression molding and optical image of the polymer microneedle array (Chen et al. 2020)
4 Fabrication methods for hollow microneedles
In contrast to solid microneedles, hollow microneedles can provide continuous administration for drug delivery. However, the manufacturing process and cost of hollow microneedles are often complex and high. Several methods have been studied for the fabrication of hollow microneedles.
4.1 Preparation of hollow microneedles without mould
4.1.1 Lithography with etching
X-ray lithography
The LIGA technology is an important method for preparing hollow microneedle arrays. Among them, deep reactive ion etching and other techniques are used for hollow microneedle formation (Iliescu et al. 2018). However, LIGA technology requires expensive synchrotron light sources and special masks, which cannot be prepared on a large scale. Microneedle molds can be prepared based on LIGA, and then microneedle arrays can be prepared in batches by combining injection molding and stamping molding processes. In LIGA technology, the improvement of exposure technology can get the ideal microneedle structure.
Mobile X-ray lithography
The mobile lithography technology is to install a phase shifter on each hole on each mask. As a result of light interference, the interference light intensity between adjacent holes cancels each other out, so that the light intensity distribution of the pattern boundary is clear, thus The hole pattern can be distinguished and the resolution of photolithography can be improved. Wu et. al used alignment exposure technology, and obtains a similar pattern of pattern on the LIGA mask by mobile X-ray lithography, and then uses alignment exposure technology to achieve the microneedle array hole processing. Then the exposure energy distribution map of microneedles on a PMMA lithographic plate and prepared a microneedle for blood extraction (Wu et al. 2018).
Double deep X-ray exposure
The first reticle is used for the first lithography. After the lithography is completed, perform etching, transfer the pattern on the photoresist to the hard mask below, and then spin-coat the photoresist to use the second mask to complete the second photolithography. This lithography can increase the high aspect ratio. The first exposure produces a single PMMA part with a sawtooth, and the second exposure removes the substrate and creates a hollow channel in Fig. 6a. The work of Perennes was to produce PMMA through dual deep x-ray lithography, then combining with the imprint technology, to prepared PMMA microneedle (Perennes et al. 2006).
X-ray processing of microneedles. a Fabrication of a microneedle array with the successive inclined deep x-ray exposure process (Perennes et al. 2006). b Fabrication of a microneedle array with a high aspect ratio by vertical deep X-ray exposure and the successive inclined deep x-ray exposure process (Moon and Lee 2005)
Tilting X-ray lithography
The silicon wafer has a slight tilt relative to the exposure lens and the reticle so that the entire thickness of the anti-reagent has been exposed to multiple different focal planes, which can achieve the effect of significantly enhancing the depth of exposure. Inclined exposure is based on double-deep X-ray exposure, continuously tilting deep x-rays during the second exposure to shape the column array into a hollow microneedle array as shown in the Fig. 6b.
UV and X-ray lithography
The biggest difference between UV-LIGA and LIGA is that it uses a common mask to expose on a universal UV exposure machine, while LIGA requires an expensive synchrotron light source and a special mask. SU-8 photoresist is a negative photoresist, and UV photolithography is a commonly used photolithography method in recent years. The combination of the two can form a high aspect ratio structure. Liao et al. used ultraviolet light instead of X-rays to obtain a similar exposure energy distribution as LIGA and prepared a good quality microneedle array with a drug-loading capacity (Liao et al. 2012). Jiaming Chen et al. introduced reshaping photoresist technology to form a hollow channel arc structure by baking sacrificial photoresist before depositing a gold seed layer. The gold layer serves as a conductive layer having good biocompatibility. Three-dimensional arrays of hollow and solid microneedles were prepared using laser micromachining technology. Lithography can prepare multiple composite structures at the same time (Chen et al. 2019).
4.1.2 Laser Processing
Excimer and infrared Laser Processing: Excimer (UV) and infrared (IR) laser processing techniques can be used to prepare metal electrodeposition molds, and they can also be used to cut solid needles directly from Titanium to produce hollow microneedles (Chen et al. 2015). Liao et al. developed a new two-photon polymerizationdirect laser writing method, which is a non-linear optical process based on two-photon absorption theory. By programming the laser focus to move in three-dimensional space, the reliable hollow three-dimensional microstructures are fabricated with nanometer resolution, including microneedles for drug delivery, and are not limited by subtractive processing or etching processes, as illustrated in Fig. 7a and b (Liao et al. 2019; Rad et al. 2017).
Femtosecond laser processing
Vinayakumar, KB and others used a new technology of femtosecond laser micromachining to prepare hollow stainless steel microneedle arrays. First, EDM was used to create a circular hole and a circular step on both sides of the stainless steel plate. The aperture and taper of a hollow microneedle array can be controlled by varying the diameter of the laser spot (Vinayakumar et al. 2016b).
Laser writing
The combination of the SU-8 material and the laser writing technology has also become an important way to prepare hollow microneedles. The laser beam from a laser writer system incident on the resist surface provides an energy for cross-linking, which can change the structure of SU-8 to prepare the microneedles (Mishra et al. 2018b). Mishra's work used a coherent laser beam to fabricate a hollow SU-8 microneedle array with the flow channels, and then convert the SU-8 polymer into the glassy carbon microneedle by pyrolysis (Mishra et al. 2018a). Liao et al. systematically studied the factors affecting the quality of the hollow microneedles in TPP technology, including material composition, laser input, and development processing (Liao et al. 2019).
4.1.3 Electric-discharge machining
Electric-Discharge Machining (EDM) is an approach for constructing the complex shapes. The functional principle is using the electrical discharges (sparks) to remove materials and erode the hardened steel with small features. Vinayakumar, KB, and others introduced a method of preparing stainless steel microneedles by a combination of EDM and focused ion beam technology. First, a planar solid SS microneedle array was fabricated by the EDM method and then a focused ion beam was used to make holes Erosion formed microstructures (Vinayakumar et al. 2016a).
4.1.4 Blowing air
The principle is that the polymer droplets are formed into microneedles by blowing air, and the polymer droplets are solidified with a blow to form a microneedle shape. This method can provide mild temperature and fast manufacturing conditions. The specific methods are: 1) dispersing the polymer droplets on a flat substrate; 2) contacting the dispensed droplets through the upper plate; 3) controlling the length of the microneedles by moving the upper plate upwards; 4) purging with air Make the droplets thin and shaped; 5) Separate the two plates so that two rows of microneedles are formed on both plates (Kim et al. 2013), as shown in Fig. 8a. Hu et al. used the thermoplastic stretching of metallic glass to prepare microneedles. The same drawing process can produce solid and hollow microneedles by changing the thickness of metallic glass. They also used the prepared hollow microneedles to inject the liquid into the skin (Hu et al. 2020), as shown in Fig. 8b.
a Fabrication of dissolving microneedles via droplet-born air blowing method (Kim et al. 2013). b Fabrication of the microneedles with adjustable lengths and tips by controlling the rheology and fracture of metallic glass (Hu et al. 2020). c Fabrication of the 3D microneedle structures by drawing lithography in a glass transition (Lee and Jung 2012). d Fabrication of the hyaluronic acid dissolving microneedles by a centrifugal lithography (CL) for (Yang et al. 2017)
4.1.5 Drawing lithography
The drawing lithography makes use of the tensile and elongating properties of viscous fluids. Micro-needle structures are formed by contacting and stretching viscous polymer droplets. The shape cannot be freely controlled and the mechanical strength is weak as shown in Fig. 8a. The hollow glass microneedles prepared by Mahadevan using a standard glass stretching process have ID tip tips of 5 μm (Mahadevan et al. 2013). In Fig. 8c, Lee, K, et al. proposed three drawing techniques of continuous drawing of UHAR hollow microneedles, step-controlled drawing of dissolving microneedles and reverse isolation drawing of folded edges (Lee and Jung 2012).
4.1.6 Centrifugal lithography
The principle is smilar to that of droplet-borne air blowing, and the droplets were elongated by applying a centrifugal force, as shown in Fig. 8b. The specific methods are: 1) the polymer droplets were placed on an inner plate, and an outer parallel plate is not in contact with the droplets; 2) by rotating, the effect of a centrifugal force is distributed in the axial direction of a polymer droplet; 3) with the rotation, the head of the droplet rises and necks until it forms an hourglass shape in contact with the outer plate, and the droplet undergoes a centrifugal evaporation and gradually solidifies; 4) Finally, the solid fracture occurs at the narrow neck of the hourglass, which becomes a column microneedle (Yang et al. 2017), as indicated in Fig. 8d.
4.1.7 3D printing
3D printing technology can use CAD software to design a personalized structure with a unique curved surface to better fit the human skin for use. Lim et al. used additive manufacturing (AM) technology to build a rugged microneedle physical model with geometrical complexity up to the micron level and printed layer by layer until manufacturing is completed (Lim et al. 2017).
For the manufacture of hollow structures, Nicholas and others' work is using a hypodermic needle to insert into the mold to form a hollow tube during 3D printing (Nicholas et al. 2018). Kundu proposed an inexpensive micromachining technique that uses micro drills or laser micromachining to obtain feature subtractive printing for the preparation of hollow microneedles (Kundu et al. 2018).
4.2 Preparation of hollow microneedles with mould
Several methods have been studied for fabricating the hollow microneedles by using pattern transfer methods.
4.2.1 Electroplating with etching
A combination of electroplating and etching is used for the preparation of hollow metal microneedles. Miller, PR et al. used a combination of laser direct writing (LDW) two-photon polymerization (2PP), and electroplating to prepare hollow metal microneedles. First, LDW and 2 pp were used to prepare solid microneedles with internal bosses, which were then formed using PDMS. Metal was then electroplated on the PDMS by pulse deposition to make metal hollow microneedles (Miller et al. 2019).
4.2.2 Coating and demolding
Aydin Sadeqi et al. carved a cross-line pattern on an acrylic plate to prepare the 3D microneedles by a CO2 laser.(Sadeqi et al. 2018) The acrylic plate was subjected to a plasma treatment and a silanization, and then a PDMS mold was obtained by casting the PDMS on the acrylic mold. Finally, through casting a chitosan solution on the PDMS mold, chitosan solid microneedles can be obtained.
The work of Yong-Hun Park et al. was to directly print out PDMS molds (Lee et al. 2016a). Specifically, when a laser beam was directed at a PDMS plate using a commercial carbon dioxide laser writer, a series of tapered holes were created. Adjusting the laser intensity and other parameters to obtain tapered holes of different sizes, shapes, and angles. However, the disadvantage of this method is that laser cauterization will bend PDMS and produce a large amount of powder, which affects the quality of the mold.
4.2.3 Electro-hydraulic atomization
In the problem of drug coverage of coated microneedles, Khan et al. used the electro-hydraulic atomization (EHDA) principle to prepare smart microneedle coatings, coupling stainless steel MNs with ground electrodes, and through coating processes such as changing the flow rate and applying voltage, controlled deposition of particles (100 nm to 3 μm) and fibers (400 nm to 1 μm) on MNs can be controlled directly (Haj-Ahmad et al. 2015; Khan et al. 2014). Angkawinitwong et al. used EHDA to coat PLGA nanoparticles coated with ovalbumin on a hydrogel's MN array. EHDA can form a uniform particle coating on the surface of MNs with a coating efficiency of 30%, and mechanical properties and Insertion performance are not much different from uncoated (Angkawinitwong et al. 2020).
5 Application of microneedles
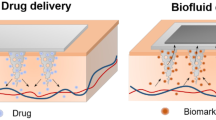
Microneedles have the advantages of being minimally invasive, low pain, and high accuracy, and are widely used in medical fields, such as drug delivery, biosensors, and fluid extraction (Fig. 9). Drug delivery and biosensors, as the two main aspects, are presented here.
5.1 Biosensing
Microneedle sensing can provide a painless and continuous detection of biomarkers for certain diseases. The microneedles have been studied for the construction of several types of biosensors, including glucose, lactate, alcohol, beta-lactam, and glutamic acid.
5.1.1 Glucose biosensor
Glucose is an important parameter for diabetes, and several types of solid and hollow microneedles have been constructed for glucose biosensors. Kim et al. used a CO2 laser to cut a PET film into solid needles and then fixed the carbon and Ag/AgCl electrodes on the top of the needles by screen printing, using a ferrocene carboxylic acid layer as the electron transfer media to enhance the sensor sensitivity. Then the bioengineered mussel adhesion protein (MAP) was used to stabilize the enzyme on it. In order to solve the errors caused by the temperature of the microneedle sensor and the time lag between interstitial and blood glucose, they proposed a new compensation algorithm to improve the performance of CGMS and apply it to clinical experiments, and its accuracy is consistent with a commercial disposable sensors (Kim et al. 2019). A high-pore solid microneedle Au electrode was constructed by an electrochemical self-template method, and glucose dehydrogenase was immobilized by a drip infusion. A microneedle glucose sensor was prepared and studied in artificial interstitial fluid. It showed an excellent sensitivity (50.86 μA cm−2 mM−1), a high stability (20% signal loss after 30 days), and a short response time (3 s) (Bollella et al. 2019a). Gabriela et al. developed a self-powered microneedle glucose sensor that integrates a carbon paste biological anode and cathode in a hollow microneedle array to achieve a continuous, non-invasive monitoring of glucose without the need for an external power supply (Valdes-Ramirez et al. 2014). As shown in Fig. 10a, our group developed an intelligent closed-loop patch based on hollow biodegradable microneedles for diabetes management. The patch can not only monitor interstitial glucose levels but also deliver insulin in real time and continously for the intelligent management of diabetes (Luo et al. 2022).
The wearable Microneedle-Based biosensor. a A diabetes sensor patch based on hollow biodegradable microneedles (Luo et al. 2022). b A bioimpedance sensor based on microneedle for precision farming (Bukhamsin et al. 2021). c A extended gate transistor based on wearable microneedles for real-time detection of sodium in interstitial fluids (Zheng et al. 2022). d A wearable patch using ion electrophoresis double extraction for rapid capture and detection of Epstein Barr virus cell-free DNA (Yang et al. 2020)
5.1.2 Lactate biosensor
The lactate accumulation can cause soreness and fatigue initially. If without any treatment, it would further result in an acidification of the body and may lead to serious diseases. Miller et al. prepared a hollow microneedle sensor using a dynamic light micro-stereolithography. To improve the stability of the lactic acid sensor in interstitial fluid with an anti-interference capability, Paolo et al. functionalized the microneedles, including electrodeposited Au multi-walled carbon nanometers, and electropolymerized mediators such as methylene blue. The sensor showed the excellent performances in artificial interstitial fluid and human serum (Bollella et al. 2019b).
5.1.3 Alcohol biosensor
Alcohol can cause a variety of liver, brain, heart, pancreas and cancer diseases. VinuMohan et al. prepared a microneedle-based subcutaneous alcohol sensing device consisting of three hollow microneedles. Two platinum and one silver wires were placed inside each hollow as the electrodes, and alcohol oxidase was immobilized on a platinum wire that can detect the alcohol concentration in artificial interstitial fluid and mouse isolated skin models (Mohan et al. 2017).
5.1.4 Beta-lactam biosensor
Beta-lactam has a strong bactericidal activity, a low toxicity, a wide indication, and an excellent clinical efficacy. Timothy et al. prepared a beta-lactam microneedle sensor by electrodepositing iridium oxide on the microneedle platinum surface and then immobilized β-lactamase with a hydrogel. The Hill potential equation and logarithmic plot were used for open circuit potential and data analysis to obtain the concentration of beta-lactam (Rawson et al. 2017).
5.1.5 Other biosensor
Windmiller et al. introduced a glutamic acid microneedle sensor for monitoring glutamic acid, using poly-o-phenylenediamine (PPD) film to electropolymerized glutamate oxidase to eliminate the influence of interfering substances, The detection limit of the sensor for glutamate in serum reached 10 μM (Windmiller et al. 2011). Yang et al. studied a wearable epidermis sensor with a reverse iontophoresis for the rapid detection of Epstein Barr virus cell-free DNA. The DNA target was successfully extracted from interstitial fluid within 10 min, and the maximum capture efficiency was 95.4% (Yang et al. 2020), as shown in Fig. 10d. Also, the microneedle sensors had been applied to agriculture, for example, Abdullah bukhamsin's group used the impedance sensor of the microneedle to pierce the wax outside of plants, and obtained the impedance spectrum in the open air environment as a non-destructive monitoring method for crops (Bukhamsin et al. 2021), as illustrated in Fig. 10b. Sodium is a potentially imporatant biomarker for assessing the health condition. As shown in Fig. 10c, Zheng's group reported a microneedle biosensor that was stretchable, stable, and biocompatible for detecting sodium to determin the health status continuously and in real-time (Zheng et al. 2022).
5.1.6 Clinical applications of microneedle sensing
Microneedle products need to undergo a series of laboratory tests, animal trials, and clinical trials before being marketed to prove their safety and effectiveness.
Recently UCSD aimed to develop a minimally invasive microneedle sensor to monitor levodopa levels in real time. The project began in November 2022 and tested the accuracy, tolerability, and safety of the device in patients with Parkinson's disease (Goud et al. 2019). Gowers et al. proposed a potential microneedle-based biosensor to detect local pH changes due to β-lactamase hydrolysis through a pH-sensitive iridium oxide layer. The ability of these biosensors to track penicillin concentrations in the body in real time has been demonstrated in trials with healthy volunteers (Gowers et al. 2019).
Ribet et al. implemented an integrated glucose sensor, which consists of a small sensing probe containing an intact three-electrode electrochemical cell inserted into the lumen of a hollow silicon microneedle. The system relies on capillaries to fill the microneedle cavity to extract tissue fluid. The transdermal portion of the device is 50 times smaller than commercial products, and amperometric tests on the human forearm have shown satisfactory sensitivity and measurement latency consistent with physiological expectations (Ribet et al. 2018). Tehrani et al. reported a fully integrated wearable microneedle technology for wireless and continuous real-time sensing of two metabolites (alcohol and glucose) in volunteer tissue fluids and validated by parallel measurements using standard reference methods. This technique addressed the practicality of wearable devices for epidermal sweat measurement (Tehrani et al. 2022). Arvind et al. presented the results of a preliminary clinical study of a novel prototype microneedle-based continuous glucose monitor in patients with diabetes. The overall mean absolute relative difference (MARD) of sensing blood glucose was 15%, with 98.4% of paired points located in the A + B region of the Clark error grid. What's more, the calibration of fingertip glucose measurement only needs to be performed 1 time per day, which is less frequent compared to most commercially available devices (Jina et al. 2014).
Current clinical applications of microneedle sensors present a number of challenges, such as biological contamination and foreign body reactions that affect the long-term operation of the sensor in humans, among other limiting issues, and microneedle sensors require ultra-sensitive responses to monitor trace levels of many important target molecules and accurately quantify analyte concentrations (Teymourian et al. 2021).
5.2 Transdermal administration of drugs
Although some small-molecule drugs can pass through human skin, the efficiency is low. The microneedle administration can enhance the penetration efficiency of small molecule drugs (Gui et al. 2017; Wu et al. 2016; Cao et al. 2016; Moreira et al. 2020; Gao et al. 2019; Ahmed et al. 2019). Both the solid microneedles and the hollow microneedles have been widely studied for the administration of drugs.
Generally speaking, solid microneedles can enhance the permeability of human skin, and genes, proteins, and drugs can be penetrated and released into the human body. As shown in Fig. 11, solid microneedles can be divided into drug-free microneedles and drug-loaded microneedles. Hollow microneedles can store trace drugs, genes, proteins, and vaccines in or outside the microneedle cavity, and the drug is injected into the tissue through a pinhole.
5.2.1 Solid microneedles
The principle of the drug-free solid microneedles for delivering drugs is that after the microneedles penetrate the skin, they can break the barrier function of the stratum corneum and establish a large number of skin microchannels, then apply a patch on the skin with the existing pores, and the drug enters the skin through the pores so that the transdermal volume of the drug increases significantly. Drug-loaded solid microneedles are divided into coated microneedles and soluble microneedles.
Drugs on solid microneedles
For the coated microneedles, the surfaces of the needles are coverd by drug molecules by a spray coating method, a dipping coating method, etc. The disadvantage is that the amount of drug loaded is relatively small, and the sharpness of the microneedle is affected after the drug load.
A number of coated microneedles were studied for drug delivery. Gao et al. developed a new gelatin/sucrose film-encapsulated polyethylene glycol diacrylate (PEGDA) microneedle patch by the polymerization process (Gao et al. 2019). The experiments on live mice showed that doxorubicin's functional properties were well maintained and that all problems associated with systemic administration of anticancer therapy were avoided. Microneedle scalp administration has a wide range of applications in insulin administration (Vora et al. 2020; Yu et al. 2020; Kim et al. 2020a; Darvishha and Amiri 2019), as shown in Fig. 12a. Due to the capillary effect and highly porous and interconnected structure, the prepared porous polymer microneedles showed a rapid extraction of dermal interstitial fluid and efficient loading. The blood glucose level of the mouse dropped to normal levels within 8 h after the drug administration (Liu et al. 2020). Uppu et al. assembled a microneedle array with a three-component protein subunit vaccine layer by layer for the detection of antigens in mice (Uppu et al. 2020). Pastor et al. used 30% w/w poly (methyl vinyl ether-maleic anhydride) aqueous blends as raw materials to prepare the vaccine microneedles for the outer membrane vesicles of Shigella flexneri. The vesicle vaccine was successfully demonstrated for being released from the microneedles into the BALB/c mice in vivo (Pastor et al. 2019).
The application of microneedles in transdermal drug delivery. a A glucose-responsive insulin patch for regulating blood glucose (Yu et al. 2020). b A porous microneedle array patch based on transdermal electroosmosis (Kusama et al. 2021). c A Patch with thermal responsive microneedles for monitoring and treatment of diabetes (Lee et al. 2016a). d The microneedle platform for buccal macromolecule transportation (Caffarel-Salvador et al. 2021). e A rapidly detachable microneedle patch for continuous release of contraceptives (Li et al. 2019b)
In adiditon, the efficiency of the druy delivery with the microneedles can be enhanced through an external electrical field. For example, as shown in Fig. 12b, Shinya Kusama's group developed a porous microneedle array patch, and an enhanced transdermal drug delivery and glucose extraction can be obtained by applying a DC to the pig skin samples (Kusama et al. 2021).
Soluable microneedles
Soluble microneedles are composed of degradable or soluble polymer materials. Drugs are stored in the needle body by mixing with these polymer materials. After the microneedles entering the human body, they are degraded or dissolved under the action of tissue fluids, thereby Drug release is performed. The advantages of soluble microneedles are that they can automatically degrade even after rupture. The disadvantage is that conditions such as high temperature during the preparation process would affect the stability of the drug.
Several types of soluble microneedles have been used for the drug delivery. Zhang et al. used PLC microneedles that can be degraded by light heating, thereby releasing the loaded metformin (Zhang et al. 2018). Zhan et al. prepared hydroxypropyl methylcellulose and poly (methyl vinyl ether-maleic anhydride) dissolution microneedles as the matrix material containing lidocaine hydrochloride for a rapid local anesthesia, which can be dissolved in rat skin in 5 min (Zhan et al. 2018).
The approaches for accelerating the dissolution of the drugs or the detachment of the microneedles from a patch substrate is the key to the applications. As shown in Fig. 12c. Lee et al. developed a thermally-responsive microneedle that can be thermally activated for the percutaneous drug delivery for diabetes monitoring and treatment (Lee et al. 2016a).
The soluble microneedles have been applied to various body regions. As shown in Fig. 12d, Esther designed a microneedle patch with a high drug load to deliver the macromolecules and applied it to the oral area, successfully delivering 1 mg of human insulin and human growth hormone payload to the buccal cavity of pigs within 30 s (Caffarel-Salvador et al. 2021). Li et al. studied a microneedle patch with a rapid separation. The bubble structure between each microneedle and the patch backing made it easier for the microneedle to penetrate the skin and fell off under shear within five seconds after the application of the patch (Li et al. 2019b), as shown in Fig. 12e.
5.2.2 Hollow microneedles
Compared with the solid microneedles, the hollow microneedles can pass the drug solution through the lumen and release quantitatively under the pressure of an external pump. Compared with traditional transdermal patches, hollow microneedles significantly increased skin permeability, resulting in faster drug absorption and action. But the preparation of hollow microneedles is cumbersome and difficult, and the tissue can create resistance to the microneedle injection (Ma and Wu 2017; Carcamo-Martinez et al. 2021).
Drago et al. constructed the hollow silicon microneedles by deep reactive ion etching to deliver insulin. Although the microneedle injection of insulin resulted in a less decrease in the glucose level compared to that with a subcutaneous infusion, an obvious increase in serum insulin (40–50%) was observed, mainly attributing to a more efficient delivery of insulin at a high insulin (200 IU/ml) by hollow microneedles (Resnik et al. 2018).
In preparation of hollow microneedles, lumens were opened in the side or the center. In side opening, the sharp beveled tip limits the patient pain by reducing the insertion force. For example, Bolton et al. developed a novel dry plasma processing to prepare the hollow microneedles with the beveled tips and vertical sidewalls with a good uniformity, which successfully injected insulin into porcine skin (Bolton et al. 2020).
In the ocular medication, the invasive treatment is sometimes required by hollow microneedles due to the low bioavailability of the drug crossing the cornea. Thakur et al. delivered a thermoresponsive orthotopic implant forming poloxamer formulation into scleral tissue, and the sustained drug delivery could be accomplished by changing the needle penetration depth, the implant gel composition, and the area injected intrasclerally (Thakur et al. 2014).
5.2.3 Clinical applications of microneedle drug delivery
In the past decade, intensive research efforts have led to the approval and commercialization of several microneedle-based products for clinical applications. Numerous clinical trials aimed at investigating the safety and efficacy of microneedle-based systems are ongoing (Bhatnagar et al. 2017). A prefilled hollow microneedle delivery system, the Fluzone Intradermal®, is marketed and the patch can penetrate the skin to deliver the vaccine. This product has been approved by the U.S. FDA for use in influenza vaccination (Jacoby et al. 2015). Tivi Biomedical's CorVax™, a microneedle patch for COVID-19 vaccination, is currently in clinical trials (Rouphael et al. 2017). Nanopatch™ is a microneedle patch used for vaccination, and utilized a miniature array of needles to deliver the vaccine to the deep layers of the skin in order to improve the immune effectiveness of the vaccine. It is undergoing clinical trials and has been ranked as one of the most potential biotechnologies (Meyer et al. 2019).
Zosano Pharma's M207 and Qtrypta™ are microneedle patches for Administration of zolmitriptan intracutaneous, and developed for acute treatment of migraine. These products are undergoing clinical trials to evaluate their effects in patients (Rapoport et al. 2020; Friedman et al. 2021). The LTS smart patch from Lohmann Therapie Systeme has been used for estrogen replacement therapy and pain treatment (Donnelly and Douroumis 2015). Lumixyl® system of Envy Medical is a microneedle patch for cosmetic skin care that can penetrate the skin to deliver skin care ingredients. This product includes a small microneedle array that can deliver skin care ingredients to the deep layers of the skin, and has been approved by the US FDA for the improvement of skin pigmentation and defects (Chen et al. 2021). Dermapen is a microneedle device for skin therapy that can be passed through multiple microneedles to penetrate the skin to treat imperfections and skin problems. This product can be used for the treatment of problems such as vaccinia, scarring, and skin aging. Dermapen has been marketed worldwide and is widely used in the clinics of dermatologists (Sabri et al. 2020).
5.3 Other application
5.3.1 Blood rxtraction
The general method of the extraction of interstital fluid by the solid microneedles is to pierce the stratum corneum with solid microneedles, and then remove interstital fluid by a vacuum chamber. Blicharz et al. prepared a device for collecting capillary blood that includes a solid microneedle patch, a storage vacuum, and a microfluidic system. The clinical studies have shown that the pain from the blood collection by the device is significantly less than that associated with the venipuncture (Blicharz et al. 2018). To solve the dynamic problem of the blood collection by the microneedles, Li and others had invented a blood collection device with an elastic self-recovering actuator and microneedles, as shown in Fig. 13a. The elastic self-restoring actuator was pressed externally to accumulate an elastic energy to drive the blood extraction and delivery. No external power supply was required (Li et al. 2012).
Illustration of the blood-collection and interstitial fluid -extraction device. a An elastic self-healing actuator integrated with microneedles for blood collection (Li et al. 2012). b A hydrogel microneedle patch for detecting interstitial fluid (He et al. 2020). c The hydrogel patch is integrated with an electronic glucose sensor for rapid extraction of microliter skin interstitial fluid (Zheng et al. 2020). d A microneedle patch based on plasma paper for molecular detection in dermal interstitial fluid (Kolluru et al. 2019). e The 3D printing device for interstitial fluid extraction with inclined microneedle penetration (Kim et al. 2021)
5.3.2 Interstitial fluid extraction
Interstitial fluid is a important sample resource that contains many target biomarkers related to disease and health, and has potential application value in health monitoring. There are a few approaches to extract interstitial fluids as follows.
Interstitial fluid collection by diffusion into hydrogel microneedles
The phase change characteristics of hydrogel make the microneedles hard when dry, which is conducive to easy penetration into the skin. At the same time, the high porous microstructure of the hydrogel provides a good swelling capacity for the extraction of interstitial fluid (He et al. 2020).
He, RY, et al. used polyvinyl alcohol and chitosan as the base material to prepare hydrogel microneedle patches. The high pore structure of the hydrogel was used to provide a good swelling and adsorption capacity for the extraction of interstitial fluid. The thermal degradation characteristics of vinyl alcohol can quickly recover the target biomarkers. The device successfully detected the glucose levels in rabbit skin throughout the day (He et al. 2020), as indicated in Fig. 13b. Zheng et al. Introduced an osmotic fluid-driven hydrogel microneedle patch that can extract interstitial fluid three times faster than the existing platform (Zheng et al. 2020), as shown in Fig. 13c.
Interstitial fluid collection by paper
Chandana Kolluru et al. produced micropores on the skin surface through micron-sized microneedles, and collected microliters of ISF on the plasma paper on the patch backing through the micropores to measure interstitial fluid in vivo and R6G in rat serum (Kolluru et al. 2019), as shown in Fig. 13d. Lee et al. inserted the microneedles into the skin at an angle of 66° so that the length of the microneedles can be extended within the safe range of skin penetration in Fig. 13e, and collected the skin interstitial fluid into the paper reservoir on the patch, obtaining 2.9 μl interstitial fluid in 30 s (Kim et al. 2021).
5.3.3 Nerve simulation and recording
In human body, the nervous system controls all voluntary and involuntary processes. Therefore, in many cases, to interfere with the performance of organs, it is necessary to manipulate the nervous system. Depending on the severity of the operation, this interference may be too intrusive or completely non-invasive. Transcutaneous electrical nerve stimulation (TENS), such as those commonly used to treat limb pain, are known as noninvasive techniques. Soltanzadeh used the SU-8 microneedle electrode coated with molybdenum for transcutaneous electrical nerve stimulation. The prepared electrode increased the capacitance and charge transfer resistance of ETI. The harmful Faraday current through the tissue is greatly reduced, which can reduce the pain of the user (Soltanzadeh et al. 2017). Mishra et al. prepared a wearable microneedle sensor array, which can be used to detect opioid drugs (OPI) and organophosphate (OP) nerve agents and can be applied to rapid human body induction (Mishra et al. 2020).
Soltanzadeh et al. studied the microneedle array electrode used for percutaneous electrical nerve stimulation and compared the current density at different depths, the space was constant under the electrode, the specific absorption rate of tissue, the stimulation selectivity, the effect of temperature rise and blood flow on the medical effect (Soltanzadeh et al. 2020). Xie et al. developed an analgesic microneedle patch with soluble microneedles, which can effectively relieve the analgesic effect of neuropathic pain (Xie et al. 2017).
6 Future development of microneedle technology
Efficient and reliable skin penetration of microneedles is one of the most important factors for achieving microneedle applications. However, this can lead to partial or incomplete microneedle penetration due to the elasticity effect of human skin. Since the thickness of human skin varies depending on the age, gender, body mass index, race and skin area of the user, this may lead to variations in the monitoring area of the microneedle sensor, resulting in unreliable monitoring signals.
Another important factor affecting the efficiency of microneedling is the interlocking nature of the needle and the tissue. When worn, the microneedle may slide on or off the skin surface, resulting in drug leakage or perceived mechanical interference creating a noisy signal. Good needle-tissue interlocking can also increase the contact area between the microneedle and skin tissue, promoting the penetration and absorption of drugs and the reliability of monitoring. In this regard, selecting appropriate microneedle materials, such as silicon and polymers, can improve the strength and stiffness of the microneedle. At the same time, optimizing parameters such as the height, tip radius, base diameter, needle density, and spacing of the microneedle can improve the permeability of the microneedle. It can also be combined with optimization of skin preparation, such as exfoliation, scrubbing, and local heating, to improve the permeability of the skin. It can be combined with a suitable applicator to control the insertion force and ensure the correct angle and depth of insertion into the skin.
For drug-delivery microneedles, drug absorption can also be improved by altering the chemical structure of the drug-delivery microneedle to include permeation enhancers, surfactants, acidifiers, etc. For microneedle sensors, the problem of unreliable signals due to random insertion of microneedle sensors can be addressed by using precise liquid dispensers or carefully controlled spraying methods to clearly define the electrode area, or by improving signal calibration algorithms.
In addition, biological contamination and foreign body reactions are other limiting issues that affect the long-term operation of microneedles in vivo. Microneedle insertion can lead to possible tissue trauma and inflammation, and the accumulation of proteins, cells, or macromolecules on the surface of the microneedle sensor through nonspecific binding. This rapid adsorption will prevent the diffusion of the target analyte to the surface of the microneedle sensor, resulting in a gradual decrease in the sensing signal over time. These problems can be eliminated through surface modification, coating, biomass molecules, etc., or multiple sub arrays with different types/thicknesses of coating can be used to sequentially activate each sensor array to extend the service life of the microneedle sensor. These improvements will promote the practical application of microneedles.
With the development of personalized and precision medicine, microneedle technology needs to be further developed to meet the needs of specific patients. For example, research can adjust the drug release rate of microneedles by changing the design, material, and drug carrier of microneedles based on the specific situation of patients, as well as intelligent microneedle systems that can adjust treatment plans in real time. In the application of drug delivery microneedles, electrochemically controlled multiple drug delivery actuators can be developed to achieve higher precision control over the delivery of multiple therapeutic agents on a single microneedle patch. In addition, a system architecture coupling drug delivery and detection of microneedle arrays has been designed to allow a highly integrated module with closed-loop functionality to appear in a microneedle patch to prepare small, low-pain, convenient disease management devices. These would be attractive new applications for microneedles.
7 Conclusions
The microneedles have attracted increasing attentions for a variety of healthcare applications, such as drug delivery, extraction of interstitial fluid, and biosensing. The ongoing challenges include the material selection for the microneedles, the configuration of the microneedles, the fabrication methods, and the target desired applications. Many materials have been introduced and characterized for microneedle construction, including silicon, glass, ceramic, glassy carbon, stainless steel, titanium, nickel, aluminum, PC, PVP, PLA, acrylate, hydrogel, PVA, PCL, PS, CMC, CAP, and chitosan. The configurations of the microneedles include solid microneedles, and hollow microneedles. The methods for fabricating microneedles of each specific shape and configuration include photolithography/machining with selective etching, direct processing, and pattern transfer. In addition, the microneedles have been explored for a variety of applications, including biosensors, drug deliveries, body fluid extractions, nerve simulation, and nerve recording. This review serves as a resource for materials and fabrication methods for microneedles in biomedical devices, and their related healthcare applications.
Availability of data and materials
The materials presented in this study are available on request.
References
M.J. Abla, A. Chaturvedula, C. O’Mahony, A.K. Banga, Transdermal delivery of methotrexate for pediatrics using silicon microneedles. Ther. Deliv. 4(5), 543–551 (2013). https://doi.org/10.4155/tde.13.24
S.S. Abubaker, Y.J. Zhang, Optimization design and fabrication of polymer micro needle by hot embossing method. Int. J. Precis. Eng. Manuf. 20(4), 631–640 (2019). https://doi.org/10.1007/s12541-019-00095-z
K.S. Ahmed, X. Shan, J. Mao, L. Qiu, J. Chen, Derma roller (R) microneedles-mediated transdermal delivery of doxorubicin and celecoxib co-loaded liposomes for enhancing the anticancer effect. Mater. Sci. Eng. C. Mater. Biol. Appl. 99, 1448–1458 (2019). https://doi.org/10.1016/j.msec.2019.02.095
T.E. Andersen, A.J. Andersen, R.S. Petersen, L.H. Nielsen, S.S. Keller, Drug loaded biodegradable polymer microneedles fabricated by hot embossing. Microelectron. Eng. 195, 57–61 (2018). https://doi.org/10.1016/j.mee.2018.03.024
A. Anderson, C. Hegarty, C. Casimero, J. Davis, Electrochemically controlled dissolution of nanocarbon-cellulose acetate phthalate microneedle arrays. ACS. Appl. Mater. Interfaces. 11(39), 35540–35547 (2019). https://doi.org/10.1021/acsami.9b09674
U. Angkawinitwong, A.J. Courtenay, A.M. Rodgers, E. Larraneta, H.O. McCarthy, S. Brocchini, R.F. Donnelly, G.R. Williams, A novel transdermal protein delivery strategy via electrohydrodynamic coating of PLGA microparticles onto microneedles. ACS. Appl. Mater. Interfaces. 12(11), 12478–12488 (2020). https://doi.org/10.1021/acsami.9b22425
M. Arai, S. Masubuchi, K. Nose, Y. Mitsuda, T. Machida, Fabrication of 10-nm-scale nanoconstrictions in graphene using atomic force microscopy-based local anodic oxidation lithography. Jpn. J. Appl. Phys. 54(4), 04dj06 (2015). https://doi.org/10.7567/jjap.54.04dj06
W. Bai, Y. Li, X. Chen, Metal micro needle arrays based on the LIGA technology. Microelectron. Tech. 49(2), 118–123 (2012). https://doi.org/10.3969/j.issn.1671-4776.2012.02.009
S. Bhatnagar, K. Dave, V.V.K. Venuganti, Microneedles in the clinic. J. Control. Release. 260, 164–182 (2017). https://doi.org/10.1016/j.jconrel.2017.05.029
T.M. Blicharz, P. Gong, B.M. Bunner, L.L. Chu, K.M. Leonard, J.A. Wakefield, R.E. Williams, M. Dadgar, C.A. Tagliabue, R. El Khaja, S.L. Marlin, R. Haghgooie, S.P. Davis, D.E. Chickering, H. Bernstein, Microneedle-based device for the one-step painless collection of capillary blood samples. Nat. Biomed. Eng. 2(3), 151–157 (2018). https://doi.org/10.1038/s41551-018-0194-1
M. Bok, Z.-J. Zhao, S. Jeon, J.-H. Jeong, E. Lim, Ultrasonically and iontophoretically enhanced drug-delivery system based on dissolving microneedle patches. Sci. Rep. 10(1), 2027–2027 (2020). https://doi.org/10.1038/s41598-020-58822-w
P. Bollella, S. Sharma, A.E.G. Cass, F. Tasca, R. Antiochia, Minimally invasive glucose monitoring using a highly porous gold microneedles-based biosensor: characterization and application in artificial interstitial fluid. Catalysts. 9(7), 14 (2019a). https://doi.org/10.3390/catal9070580
P. Bollella, S. Sharma, A.E.G. Cass, R. Antiochia, Microneedle-based biosensor for minimally-invasive lactate detection. Biosens. Bioelectron. 123, 152–159 (2019b). https://doi.org/10.1016/j.bios.2018.08.010
C.J.W. Bolton, O. Howells, G.J. Blayney, P.F. Eng, J.C. Birchall, B. Gualeni, K. Roberts, H. Ashraf, O.J. Guy, Hollow silicon microneedle fabrication using advanced plasma etch technologies for applications in transdermal drug delivery. Lab. Chip. 20(15), 2788–2795 (2020). https://doi.org/10.1039/d0lc00567c
A. Bukhamsin, K. Moussi, R. Tao, G. Lubineau, I. Blilou, K.N. Salama, J. Kosel, Robust, long-term, and exceptionally sensitive microneedle-based bioimpedance sensor for precision farming. Adv. Sci. 8(16), 2101261 (2021). https://doi.org/10.1002/advs.202101261
S. Bystrova, R. Luttge, Micromolding for ceramic microneedle arrays. Microelectron. Eng. 88(8), 1681–1684 (2011). https://doi.org/10.1016/j.mee.2010.12.067
E. Caffarel-Salvador, S. Kim, V. Soares, R.Y. Tian, S.R. Stern, D. Minahan, R. Yona, X. Lu, F.R. Zakaria, J. Collins, J. Wainer, J. Wong, R. McManus, S. Tamang, S. McDonnell, K. Ishida, A. Hayward, X. Liu, F. Hubalek, J. Fels, A. Vegge, M.R. Frederiksen, U. Rahbek, T. Yoshitake, J. Fujimoto, N. Roxhed, R. Langer, G. Traverso, A microneedle platform for buccal macromolecule delivery. Sci. Adv. 7(4), eabe2620 (2021). https://doi.org/10.1126/sciadv.abe2620
E.M. Cahill, S. Keaveney, V. Stuettgen, P. Eberts, P. Ramos-Luna, N. Zhang, M. Dangol, E.D. O’Cearbhaill, Metallic microneedles with interconnected porosity: a scalable platform for biosensing and drug delivery. Acta. Biomater. 80, 401–411 (2018). https://doi.org/10.1016/j.actbio.2018.09.007
Y. Cao, Y. Tao, Y. Zhou, S. Gui, Development of sinomenine hydrochloride-loaded polyvinylalcohol/maltose microneedle for transdermal delivery. J. Drug. Deliv. Sci. Technol. 35, 1–7 (2016). https://doi.org/10.1016/j.jddst.2016.06.007
A. Carcamo-Martinez, B. Mallon, J. Dominguez-Robles, L.K. Vora, Q.K. Anjani, R.F. Donnelly, Hollow microneedles: a perspective in biomedical applications. Int. J. Pharm. 599, 120455 (2021). https://doi.org/10.1016/j.ijpharm.2021.120455
M.-C. Chen, K.-W. Wang, D.-H. Chen, M.-H. Ling, C.-Y. Liu, Remotely triggered release of small molecules from LaB6@SiO2-loaded polycaprolactone microneedles. Acta Biomater. 13, 344–353 (2015). https://doi.org/10.1016/j.actbio.2014.11.040
M.-C. Chen, H.-A. Chan, M.-H. Ling, L.-C. Su, Implantable polymeric microneedles with phototriggerable properties as a patient-controlled transdermal analgesia system. J. Mater. Chem. B. 5(3), 496–503 (2017). https://doi.org/10.1039/c6tb02718k
J. Chen, P. Cheng, Y. Sun, Y. Wang, X. Zhang, Z. Yang, G. Ding, A minimally invasive hollow microneedle with a cladding structure: ultra-thin but strong, batch manufacturable. I.E.E.E. Trans. Biomed. Eng. 66(12), 3480–3485 (2019). https://doi.org/10.1109/tbme.2019.2906571
J. Chen, J. Bian, B.M. Hantash, L. Albakr, D.E. Hibbs, X. Xiang, P. Xie, C. Wu, L. Kang, Enhanced skin retention and permeation of a novel peptide via structural modification, chemical enhancement, and microneedles. Int. J. Pharm. 606 (2021). https://doi.org/10.1016/j.ijpharm.2021.120868
P.C. Chen, S.J. Hsieh, C.C. Chen, J. Zou, A three-dimensional enormous surface area aluminum microneedle array with nanoporous structure. J. Nanomater. 6 (2013). https://doi.org/10.1155/2013/164953
S. Chen, D. Wu, Y. Liu, Y. Huang, H. Xu, W. Gao, J. Zhang, J. Sun, J. Zhuang, Optimal scaling analysis of polymeric microneedle length and its effect on transdermal insulin delivery. J. Drug. Deliv. Sci. Technol. 56, 101547 (2020). https://doi.org/10.1016/j.jddst.2020.101547
P. Dardano, A. Calio, V. Di Palma, M.F. Bevilacqua, A. Di Matteo, L. De Stefano, A photolithographic approach to polymeric microneedles array fabrication. Materials. 8(12), 8661–8673 (2015). https://doi.org/10.3390/ma8125484
S. Darvishha, S. Amiri, (Trans) dermal insulin delivery based on polymeric systems. Int. J. Polym. Mater. Polym. Biomater. 68(18), 1118–1132 (2019). https://doi.org/10.1080/00914037.2018.1534113
A. Das, C. Singha, A. Bhattacharyya, Development of silicon microneedle arrays with spontaneously generated micro-cavity ring for transdermal drug delivery. Microelectron. Eng. 210, 14–18 (2019). https://doi.org/10.1016/j.mee.2019.03.019
R. Donnelly, D. Douroumis, Microneedles for drug and vaccine delivery and patient monitoring. Drug. Deliv. Transl. Res. 5(4), 311–312 (2015). https://doi.org/10.1007/s13346-015-0250-2
S.N. Economidou, C.P.P. Pere, A. Reid, M.J. Uddin, J.F.C. Windmill, D.A. Lamprou, D. Douroumis, 3D printed microneedle patches using stereolithography (SLA) for intradermal insulin delivery. Mater. Sci. Eng. C. Mater. Biol. Appl. 102, 743–755 (2019). https://doi.org/10.1016/j.msec.2019.04.063
D. Friedman, E. Spierings, J. Engels, D. Kellerman, S. Tepper, Onset of action of a zolmitriptan microneedle system (M207, Qtrypta (TM)) for migraine: comparison with recent early time to onset recommendations, pain relief results and placebo response. Neurology. 96(15) (2021)
Y. Gao, M. Hou, R. Yang, L. Zhang, Z. Xu, Y. Kang, P. Xue, Transdermal delivery of therapeutics through dissolvable gelatin/sucrose films coated on PEGDA microneedle arrays with improved skin permeability. J. Mater. Chem. B. 7(47), 7515–7524 (2019). https://doi.org/10.1039/c9tb01994d
E. Garcia-Lopez, H.R. Siller, C.A. Rodriguez, Study of the fabrication of AISI 316L microneedle arrays. Procedia. Manuf. 26, 117–124 (2018). https://doi.org/10.1016/j.promfg.2018.07.014
S. Gholami, M.M. Mohebi, E. Hajizadeh-Saffar, M.H. Ghanian, I. Zarkesh, H. Baharvand, Fabrication of microporous inorganic microneedles by centrifugal casting method for transdermal extraction and delivery. Int. J. Pharm. 558, 299–310 (2019). https://doi.org/10.1016/j.ijpharm.2018.12.089
S.D. Gittard, B. Chen, H. Xu, A. Ovsianikov, B.N. Chichkov, N.A. Monteiro-Riviere, R.J. Narayan, The effects of geometry on skin penetration and failure of polymer microneedles. J. Adhes. Sci. Technol. 27(3), 227–243 (2013). https://doi.org/10.1080/01694243.2012.705101
K.Y. Goud, C. Moonla, R.K. Mishra, C. Yu, R. Narayan, I. Litvan, J. Wang, Wearable electrochemical microneedle sensor for continuous monitoring of levodopa: toward Parkinson management. ACS. Sens. 4(8), 2196–2204 (2019). https://doi.org/10.1021/acssensors.9b01127
S.A.N. Gowers, D.M.E. Freeman, T.M. Rawson, M.L. Rogers, R.C. Wilson, A.H. Holmes, A.E. Cass, D. O'Hare, Development of a minimally invasive microneedle-based sensor for continuous monitoring of beta-lactam antibiotic concentrations in vivo. Acs. Sens. 4(4), 1072 (2019). https://doi.org/10.1021/acssensors.9b00288
Z. Gui, X. Wu, S. Wang, Y. Cao, J. Wan, Q. Shan, Z. Yang, J. Zhang, S. Gui, Dissolving microneedles integrated with liquid crystals facilitate transdermal delivery of sinomenine hydrochloride. J. Pharm. Sci. 106(12), 3548–3555 (2017). https://doi.org/10.1016/j.xphs.2017.07.027
J. Gupta, E.I. Felner, M.R. Prausnitz, Rapid pharmacokinetics of intradermal insulin administered using microneedles in type 1 diabetes subjects. Diabetes. Technol. Ther. 13(4), 451–456 (2011). https://doi.org/10.1089/dia.2010.0204
R. Haj-Ahmad, H. Khan, M.S. Arshad, M. Rasekh, A. Hussain, S. Walsh, X. Li, M.-W. Chang, Z. Ahmad, Microneedle coating techniques for transdermal drug delivery. Pharmaceutics. 7(4), 486–502 (2015). https://doi.org/10.3390/pharmaceutics7040486
D. Han, R.S. Morde, S. Mariani, A.A. La Mattina, E. Vignali, C. Yang, G. Barillaro, H. Lee, 4D Printing of a bioinspired microneedle array with backward-facing barbs for enhanced tissue adhesion. Adv. Funct. Mater. 30(11), 1909197 (2020). https://doi.org/10.1002/adfm.201909197
X.H.M. Hartmann, P. van der Linde, E.F.G.A. Homburg, L.C.A. van Breemen, A.M. de Jong, R. Luttge, Insertion process of ceramic nanoporous microneedles by means of a novel mechanical applicator design. Pharmaceutics. 7(4), 503–522 (2015). https://doi.org/10.3390/pharmaceutics7040503
R.Y. He, Y. Niu, Z.D. Li, A.Y. Li, H. Yang, F. Xu, F. Li, A hydrogel microneedle patch for point-of-care testing based on skin interstitial fluid. Adv. Healthc. Mater. 9(4), 11 (2020). https://doi.org/10.1002/adhm.201901201
J. Held, J. Gaspar, P. Ruther, M. Hagner, A. Cismak, A. Heilmann, O. Paul, Design of experiment characterization of microneedle fabrication processes based on dry silicon etching. J. Micromech. Microeng. 20(2), 11 (2010). https://doi.org/10.1088/0960-1317/20/2/025024
S. Henry, D.V. McAllister, M.G. Allen, M.R. Prausnitz, Ieee, Micromachined needles for the transdermal delivery of drugs (Ieee, New York, 1998)
T. Hoa Le, T. Bao Quoc, T. Hai Le, N. Vy, K. Wang, F. Karlsen, Low-cost fabrication of hollow microneedle arrays using CNC machining and UV lithography. J. Microelectromech. Syst. 24(5), 1583–1593 (2015). https://doi.org/10.1109/jmems.2015.2424926
O. Howells, G.J. Blayney, B. Gualeni, J.C. Birchall, P.F. Eng, H. Ashraf, S. Sharma, O.J. Guy, Design, fabrication, and characterisation of a silicon microneedle array for transdermal therapeutic delivery using a single step wet etch process. Eur. J. Pharm. Biopharm. 171, 19–28 (2022). https://doi.org/10.1016/j.ejpb.2021.06.005
Z. Hu, C.S. Meduri, R.S.J. Ingrole, H.S. Gill, G. Kumar, Solid and hollow metallic glass microneedles for transdermal drug-delivery. Appl. Phys. Lett. 116(20), 203703 (2020). https://doi.org/10.1063/5.0008983
K. Ita, Transdermal delivery of drugs with microneedles-potential and challenges. Pharmaceutics. 7(3), 90–105 (2015). https://doi.org/10.3390/pharmaceutics7030090
E. Jacoby, C. Jarrahian, H.F. Hull, D. Zehrung, Opportunities and challenges in delivering influenza vaccine by microneedle patch. Vaccine. 33(37), 4699–4704 (2015). https://doi.org/10.1016/j.vaccine.2015.03.062
A. Jina, M.J. Tierney, J.A. Tamada, S. McGill, S. Desai, B. Chua, A. Chang, M. Christiansen, Design, development, and evaluation of a novel microneedle array-based continuous glucose monitor. J. Diabetes. Sci. Technol. 8(3), 483–487 (2014). https://doi.org/10.1177/1932296814526191
J.H. Jung, S.G. Jin, Microneedle for transdermal drug delivery: current trends and fabrication. J. Pharm. Investig. 51(5), 503–517 (2021). https://doi.org/10.1007/s40005-021-00512-4
H. Kalluri, A.K. Banga, Microneedles and transdermal drug delivery. J. Drug. Deliv. Sci. Technol. 19(5), 303–310 (2009). https://doi.org/10.1016/s1773-2247(09)50065-2
N.A.M. Kamal, T.M.T. Mahmood, I. Ahmad, S. Ramli, Improving rate of gelatin/carboxymethylcellulose dissolving microneedle for transdermal drug delivery. Sains. Malaysiana. 49(9), 2269–2279 (2020). https://doi.org/10.17576/jsm-2020-4909-24
H. Khan, P. Mehta, H. Msallam, D. Armitage, Z. Ahmad, Smart microneedle coatings for controlled delivery and biomedical analysis. J. Drug Target. 22(9), 790–795 (2014). https://doi.org/10.3109/1061186x.2014.921926
O. Khandan, M.Y. Kahook, M.P. Rao, Fenestrated microneedles for ocular drug delivery. Sens. Actuator. B. Chem. 223, 15–23 (2016). https://doi.org/10.1016/j.snb.2015.09.071
P. Khanna, K. Luongo, J.A. Strom, S. Bhansali, Axial and shear fracture strength evaluation of silicon microneedles. Microsyst. Technol. Micro Nanosyst. Inf. Storage. Process. Syst. 16(6), 973–978 (2010). https://doi.org/10.1007/s00542-010-1070-4
P. Khanna, B.R. Flam, B. Osborn, J.A. Strom, S. Bhansali, Skin penetration and fracture strength testing of silicon dioxide microneedles. Sens. Actuator. A. Phys. 170(1–2), 180–186 (2011). https://doi.org/10.1016/j.sna.2010.09.024
J.D. Kim, M. Kim, H. Yang, K. Lee, H. Jung, Droplet-born air blowing: novel dissolving microneedle fabrication. J. Control. Release 170(3), 430–436 (2013). https://doi.org/10.1016/j.jconrel.2013.05.026
M.J. Kim, S.C. Park, B. Rizal, G. Guanes, S.K. Baek, J.H. Park, A.R. Betz, S.O. Choi, Fabrication of circular obelisk-type multilayer microneedles using micro-milling and spray deposition. Front. Bioeng. Biotechnol. 6, 13 (2018). https://doi.org/10.3389/fbioe.2018.00054
K.B. Kim, H. Choi, H.J. Jung, Y.J. Oh, C.H. Cho, J.H. Min, S. Yoon, J. Kim, S.J. Cho, H.J. Cha, Mussel-inspired enzyme immobilization and dual real-time compensation algorithms for durable and accurate continuous glucose monitoring. Biosens. Bioelectron. 143, 7 (2019). https://doi.org/10.1016/j.bios.2019.111622
D.-S. Kim, J.-T. Choi, C.B. Kim, Y.-R. Shin, P.-G. Park, H. Kim, J.M. Lee, J.-H. Park, Microneedle array patch (MAP) consisting of crosslinked hyaluronic acid nanoparticles for processability and sustained release. Pharm. Res. 37(3), 50 (2020a). https://doi.org/10.1007/s11095-020-2768-3
S. Kim, H. Yang, J. Eum, Y. Ma, S. Fakhraei Lahiji, H. Jung, Implantable powder-carrying microneedles for transdermal delivery of high-dose insulin with enhanced activity. Biomaterials. 232, 119733 (2020b). https://doi.org/10.1016/j.biomaterials.2019.119733
S. Kim, M.S. Lee, H.S. Yang, J.H. Jung, Enhanced extraction of skin interstitial fluid using a 3D printed device enabling tilted microneedle penetration. Sci. Rep. 11(1), 14018 (2021). https://doi.org/10.1038/s41598-021-93235-3
C. Kolluru, R. Gupta, Q. Jiang, M. Williams, H.G. Derami, S. Cao, R.K. Noel, S. Singamaneni, M.R. Prausnitz, Plasmonic paper microneedle patch for on-patch detection of molecules in dermal interstitial fluid. ACS. Sensors. 4(6), 1569–1576 (2019). https://doi.org/10.1021/acssensors.9b00258
K.J. Krieger, N. Bertollo, M. Dangol, J.T. Sheridan, M.M. Lowery, E.D. O’Cearbhaill, Simple and customizable method for fabrication of high-aspect ratio microneedle molds using low-cost 3D printing. Microsyst. Nanoeng. 5, 42 (2019). https://doi.org/10.1038/s41378-019-0088-8
A. Kundu, T. Ausaf, S. Rajaraman, 3D Printing, Ink casting and micromachined lamination (3D PICLM): a makerspace approach to the fabrication of biological microdevices. Micromachines. 9(2), 23 (2018). https://doi.org/10.3390/mi9020085
S. Kusama, K. Sato, Y. Matsui, N. Kimura, H. Abe, S. Yoshida, M. Nishizawa, Transdermal electroosmotic flow generated by a porous microneedle array patch. Nat. Commun. 12(1), 658 (2021). https://doi.org/10.1038/s41467-021-20948-4
K. Lee, H. Jung, Drawing lithography for microneedles: A review of fundamentals and biomedical applications. Biomaterials. 33(30), 7309–7326 (2012). https://doi.org/10.1016/j.biomaterials.2012.06.065
J.W. Lee, S.-O. Choi, E.I. Felner, M.R. Prausnitz, Dissolving microneedle patch for transdermal delivery of human growth hormone. Small. 7(4), 531–539 (2011). https://doi.org/10.1002/smll.201001091
H. Lee, T.K. Choi, Y.B. Lee, H.R. Cho, R. Ghaffari, L. Wang, H.J. Choi, T.D. Chung, N.S. Lu, T. Hyeon, S.H. Choi, D.H. Kim, A graphene-based electrochemical device with thermoresponsive microneedles for diabetes monitoring and therapy. Nat. Nanotechnol. 11(6), 566 (2016a). https://doi.org/10.1038/nnano.2016.38
S.J. Lee, H.S. Yoon, X. Xuan, J.Y. Park, S.-J. Paik, M.G. Allen, A patch type non-enzymatic biosensor based on 3D SUS micro-needle electrode array for minimally invasive continuous glucose monitoring. Sens. Actuator. B. Chem. 222, 1144–1151 (2016b). https://doi.org/10.1016/j.snb.2015.08.013
C.G. Li, K. Lee, C.Y. Lee, M. Dangol, H. Jung, A Minimally invasive blood-extraction system: elastic self-recovery actuator integrated with an ultrahigh- aspect-ratio microneedle. Adv. Mater. 24(33), 4583–4586 (2012). https://doi.org/10.1002/adma.201201109
J.Y. Li, B. Liu, Y.Y. Zhou, Z.P. Chen, L.L. Jiang, W. Yuan, L. Liang, Fabrication of a Ti porous microneedle array by metal injection molding for transdermal drug delivery. PLoS. ONE. 12(2), 15 (2017). https://doi.org/10.1371/journal.pone.0172043
J.Y. Li, Y.Y. Zhou, J.B. Yang, R. Ye, J. Gao, L. Ren, B. Liu, L. Liang, L.L. Jiang, Fabrication of gradient porous microneedle array by modified hot embossing for transdermal drug delivery. Mater. Sci. Eng. C. Mater. Biol. Appl. 96, 576–582 (2019a). https://doi.org/10.1016/j.msec.2018.11.074
W. Li, R.N. Terry, J. Tang, M.R. Feng, S.P. Schwendeman, M.R. Prausnitz, Rapidly separable microneedle patch for the sustained release of a contraceptive. Nat. Biomed. Eng. 3(3), 220 (2019b). https://doi.org/10.1038/s41551-018-0337-4
Z.-X. Liao, Y.-G. Li, J. Zhu, Design and fabrication of micro needles array based on UV-LIGA technology. J. Shanghai. Jiaotong. Univ. 46(11), 1848–1851 (2012)
C. Liao, W. Anderson, F. Antaw, M. Trau, Two-photon nanolithography of tailored hollow three-dimensional microdevices for biosystems. ACS. Omega. 4(1), 1401–1409 (2019). https://doi.org/10.1021/acsomega.8b03164
F.S. Iliescu, J.C.M. Teo, D. Vrtacnik, H. Taylor, C. Iliescu, Cell therapy using an array of ultrathin hollow microneedles. Microsystem Technologies-Micro-and Nanosystems-Information Storage and Processing Systems 24(7), 2905–2912. (2018). https://doi.org/10.1007/s00542-017-3631-2
S.H. Lim, J.Y. Ng, L.F. Kang, Three-dimensional printing of a microneedle array on personalized curved surfaces for dual-pronged treatment of trigger finger. Biofabrication. 9(1), 13 (2017). https://doi.org/10.1088/1758-5090/9/1/015010
D.P. Liu, B. Yu, G.H. Jiang, W.J. Yu, Y. Zhang, B. Xu, Fabrication of composite microneedles integrated with insulin-loaded CaCO3 microparticles and PVP for transdermal delivery in diabetic rats. Mater. Sci. Eng. C. Mater. Biol. Appl. 90, 180–188 (2018). https://doi.org/10.1016/j.msec.2018.04.055
R. Liu, X. Wang, Z. Zhou, Application of MEMS microneedles array in biomedicine. J. Biomed. Eng. 21(3), 482–485 (2004)
P. Liu, H. Du, Y. Chen, H. Wang, J. Mao, L. Zhang, J. Tao, J. Zhu, Polymer microneedles with interconnected porous structures via a phase inversion route for transdermal medical applications. J. Mat. Chem. B. 8(10), 2032–2039 (2020). https://doi.org/10.1039/c9tb02837d
W. Luangveera, S. Jiruedee, W. Mama, M. Chiaranairungroj, A. Pimpin, T. Palaga, W. Srituravanich, Fabrication and characterization of novel microneedles made of a polystyrene solution. J. Mech. Behav. Biomed. Mater. 50, 77–81 (2015). https://doi.org/10.1016/j.jmbbm.2015.06.009
X. Luo, Q. Yu, Y. Liu, W. Gai, L. Ye, L. Yang, Y. Cui, Closed-loop diabetes minipatch based on a biosensor and an electroosmotic pump on hollow biodegradable microneedles br. Acs. Sens. 7(5), 1347–1360 (2022). https://doi.org/10.1021/acssensors.1c02337
M.A. Luzuriaga, D.R. Berry, J.C. Reagan, R.A. Smaldone, J.J. Gassensmith, Biodegradable 3D printed polymer microneedles for transdermal drug delivery. Lab. Chip. 18(8), 1223–1230 (2018). https://doi.org/10.1039/c8lc00098k
G. Ma, C. Wu, Microneedle, bio-microneedle and bio-inspired microneedle: a review. J. Control. Release. 251, 11–23 (2017). https://doi.org/10.1016/j.jconrel.2017.02.011
G. Mahadevan, H. Sheardown, P. Selvaganapathy, PDMS embedded microneedles as a controlled release system for the eye. J. Biomater. Appl. 28(1), 20–27 (2013). https://doi.org/10.1177/0885328211433778
A. McConville, J. Davis, Transdermal microneedle sensor arrays based on palladium: Polymer composites. Electrochem. Commun. 72, 162–165 (2016). https://doi.org/10.1016/j.elecom.2016.09.024
B.K. Meyer, M.A.F. Kendall, D.M. Williams, A.J. Bett, S. Dubey, R.C. Gentzel, D. Casimiro, A. Forster, H. Corbett, M. Crichton, S. Ben Baker, R.K. Evans, A. Bhambhani, Immune response and reactogenicity of an unadjuvanted intradermally delivered human papillomavirus vaccine using a first generation Nanopatch (TM) in rhesus macaques: an exploratory, pre-clinical feasibility assessment. Vaccine. X. 2 (2019). https://doi.org/10.1016/j.jvacx.2019.100030
P.R. Miller, M. Moorman, R.D. Boehm, S. Wolfley, V. Chavez, J.T. Baca, C. Ashley, I. Brener, R.J. Narayan, R. Polsku, Fabrication of hollow metal microneedle arrays using a molding and electroplating method. Mrs. Adv. 4(24), 1417–1426 (2019). https://doi.org/10.1557/adv.2019.147
K.B. Mirza, C. Zuliani, B. Hou, F.S. Ng, N.S. Peters, C. Toumazou, Ieee, Injection moulded microneedle sensor for real-time wireless pH monitoring. In: 2017 39th Annual International Conference of the Ieee Engineering in Medicine and Biology Society, pp. 189–192 (2017)
R. Mishra, B. Pramanick, T.K. Maiti, T.K. Bhatracharyya, Glassy carbon microneedles-new transdermal drug delivery device derived from a scalable C-MEMS process. Microsyst. Nanoeng. 4, 11 (2018a). https://doi.org/10.1038/s41378-018-0039-9
R. Mishra, T.K. Maiti, T.K. Bhattacharyya, Development of SU-8 hollow microneedles on a silicon substrate with microfluidic interconnects for transdermal drug delivery. JMiMi. 28(10), 105017 (2018b). https://doi.org/10.1088/1361-6439/aad301
R.K. Mishra, K.Y. Goud, Z. Li, C. Moonla, M.A. Mohamed, F. Tehrani, H. Teymourian, J. Wang, Continuous opioid monitoring along with nerve agents on a wearable microneedle sensor array. J. Am. Chem. Soc. 142(13), 5991–5995 (2020). https://doi.org/10.1021/jacs.0c01883
A.M.V. Mohan, J.R. Windmiller, R.K. Mishra, J. Wang, Continuous minimally-invasive alcohol monitoring using microneedle sensor arrays. Biosens. Bioelectron. 91, 574–579 (2017). https://doi.org/10.1016/j.bios.2017.01.016
S.J. Moon, S.S. Lee, A novel fabrication method of a microneedle array using inclined deep x-ray exposure. J. Micromech. Microeng. 15(5), 903–911 (2005). https://doi.org/10.1088/0960-1317/15/5/002
A.F. Moreira, C.F. Rodrigues, T.A. Jacinto, S.P. Miguel, E.C. Costa, I.J. Correia, Poly (vinyl alcohol)/chitosan layer-by-layer microneedles for cancer chemo-photothermal therapy. Int. J. Pharm. 576, 118907–118907 (2020). https://doi.org/10.1016/j.ijpharm.2019.118907
K. Nair, B. Whiteside, C. Grant, R. Patel, C. Tuinea-Bobe, K. Norris, A. Paradkar, Investigation of plasma treatment on micro-injection moulded microneedle for drug delivery. Pharmaceutics. 7(4), 471–485 (2015). https://doi.org/10.3390/pharmaceutics7040471
S.P. Narayanan, S. Raghavan, Fabrication and characterization of gold-coated solid silicon microneedles with improved biocompatibility. Int. J. Adv. Manuf. Technol. 104(9–12), 3327–3333 (2019). https://doi.org/10.1007/s00170-018-2596-3
A. Nayak, D.B. Das, G.T. Vladisavljevic, Microneedle-assisted permeation of lidocaine carboxymethylcellulose with gelatine co-polymer hydrogel. Pharm. Res. 31(5), 1170–1184 (2014). https://doi.org/10.1007/s11095-013-1240-z
D. Nicholas, K.A. Logan, Y.J. Sheng, J.H. Gao, S. Farrell, D. Dixon, B. Callan, A.P. McHale, J.F. Callan, Rapid paper based colorimetric detection of glucose using a hollow microneedle device. Int. J. Pharm. 547(1–2), 244–249 (2018). https://doi.org/10.1016/j.ijpharm.2018.06.002
Y. Nishinaka, R. Jun, G.S. Prihandana, N. Miki, Fabrication of polymer microneedle electrodes coated with nanoporous parylene. Jpn. J. Appl. Phys. 52(6), 5 (2013). https://doi.org/10.7567/jjap.52.06gl10
C. O'Mahony, A. Bocchino, M.J. Haslinger, S. Brandstaetter, H. Aufsserhuber, K. Schossleitner, A.J.P. Clover, D. Fechtig, Piezoelectric inkjet coating of injection moulded, reservoir-tipped microneedle arrays for transdermal delivery. JMiMi. 29(8), 085004 (2019). https://doi.org/10.1088/1361-6439/ab222b
T. Omatsu, K. Chujo, K. Miyamoto, M. Okida, K. Nakamura, N. Aoki, R. Morita, Metal microneedle fabrication using twisted light with spin. Opt. Express. 18(17), 17967–17973 (2010). https://doi.org/10.1364/oe.18.017967
A. Ovsianikov, B. Chichkov, P. Mente, N.A. Monteiro-Riviere, A. Doraiswamy, R.J. Narayan, Two photon polymerization of polymer-ceramic hybrid materials for transdermal drug delivery. Int. J. Appl. Ceram. Technol. 4(1), 22–29 (2007). https://doi.org/10.1111/j.1744-7402.2007.02115.x
J.H. Park, M.G. Allen, M.R. Prausnitz, Biodegradable polymer microneedles: fabrication, mechanics and transdermal drug delivery. J. Control. Release. 104(1), 51–66 (2005). https://doi.org/10.1016/j.jconrel.2005.02.002
Y. Pastor, E. Larraneta, A. Erhard, G. Quincooces, I. Penuelas, J.M. Irache, R. Donnelly, C. Gamazo, Dissolving microneedles for intradermal vaccination against shigellosis. Vaccines. 7(4), 15 (2019). https://doi.org/10.3390/vaccines7040159
F. Perennes, B. Marmiroli, M. Matteucci, M. Tormen, L. Vaccari, E. Di Fabrizio, Sharp beveled tip hollow microneedle arrays fabricated by LIGA and 3D soft lithography with polyvinyl alcohol. J. Micromech. Microeng. 16(3), 473–479 (2006). https://doi.org/10.1088/0960-1317/16/3/001
S. Pradeep Narayanan, S. Raghavan, Solid silicon microneedles for drug delivery applications. Int. J. Adv. Manuf. Technol. 93(1), 407–422 (2017). https://doi.org/10.1007/s00170-016-9698-6
M.R. Prausnitz, R. Langer, Transdermal drug delivery. Nat. Biotechnol. 26(11), 1261–1268 (2008). https://doi.org/10.1038/nbt.1504
Z.F. Rad, R.E. Nordon, C.J. Anthony, L. Bilston, P.D. Prewett, J.Y. Arns, C.H. Arns, L.C. Zhang, G.J. Davies, High-fidelity replication of thermoplastic microneedles with open microfluidic channels. Microsyst. Nanoeng. 3, 11 (2017). https://doi.org/10.1038/micronano.2017.34
A.M. Rapoport, M. Ameri, H. Lewis, D.J. Kellerman, Development of a novel zolmitriptan intracutaneous microneedle system (Qtrypta (TM)) for the acute treatment of migraine. Pain. Manag. 10(6), 359–366 (2020). https://doi.org/10.2217/pmt-2020-0041
T.M. Rawson, S. Sharma, P. Georgiou, A. Holmes, A. Cass, D. O’Hare, Towards a minimally invasive device for beta-lactam monitoring in humans. Electrochem. Commun. 82, 1–5 (2017). https://doi.org/10.1016/j.elecom.2017.07.011
D. Resnik, M. Mozek, B. Pecar, A. Janez, V. Urbancic, C. Iliescu, D. Vrtacnik, In vivo experimental study of noninvasive insulin microinjection through hollow Si microneedle array. Micromachines. 9(1), 40 (2018). https://doi.org/10.3390/mi9010040
F. Ribet, G. Stemme, N. Roxhed, Real-time intradermal continuous glucose monitoring using a minimally invasive microneedle-based system. Biomed. Microdevices. 20(4) (2018). https://doi.org/10.1007/s10544-018-0349-6
N.G. Rouphael, M. Paine, R. Mosley, S. Henry, D.V. McAllister, H. Kalluri, W. Pewin, P.M. Frew, T. Yu, N.J. Thornburg, S. Kabbani, L. Lai, E.V. Vassilieva, I. Skountzou, R.W. Compans, M.J. Mulligan, M.R. Prausnitz, T.M.S. Grp, The safety, immunogenicity, and acceptability of inactivated influenza vaccine delivered by microneedle patch (TIV-MNP 2015): a randomised, partly blinded, placebo-controlled, phase 1 trial. Lancet. 390(10095), 649–658 (2017). https://doi.org/10.1016/s0140-6736(17)30575-5
A.H. Sabri, Z. Cater, J. Ogilvie, D.J. Scurr, M. Marlow, J. Segal, Characterisation of mechanical insertion of commercial microneedles. J. Drug. Deliv. Sci. Technol. 58 (2020). https://doi.org/10.1016/j.jddst.2020.101766
A. Sadeqi, H.R. Nejad, G. Kiaee, S. Sonkusale, Cost-effective fabrication of chitosan microneedles for transdermal drug delivery. Conf. Proc. Annu. Int. Conf. IEEE. Eng. Med. Biol. Soc. 2018, 5737–5740 (2018). https://doi.org/10.1109/embc.2018.8513691
F. Sammoura, J.J. Kang, Y.-M. Heo, T. Jung, L. Lin, Polymeric microneedle fabrication using a microinjection molding technique. Microsyst. Technol. Micro. Nanosyst. Inf. Storage. Process. Syst. 13(5–6), 517–522 (2007). https://doi.org/10.1007/s00542-006-0204-1
J. Saroia, Y.N. Wang, Q.H. Wei, M.J. Lei, X.P. Li, Y. Guo, K. Zhang, A review on 3D printed matrix polymer composites: its potential and future challenges. Int. J. Adv. Manuf. Technol. 106(5–6), 1695–1721 (2020). https://doi.org/10.1007/s00170-019-04534-z
H. Seddiqi, E. Oliaei, H. Honarkar, J. Jin, L.C. Geonzon, R.G. Bacabac, J. Klein-Nulend, Cellulose and its derivatives: towards biomedical applications. Cellulose. 28(4), 1893–1931 (2021). https://doi.org/10.1007/s10570-020-03674-w
S.A. Skoog, P.R. Miller, R.D. Boehm, A.V. Sumant, R. Polsky, R.J. Narayan, Nitrogen-incorporated ultrananocrystalline diamond microneedle arrays for electrochemical biosensing. Diamond. Relat. Mater. 54, 39–46 (2015). https://doi.org/10.1016/j.diamond.2014.11.016
R. Soltanzadeh, E. Afsharipour, C. Shafai, N. Anssari, B. Mansouri, Z. Moussavi, Molybdenum coated SU-8 microneedle electrodes for transcutaneous electrical nerve stimulation. Biomed. Microdevices. 20(1), 1 (2017). https://doi.org/10.1007/s10544-017-0241-9
R. Soltanzadeh, E. Afsharipour, C. Shafai, Investigation of transcutaneous electrical nerve stimulation improvements with microneedle array electrodes based on multiphysics simulation. Int. J. Numer. Method. Biomed. Eng. 36(3), e3318 (2020). https://doi.org/10.1002/cnm.3318
F. Tehrani, H. Teymourian, B. Wuerstle, J. Kavner, R. Patel, A. Furmidge, R. Aghavali, H. Hosseini-Toudeshki, C. Brown, F. Zhang, K. Mahato, Z. Li, A. Barfidokht, L. Yin, P. Warren, N. Huang, Z. Patel, P.P. Mercier, J. Wang, An integrated wearable microneedle array for the continuous monitoring of multiple biomarkers in interstitial fluid. Nat. Biomed. Eng. 6(11), 1214–1224 (2022). https://doi.org/10.1038/s41551-022-00887-1
H. Teymourian, F. Tehrani, K. Mahato, J. Wang, Lab under the skin: microneedle based wearable devices. Adv. Healthc. Mater. 10(17) (2021). https://doi.org/10.1002/adhm.202002255
R.R.S. Thakur, S.J. Fallows, H.L. McMillan, R.F. Donnelly, D.S. Jones, Microneedle- mediated intrascleral delivery of in situ forming thermoresponsive implants for sustained ocular drug delivery. J. Pharm. Pharmacol. 66(4), 584–595 (2014). https://doi.org/10.1111/jphp.12152
A. Trautmann, G.L. Roth, B. Nujiqi, T. Walther, R. Hellmann, Towards a versatile point-of-care system combining femtosecond laser generated microfluidic channels and direct laser written microneedle arrays. Microsyst. Nanoeng. 5, 9 (2019). https://doi.org/10.1038/s41378-019-0046-5
M.J. Uddin, N. Scoutaris, S.N. Economidou, C. Giraud, B.Z. Chowdhry, R.F. Donnelly, D. Douroumis, 3D printed microneedles for anticancer therapy of skin tumours. Mater. Sci. Eng. C. Mater. Biol. Appl. 107, 12 (2020). https://doi.org/10.1016/j.msec.2019.110248
A. Ullah, C.M. Kim, G.M. Kim, Porous polymer coatings on metal microneedles for enhanced drug delivery. R. Soc. Open. Sci. 5(4), 11 (2018). https://doi.org/10.1098/rsos.171609
D.S.S.M. Uppu, M.E. Turvey, A.R.M. Sharif, K. Bidet, Y. He, V. Ho, A.D. Tambe, J. Lescar, E.Y. Tan, K. Fink, J. Chen, P.T. Hammond, Temporal release of a three-component protein subunit vaccine from polymer multilayers. J. Control. Release. 317, 130–141 (2020). https://doi.org/10.1016/j.jconrel.2019.11.022
G. Valdes-Ramirez, Y.-C. Li, J. Kim, W. Jia, A.J. Bandodkar, R. Nunez-Flores, P.R. Miller, S.-Y. Wu, R. Narayan, J.R. Windmiller, R. Polsky, J. Wang, Microneedle-based self-powered glucose sensor. Electrochem. Commun. 47, 58–62 (2014). https://doi.org/10.1016/j.elecom.2014.07.014
K. van der Maaden, W. Jiskoot, J. Bouwstra, Microneedle technologies for (trans)dermal drug and vaccine delivery. J. Control. Release. 161(2), 645–655 (2012). https://doi.org/10.1016/j.jconrel.2012.01.042
M. Verhoeven, S. Bystrova, L. Winnubst, H. Qureshi, T.D. de Gruijl, R.J. Scheper, R. Luttge, Applying ceramic nanoporous microneedle arrays as a transport interface in egg plants and an ex-vivo human skin model. Microelectron. Eng. 98, 659–662 (2012). https://doi.org/10.1016/j.mee.2012.07.022
K.B. Vinayakumar, G.M. Hegde, M.M. Nayak, N.S. Dinesh, K. Rajanna, Fabrication and characterization of gold coated hollow silicon microneedle array for drug delivery. Microelectron. Eng. 128, 12–18 (2014). https://doi.org/10.1016/j.mee.2014.05.039
K.B. Vinayakumar, P.G. Kulkarni, M.M. Nayak, N.S. Dinesh, G.M. Hegde, S.G. Ramachandra, K. Rajanna, A hollow stainless steel microneedle array to deliver insulin to a diabetic rat. J. Micromech. Microeng. 26(6), 9 (2016a). https://doi.org/10.1088/0960-1317/26/6/065013
K.B. Vinayakumar, K. Rajanna, N.S. Dinesh, M.M. Nayak, Out-of-plane cup shaped stainless steel microneedle array for drug delivery. 2016 IEEE 11th Annual International Conference on Nano/Micro-Engineered and Molecular Systems. Sendai, IEEE (2016b), pp. 172–175.
L.K. Vora, A.J. Courtenay, I.A. Tekko, E. Larraneta, R.F. Donnelly, Pullulan-based dissolving microneedle arrays for enhanced transdermal delivery of small and large biomolecules. Int. J. Biol. Macromol. 146, 290–298 (2020). https://doi.org/10.1016/j.ijbiomac.2019.12.184
J.R. Windmiller, G. Valdes-Ramirez, N. Zhou, M. Zhou, P.R. Miller, C. Jin, S.M. Brozik, R. Polsky, E. Katz, R. Narayan, J. Wang, Bicomponent Microneedle Array Biosensor for Minimally-Invasive Glutamate Monitoring. Electroanalysis 23(10), 2302–2309. (2011). https://doi.org/10.1002/elan.201100361
M. Worgull, J.F. Hetu, K.K. Kabanemi, M. Heckele, Hot embossing of microstructures: characterization of friction during demolding. Microsyst. Technol. Micro Nanosyst. Inf. Storage. Process. Syst. 14(6), 767–773 (2008). https://doi.org/10.1007/s00542-007-0492-0
X. Wu, Y. Chen, S. Gui, X. Wu, L. Chen, Y. Cao, D. Yin, P. Ma, Sinomenine hydrochloride-loaded dissolving microneedles enhanced its absorption in rabbits. Pharm. Dev. Technol. 21(7), 787–793 (2016). https://doi.org/10.3109/10837450.2015.1055766
W. Wu, Y. Li, H. Wang, J. Cai, T. Lu, Y. He, Preparation of the blood extraction microneedle array based on the moving X-ray lithography. Microelectron. Tech. 55(9), 671–682 (2018)
X. Xie, C. Pascual, C. Lieu, S. Oh, J. Wang, B. Zou, J. Xie, Z. Li, J. Xie, D.C. Yeomans, M.X. Wu, X.S. Xie, Analgesic microneedle patch for neuropathic pain therapy. ACS. Nano. 11(1), 395–406 (2017). https://doi.org/10.1021/acsnano.6b06104
X.-X. Yan, X.-C. Shen, J.-Q. Liu, C.-S. Yang, Y.-G. Li, Out-of-plane hollow microneedles fabricated by combining silicon and non-silicon method. Nanotechnol. Precis. Eng. 9(6), 561–564 (2011)
X.X. Yan, G. Tang, R. Hu, B. Yang, L.L. Zhang, B. Xu, Analysis of process parameters and performance test for fabricating stainless-steel metal microneedles. Sens. Mater. 30(6), 1333–1340 (2018). https://doi.org/10.18494/sam.2018.1781
H. Yang, S. Kim, G. Kang, S.F. Lahiji, M. Jang, Y.M. Kim, J.-M. Kim, S.-N. Cho, H. Jung, Centrifugal lithography: self-shaping of polymer microstructures encapsulating biopharmaceutics by centrifuging polymer drops. Adv. Healthc. Mater. 6(19), 1700326 (2017). https://doi.org/10.1002/adhm.201700326
J. Yang, X. Liu, Y. Fu, Y. Song, Recent advances of microneedles for biomedical applications: drug delivery and beyond. Acta. Pharm. Sin. B 9(3), 469–483 (2019). https://doi.org/10.1016/j.apsb.2019.03.007
B. Yang, X. Fang, J. Kong, Engineered microneedles for interstitial fluid cell-free DNA capture and sensing using iontophoretic dual-extraction wearable patch. Adv. Func. Mater. 30(24), 2000591 (2020). https://doi.org/10.1002/adfm.202000591
Q. Yang, W. Zhong, L. Xu, H. Li, Q. Yan, Y. She, G. Yang, Recent progress of 3D-printed microneedles for transdermal drug delivery. Int. J. Pharm. 593, 60–69 (2021). https://doi.org/10.1016/j.ijpharm.2020.120106
W. Yao, D. Li, Y. Zhao, Z. Zhan, G. Jin, H. Liang, R. Yang, 3D printed multi-functional hydrogel microneedles based on high-precision digital light processing. Micromachines. 11(1), 31877987 (2019). https://doi.org/10.3390/mi11010017
J. Yu, J. Wang, Y. Zhang, G. Chen, W. Mao, Y. Ye, A.R. Kahkoska, J.B. Buse, R. Langer, Z. Gu, Glucose-responsive insulin patch for the regulation of blood glucose in mice and minipigs. Nat. Biomed. Eng. 4, 499–506 (2020). https://doi.org/10.1038/s41551-019-0508-y
H.F. Yun, J. Ling Liu, D.D. Zhu, Y.Y. Hao, X. Dong Guo, Multiscale simulations of drug distributions in polymer dissolvable microneedles. Colloids. Surf. B. Biointerfaces. 189, 110844 (2020). https://doi.org/10.1016/j.colsurfb.2020.110844
Z. Zhao, Y. Chen, Y. Shi, Microneedles: a potential strategy in transdermal delivery and application in the management of psoriasis. Rsc Advances 10(24), 14040–14049. (2020). https://doi.org/10.1039/d0ra00735h
H.H. Zhan, F.S. Ma, Y.C. Huang, J. Zhang, X.Y. Jiang, Y.C. Qian, Application of composite dissolving microneedles with high drug loading ratio for rapid local anesthesia. Eur. J. Pharm. Sci. 121, 330–337 (2018). https://doi.org/10.1016/j.ejps.2018.06.014
Y. Zhang, D. Wang, M. Gao, B. Xu, J. Zhu, W. Yu, D. Liu, G. Jiang, Separable microneedles for near-infrared light-triggered transdermal delivery of metformin in diabetic rats. ACS. Biomater. Sci. Eng. 4(8), 2879–2888 (2018). https://doi.org/10.1021/acsbiomaterials.8b00642
Y. Zhang, D. Chai, M. Gao, B. Xu, G. Jiang, Thermal ablation of separable microneedles for transdermal delivery of metformin on diabetic rats. Int. J. Polym. Mater. Polym. Biomater. 68(14), 850–858 (2019). https://doi.org/10.1080/00914037.2018.1517347
M. Zheng, Z. Wang, H. Chang, L. Wang, S.W.T. Chew, D.C.S. Lio, M. Cui, L. Liu, B.C.K. Tee, C. Xu, Osmosis-powered hydrogel microneedles for microliters of skin interstitial fluid extraction within minutes. Adv. Healthc. Mater. 9(10), 1901683 (2020). https://doi.org/10.1002/adhm.201901683
Y. Zheng, R. Omar, R. Zhang, N. Tang, M. Khatib, Q. Xu, Y. Milyutin, W. Saliba, Y.Y. Broza, W. Wu, M. Yuan, H. Haick, A wearable microneedle-based extended gate transistor for real-time detection of sodium in interstitial fluids. Adv. Mater. 34(10), 2108607 (2022). https://doi.org/10.1002/adma.202108607
J. Zhuang, S. Chen, H. Xu, Y. Liu, Y. Huang, D. Wu, Study on process parameters of micro-injection compression molding for microneedles with flexible substrate. China. Plast. 32(12), 80–85 (2018)
Funding
This research was funded by grants from National High Level Hospital Clinical Research Funding (High Quality Clinical Research Project of Peking University First Hospital, No. 2022CR83), National Natural Science Foundation of China (No. 52072007, and No. 82130021), National Key R&D Program of China (No. 2018YFB1307301, and No. 2022YFB3204400), Beijing Young Scientist Program (No. BJJWZYJH01201910001006), CAMS Innovation Fund for Medical Sciences (No. 2019-I2M-5-046, and No. 2020-JKCS-009), PKU-Baidu Fund (No. 2020BD026, and No. 2020BD044), and Capital's Funds for Health Improvement and Research (No. CFH2022-1-4071).
Author information
Authors and Affiliations
Contributions
The manuscript was written through contributions of all au-thors. All authors have given approval to the final version of the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luo, X., Yang, L. & Cui, Y. Microneedles: materials, fabrication, and biomedical applications. Biomed Microdevices 25, 20 (2023). https://doi.org/10.1007/s10544-023-00658-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s10544-023-00658-y