Abstract
The objective of this study is to propose a unified, continuous, and bodyweight-only equation to quantify the changes of human basal metabolic rate (BMR), glomerular filtration rate (GFR), and drug clearance (CL) from infancy to adulthood. The BMR datasets were retrieved from a comprehensive historical database of male and female subjects (0.02 to 64 years). The CL datasets for 17 drugs and the GFR dataset were generated from published maturation and growth models with reported parameter values. A statistical approach was used to simulate the model-generated CL and GFR data for a hypothetical population with 26 age groups (from 0 to 20 years). A biphasic equation with two power-law functions of bodyweight was proposed and evaluated as a general model using nonlinear regression and dimensionless analysis. All datasets universally reveal biphasic curves with two distinct linear segments on log–log plots. The biphasic equation consists of two reciprocal allometric terms that asymptotically determine the overall curvature. The fitting results show a superlinear scaling phase (asymptotic exponent >1; ca. 1.5–3.5) and a sublinear scaling phase (asymptotic exponent <1; ca. 0.5–0.7), which are separated at the phase transition bodyweight ranging from 5 to 20 kg with a mean value of 10 kg (corresponding to 1 year of age). The dimensionless analysis generalizes and offers quantitative realization of the maturation and growth process. In conclusion, the proposed mixed-allometry equation is a generic model that quantitatively describes the phase transition in the human maturation process of diverse human functions.
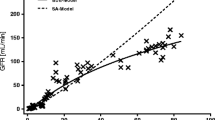
Graphical Abstract










Similar content being viewed by others
References
Kuzawa CW, Chugani HT, Grossman LI, Lipovich L, Muzik O, Hof PR, Wildman DE, Sherwood CC, Leonard WR, Lange N. Metabolic costs and evolutionary implications of human brain development. Proc Natl Acad Sci. 2014;111(36):13010–5.
Pontzer H, Brown MH, Raichlen DA, Dunsworth H, Hare B, Walker K, Luke A, Dugas LR, Durazo-Arvizu R, Schoeller D. Metabolic acceleration and the evolution of human brain size and life history. Nature. 2016;533(7603):390–2.
Tegenge MA, Mahmood I. Age-and bodyweight-dependent allometric exponent model for scaling clearance and maintenance dose of theophylline from neonates to adults. Ther Drug Monit. 2018;40(5):635–41.
Bowes HM, Burdon CA, Taylor NA. The scaling of human basal and resting metabolic rates. Eur J Appl Physiol. 2021;121(1):193–208.
O’flaherty EJ. Physiologic changes during growth and development. Environ Health Perspect. 1994;102(suppl 11):103–6.
Mahmood I, Staschen C-M. Prediction of human glomerular filtration rate from preterm neonates to adults: evaluation of predictive performance of several empirical models. AAPS J. 2016;18(2):445–54.
Hayton WL. Maturation and growth of renal function: dosing renally cleared drugs in children. AAPS PharmSci. 2000;2(1):22–8.
Calvier E, Krekels E, Johnson T, Rostami-Hodjegan A, Tibboel D, Knibbe CA. Scaling drug clearance from adults to the young children for drugs undergoing hepatic metabolism: a simulation study to search for the simplest scaling method. AAPS J. 2019;21(3):1–11.
Klingenberg CP. Heterochrony and allometry: the analysis of evolutionary change in ontogeny. Biol Rev. 1998;73(1):79–123.
Glazier DS. Beyond the ‘3/4-power law’: variation in the intra-and interspecific scaling of metabolic rate in animals. Biol Rev. 2005;80(4):611–62.
Glazier DS. Is metabolic rate a universal ‘pacemaker’ for biological processes? Biol Rev. 2015;90(2):377–407.
Mori S, Yamaji K, Ishida A, Prokushkin SG, Masyagina OV, Hagihara A, Hoque AR, Suwa R, Osawa A, Nishizono T. Mixed-power scaling of whole-plant respiration from seedlings to giant trees. Proc Natl Acad Sci. 2010;107(4):1447–51.
DeLong JP, Okie JG, Moses ME, Sibly RM, Brown JH. Shifts in metabolic scaling, production, and efficiency across major evolutionary transitions of life. Proc Natl Acad Sci. 2010;107(29):12941–5.
Germovsek E, Barker CI, Sharland M, Standing JF. Scaling clearance in paediatric pharmacokinetics: all models are wrong, which are useful? Br J Clin Pharmacol. 2017;83(4):777–90.
Holford N, Heo Y-A, Anderson B. A pharmacokinetic standard for babies and adults. J Pharm Sci. 2013;102(9):2941–52.
Wang C, Peeters MY, Allegaert K, van Oud-Alblas HJB, Krekels EH, Tibboel D, Danhof M, Knibbe CA. A bodyweight-dependent allometric exponent for scaling clearance across the human life-span. Pharm Res. 2012;29(6):1570–81.
Mahmood I. Prediction of drug clearance in children from adults: a comparison of several allometric methods. Br J Clin Pharmacol. 2006;61(5):545–57.
Henry C. Basal metabolic rate studies in humans: measurement and development of new equations. Public Health Nutr. 2005;8(7a):1133–52.
EFSA Panel on Dietetic Products N & Allergies. Scientific opinion on nutrient requirements and dietary intakes of infants and young children in the European Union. EFSA J. 2013;11(10):3408.
Oussaada SM, van Galen KA, Cooiman MI, Kleinendorst L, Hazebroek EJ, van Haelst MM, Ter Horst KW, Serlie MJ. The pathogenesis of obesity. Metabolism. 2019;92:26–36.
Kliemann N, Murphy N, Viallon V, Freisling H, Tsilidis KK, Rinaldi S, Mancini FR, Fagherazzi G, Boutron-Ruault MC, Boeing H. Predicted basal metabolic rate and cancer risk in the European Prospective Investigation into Cancer and Nutrition. Int J Cancer. 2020;147(3):648–61.
Den Broeder E, Oeseburg B, Lippens R, Van Staveren W, Sengers R, van’t Hof M, Tolboom J. Basal metabolic rate in children with a solid tumour. Eur J Clin Nutr. 2001;55(8):673–81.
WHO (2004) Human energy requirements: report of a joint FAO/WHO/UNU expert consultation: Rome, 17-24 October 2001 (Food & Agriculture Org.).
Rhodin MM, Anderson BJ, Peters AM, Coulthard MG, Wilkins B, Cole M, Chatelut E, Grubb A, Veal GJ, Keir MJ. Human renal function maturation: a quantitative description using weight and postmenstrual age. Pediatr Nephrol. 2009;24(1):67–76.
Liu T, Ghafoori P, Gobburu JV. Allometry is a reasonable choice in pediatric drug development. J Clin Pharmacol. 2017;57(4):469–75.
Strougo A, Eissing T, Yassen A, Willmann S, Danhof M, Freijer J. First dose in children: physiological insights into pharmacokinetic scaling approaches and their implications in paediatric drug development. J Pharmacokinet Pharmacodyn. 2012;39(2):195–203.
Brussee JM, Krekels EH, Calvier EA, Palić S, Rostami-Hodjegan A, Danhof M, Barrett JS, de Wildt SN, Knibbe CA. A pediatric covariate function for CYP3A-mediated midazolam clearance can scale clearance of selected CYP3A substrates in children. AAPS J. 2019;21(5):1–11.
Wang C, Allegaert K, Peeters MY, Tibboel D, Danhof M, Knibbe CA. The allometric exponent for scaling clearance varies with age: a study on seven propofol datasets ranging from preterm neonates to adults. Br J Clin Pharmacol. 2014;77(1):149–59.
Björkman S. Prediction of drug disposition in infants and children by means of physiologically based pharmacokinetic (PBPK) modelling: theophylline and midazolam as model drugs. Br J Clin Pharmacol. 2005;59(6):691–704.
Calvier EA, Krekels EH, Välitalo PA, Rostami-Hodjegan A, Tibboel D, Danhof M, Knibbe CA. Allometric scaling of clearance in paediatric patients: when does the magic of 0.75 fade? Clin Pharmacokinet. 2017;56(3):273–85.
Colin PJ, Allegaert K, Thomson AH, Touw DJ, Dolton M, de Hoog M, Roberts JA, Adane ED, Yamamoto M, Santos-Buelga D. Vancomycin pharmacokinetics throughout life: results from a pooled population analysis and evaluation of current dosing recommendations. Clin Pharmacokinet. 2019;58(6):767–80.
Wu Q, Peters SA. A retrospective evaluation of allometry, population pharmacokinetics, and physiologically-based pharmacokinetics for pediatric dosing using clearance as a surrogate. CPT Pharmacometrics Syst Pharmacol. 2019;8(4):220–9.
Mahmood I, Staschen C-M, Goteti K. Prediction of drug clearance in children: an evaluation of the predictive performance of several models. AAPS J. 2014;16(6):1334–43.
van Groen BD, Pilla Reddy V, Badée J, Olivares-Morales A, Johnson TN, Nicolaï J, Annaert P, Smits A, de Wildt SN, Knibbe CA. Pediatric pharmacokinetics and dose predictions: a report of a satellite meeting to the 10th Juvenile Toxicity Symposium. Clinical and Translational Science. 2021;14(1):29–35.
Foissac F, Bouazza N, Valade E, De Sousa MM, Fauchet F, Benaboud S, Hirt D, Tréluyer JM, Urien S. Prediction of drug clearance in children. J Clin Pharmacol. 2015;55(7):739–47.
Lonsdale DO, Baker EH, Kipper K, Barker C, Philips B, Rhodes A, Sharland M, Standing JF. Scaling beta-lactam antimicrobial pharmacokinetics from early life to old age. Br J Clin Pharmacol. 2019;85(2):316–46.
Anderson BJ, Holford NH. Mechanistic basis of using body size and maturation to predict clearance in humans. Drug metabolism and pharmacokinetics. 2009;24(1):25–36.
Krekels EHJ, Calvier EAM, van der Graaf PH, Knibbe CAJ. Children are not small adults, but can we treat them as such? CPT Pharmacometrics Syst Pharmacol. 2019;8(1):34–8.
Mansoor N, Ahmad T, Khan RA, Sharib SM, Mahmood I. Prediction of clearance and dose of midazolam in preterm and term neonates: a comparative study between allometric scaling and physiologically based pharmacokinetic modeling. Am J Ther. 2019;26(1):e32–7.
Shimamura K, Wajima T, Yano Y. Pharmacokinetic prediction for intravenous β-lactam antibiotics in pediatric patients. J Pharm Sci. 2007;96(11):3125–39.
Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1985;39:5–41.
Anderson BJ, Holford NH. Mechanism-based concepts of size and maturity in pharmacokinetics. Annu Rev Pharmacol Toxicol. 2008;48:303–32.
WHO (1985) Energy and protein requirements: report of a Joint FAO/WHO/UNU Expert Consultation [held in Rome from 5 to 17 October 1981] (World Health Organization).
Lacey L, Keene O, Pritchard J, Bye A. Common noncompartmental pharmacokinetic variables: are they normally or log-normally distributed? J Biopharm Stat. 1997;7(1):171–8.
Gualandi S, Toscani G. Human behavior and lognormal distribution. A kinetic description. Mathematical Models and Methods in Applied Sciences. 2019;29(04):717–53.
Daly L, Bourke GJ. Interpretation and uses of medical statistics: (John Wiley & Sons); 2008.
Kirkwood TB (1979) Geometric means and measures of dispersion. Biometrics:908-909.
Hayton WL, Kneer J, de Groot R, Stoeckel K. Influence of maturation and growth on cefetamet pivoxil pharmacokinetics: rational dosing for infants. Antimicrob Agents Chemother. 1996;40(3):567–74.
Hayton W, Walstad R, Thurmann-Nielsen E, Kufaas T, Kneer J, Ambros R, Rugstad H, Monn E, Bodd E, Stoeckel K. Pharmacokinetics of intravenous cefetamet and oral cefetamet pivoxil in children. Antimicrob Agents Chemother. 1991;35(4):720–5.
Koup JR, Dubach U, Brandt R, Wyss R, Stoeckel K. Pharmacokinetics of cefetamet (Ro 15-8074) and cefetamet pivoxil (Ro 15-8075) after intravenous and oral doses in humans. Antimicrob Agents Chemother. 1988;32(4):573–9.
Kneer J, Tam Y, Blouin R, Frey F, Keller E, Stathakis C, Luginbuehl B, Stoeckel K. Pharmacokinetics of intravenous cefetamet and oral cefetamet pivoxil in patients with renal insufficiency. Antimicrob Agents Chemother. 1989;33(11):1952–7.
Rubin MI, Bruck E, Rapoport M, Snively M, McKay H, Baumler A. Maturation of renal function in childhood: clearance studies. J Clin Investig. 1949;28(5):1144–62.
Bogin B. Patterns of human growth: (Cambridge University Press); 2020.
Holliday M (1971) Metabolic rate and organ size during growth from infancy to maturity and during late gastation and early infancy. Pediatrics 47(1):Suppl 2: 169+-Suppl 162: 169+.
West GB, Brown JH, Enquist BJ. A general model for ontogenetic growth. Nature. 2001;413(6856):628–31.
Sumpter AL, Holford NH. Predicting weight using postmenstrual age–neonates to adults. Pediatr Anesth. 2011;21(3):309–15.
Meibohm B, Läer S, Panetta JC, Barrett JS. Population pharmacokinetic studies in pediatrics: issues in design and analysis. AAPS J. 2005;7(2):E475–87.
Tod M, Jullien V, Pons G. Facilitation of drug evaluation in children by population methods and modelling. Clin Pharmacokinet. 2008;47(4):231–43.
Chen N, Aleksa K, Woodland C, Rieder M, Koren G. Ontogeny of drug elimination by the human kidney. Pediatr Nephrol. 2006;21(2):160–8.
Edginton AN, Schmitt W, Voith B, Willmann S. A mechanistic approach for the scaling of clearance in children. Clin Pharmacokinet. 2006;45(7):683–704.
Johnson TN, Rostami-Hodjegan A, Tucker GT. Prediction of the clearance of eleven drugs and associated variability in neonates, infants and children. Clin Pharmacokinet. 2006;45(9):931–56.
Edginton AN, Schmitt W, Willmann S. Development and evaluation of a generic physiologically based pharmacokinetic model for children. Clin Pharmacokinet. 2006;45(10):1013–34.
Alcorn J, McNamara PJ. Ontogeny of hepatic and renal systemic clearance pathways in infants part I. Clin Pharmacokinet. 2002;41(12):959–98.
Alcorn J, McNamara PJ. Ontogeny of hepatic and renal systemic clearance pathways in infants: part II. Clin Pharmacokinet. 2002;41(13):1077–94.
Allegaert K, van den Anker JN, Naulaers G, de Hoon J. Determinants of drug metabolism in early neonatal life. Curr Clin Pharmacol. 2007;2(1):23–9.
Anderson GD (2010) Developmental pharmacokinetics. Seminars in Pediatric Neurology, (Elsevier), pp 208-213.
Hines RN, McCarver DG. The ontogeny of human drug-metabolizing enzymes: phase I oxidative enzymes. J Pharmacol Exp Ther. 2002;300(2):355–60.
McCarver DG, Hines RN. The ontogeny of human drug-metabolizing enzymes: phase II conjugation enzymes and regulatory mechanisms. J Pharmacol Exp Ther. 2002;300(2):361–6.
Holliday M, Potter D, Jarrah A, Bearg S. The relation of metabolic rate to body weight and organ size. Pediatr Res. 1967;1(3):185–95.
Wang C, Sadhavisvam S, Krekels EH, Dahan A, Tibboel D, Danhof M, Vinks AA, Knibbe CA. Developmental changes in morphine clearance across the entire paediatric age range are best described by a bodyweight-dependent exponent model. Clinical Drug Investigation. 2013;33(7):523–34.
Bartelink I, Boelens JJ, Bredius RG, Egberts AC, Wang C, Bierings MB, Shaw PJ, Nath CE, Hempel G, Zwaveling J. Body weight-dependent pharmacokinetics of busulfan in paediatric haematopoietic stem cell transplantation patients. Clin Pharmacokinet. 2012;51(5):331–45.
Mahmood I, Tegenge M. A bodyweight-dependent allometric exponent model for scaling clearance of clotting factor VIII and IX from infants to adults. Haemophilia. 2016;22(6):e570–3.
Mahmood I, Tegenge MA. A comparative study between allometric scaling and physiologically based pharmacokinetic modeling for the prediction of drug clearance from neonates to adolescents. J Clin Pharmacol. 2019;59(2):189–97.
Holford N. Dosing in children. Clinical Pharmacology & Therapeutics. 2010;87(3):367–70.
Mahmood I. Dosing in children: a critical review of the pharmacokinetic allometric scaling and modelling approaches in paediatric drug development and clinical settings. Clin Pharmacokinet. 2014;53(4):327–46.
Barrett JS, Barrett RF, Vinks AA. Status toward the implementation of precision dosing in children. J Clin Pharmacol. 2021;61:S36–51.
Anderson BJ, Holford NH. Understanding dosing: children are small adults, neonates are immature children. Arch Dis Child. 2013;98(9):737–44.
Jotterand Chaparro C, Moullet C, Taffé P, Laure Depeyre J, Perez MH, Longchamp D, Cotting J. Estimation of resting energy expenditure using predictive equations in critically ill children: results of a systematic review. J Parenter Enter Nutr. 2018;42(6):976–86.
Müller MJ, Geisler C, Hübers M, Pourhassan M, Braun W, Bosy-Westphal A. Normalizing resting energy expenditure across the life course in humans: challenges and hopes. Eur J Clin Nutr. 2018;72(5):628–37.
Fuentes-Servín J, Avila-Nava A, González-Salazar LE, Pérez-González OA, Servín-Rodas MDC, Serralde-Zuñiga AE, Medina-Vera I, & Guevara-Cruz M (2021) Resting energy expenditure prediction equations in the pediatric population: a systematic review. Frontiers in Pediatrics 9.
Funding
The author is supported by the Ministry of Science and Technology (MOST) and Higher Education Sprout Project — Ministry of Education (MOE), Taiwan.
Author information
Authors and Affiliations
Contributions
Teh-Min Hu is the sole author who contributes to the conception of the work and acquisition, analysis, and interpretation of data and performs modeling and simulation, derivations of equations, and writing, revising, and submitting the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The author declares no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
APPENDIX
Characteristics of the Biphasic Model
This study proposes a mixed-power function (the biphasic allometry model) (Equation 4) to scale human BMR, GFR, and drug CL from adults to neonates. In fact, this study was inspired by allometric scaling of whole-plant respiration from small seedlings to giant trees (12). Equation 4 states that the reciprocal of a physiological or metabolic parameter (P) is equal to the sum of reciprocals of each of two individual power-law bodyweight functions (i.e., allometric functions). To understand the key features of the model, a simulation was conducted to characterize the mixed-power function. The following hypothetical parameters were used: A = 0.1, B = 10, α= 2.5, and β= 0.5. By plugging the parameter values into Equation 4, a set of hypothetical (P, W) data was generated for a simulated bodyweight range of 3–70 kg (at a 1-kg interval). Figure 10A shows the simulated data and two asymptotic lines on log–log coordinates. Let P1 and P2 be the first and second asymptotic functions, respectively, and then the asymptotic bodyweight functions are
and Equation 4 can be expressed as
when P1 ≪ P2, P ≈ P1, which is the first asymptote near the low bodyweight region of W ≪ (B/A)1/(α − β) (by solving the inequality relationship). In contrast, when P1 ≫ P2, P ≈ P2, the second asymptote occurs at W ≫ (B/A)1/(α − β). Thus, the characteristic bodyweight (\(\overset{\sim }{w}\)) is revealed as
Mathematically, \(\overset{\sim }{w}\) is exactly the bodyweight at which the two asymptotic lines intersect (P1 = P2 and \(A{\overset{\sim }{w}}^{\alpha }=B{\overset{\sim }{w}}^{\beta }\)). Biologically, it is considered here as the critical bodyweight at which the body undergoes transition from maturation phase to growth phase (i.e., the phase transition bodyweight). By taking the derivative of Equation 4, the following expression for the slope (S) of the biphasic curve is obtained:
Therefore, according to Equation 27, the slope of the biphasic model can be estimated at any given bodyweight. Figure 10B shows that the slope decreases with increasing bodyweight. The slope curve is indeed flanked by two asymptotic lines: slope ≈ α, at the low body weight region where \(W\ll \overset{\sim }{w}\) or when P1 ≪ P2; whereas slope ≈ β, at \(W\gg \overset{\sim }{w}\) or when P1 ≫ P2. Note that the characteristic slope (S*) at the phase transition bodyweight is exactly the mean of the two asymptotic exponents, since at \(W=\overset{\sim }{w}\), P1 = P2, Equation 27 is reduced to
In sum, Fig. 10 captures the essence of the proposed mixed-allometry model by revealing all the parameter values used for the simulation: two asymptotic exponents of 2.5 and 0.5 (exactly α and β), two asymptotic allometric coefficients (A = 0.1, B = 10), and a critical bodyweight of 10 kg (i.e.,\(\overset{\sim }{w}={\left(B/A\right)}^{1/\left(\alpha -\beta \right)}={\left(10/0.1\right)}^{1/2}\)) where the slope of the biphasic curve at this critical point is exactly the mean of the two exponents (i.e., 1.5).
Characteristics of the mixed-power function. A Simulated data of physiological quantity (P) vs. bodyweight (W). The lines represent the two asymptotic power-law functions with respective y-intercepts (i.e., 0.1 and 10, at W = 1 kg) and an interception point which defines the critical point of phase transition (at W = 10 kg). B Slope as a function of bodyweight. The plot highlights the two allometric exponents (α and β) and the corresponding mean value at the point of phase transition
Rights and permissions
About this article
Cite this article
Hu, TM. A General Biphasic Bodyweight Model for Scaling Basal Metabolic Rate, Glomerular Filtration Rate, and Drug Clearance from Birth to Adulthood. AAPS J 24, 67 (2022). https://doi.org/10.1208/s12248-022-00716-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-022-00716-y