Abstract
Introduction
Angiomatous polyp is a benign, non-neoplastic variant of antrochoanal polyp that is extremely uncommon.
Objectives
Reviewing the prevalence, clinical characteristics, preoperative assessment, histology, and treatment of angiomatous antrochoanal polyps.
Methods
All patients presented with antrochoanal polyps accompanied by epistaxis during the period from 2012 to 2022 were included in the study. Based on a detailed history, clinical examination, findings of nasal endoscopy, radiological examination (CT scan nose and paranasal sinuses), and intraoperative data. A histopathological examination for the polyp biopsy specimens was done for all patients presented with epistaxis.
Results
Over 10 years, among 94 patients with lesions that met the diagnostic criteria for antrochoanal polyp, 16 patients (17%) presented with recurrent ipsilateral epistaxis. All lesions were unilateral, 9 on the right side and 7 on the left side, with no affection of the contralateral sinonasal cavity. Clinical, radiological, and histopathological examinations showed a picture suggestive of an angiomatous antrochoanal polyp. Endoscopic sinus surgery under general anesthesia was performed and no recurrence was detected in the patients with angiomatous antrochoanal polyps.
Conclusion
It seems that epistaxis exclusively occurs in the angiomatous variety of the antrochoanal polyp. This polyp is not only a variation of the common antrochoanal polyp but rather a unique variety. The identification of the distinctive physical characteristics of an angiomatous antrochoanal polyp will aid in avoiding the incorrect diagnosis of a vascular tumor and the need for unnecessary surgery.
Similar content being viewed by others
Background
Sinochoanal polyps (SCPs) develop from the paranasal sinuses or the nasal cavity and reach the nasopharynx through the choana [1]. Antrochoanal polyps (ACP), which grow from the mucosa of the maxillary sinus and spread into the choana through the maxillary sinus ostium, are the most common type of sinochoanal polyps (SCPs) [2, 3].
A very uncommon variety of antrochoanal polyps is the benign, non-neoplastic lesion known as the angiomatous antrochoanal polyp (AACP) [4]. It also is known as an “angiectatic polyp,” and it is distinguished by significant vascular proliferation, angiectasis, and regions that are vulnerable to vascular compromise, leading to venous stasis, thrombosis, and infarction [5]. Only 4–5% of all sinonasal polyps (SNPs) are angiomatous nasal polyps (ANPs), which are extremely uncommon [6]. Nasal obstruction and epistaxis are the most typical manifestations of AACPs [7].
These lesions have a high risk of being mistaken for neoplastic processes such as juvenile angiofibroma, inverted papilloma, hemangioma, and even malignant sinonasal tumors due to their clinical and radiological characteristics [8]. Computed tomography (CT) scans and a nasal endoscopy are necessary for diagnosis and therapy planning. The preferred course of treatment is thought to be endoscopic surgical excision with sinus drainage restoration [6, 7, 9].
The goal of this study is to reviewing the prevalence, clinical characteristics, preoperative assessment, histology, and treatment of angiomatous ACPs.
Methods
This retrospective study was conducted at Sohag University Hospital, otorhinolaryngology department. The local ethical committee approved the study with No. Soh-Med-23-01-38. Written informed consent for publication of their clinical details was obtained from the participants (or from their parent or legal guardian in the case of children under 16). Ninety-four patients presented to the ENT outpatient clinic with lesions that met the diagnostic criteria for antrochoanal polyp during the period from 2012 to 2022 and they were operated on by endoscopic sinus surgery. Patients presented with antrochoanal polyps accompanied by epistaxis and diagnosed to have angiomatous antrochoanal polyps were included in the study. Previously operated or recurrent cases were excluded from the study.
Revision of the presenting symptoms, history, details of clinical examination, findings of nasal endoscopy, details of radiological examination (CT scan nose and paranasal sinuses), and intraoperative data was done. Endoscopic sinus surgery under general anesthesia was performed for all patients with the same surgeon. A histopathological examination for the polyp biopsy specimens was done for all patients presented with epistaxis.
Statistical analysis was performed by SPSS software (version 17). Continuous variables are presented as mean ± SD, and categorical variables are presented as absolute numbers and percentages. Categorical variables were analyzed using the chi-square test or Fisher’s exact test as appropriate. Statistical significance was defined as a P value < 0.05.
Results
Ninety-four patients were encountered between January 2012 and January 2022 who had lesions that fulfilled the diagnostic criteria for antrochoanal polyps. In 16 patients (16/94; 17%), recurrent ipsilateral epistaxis was the primary symptom, which was initially thought to be a vascular nasal tumor.
Their ages ranged from 8 to 43 years, with a mean age of 20.3 years, and the male/ female ratio was 7/9. All lesions were unilateral, nine on the right side and seven on the left side, with no affection of the contralateral sinonasal cavity. In addition to unilateral recurrent epistaxis as a presenting symptom in all 16 (100%) patients, the patients also presented with nasal obstruction in 15 cases (93.75%) and rhinorrhea in 13 cases (81.25%). The symptoms ranged from four to 8 months in duration as shown in Table 1.
However, clinical presentation, preoperative endoscopic examination, and intraoperative endoscopic examination under general anesthesia revealed a unilateral polypoid mass that satisfied the diagnostic criteria of antrochoanal polyp; in addition, these lesions had a reddish, vascular surface in parts (Fig. 1A, B).
A A photograph of a freshly resected angiomatous ACP displaying a reddish, vascular surface in some parts (Vs) and a pale surface in others. B A photograph of a bisected angiomatous ACP to demonstrate a highly vascular cut surface (Vs). Note the well-defined, narrow pedicle (P) in both specimens. C Light microscopy of an angiomatous ACP shows the highly vascular stroma with multiple dilated vascular spaces of varying size (black arrows) (H&E; Â100). D Higher magnification shows that these vascular spaces are lined by a single layer of flat endothelial cells (black arrows) and separated by loose fibro-connective stroma that exhibited chronic inflammatory cellular infiltration and areas of interstitial hemorrhage (H&E; Â200)
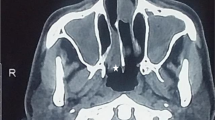
CT scan of the nose and paranasal sinuses revealed a polypoidal mass arising from the maxillary sinus with involvement of the osteomeatal complex, filling the ipsilateral nasal cavity and extending posteriorly to the nasopharynx through the choana (Fig. 2).
The mass was heterogeneous in density with the remodeling of bone. No bony destruction was detected in any patient. A contrast-enhanced CT scan of the nose & PNS revealed minimal enhancement of the mass without pterygopalatine fossa involvement (Fig. 3).
Endoscopic sinus surgery with a middle meatal antrostomy to remove the polyp and restore optimal sinus function was performed in all cases. Polyps revealed a tendency to bleed on touching. The polyp biopsy specimens from the patients presented with epistaxis were sent for histopathological examination. The pathology reports of these biopsies showed a highly vascular stroma with multiple dilated blood vessels, separated by loose fibro-connective stroma that exhibited chronic inflammatory cellular infiltration, mostly plasma cells, with thrombi at different stages of development, a picture suggestive of an angiomatous antrochoanal polyp (AACP) (Fig. 1C, D).
Postoperatively, follow-up of the patients for at least 12 months was done, and the preoperative symptoms were improved, No recurrence was detected in the patients with angiomatous antrochoanal polyps (AACPs).
Discussion
Sinonasal polyps (SNPs) have been divided into five kinds based on the main characteristics observed during histological evaluation: edematous, glandular, fibrous, cystic, and angiomatous 10. Only 4–5% of all SNPs are angiomatous nasal polyps (ANPs), which are extremely uncommon. ANPs can develop quickly and show violent clinical presentations that can mimic [6].
Angiomatous antrochoanal polyps (AACPs) are fibrosed, vascularized nasal polyps, probably a response to a minor trauma [9]. Although various theories have been given, the precise etiology of AACPs is still unknown. According to the most widely accepted theories, there are many places where the sinonasal polyps are more susceptible to vascular compromise or constriction. These sensitive regions include the most dependent component of the nasopharyngeal polyp, the posterior end of the inferior turbinate, the choana, and the maxillary sinus ostium [5]. Vascular dilatation, stasis, edema, and ischemia of the polyp occur as a result of the vessels being compressed. Additionally, this may result in thrombosis, venous infarction, and subsequently neovascularization and fibrosis of the polyp [4, 8, 10], for which the name “angiomatous” was proposed. The gradual growth and localized bone degradation linked to ANPs are also explained by this process [7].
It is highly unusual for an antrochoanal nasal polyp to manifest with considerable epistaxis [11]. In our study, unilateral recurrent epistaxis was a presenting symptom in all 16 (100%) patients. The patients also presented with nasal obstruction in 15 cases (93.75%) and rhinorrhea in 13 cases (81.25%).
Histopathological examination of AACPs showed a highly vascular stroma with multiple dilated blood vessels, separated by loose fibro-connective stroma that exhibited chronic inflammatory cellular infiltration, mostly plasma cells, with thrombi at different stages of development. The same microscopic picture is reported in the literature [11, 12].
AACPs are more difficult to be radiologically differentiated due to their non-specific CT findings. There is an expanding mass coming from the maxillary sinus, the osteomeatal complex is involved, the nasal cavity is completely obstructed, the mass extends posteriorly to the nasopharynx through the choana, and the bony walls are destroyed and remodeled. Contrast-enhanced CT scans may show angiomatous polyps as non-enhancing or minimally enhancing nasal vault masses without pterygopalatine fossa involvement [7, 10, 11, 13]. The same picture was detected with our patients with AACPs but without bony destruction.
The clinical and imaging characteristics of AACPs might mimic neoplastic lesions such as malignant sinonasal tumors, inverted papillomas, juvenile angiofibromas, and hemangiomas [8]. This should trigger an additional histological and radiological investigation and allow for an appropriate diagnosis.
Embolization just before surgery is not required for the treatment of angiomatous ACPs. The removal of a nasopharyngeal angiofibroma, in contrast, necessitates preoperative embolization since there may be significant intraoperative bleeding. Angiomatous ACPs appear to have fewer feeding arteries on angiography than nasopharyngeal angiofibroma, which has a rich, irregular vascular supply. This is explained by the aberrant configurations of dilated capillary-type vasculature and newly endothelialized voids with endoluminal thrombosis present in angiomatous ACPs instead of the typical arborizing vascularity pattern [14].
The preferred treatment option is transnasal endoscopic surgical excision of AACPs with the restoration of sinus drainage. It is proved to be more feasible and effective with short recovery time and very rare recurrence rates [6, 13, 15, 16]. In our research, all patients had angiomatous polyps that began in the maxillary sinus, and spread into the nasal cavity, reaching the nasopharynx through the choana with complete excision of the polyp and its connection is required to reduce regrowth. Additionally, all of the patients had sinus expansion with no bony destruction. All patients underwent transnasal endoscopic sinus surgery with the removal of the antral part. The polyp is fragile during removal. The fragility of the AACP is due to infarction, and hence it is difficult to remove them en bloc [17].
Regular post-operative follow-up was recommended to diagnose a possible recurrence. In our study, no recurrence was detected after a follow-up of the patients with AACPs for at least 12 months without other complications.
The study included a number of limitations. First, the study is being a retrospective and a small sample size. Second, no control group with other disorders was present to confirm the unique characteristics of SAP. Third, while our findings indicate that CT may help with SAP diagnosis, it lacked information from MRI, which is thought to display distinguishing characteristics.
Conclusion
It seems that epistaxis exclusively occurs in the angiomatous variety of antrochoanal polyps. This polyp is not only a variation of the common antrochoanal polyp but rather a unique variety. The identification of the distinctive physical characteristics of an angiomatous antrochoanal polyp will aid in avoiding the incorrect diagnosis of a vascular tumor and the need for unnecessary surgery.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Lessa MM, Voegels RL, Pádua F, Wiikmann C, Romano FR, Butugan O (2002) Sphenochoanal polyp: diagnose and treatment. Rhinology. 40(4):215–216
Aydin Ö, Keskin G, Üstündağ E, İşeri M, Özkarakaş H (2007) Choanal polyps: an evaluation of 53 cases. Am J Rhinol 21(2):164–168
Choudhury N, Hariri A, Saleh H, Sandison A (2018) Diagnostic challenges of antrochoanal polyps: a review of sixty-one cases. Clin Otolaryngol 43(2):670–674
De Vuysere S, Hermans R, Marchal G (2001) Sinochoanal polyp and its variant, the angiomatous polyp: MRI findings. Eur Radiol 11(1):55–58
Batsakis JG, Sneige N (1992) Choanal and angiomatous polyps of the sinonasal tract. Ann Otol Rhinol Laryngol 101(7):623–625
Yfantis HG, Drachenberg CB, Gray W, Papadimitriou JC (2000) Angiectatic nasal polyps that clinically simulate a malignant process: report of 2 cases and review of the literature. Arch Pathol Lab Med 124(3):406–410
Zou J, Man F, Deng K, Zheng Y, Hao D, Xu W (2014) CT and MR imaging findings of sinonasal angiomatous polyps. Eur J Radiol 83(3):545–551
Sheahan P, Crotty PL, Hamilton S, Colreavy M, McShane D (2005) Infarcted angiomatous nasal polyps. Eur Arch Oto Rhino Laryngol Head Neck 262(3):225–230
Batsakis JG (1979) Tumors of the head and neck: clinical and pathological considerations. Williams & Wilkins
Dai L-B, Zhou S-H, Ruan L-X, Zheng Z-J (2012) Correlation of computed tomography with pathological features in angiomatous nasal polyps. PloS one. 7(12):e53306
Idris AI, Ramli RR, Sachlin ISa. (2017) Angiomatous antrochoanal polyps: challenge in diagnosis. Egypt J Ear Nose Throat Allied Sci. 18(2):137–139
Sayed R, Abu-Dief E (2010) Does antrochoanal polyp present with epistaxis? J Laryngol Otol. 124(5):505–509
Jagadeeswaran V, Vallur S, Shivanand JS. Management of angiomatous antrochoanal polyp: our experience. Indian J Otolaryngol Head Neck Surg. 2020:1–6.
Ceylan A, Asal K, Celenk F, Uslu S (2007) An angiomatous nasal polyp: a very rare variant of sinochoanal nasal polyps. B ENT. 3(3):145–148
Bhama LK, Soni NK (2019) Angiomatous antrochoanal polyp causing epistaxis and bone destruction. An Int J Clin Rhinol 11(1):25–28
Karthikeyan P, Joy SM, Pulimootil DT, Vijayan N (2019) Bleeding angiomatous polyps of the maxillary sinus: Review of literature and a rare case report. Roman J Rhinol 9(35):145–149
Verma N, Kumar N, Sharma N (2011) Angiomatous nasal polyp: a condition difficult to diagnose. An Int J Otorhinolaryngol Clin 3(2):93–97
Acknowledgments
Not applicable.
Funding
There were no financial sources of funding to declare by any of the authors.
Author information
Authors and Affiliations
Contributions
RHS contributed to overall study design and ethics application. AAA contributed to data collection and overall statistical analysis of the data. KGD completed paper write-up, including the development of manuscript figures. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Study design and methodology were reviewed and affirmed by the Institutional Review Board of Sohag University, Faculty of Medicine with No. Soh-Med-23-01-38. Consent to participate is not applicable as this was a retrospective study.
Consent for publication
Written informed consent for publication of their clinical details was obtained from the participants (or from their parent or legal guardian in the case of children under 16).
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ali, A.A., Sayed, R.H. & Dahy, K.G. Angiomatous antrochoanal polyp: a rare entity of choanal polyps. Egypt J Otolaryngol 39, 48 (2023). https://doi.org/10.1186/s43163-023-00411-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00411-5