Abstract
Background
Antrochoanal or Killian polyp is a rare polyp of the maxillary sinus in adults. It is generally unilateral, implanted on the lateral wall of the maxillary sinus upon the uncinate process. Bilateral cases are very rare; only 14 cases have been cited from 1980 to 2020.
Case presentation
Our patient presented with a complete bilateral nasal obstruction, this symptom persisted for more than 10 years, with a perceived prolapse in his throat in the last 4 months. Anterior rhinoscopy showed a polyp that took up the totality of his nasal vestibule. Posterior rhinoscopy showed a polyp bulging behind the uvula.
The challenge in this case is related to diagnosis decision; conditions with the same clinical presentation are several.
Diagnosis was established through the clinical, radiological, and endoscopic aspects, and confirmed by histological findings. Management was obtained through functional endoscopic sinus surgery; no recurrence was noted in the 12-month follow-up, and clinical signs had completely subsided.
Conclusion
Diagnosis in bilateral forms of Killian polyp is perplexing; however, its management is generally simple, with excellent outcome. We report the case of the 15th patient along with a systematic literature review discussing bilateral Killian polyps, illustrated by a rare case of enormous bilateral antrochoanal polyps.
Similar content being viewed by others
Background
Antrochoanal polyp is a rare form of nasal polyps in adults; they are more seen in children and adolescents [1]. Bilateral forms are very rare [1,2,3,4,5,6,7]. Only 14 cases have been mentioned in the literature [8,9,10,11,12,13,14,15,16,17,18,19,20,21]. Diagnosis difficulty is generally due to the scarcity of this disease, and the similar clinical presentation of more frequent differential diagnosis [1,2,3,4]. Management is generally surgical through functional endoscopic sinus surgery, and outcome is great with clinical improvement and no recurrence in follow-up [8,9,10,11,12,13,14,15,16,17,18,19,20,21].
This is a very rare case of bilateral antrochoanal polyp that has long been treated as sinonasal polyposis, without any response to treatment; the aim of this article is to pinpoint the importance of thorough evaluation of clinical and endoscopic findings during patient’s follow-up in chronic rhinosinusitis to re-establish diagnosis and rearrange management strategy according to patient’s case.
Case presentation
A 45-year-old man came to daytime clinic in the Oto-rhino-laryngology department; he had no history of atopy or allergic rhinitis, and no other general conditions and comorbidities.
This patient have had bilateral chronic nasal obstruction for more than 10 years, associated with sporadic headaches, anosmia, nasal discharge, and the sensation of a mass in his throat. No other symptoms were noted.
No relevant medical or familial history was noted; there were no similar cases in the family.
He had never had any surgical interventions.
Anterior rhinoscopy showed a greyish polyp that took on the totality of both nasal cavities, visible in the nasal vestibule. No further landmarks of nasal cavity were visible. Oropharyngeal examination showed exteriorization of a multi-lobular mass behind the uvula.
The patient underwent laboratory and radiological tests. A mild inflammatory syndrome was found with CRP (C Reactive protein) at 35; white blood count was at 12,000, and no other anomalies were found. Respiratory assessment did not find any signs of chronic obstructive diseases, and cardiac assessment was unremarkable.
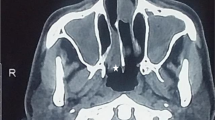
Computed tomography of paranasal sinuses showed an almost complete opacification of maxillary sinuses and the presence of soft tissue masses passing through the maxillary ostium and extending into the corresponding nasal cavities and posteriorly to the adjacent nasopharynx. The other sinuses were normally aerated. (Figs. 1 and 2).
A biopsy was performed and showed an inflammatory polyp.
The diagnostic challenge consisted on the heterogeneous pool of differential diagnosis, and the non-specific clinical presentation of this chronic condition.
Malignancy was first ruled out based on the chronic evolution and the absence of signs of infiltration to osseous walls. Then several chronic conditions were considered: Fernand-Widal syndrome, nasal polyposis, and allergic or infectious chronic rhinosinusitis. The diagnosis of bilateral antrochoanal polyp was maintained upon clinical, radiological, endoscopic and histological findings.
These polyps were classified grade III according to Chung et al.’s classification [6].
The patient first received a medical preparation with steroids and antibiotics before endoscopic surgery.
Oral steroids were prescribed: Prednisone 20 mg, 3 tablets once a day for 5 days, and a course of amoxicillin clavulanate, 1g three times a day for a week. No local treatment was prescribed because of the total obstruction of both nasal cavities.
The surgical procedure relied on functional endoscopic sinus surgery (FESS) under general anesthesia. It consisted of an uncinectomy, an antrostomy of the middle meatus, and a marsupialization of the polyps that were both implanted upon the uncinate process, and the polyps were then pulled through the oral cavity. The surgical intervention went on without any particular adverse event.
No changes in surgical technique were necessary.
In immediate postoperative care, the patient received first-line analgesia; ablation of nasal packing was performed 24 h postoperatively. No adverse events were reported.
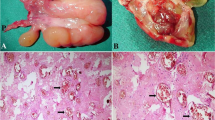
The macroscopic aspect is typical of an antrochoanal polyp (Fig. 3). Histological examination confirmed the diagnosis of a bilateral form of Killian polyps.
The 12-month postoperative endoscopic control showed that mucosa was undergoing a healthy recovery process; no signs of recurrence or other abnormalities were noted.
The patient adhered to treatment; no complaints were reported.
No adverse events were reported.
Discussion
Antrochoanal polyps (ACP) are a rare form of polyps of the maxillary sinus in adults; the bilateral forms are even rarer [1,2,3,4,5,6,7,8,9]. Professor Killian was the first to describe an antrochoanal polyp in 1906 [1]. This polyp is generally implanted on the lateral and inferior wall of the maxillary sinus, most specifically inserted on the uncinate process [1,2,3,4]. It is seen mostly in adolescents and young adults, with no predilection for a certain gender. The most frequent symptoms are related to a dysfunction in the sinus drainage: pus discharge, headache, and nasal obstruction. Prolapse into the oropharynx can be responsible for snoring [2]. Bilateral forms are very rare; they have the same benign prognosis as the unilateral forms [1,2,3,4].
Etiological notions
The causes of antrochoanal polyps is still unclear: allergy, chronic rhinosinusitis, viral infections as well as bacterial ones are associated with a higher incidence of this benign tumor. Besides, anatomical variants that increase pressure inside the maxillary sinus are also incriminated in their formation (Fig. 4).
Epidemiological notions
Ages of patients ranged from 6 years old to 62 (Fig. 5).
Among the 14 patients, we found 7 females and 7 males (Fig. 6).
Ethnic origin is shown in Fig. 7.
Clinical presentation
The most common clinical presentation of ACP is nasal obstruction, sometimes bilateral, depending on the prolapse in the oropharynx [1,2,3,4,5]. Other symptoms are also cited in the literature, such as epistaxis, rhinorrhea, posterior nasal discharge, anosmia, foreign body sensation, halitosis, and snoring [1].
Rhinoscopy findings
Often, ACP is present as a bright mass coming in the middle meatus, with a stalk through the accessory ostium, with the presence of an egg-shaped mass behind the uvula [1,2,3,4,5].
Radiological findings
Radiological investigation through computed tomography and/or magnetic resonance imaging, allows to see the origin of the mass, the sinuses involved, as well as the absence of extension to cranial cavity and orbital cavities [1,2,3,4,5,6].
In the CT (computed tomography) scan, the diagnosis of ACP is established upon the presence of a mass filling the maxillary sinus into the middle meatus through the maxillary ostium, and into the choanae [1]. In the magnetic resonance imaging, the typical aspect is hypo-intense T1, enhanced T2 signals, and peripheral enhancement after gadolinium administration [1].
Shung et al. have established a radiological classification to antrochoanal polyps according to extension to nasopharynx and visibility of accessory ostium [6].
In Stage I, polyp does not reach nasopharynx.
Stage II is defined as a polyp that goes through the accessory ostium of the maxillary ostium that is fully occluded.
Stage III is defined when the antrochoanal polyp goes to the choanae, and the accessory ostium is partially occluded.
Besides, the same authors established a correlation between radiological aspect and histological findings, the more advanced the stage, the more important the inflammatory aspect in histological specimen [6].
Lee DH et al. find that children tend to present more advanced stages, which is explained by authors with late diagnosis in this age group [4].
Matrix organizing findings in 14 cases
The matrix for organizing findings concerning 14 cases are found in the literature (Table 1) [8,9,10,11,12,13,14,15,16,17,18,19,20,21].
Macroscopic and histological aspects
Macroscopically, ACP appears like a white greyish mass, originating from the middle meatus into the nasal cavity, in some cases, with exteriorization into the oral cavity behind the uvula [1, 5]. Histological examination shows inflammatory polyps [1, 5]. The histological aspect shows infiltrates that are less inflammatory and eosinophilic than nasal polyposis [1, 4, 7, 8].
Differential diagnosis
Differential diagnoses are established upon clinical, endoscopic, and radiological findings (Table 2) [5].
Positive diagnosis
Histological aspect is the gold standard diagnostic tool. However, the combination of endoscopy and computed tomography, and MRI of sinonasal cavities in some cases can guide diagnostic reasoning [1, 4,5,6].
Management
However, mini-Caldwell and trans-canine have been described for good exposure and hence the complete removal of ACP [6]. However, the mini-invasive endoscopic technics by FESS (Functional endoscopic sinus surgery) is the gold standard surgical technic, since it has the same outcome with less risk of complications [1, 4,5,6].
The cornerstone of successful surgical removal of ACP is the identification and removal of its origin and bulk [5].
The surgical management though FESS is successful in most cases; the recurrent cases are due most probably to the growth of residual polypoid tissue in the maxillary antrum [6].
Establishing a communication between the natural maxillary ostium and the accessory ostium is key to avoid recirculation phenomenon postoperatively [4].
Shayasate et al. claim that recurrences are more frequent in children, and that follow-up for 24 months allows to diagnose 95% of recurrences [7].
Bilateral forms of antrochoanal polyp are very rare [1,2,3,4]. Establishing the right diagnosis and planning the surgical procedure are based on the presence of bilateral nasal obstruction, nasopharyngeal mass, the endoscopic aspect on preoperative evaluation and on computed tomography; the histological aspect confirms this diagnosis [1,2,3,4,5,6,7,8,9, 11, 14, 17,18,19,20,21].
Conclusions
Bilateral antrochoanal polyp is a rare benign condition that is very ill-lived by patients. Only 14 cases have been found in the literature. Strengths of this case reside in the presentation of a rare condition, presenting outside the age group in unilateral forms, and in a clinical context that had been misleading into considering other differential diagnosis.
It can be present in patients with all ages, and without particular pattern of gender predilection, early diagnoses upon clinical, endoscopic, and radiological and histological findings is possible. And treatment is generally surgical, with excellent prognosis
Patient’s perspective
The patient claimed that nasal obstruction subsided along with all the other symptoms, with a significant improvement of his sense of smell.
Availability of data and materials
Not applicable
Abbreviations
- ACP:
-
Antrochoanal polyp
- CRP:
-
C-Reactive protein
- FESS:
-
Functional endoscopic surgery
- CT:
-
Computed tomography
References
Frosini P, Picarella G, De Campora E (2009) Antrochoanal polyp: analysis of 200 cases. Acta Otorhinolaryngol Ital 29(1):21–26
Piquet JJ, Chevalier D, Leger GP, Rouquette I, LeconteHoucke M (1992) Microchirurgie endo-nasale du polype antrochoanal. Acta Otorhinolaryngol Belg 46(3):267–271
Yılmaz E, Alatas N, Ucar F, Cora T, Buruk K, Unlu Y (2019) Investigation of human papillomavirus (HPV) and Epstein-Barr virus (EBV) in antrochoanal polyps. Am J Otolaryngol 40(3):389–392. https://doi.org/10.1016/j.amjoto.2019.02.008 Epub 2019 Feb 19. PMID: 30808528
Lee DH, Yoon TM, Lee JK, Lim SC (2016) Difference of antrochoanal polyp between children and adults. Int J Pediatr Otorhinolaryngol 84:143–146. https://doi.org/10.1016/j.ijporl.2016.03.004
Woodworth BA, Poetker DM, Reh DD (2016) Rhinosinusitis with nasal polyposis. Adv OtorhinolaryngolBasel, Karger 79:1–12. https://doi.org/10.1159/000444957
Chung S-K, Chang B-C, Dhong H-J (2002) Surgical, radiologic, and histologic findings of the antrochoanal polyp. Am J Rhinol 16(2):71–76. https://doi.org/10.1177/194589240201600201
Chaiyasate S, Roongrotwattanasiri K, Patumanond J, Fooanant S (2015) Antrochoanal polyps: how long should follow-up be after surgery? Int J Otolaryngol 2015:2974175 pages. https://doi.org/10.1155/2015/297417
Sinha SN, Kumar A (1980) Bilateral antrochoanal polyps. Ear Nose Throat J 59(4):178–179PMID: 7363852. https://doi.org/10.1177/014556138005900409
Myatt HM, Cabrera M (1996) Bilateral antrochonanal polyps in a child: a case report. J Laryngol Otol 110(3):272–274. https://doi.org/10.1017/S0022215100133390
Basu SK, Bandyopadhyay SN, Bora H (2001) Bilateral antrochoanal polyps. J Laryngol Otol 115(7):561–562. https://doi.org/10.1258/0022215011908225
Jmeian S (2006) Bilateral antrochoanal polyps in a child: an extremely rare case. JRMS 13(6):57–58
Yilmaz YF, Titiz A, Özcan M, Tezer MS (2007) Bilateral antrochoanal polyps in an adult: a case report. B-ENT 3(2):97–99
Konstantinidis I, Tsakiropoulou E, Vital I (2008) Bilateral antrochoanal polyps originated from inferior meatal antrostomies. Laryngo-Rhino-Otol 87(6):417–419. https://doi.org/10.1055/s-2007-995464
Sousa DW, Pinheiro SD, Silva VC, Bastos JP (2011) Bilateral antrochoanal polyps in an adult. Braz J Otorhinolaryngol 77(4):539. English, Portuguese. PMID: 21860986. https://doi.org/10.1590/s1808-86942011000400023
Singhal P, Gupta N (2011) Bilateral antrochoanal polyp in an adult: a rarity. Clin Rhinol 4(9):145–146
Sabino HA, Faria FM, Tamashiro E, Lima WT, Valera FC (2014) Bilateral antrochoanal polyp: case report. Braz J Otorhinolaryngol 80(2):182–183. https://doi.org/10.5935/1808-8694.20140037
Oner F, Sakat MS, Gozeler MS, Altas E, Ucuncu H, Kilic K (2015) Bilateral antrochoanal polyp. J Craniofac Surg 26(7):e661–e662. https://doi.org/10.1097/SCS.0000000000002072 PMID: 26468860
Chodankar S, Tiwari M. Bilateral antrochoanal polyp in an elderly male—a rarity. Odisha J Otorhinolaryngol 2015;9.
Alashoura AS, Alshaikh NA, Yeak S (2016) Bilateral antrochoanal polyps: a case report and literature review. Pan Arab J Rhinol 6(2):59–63. https://doi.org/10.4103/2090-7540.200619
Aksakal C (2018) Bilateral antrochoanal polyp in a child. J Craniofac Surg 29(8):2368–2369. https://doi.org/10.1097/SCS.0000000000004947 PMID: 30320689
Iziki O, Rouadi S, Abada RL, Roubal M, Mahtar M (2019) Bilateral antrochoanal polyp: report of a new case and systematic review of the literature. J Surg Case Rep 2019(3):rjz074. https://doi.org/10.1093/jscr/rjz074
Acknowledgements
Not applicable
Informed consent
The patient understood the conditions, the importance of different tests, the different steps of surgical management, the medical treatment, and the postoperative follow-up, and consented to the different steps of management, and publication.
Funding
None
Author information
Authors and Affiliations
Contributions
KC conceived and designed the analysis, collected the data, performed the analysis and wrote the paper. NT contributed data or analysis tools and wrote the paper. IN contributed in surgery. KN assisted in writing the paper. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
A written informed consent for publication was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
cherrabi, K., Touihem, N., Nakkabi, I. et al. Bilateral antrochoanal polyps: a case report. Egypt J Otolaryngol 37, 30 (2021). https://doi.org/10.1186/s43163-021-00090-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-021-00090-0