Abstract
Background
Antrochoanal polyps (ACPs) are pathologically benign nasal swellings. The maxillary sinus is the commonest reported origin. The polyps are usually unilateral and often exit through the progressively widened maxillary sinus ostium to occupy the choana and may reach the nasopharynx. It is a disease of adolescents and young adults who often present with progressive unilateral nasal obstruction. Encountering bilateral antrochoanal polyps is very rare.
Case presentation
We report a forty years old male who had progressive bilateral nasal obstruction for 8 years associated with hyposmia and intermittent facial pain and headaches. A nasal mass could be seen on anterior rhinoscopy on both sides, more prominent on the left. Endoscopy revealed bilateral masses hanging down the choanae. Computerized tomography scan of the nose and paranasal sinuses demonstrated bilateral nasal polypi and widening of the maxillary sinus ostia. During endoscopic surgical excision of the lesions, polypi were found to dilate the ostia of both maxillary sinuses. The polypi had antral, nasal, and choanal parts typical of antrochoanal polypi on both sides. The histopathology showed the inflammatory nature characteristic of antrochoanal polyp. Postoperatively, the patient’s symptoms resolved dramatically, and he is on continuous regular scheduled follow-up.
Conclusion
Bilateral antrochoanal polyps can present with nasal obstruction and can be misdiagnosed as sinusitis; radiological and endoscopic features are useful to reach specific diagnosis; what is special about our presentation is that it is an addition to the literature of a rare disease (bilateral ACPs), and we are reporting it in an older age rather than the common younger age of presentation in the literature reports, which is an addition to the demographic data.
Similar content being viewed by others
Background
Antrochoanal polyps (ACPs) are an uncommon variety of nasal polyps that are seen in adolescents, young adults, and children. Palyin was the first to report it in 1753 [1]. Killian added in 1906 that the origin of the polyp is the maxillary antrum [2]. Antrochoanal polyps are usually unilateral; bilateral antrochoanal polypi were infrequently reported in the literature [3]. The age of presentation of an antrochoanal polyp is usually the second or third decade, and the complaint is progressive nasal obstruction, hyposmia, facial pains, and headaches. There may be postnasal drip, hyponasality of speech, and symptoms of Eustachian tube obstruction. Quite a lot of time is spent in treatment with the general practitioner and further in investigations in the rhinology clinic to reach a final diagnosis [4]. Computerized tomography (CT) scan, endoscopy, and magnetic resonance imaging (MRI) of the paranasal sinuses eventually lead to the diagnosis [4]; however, the final diagnosis is by histopathology. The definitive management of an antrochoanal polyp is surgical, preferably using functional endoscopic sinus surgery (FESS) with the aim of complete and radical excision of the antrochoanal polyp. Prevention of recirculation phenomenon which could occur postoperatively is by creating a good connection between the natural and the accessory maxillary sinus ostia [4]. The overall prognosis is excellent, and recurrences are negligible [5].
Our report adds to the scarce literature reports about bilateral antrochoanal polyps and with a new feature; our patient age is significantly older than the commonly reported age, which is an addition to the demographic data.
Case presentation
A 40-year-old farmer presented to our otorhinolaryngology clinic referred by a general practitioner who noticed an obvious unilateral nasal mass; on careful history taking, the patient claimed a history of nasal obstruction which was worsening for the last 8 years. At the time of presentation, he could hardly distinguish between common olfactory odors. He complained of frequent watery nasal discharge but had no epistaxis. He experienced recurrent bouts of facial pain and headaches which were intense in the morning and gradually improve during the day. Furthermore, he had dull earaches and frequent tinnitus but no obvious hearing impairment. The patient experienced a 2-year history of shortness of breath which was diagnosed as bronchial asthma, and prophylactic bronchodilator was prescribed. The patient is not known to be sensitive to any specific allergens. No similar condition was elicited in the family; there was no significant medical, surgical, or drug history. He is not a smoker or alcohol consumer, and he is not on chronic medication.
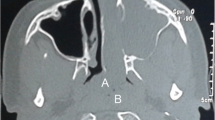
On the examination, nasal patency was reduced on both nostrils (using cold spatula test). Anterior rhinoscopy revealed a pale polypoidal mass on each nostril; the left one was protruding out of the nasal vestibule, while the right was filling the right nostril; on posterior endoscopic rhinoscopy, extension of the polypi was visible on both sides. Complete blood count showed eosinophilia. The C-reactive protein was 1.9 mg/dl (normal level is 0.3–1.0 mg/dl). The chest x-ray appearance was unremarkable. Axial and coronal computed tomography of the paranasal sinuses showed almost complete opacification of both the maxillary sinuses and soft tissue masses coming through the maxillary ostia and extending into the choanae to the nasopharynx (Figs. 1, 2, and 3).
Differential diagnosis at that time was bilateral ethmoidal polypi, allergic fungal rhinosinusitis, and chronic rhinosinusitis with nasal polypi (CRSwNP).
Malignancy and angiofibroma were ruled out by the noninvasiveness and nonvascular nature of the lesion on CT scan. The patient received a short course of systemic steroid (prednisolone tablets, 1 mg per kg, in three divided doses per day for 1 week preoperative and continued for 3 weeks then tapered off, and he continued on topical nasal steroid (betamethasone) in the form of nasal spray. Careful intraoperative assessment was conducted during functional endoscopic sinus surgery (FESS) under general hypotensive anesthesia. The polyps were causing widening of both maxillary sinus ostia; each polyp has typical antral, nasal meatal, and choanal parts characteristic for ACP. The polypi were removed as one-piece en bloc through the nose from each side; the surgical specimen is shown in Fig. 4.
The nasal pack was removed after 24 h. The postoperative recovery was uneventful, and the patient was discharged home. The patient was assessed on days 7 and 14 at the outpatient clinic and then at monthly basis for the following 4 months without evidence of recurrence. The histopathology report showed symmetrical inflammatory polypi, partially lined by the upper respiratory epithelium, with edematous stroma and mixed inflammatory infiltrate composed mainly of plasma cells, with no evidence of vascularity, malignancy, granuloma, or fungal infection, consistent with antrochoanal polyp.
No adverse events were reported on postoperative follow-up. The patient experienced immediate relief of symptoms regarding nasal obstruction and hyposmia. The patient’s wellness is sustained, and he was instructed to report any new complaints.
Discussion
Killian or antrochoanal polyps (ACPs) are uncommon benign polypoidal lesions which constitute approximately 4–6% of all nasal polyps in the general population [6]. They originate due to unknown etiopathogenesis [7] from the inflamed and edematous mucosa of the maxillary antrum and extending into the choana and postnasal space and can reach oropharynx. Frosini et al., who studied 200 patients with ACPs, suggested an association of inflammatory-anatomical alteration that forces the polyp to herniate through the accessory ostium.
Lee and Huang found that the most common site of origin was the posterior wall of maxillary sinus in 92% of their cases [8]. However, there are reports for other origins: from the nasal septum, sphenoid sinus, ethmoid sinus, hard and soft palates, and nasal turbinates [9, 10]. ACPs are almost always unilateral, but limited cases of bilateral ACPs have been reported in the literature [11]. Myatt et al. described the first bilateral ACP in 12-year-old patient [12]. Most of the patients with ACPs were children and young adults [13], presenting with nasal obstruction and postnasal discharge, with males affected more than females [5].
The differential diagnosis includes retention mucous cysts, mucocele, maxillary rhinosinusitis, meningoencephalocele, olfactory esthesioneuroblastoma, angiofibroma, and inverted papilloma [14]. Computed scan and nasofibroscopy are diagnostic for ACPs [14].
ACPs are treated with surgery, preferably functional endoscopic surgery (FESS), to target the exact origin and extension to minimize recurrence.
Our patient is 40 years in contradistinction to most reported cases of bilateral ACPs which occurred in younger age groups [3, 10]. Our patient is a male which is in agreement with the literature; ACPs affect males more than females [5]. Cherrabi et al. had reviewed the bilateral antrochoanal polyps reported in the international literature [3]. Allergy and atopy are evident by the history of bronchial asthma and the eosinophilia; sinusitis also is likely due to the clinical presentation and raised C-reactive protein; these two factors are associated with ACPs as stated by Lee and Huang who reported that 65% of the patients with ACP had chronic sinusitis [6]. Sunagawa et al. demonstrated the possible role of plasminogen activator and inhibitor in the pathogenesis of ACPs in their study; these are still experimental tests and have not been applied to routine clinical practice [15]. Clinical presentation of our patient is consistent with the reports by Orvidas et al. who observed nasal obstruction (100%), rhinorrhea (48%), snoring (36%), and mouth breathing (32%) in their patients with ACP [16].
Anterior rhinoscopy demonstrated the intranasal polyp. Nasal endoscopy and CT were the main diagnostic techniques. Features on CT scans were typical to reports by Pruna et al. [17]. Our histopathology report except for variation in evidence of vascularity was consistent with the Skladzien J report stating that characteristics of ACPs are similar to those of non-allergic polyps of the maxillary sinus; ACPs are lined with pseudostratified ciliated epithelium, and their stromal connective tissue contains a variable infiltration of inflammatory cells [18]. The stroma is usually edematous and highly vascular, and it is composed of loose connective tissue that is mainly infiltrated with plasma cells and a few eosinophils.
Simple polypectomy and a Caldwell-Luc procedure were the previously preferred methods for the surgical treatment of ACPs. In recent years, endoscopic sinus surgery (ESS) became the most preferred surgical technique. Simple polypectomy is associated with a high recurrence rate [8]. The antral part of the polyp should be removed to avoid post-operative recurrence. FESS has recently been shown to be a safe as well as effective method for treating ACPs; it consists of avulsion then resection of the nasal component of the polyp and the cystic antral component which is tethered to the maxillary wall through the middle meatus [19]; it is advisable to resect the lower part of the uncinate process and to widen the maxillary ostium. Cook et al. [7] observed no recurrences for 33 patients with ACPs after FESS. We adopted the FESS technique in our surgery with meticulous follow-up of all the necessary steps, and the polyps were exenterated from the roots and removed in toto.
Conclusion
Bilateral antrochoanal polyps are a rare disease entity; patients can be misdiagnosed initially as rhinosinusitis for years until the nasal mass was quite evident. What is special about our presentation is that it is an addition to the literature of a rare disease (bilateral ACPs), and we added to the demographic data as well by reporting it in an older age from the common younger age of presentation in the literature reports.
Availability of data and materials
Data is available upon reasonable request from the corresponding author.
References
Palfyn J (1753) Anatomie chirurgicale. Paris. https://scholar.google.com/scholar_lookup?title=Anatomie+Chirurgicale&author=J+Palfyn&publication_year=1753&
Frosini P, Picarella G, De Campora E (2009) Antrochoanal polyp: analysis of 200 cases. Acta Otorhinolaryngol Ital 29(1):21–6. PMID: 19609378; PMCID: PMC2689564
Cherrabi K, Touihem N, Nakkabi I et al (2021) Bilateral antrochoanal polyps: a case report. Egypt J Otolaryngol 37:30. https://doi.org/10.1186/s43163-021-00090-03
Lee DH, Yoon TM, Lee JK, Lim SC (2016) Difference of antrochoanal polyp between children and adults. Int J Pediatr Otorhinolaryngol 84:143–146. https://doi.org/10.1016/j.ijporl.2016.03.004. Epub 2016 Mar 12 PMID: 27063770
Yuca K, Bayram I, Kiroğlu AF, Etlik O, Cankaya H, Sakin F, Kiriş M (2006) Evaluation and treatment of antrochoanal polyps. J Otolaryngol 35(6):420–423. PMID: 17380838
Başak S, Karaman CZ, Akdilli A, Metin KK (1998) Surgical approaches to antrochoanal polyps in children. Int J Pediatr Otorhinolaryngol 46(3):197–205. https://doi.org/10.1016/s0165-5876(98)00160-8. PMID: 10190590
Cook PR, Davis WE, McDonald R, McKinsey JP (1993) Antrochoanal polyposis: a review of 33 cases. Ear Nose Throat J 72(6):401–2, 404-10. PMID: 8344181
Lee TJ, Huang SF (2006) Endoscopic sinus surgery for antrochoanal polyps in children. Otolaryngol Head Neck Surg 135(5):688–692. https://doi.org/10.1016/j.otohns.2006.02.035. PMID: 17071295
Ileri F, Köybaşioĝlu A, Uslu S (1998) Clinical presentation of a sphenochoanal polyp. Eur Arch Otorhinolaryngol 255(3):138–139. https://doi.org/10.1007/s004050050030. PMID: 9561861
Aydil U, Karadeniz H, Sahin C (2008) Choanal polyp originated from the inferior nasal concha. Eur Arch Otorhinolaryngol 265(4):477–479. https://doi.org/10.1007/s00405-007-0461-3. Epub 2007 Sep 28 PMID: 17901966
Basu SK, Bandyopadhyay SN, Bora H (2001) Bilateral antrochoanal polyps. J Laryngol Otol 115(7):561–562. https://doi.org/10.1258/0022215011908225. PMID: 11485589
Myatt HM, Cabrera M (1996) Bilateral antrochoanal polyps in a child: a case report. J Laryngol Otol 110(3):272–274. https://doi.org/10.1017/s0022215100133390. PMID: 8730368
Ozdek A, Samim E, Bayiz U, Meral I, Safak MA, Oğuz H (2002) Antrochoanal polyps in children. Int J Pediatr Otorhinolaryngol 65(3):213–218. https://doi.org/10.1016/s0165-5876(02)00153-2. PMID: 12242136
Freitas MR, Giesta RP, Pinheiro SD, Silva VC (2006) Antrochoanal polyp: a review of sixteen cases. Braz J Otorhinolaryngol 72:831–835
Sunagawa M, Kinjoh K, Nakamura M, Kosugi T (1999) Urokinase-type plasminogen activator and plasminogen activator inhibitor antigen in tissue extracts of paranasal sinus mucous membranes affected by chronic sinusitis and antrochoanal polyps. Eur Arch Otorhinolaryngol 256(5):237–241. https://doi.org/10.1007/s004050050149. PMID: 10392298
Orvidas LJ, Beatty CW, Weaver AL (2001) Antrochoanal polyps in children. Am J Rhinol 15(5):321–5. PMID: 11732819
Pruna X, Ibañez JM, Serres X, Garriga V, Barber I, Vera J (2000) Antrochoanal polyps in children: CT findings and differential diagnosis. Eur Radiol 10(5):849–851. https://doi.org/10.1007/s003300051017. PMID: 10823646
Składzień J, Litwin JA, Nowogrodzka-Zagórska M, Wierzchowski W (2001) Morphological and clinical characteristics of antrochoanal polyps: comparison with chronic inflammation-associated polyps of the maxillary sinus. Auris Nasus Larynx 28(2):137–141. https://doi.org/10.1016/s0385-8146(00)00108-5. PMID: 11240321
Sato K, Nakashima T (2000) Endoscopic sinus surgery for chronic sinusitis with antrochoanal polyp. Laryngoscope 110(9):1581–1583. https://doi.org/10.1097/00005537-200009000-00036. PMID: 10983967
Acknowledgements
Not applicable.
Funding
The authors had not received any funding.
Author information
Authors and Affiliations
Contributions
S.E. K prepared the manuscript and operated on the patient. O.M.K participated in the writing and reviewing of the case report. H.I.Y supervised and edited the case report. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient.
Ethical approval was obtained from Soba Center for AUDIT and Research committee at Soba University hospital Khartoum (Sudan).
Consent for publication
An informed written consent for publication had been obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kardman, S.E., Khalid, O.M. & Yagi, H.I. Bilateral antrochoanal polyps in a Sudanese patient: a case report. Egypt J Otolaryngol 39, 88 (2023). https://doi.org/10.1186/s43163-023-00455-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00455-7