Abstract
Background
Symptomatic knee osteoarthritis (OA) commonly co-occurs in people with type 2 diabetes (T2DM) and increases the risk for diabetes complications, yet uptake of evidence-based treatment is low. We combined theory, stakeholder involvement and existing evidence to develop a multifaceted intervention to improve OA care in persons with T2DM. This was done in partnership with Arthritis Society Canada to leverage the existing infrastructure and provincial funding for community arthritis care.
Methods
Each step was informed by a User Advisory Panel of stakeholder representatives, including persons with lived experience. First, we identified the target groups and behaviours through consulting stakeholders and current literature. Second, we interviewed persons living with T2DM and knee OA (n = 18), health professionals (HPs) who treat people with T2DM (n = 18) and arthritis therapists (ATs, n = 18) to identify the determinants of seeking and engaging in OA care (patients), assessing and treating OA (HPs) and considering T2DM in OA treatment (ATs), using the Theoretical Domains Framework (TDF). We mapped the content to behavioural change techniques (BCTs) to identify the potential intervention components. Third, we conducted stakeholder meetings to ascertain the acceptability and feasibility of intervention components, including content and modes of delivery. Fourth, we selected intervention components informed by prior steps and constructed a programme theory to inform the implementation of the intervention and its evaluation.
Results
We identified the barriers and enablers to target behaviours across a number of TDF domains. All stakeholders identified insufficient access to resources to support OA care in people with T2DM. Core intervention components, incorporating a range of BCTs at the patient, HP and AT level, sought to identify persons with knee OA within T2DM care and refer to Arthritis Society Canada for delivery of evidence-based longitudinal OA management. Diverse stakeholder input throughout development allowed the co-creation of an intervention that appears feasible and acceptable to target users.
Conclusions
We integrated theory, evidence and stakeholder involvement to develop a multifaceted intervention to increase the identification of knee OA in persons with T2DM within diabetes care and improve the uptake and engagement in evidence-based OA management. Our partnership with Arthritis Society Canada supports future spread, scalability and sustainability. We will formally assess the intervention feasibility in a randomized pilot trial.
Similar content being viewed by others
Background
Driven by the ageing of the population and the epidemic of overweight and obesity, the prevalence of osteoarthritis (OA), the most common form of arthritis, is rapidly rising [1]. This has resulted in an increasing number of people living with OA-related functional limitations and has situated OA as a leading cause of disability worldwide [1]. Knee OA accounts for nearly 80% of the burden of OA [1]. Knee OA-related disability has many potential consequences, including impacts on individuals’ other complex chronic conditions [2,3,4,5,6,7,8].
In people with type 2 diabetes (T2DM), OA frequently co-occurs [9] and has detrimental effects [10]. At least one in six individuals with T2DM also has knee OA [11], due to shared risk factors and potentially metabolic pathways [12]. In those with T2DM and knee OA, OA-related walking difficulty increases the risk for diabetes-specific complications and cardiovascular events [4], which may be a result of more sedentary time and/or less engagement in the physical activity [13] that is a cornerstone of T2DM management [14]. Symptomatic OA may also challenge T2DM self-management through poor sleep, low mood and fatigue [15] limiting reserves for the “extra work” of T2DM management [16]. It is therefore incumbent upon the medical community to improve recognition of OA and implementation of evidence-based OA treatment in people with T2DM.
Despite the consequences of knee OA-related functional limitations, safe, effective and guideline-recommended [17] knee OA treatments, such as education, physical activity and weight management, are underused [18]. One problem is the under-diagnosis of OA in the community [19], precluding patient provision of and engagement in care [20, 21]. Those with other chronic conditions, such as T2DM, are even less likely to have their OA addressed [22]. A further challenge is care delivery, with a need for services and programmes to support the necessary behavioural changes that are inherent in OA first-line treatments [23, 24]. Physical activity is also a key treatment for OA, resulting in long-term improvements in pain and function [25]. However, without adequate guidance from health professionals, people often are unclear about what they should do and may avoid participating in physical activity for fear of causing harm [26]. Finally, the current single-condition paradigm for chronic disease management [27] inefficiently slices up care, placing added burden and responsibility on patients for harmonizing chronic disease management strategies. Services that situate OA within the context of multimorbidity may be most successful and best optimize whole-person health.
Multiple complex interventions have been developed in an attempt to put evidence-based OA care into practice, including providing support for the behaviour change required [28]. Most interventions target persons with an established diagnosis of OA and have used strategies such as leveraging non-physician clinicians and/or digital technologies in the provision of care [29,30,31,32,33,34,35,36,37,38,39,40,41]. The Goodlife with osteoArthritis in Denmark (GLA:D) programme is an example of a successful education and exercise intervention delivered by trained physical therapists (and other clinicians) to improve pain and function in people with knee and/or hip OA [42]. However, few strategies have been developed to identify, assess and diagnose the many people with joint symptoms consistent with OA who lack a formal OA diagnosis. Marra et al. showed that a complex intervention involving screening persons with knee pain presenting to pharmacies improved the utilization of OA treatments and patient outcomes [43]. To our knowledge, no intervention has been developed specifically to improve OA care in individuals with other complex chronic conditions, such as T2DM, where competing demands may make OA care particularly challenging and necessitate a personalized approach [44]. Overcoming these challenges to improving uptake of and engagement in evidence-based knee OA care in persons with other chronic conditions, such as T2DM, with a view to increasing physical activity, holds the potential to improve both OA outcomes and outcomes related to the other chronic conditions.
Our aim, guided by the UK Medical Research Council (MRC) framework [45], was to use a systematic process combining theory, stakeholder involvement and existing evidence to develop a multifaceted implementation intervention to improve the uptake of evidence-based OA care including physical activity in persons with T2DM and knee OA. A broader aim was to outline this process of systematically developing a complex intervention that seeks to change the behaviours of health professionals (HPs) and patients to provide a template for researchers tackling similar implementation problems.
Methods
Setting
In Ontario, Canada, individuals with chronic conditions, such as T2DM, present to primary care providers (family physicians or nurse practitioners) as the first point of contact in the health care system. A referral from a primary care provider or other physician is needed for an individual to access medical specialist services. The health care system in Ontario is publicly funded and privately administered. The Ontario Health Insurance Plan provides coverage for most medical and emergency services provided in Ontario. However, it does not provide universal coverage. Relevant to persons with T2DM and OA, prescription drugs and physiotherapy for those who are not on social assistance and/or under age 65 are paid for out-of-pocket by patients.
Design
Overarching framework
We developed our complex intervention within the first phase of the Treatment of Knee Osteoarthritis in Persons with Diabetes Mellitus (TOP-DM) study, combining relevant theory, current evidence and stakeholder input. The intervention development work took place from 2020 to 2021. We followed the 2008 and 2021 UK MRC updated guidance for the development and evaluation of complex interventions [45, 46] that divide the research process into four phases. As recommended within the intervention development phase, we used theory to comprehensively identify the determinants of behaviour and linked them to the mechanisms of change [47], while meaningfully engaging stakeholders [45], to maximize the potential for developing an intervention that will have positive impacts on health-related outcomes. We also placed strong importance on understanding context throughout the research process, including theorizing how the intervention generates its effects and ensuring it would be implementable among the target population and setting.
Arthritis Society Canada
At the conception of this study, we partnered with Arthritis Society Canada, a not-for-profit non-governmental organization in Canada that seeks to elevate arthritis awareness, education and research. Within the province of Ontario, Arthritis Society Canada is directly involved in the provision of arthritis care through the Arthritis Rehabilitation and Education Program (AREP) [48], which provides provincially funded arthritis services, including group and one-on-one education and self-management sessions delivered by a team of trained physical therapists and occupational therapists, at no cost to patients. Thinking ahead to the eventual spread, scalability and sustainability of our intervention, the partnership allowed us to benefit from the existing infrastructure and provincial funding for arthritis care.
User advisory panel
We constructed a user advisory panel (UAP) comprising diverse stakeholder membership to facilitate intervention co-design [49,50,51]. The UAP comprised three patient research partners living with T2DM and OA, the director of AREP and HPs from physical therapy, family medicine, endocrinology and rheumatology. Members of the UAP were consulted throughout the research process.
Approach to intervention development
As the MRC framework lacks detailed operational guidance on the intervention development process, we followed the systematic step-wise approach to intervention development described by French et al. [47]. We outline these four steps below. We also present a summary of our intervention development process in Fig. 1.
Overview of the step-wise intervention development process. Figure adapted from Riordan et al. [52]. BCT, behavioural change technique; TDF; theoretical domains framework
Ethics approval was obtained from Women’s College Hospital and University of Toronto Research Ethics Boards.
Step 1: Who needs to do what, differently?
The process of identifying individuals with T2DM who also have knee OA and providing evidence-based OA care involves multiple separate behaviours being performed by different individuals. Our research team, comprising individuals with expertise in both OA and T2DM, began by brainstorming potential behaviours to target and by whom. We first envisioned the care pathway of a person with T2DM and the steps that are needed for them to have joint symptoms assessed and diagnosed and for evidence-based OA care to be provided. Behaviours were reviewed with and refined through consultation with the UAP.
Step 2: Using a theoretical framework, which barriers and enablers need to be addressed?
We undertook qualitative studies in three stakeholder groups (patients; diabetes HPs, including family physicians, endocrinologists and diabetes educators; and AREP arthritis therapists [ATs]), to identify the barriers and enablers to the target behaviours [53,54,55]. Semi-structured telephone interviews, conducted between September 2020 and January 2021, comprehensively explored the behaviours of interest for each group, guided by the Theoretical Domains Framework (TDF) [56]. The interview guides are provided in Additional file 2: Tables B, C and D.
We recruited individuals who had a physician diagnosis of T2DM and knee OA (“patients”), from a hospital-based family medicine clinic and through an email invitation to past clients of AREP. Interviews focused on individuals’ prior experiences living with T2DM and knee OA and behavioural determinants of seeking and engaging in OA care. We purposefully sampled diabetes HPs according to role and practice location to achieve a mix of family physician, endocrinologist and diabetes educator participants and practice locations in Ontario, Canada. Interviews explored the HP experiences with individuals with T2DM who also had knee OA and behavioural determinants of addressing and managing OA. We recruited practising AREP ATs through email invitations. These interviews explored the ATs’ experiences caring for persons with knee OA and other complex chronic conditions and the behavioural determinants of considering T2DM when formulating an OA treatment plan, including prescribing and monitoring physical activity. These interviews also allowed us to better understand the structure and practices within the current AREP care model to enrich our contextual understanding.
All interviews were digitally recorded and transcribed verbatim, and data were organized in NVivo 10. We deductively analysed the data informed by the TDF; within each TDF domain, data were inductively analysed to develop themes/belief statements [57].
Step 3: Which intervention components (behaviour change techniques and mode(s) of delivery) could overcome the modifiable barriers and enhance the enablers?
Mapping TDF domains to appropriate behaviour change techniques
We mapped the barriers and enablers, organized by TDF domains, to behaviour change techniques (BCTs), using the Theory and Technique Tool (https://theoryandtechniquetool.humanbehaviourchange.org/) developed by Michie et al. [58]. A BCT is defined as “a replicable component of an intervention designed to alter or redirect causals processes that regular behaviour” [59]. The tool shows where there are links between BCTs and mechanisms of action (including each TDF domain) based on a literature synthesis and expert consensus. Using this tool, we generated a list of potential BCTs for each identified TDF domain including those with confirmed or inconclusive evidence to support a link.
The list of BCTs was refined by members of the research team as those considered feasible, locally relevant and that could be operationalized within the scope of the current study. Multiple BCTs spanned more than one TDF domain.
Developing intervention components and combining them into an acceptable deliverable intervention
To develop intervention components that were likely to be feasible, relevant in the local context and acceptable to stakeholders, we conducted two meetings (2 h each) with our UAP. Meetings were conducted by videoconference and facilitated by two of the authors (LK and GH). At the first meeting, we reviewed the existing literature and our qualitative interview findings and brainstormed potential intervention components. This information was then used by the research team to develop a preliminary sketch of intervention components, considering the APEASE (affordability, practicability, effectiveness, acceptability, side effects, equity) criteria [60]. We drew on practice guidelines for persons with knee OA [17], T2DM [61] and results of prior OA interventions and considered many different potential intervention components and modes of delivery.
At the second meeting, we discussed the sketch of the intervention. We presented unrefined potential components to invite input from our UAP. The UAP deliberated on the modes of delivery of intervention components and how to select and tailor specific strategies to address contextual needs. The research team made revisions to the draft intervention and presented the updates to our three patient partners, separately in 30–60-min meetings, to confirm acceptability and feasibility and whether other alternatives should be considered. Based on these discussions, we made further modifications. We then discussed the proposed intervention with two family physicians from our UAP, one rural and one urban, separately, to review the feasibility of the intervention components in their clinical practices. We reviewed the intervention with a rheumatologist, to confirm the acceptability of the identified ways to address OA. We conducted a meeting with a group of four endocrinologists who practised in different clinical settings to get diverse perspectives on how the intervention could be applied. We then presented and discussed the intervention with stakeholders at Arthritis Society Canada, including three ATs, the director of AREP and the vice president of AREP for Arthritis Society Canada. Some components that were not considered feasible were removed.
Step 4: How can behaviour change be measured and understood?
We conducted evaluability assessments [45] through engaging experts in quality and innovation (NG) and implementation science (NI) to decide on proximal and feasibility outcomes of the intervention, the data to be collected and assessed and the options for evaluation. This resulted in a plan for feasibility evaluation that will be fully reported separately.
To describe our programme theory, we developed logic models of the final intervention, presenting the inputs, processes and the causal mechanisms by which we expect intervention components to have positive effects.
Results
The final intervention has been reported according to TiDierR [62].
Step 1: Identify who needs to do what, differently
We confirmed the following behaviours of interest: (1) for HPs, to identify and treat knee OA; (2) for persons with T2DM and knee OA, to seek and engage in knee OA care; and (3) for Arthritis Society Canada ATs, to consider T2DM when formulating an OA treatment plan, including a focus on prescribing and monitoring physical activity. Using the Action, Actor, Context, Target, Time (AACTT) framework [63], we further specify these behaviours in Table 1.
Step 2: Identify the barriers and enablers that need to be addressed using a theoretical framework
We conducted qualitative interviews with 18 persons with T2DM and knee OA, 18 HPs who treat persons with T2DM (8 endocrinologists, 7 family physicians, 3 diabetes educators) and 18 ATs. These studies, reported elsewhere [53,54,55], are summarized below, and we list the TDF domains that we identified as relevant in parentheses.
Interviews with persons living with knee OA and T2DM
Of the 14 TDF domains, seven prominently influenced the behaviour of patients to seek and engage in OA care. Important barriers included the insufficient provision of OA knowledge to fully engage in care (knowledge), feeling incapable of participating in physical activity/exercise due to joint pain (beliefs about capabilities), lack of guidance from HPs and insufficient access to community programmes/supports (environmental context and resources) and being uncertain that OA therapies would help them (optimism). Key enablers were strong social support (social influences), sources of accountability (behavioural regulation) and experiencing benefit from prior use of treatment (reinforcement).
Interviews with T2DM health professionals
We identified six TDF domains that prominently influenced the behaviours of HPs to assess and treat knee OA. For all HPs, important barriers included not seeing joint pain as a priority (intention), perceived lack of programmes to which they could refer their patients (environmental context and resources), insufficient knowledge and skills to assess OA, particularly for endocrinologists and diabetes educators (knowledge, skills), belief that it was not within their professional role to address OA (professional role and identity) and that other physicians would not want to receive a referral for OA care (social influences).
Interviews with AREP arthritis therapists
We identified five TDF domains that were relevant to the ATs’ behaviour to consider T2DM when formulating a knee OA management plan. ATs’ perceived lack of specific knowledge around comorbidities including T2DM (knowledge); there was a lack of breadth in skills in behavioural change techniques to help patients set and reach their goals, particularly when it came to physical activity (skills); therapists generally had no intention for a patient’s comorbidity profile to influence their treatment recommendations (intention); they saw their role as joint focused (professional role and identity); and lack of a formalized follow-up structure of the current Arthritis Society Canada AREP programme limited sufficient patient monitoring and follow-up (environmental context and resources).
Step 3: Which intervention components (behaviour change techniques and mode(s) of delivery) could overcome the modifiable barriers and enhance the enablers?
Identify potential behavioural change techniques and modes of delivery to overcome barriers and enhance the enablers
Our initial list of BCTs, at each of the patient; HP; and AT levels, is shown in Additional file 1: Table A.
Identify what is likely to be feasible, locally relevant and acceptable and combine identified components into an acceptable intervention that can be delivered
At our first UAP meeting, there was a broad agreement with qualitative findings and support for leveraging the Arthritis Society Canada AREP programme infrastructure as a vehicle to provide OA care. UAP members suggested the following ideas to operationalize BCTs and optimize modes of delivery: development of simple ways T2DM clinicians could screen for OA, improving diabetes HPs awareness around the impact of OA, different ways to provide T2DM patients with guidance about exercise for OA and use of diabetes flow sheets to prompt discussion about reasons for physical inactivity, including inquiring about OA. Based on this discussion, we refined our list of BCTs and excluded those deemed outside the scope of the study or not feasible. Our selected operationalizable BCTs, within each domain and mode of delivery, targeting patient, diabetes HP and AT level, are summarized in Additional file 1: Table A.
At the second UAP meeting, all members supported our intervention sketch. In particular, stakeholders from Arthritis Society Canada supported adapting the existing AREP model to deliver longitudinal OA care. There was a widespread interest in ensuring that access to the intervention would be equitable for all and not rely on the need for advanced technology, and therefore, we removed some elements of the proposed intervention that centred around digital technologies. There was however interest in ensuring flexibility in how care was delivered to take into account patient preferences and so designed the intervention to be delivered in-person or virtually (telephone and/or video visits).
There were two main steps of the draft intervention. The first step involved screening for and identification of symptomatic knee OA within diabetes care, with referral to Arthritis Society Canada AREP in those identified as having suspected or confirmed OA for further evaluation and care. The second step involved a longitudinal treatment programme over 4 months delivered by AREP ATs, comprising one-on-one individualized OA management within the context of T2DM and including a focus on supporting the behaviour change requirement to increasing aerobic physical activity. We named this the Arthritis Society Diabetes & Osteoarthritis Program.
During small group meetings, reviewing detailed intervention components, patient partners described that an early check-in would help to support engagement with OA care through promoting accountability and allowing early troubleshooting to take place if any barriers arose. Several physicians emphasized the need to provide communication from the OA programme back to primary care and endocrinology so that care plans could be recognized and reinforced at those clinical encounters. We refined the intervention to incorporate these suggestions. We heard from AREP ATs about specific elements that would be required to support their delivery of OA care as part of the intervention, to prepare them for assessing and treating persons with T2DM and knee OA. We confirmed topics to be delivered in a 1-day workshop for ATs, drawn from results of the AT qualitative interviews, which included an overview of T2DM, behavioural change techniques and health coaching, wearables and technology that can be offered to support patients to meet physical activity goals and an update on the management of knee OA.
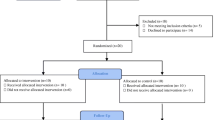
In Table 2, we show the final intervention components, including content and modes of delivery, mapped to the selected BCT and TDF domain being targeted. We organize this by group (patient, HP and AT); however, the order is not meant to convey the temporality or importance of a single group or behaviour. Intervention steps and major components are shown in Fig. 2.
Step 4: How can behaviour change be measured and understood?
Programme theory
We expect our intervention to work by enabling change in the behaviours of patients, diabetes HPs and ATs, as shown in our logic models (Fig. 3). For patients, our intervention will increase intention and motivation to engage in OA care, through both facilitating receipt of a diagnosis of OA and providing support for management. For HPs, it will increase the intention to screen for knee OA and refer for assessment and treatment when OA is suspected or confirmed. For ATs, through adapting the existing AREP programme and creating the Arthritis Society Diabetes & Osteoarthritis Program, we have created an environmental change to support the provision of individualized longitudinal care. This programme also shifts the focus in care from joint-specific therapeutic exercise to increase overall physical activity. We intend for there to be flexibility in the delivery of intervention components to allow for variation in practices of different diabetes HPs, including clinic resources, yet maintain the integrity of the core intervention components [45].
Logic models of the multi-level intervention for A patients, B health professionals and C arthritis therapists. Barriers and enablers according to the Theoretical Domains Framework (TDF) are mapped to behavioural change techniques and then proximal, feasibility and clinical outcomes. AT, Arthritis Therapist; BCT, behavioural change technique; HP, health professional; PA, physical activity; TDF; Theoretical Domains Framework
Discussion
In this paper, we describe the development phase of a multifaceted intervention to overcome barriers to the assessment and diagnosis of OA in persons with T2DM. The TOP-DM intervention promotes evidence-based OA treatment with a focus on physical activity, including the mechanisms to support the behaviour change this requires, given its importance in both T2DM and OA care. We expect our intervention to work by enabling change in behaviours of patients, diabetes HPs and ATs and have targeted multiple groups given the complexity of this health challenge. In keeping with MRC guidance [45], our intervention development process has incorporated theory, in this case, of behaviour change [64], existing evidence and stakeholder involvement, while considering local context, to maximize the likelihood of success. The final intervention brings together a range of components that were specifically developed in the context of concomitant T2DM. Some of the components are similar to those incorporated in prior knee OA interventions, including strategies to screen for knee OA [43], increase health professional knowledge [65, 66], provide patient education [67, 68] and improve uptake of physical activity through health professional support [42].
We involved multiple stakeholders in a co-design process, to develop our intervention alongside those for whom it is designed [49,50,51]. Our UAP brought together patient partners, Arthritis Society Canada and diverse HPs, in a focus group-like setting where concepts could be tackled from many important perspectives. Given the focus on implementation in the context of multiple chronic conditions, this involved a large number of individuals. One lesson learned was that when bringing a large group together, any one individual could get relatively little “air time”. To address this, we also engaged stakeholders (patients, Arthritis Society Canada and HPs) individually or in small stakeholder groups to allow sufficient time to garner their inputs and to mitigate any possible hierarchal dynamics that might prevent individuals from expressing their views. Teams undertaking implementation research should carefully consider the modes in which they plan to engage stakeholders [69].
Strengths of this work include the use of a systematic step-wise approach [47]. Through the use of theory, and linking identified barriers to health behaviour to relevant and effective BCTs, we have explicitly outlined how we expect our intervention to work, and we will be able to evaluate these proposed mechanisms of change in future work. With our transdisciplinary approach, including collaborating with end-users and community stakeholders throughout the research process, we have sought to enhance the potential feasibility and effectiveness of our intervention [70, 71]. This work fills an important gap. To our knowledge, our intervention is one of only a few seeking to increase the identification and diagnosis of individuals with symptomatic knee OA to facilitate care, and none to our knowledge has done so within the context of another complex chronic condition. Our work to integrate OA care within T2DM complex chronic disease management is in an effort to break down the current, mostly siloed, models of chronic disease care. Our intervention leverages the existing Arthritis Society Canada AREP infrastructure and provincial funding, supporting potential intervention spread, scalability and sustainability.
Our work has some limitations. First, this approach to intervention development requires significant time and resources. While explicit use of theory has several advantages, including helping to inform important intervention elements [72], the evidence base to support that theory-informed interventions are superior to those not based on theory is sparse, largely due to the challenges of empirically addressing this question [73]. Multiple theories and frameworks of individual and organizational behaviour change exist, with little consensus on how to optimally select one [74]. We selected the TDF as it is recognized as the most comprehensive framework for designing implementation interventions [47]; however, other frameworks or theories can be used. While we sought to bridge the distance between OA and T2DM care, we expect many patients to have additional chronic conditions that may present additional barriers to OA care that were not explicitly addressed through this intervention. Our intervention may have limited generalizability given the use of AREP, as other jurisdictions may not have a similar infrastructure.
Conclusions
In conclusion, using a systematic process combining theory, stakeholder involvement and existing evidence, we have developed a complex implementation intervention to improve OA care in persons with T2DM with the goal to improve both OA and T2DM outcomes and optimize overall health and well-being. While we have used robust methods in development, our next steps include assessment of proximal and feasibility outcomes using rapid-cycle change quality improvement methods and engaging potential intervention users to inform refinements to our intervention before evaluation of both feasibility and effectiveness outcomes in a pilot cluster randomized clinical trial.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- AACTT:
-
Action, Actor, Context, Target, Time framework
- APEASE:
-
Acceptability, Practicability, Effectiveness, Affordability, Side-effects, and Equity criteria
- AREP:
-
Arthritis Rehabilitation and Education Program
- AT:
-
Arthritis therapist
- BCT:
-
Behavioural change technique
- GLA:D:
-
GoodLife with osteoArthritis in Denmark
- HP:
-
Health professional
- MRC:
-
UK Medical Research Council
- OA:
-
Osteoarthritis
- T2DM:
-
Type 2 diabetes
- TiDieR:
-
Template for Intervention Description and Replication Checklist
- TDF:
-
Theoretical Domains Framework
- TOP-DM:
-
Treatment of Knee Osteoarthritis in Persons with Diabetes Mellitus
- UAP:
-
User advisory panel
References
Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388:1545–602.
Hawker GA, Croxford R, Bierman AS, Harvey PJ, Ravi B, Stanaitis I, et al. All-cause mortality and serious cardiovascular events in people with hip and knee osteoarthritis: a population based cohort study. PLoS ONE. 2014;9:e91286.
Kendzerska T, King LK, Lipscombe L, Croxford R, Stanaitis I, Hawker G. The impact of hip and knee osteoarthritis on the subsequent risk of incident diabetes: a population-based cohort study. Diabetologia. 2018;61:2290–9.
Hawker GA, Croxford R, Bierman AS, Harvey P, Ravi B, Kendzerska T, et al. Osteoarthritis-related difficulty walking and risk for diabetes complications. Osteoarthritis Cartilage. 2017;25:67–75.
Zheng S, Tu L, Cicuttini F, Zhu Z, Han W, Antony B, et al. Depression in patients with knee osteoarthritis: risk factors and associations with joint symptoms. BMC Musculoskelet Disord. 2021;22:40.
Kendzerska T, Juni P, King LK, Croxford R, Stanaitis I, Hawker GA. The longitudinal relationship between hand, hip and knee osteoarthritis and cardiovascular events: a population-based cohort study. Osteoarthritis Cartilage. 2017;25:1771–80.
Innes KE, Sambamoorthi U. The association of osteoarthritis and related pain burden to incident Alzheimer’s disease and related dementias: a retrospective cohort study of U.S. Medicare beneficiaries. J Alzheimers Dis. 2020;75:789–805.
Kiadaliri A, Englund M. Osteoarthritis and risk of hospitalization for ambulatory care-sensitive conditions: a general population-based cohort study. Rheumatology (Oxford). 2021;60:4340–7.
Quiñones AR, Markwardt S, Botoseneanu A. Diabetes-multimorbidity combinations and disability among middle-aged and older adults. J Gen Intern Med. 2019;34:944–51.
Swain S, Sarmanova A, Coupland C, Doherty M, Zhang W. Comorbidities in osteoarthritis: a systematic review and meta-analysis of observational studies. Arthritis Care Res. 2020;72:991–1000.
Louati K, Vidal C, Berenbaum F, Sellam J. Association between diabetes mellitus and osteoarthritis: systematic literature review and meta-analysis. RMD Open. 2015;1:e000077.
Veronese N, Cooper C, Reginster JY, Hochberg M, Branco J, Bruyère O, et al. Type 2 diabetes mellitus and osteoarthritis. Semin Arthritis Rheum. 2019;49:9–19.
Centers for Disease Control and Prevention (CDC). Arthritis as a potential barrier to physical activity among adults with diabetes--United States, 2005 and 2007. MMWR Morb Mort Wkly Rep. 2008;57:486–9.
Sigal RJ, Armstrong MJ, Bacon SL, Boule NG, Dasgupta K, Kenny GP, et al. Physical activity and diabetes. Can J Diabetes. 2018;42(Suppl 1):S54-s63.
King LK, Waugh E, McKay C, Stanaitis I, Stretton J, Weisman A, et al. 'It’s a dance between managing both': a qualitative study exploring perspectives of persons with knee osteoarthritis and type 2 diabetes mellitus on the impact of osteoarthritis on diabetes management and daily life. BMJ Open. 2022;2(11):061472.
Stuckey H, Peyrot M. Living with diabetes: literature review and secondary analysis of qualitative data. Diabet Med. 2020;37:493–503.
Bannuru RR, Osani MC, Vaysbrot EE, Arden N, Bennell K, Bierma-Zeinstra SMA, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27:1578–89.
King LK, Marshall DA, Faris P, Woodhouse LJ, Jones CA, Noseworthy T, et al. Use of recommended non-surgical knee osteoarthritis management in patients prior to total knee arthroplasty: a cross-sectional study. J Rheumatol. 2020;47:1253–60.
Yu D, Jordan KP, Peat G. Underrecording of osteoarthritis in United Kingdom primary care electronic health record data. Clin Epidemiol. 2018;10:1195–201.
Jackson H, Barnett LA, Jordan KP, Dziedzic KS, Cottrell E, Finney AG, et al. Patterns of routine primary care for osteoarthritis in the UK: a cross-sectional electronic health records study. BMJ Open. 2017;7:e019694.
Edwards JJ, Jordan KP, Peat G, Bedson J, Croft PR, Hay EM, et al. Quality of care for OA: the effect of a point-of-care consultation recording template. Rheumatology. 2014;54:844–53.
Christiansen MB, White DK, Christian J, Waugh E, Gakhal N, King L, et al. “It … doesn’t always make it [to] the top of the list”: primary care physicians’ experiences with prescribing exercise for knee osteoarthritis. Can Fam Physic. 2020;66:e14–20.
Egerton T, Diamond LE, Buchbinder R, Bennell KL, Slade SC. A systematic review and evidence synthesis of qualitative studies to identify primary care clinicians’ barriers and enablers to the management of osteoarthritis. Osteoarthritis Cartilage. 2017;25:625–38.
Rosemann T, Wensing M, Joest K, Backenstrass M, Mahler C, Szecsenyi J. Problems and needs for improving primary care of osteoarthritis patients: the views of patients, general practitioners and practice nurses. BMC Musculoskelet Disord. 2006;7:48.
Kraus VB, Sprow K, Powell KE, Buchner D, Bloodgood B, Piercy K, et al. Effects of physical activity in knee and hip osteoarthritis: a systematic umbrella review. Med Sci Sports Exerc. 2019;51:1324–39.
Hurley M, Dickson K, Hallett R, Grant R, Hauari H, Walsh N, et al. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database Syst Rev. 2018;4:Cd010842.
Grembowski D, Schaefer J, Johnson KE, Fischer H, Moore SL, Tai-Seale M, et al. A conceptual model of the role of complexity in the care of patients with multiple chronic conditions. Med Care. 2014;52(Suppl 3):S7–14.
Tan BY, Thach T, Munro YL, Skou ST, Thumboo J, Car J, et al. Complex lifestyle and psychological intervention in knee osteoarthritis: scoping review of randomized controlled trials. Int J Environ Res Public Health. 2021;18:12757.
Allen KD, Oddone EZ, Coffman CJ, Datta SK, Juntilla KA, Lindquist JH, et al. Telephone-based self-management of osteoarthritis: a randomized trial. Ann Intern Med. 2010;153:570–9.
Bennell KL, Lawford BJ, Keating C, Brown C, Kasza J, Mackenzie D, et al. Comparing video-based, telehealth-delivered exercise and weight loss programs with online education on outcomes of knee osteoarthritis. Ann Intern Med. 2021;175:198–209.
Baker K, LaValley MP, Brown C, Felson DT, Ledingham A, Keysor JJ. Efficacy of computer-based telephone counseling on long-term adherence to strength training in elderly patients with knee osteoarthritis: a randomized trial. Arthritis Care Res. 2020;72:982–90.
Wang L, Chen H, Lu H, Wang Y, Liu C, Dong X, et al. The effect of transtheoretical model-lead intervention for knee osteoarthritis in older adults: a cluster randomized trial. Arthritis Res Ther. 2020;22:134.
Nelligan RK, Hinman RS, Kasza J, Crofts SJC, Bennell KL. Effects of a self-directed web-based strengthening exercise and physical activity program supported by automated text messages for people with knee osteoarthritis: a randomized clinical trial. JAMA Intern Med. 2021;181:776–85.
Kloek CJJ, Bossen D, Spreeuwenberg PM, Dekker J, de Bakker DH, Veenhof C. Effectiveness of a blended physical therapist intervention in people with hip osteoarthritis, knee osteoarthritis, or both: a cluster-randomized controlled trial. Phys Ther. 2018;98:560–70.
Bennell KL, Nelligan R, Dobson F, Rini C, Keefe F, Kasza J, et al. Effectiveness of an Internet-delivered exercise and pain-coping skills training intervention for persons with chronic knee pain. Ann Intern Med. 2017;166:453–62.
Bennell KL, Ahamed Y, Jull G, Bryant C, Hunt MA, Forbes AB, et al. Physical therapist-delivered pain coping skills training and exercise for knee osteoarthritis: randomized controlled trial. Arthritis Care Res. 2016;68:590–602.
Preece SJ, Brookes N, Williams AE, Jones RK, Starbuck C, Jones A, et al. A new integrated behavioural intervention for knee osteoarthritis: development and pilot study. BMC Musculoskelet Disord. 2021;22:526.
Hinman RS, Campbell PK, Lawford BJ, Briggs AM, Gale J, Bills C, et al. Does telephone-delivered exercise advice and support by physiotherapists improve pain and/or function in people with knee osteoarthritis? Telecare randomised controlled trial. Br J Sports Med. 2020;54:790–7.
Bennell K, Nelligan RK, Schwartz S, Kasza J, Kimp A, Crofts SJ, et al. Behavior change text messages for home exercise adherence in knee osteoarthritis: randomized trial. J Med Internet Res. 2020;22:e21749e.
Thorstensson CA, Garellick G, Rystedt H, Dahlberg LE. Better management of patients with osteoarthritis: development and nationwide implementation of an evidence-based supported osteoarthritis self-management programme. Musculoskeletal Care. 2015;13:67–75.
Allen KD, Woolson S, Hoenig HM, Bongiorni D, Byrd J, Caves K, et al. Stepped exercise program for patients with knee osteoarthritis: a randomized controlled trial. Ann Intern Med. 2021;174:298–307.
Skou ST, Roos EM. Good Life with osteoArthritis in Denmark (GLA:D™): evidence-based education and supervised neuromuscular exercise delivered by certified physiotherapists nationwide. BMC Musculoskelet Disord. 2017;18:72.
Marra CA, Cibere J, Grubisic M, Grindrod KA, Gastonguay L, Thomas JM, et al. Pharmacist-initiated intervention trial in osteoarthritis: a multidisciplinary intervention for knee osteoarthritis. Arthritis Care Res. 2012;64:1837–45.
Bossen D, Buskermolen M, Veenhof C, de Bakker D, Dekker J. Adherence to a web-based physical activity intervention for patients with knee and/or hip osteoarthritis: a mixed method study. J Med Internet Res. 2013;15(10):e223.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ (Clinical research ed). 2021;374:n2061.
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ (Clinical research ed). 2008;337:a1655.
French SD, Green SE, O’Connor DA, McKenzie JE, Francis JJ, Michie S, et al. Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci. 2012;7:38.
Arthritis Society Canada. Arthritis Rehabilitation and Education Program. https://arthritis.ca/support-education/support-in-your-community/arthritis-rehabilitation-and-education-program-(ar. Accessed 30 Aug 2022.
Harte R, Quinlan LR, Glynn L, Rodríguez-Molinero A, Baker PM, Scharf T, et al. Human-centered design study: enhancing the usability of a mobile phone app in an integrated falls risk detection system for use by older adult users. JMIR Mhealth Uhealth. 2017;5(5):e71.
McCurdie T, Taneva S, Casselman M, Yeung M, McDaniel C, Ho W, et al. mHealth consumer apps: the case for user-centered design. Biomed Instrum Technol. 2012;46:49–56.
Portalupi LB, Lewis CL, Miller CD, Whiteman-Jones KL, Sather KA, Nease DE Jr, et al. Developing a patient and family research advisory panel to include people with significant disease, multimorbidity and advanced age. Fam Pract. 2017;34:364–9.
Riordan F, Racine E, Phillip ET, Bradley C, Lorencatto F, Murphy M, et al. Development of an intervention to facilitate implementation and uptake of diabetic retinopathy screening. Implement Sci. 2020;15:34.
King LK, Krystia O, Waugh EJ, MacKay C, Stanaitis I, Stretton J, et al. Barriers and enablers to health care providers assessment and treatment of knee osteoarthritis in persons with type 2 diabetes mellitus: a qualitative study using the Theoretical Domains Framework. Osteoarthritis Cartilage Open. 2022;4(4):100299.
King LK, Krystia O, Waugh EJ, MacKay C, Stanaitis I, Stretton J, et al. Understanding the behavioural determinants of seeking and engaging in care for knee osteoarthritis in persons with type 2 diabetes mellitus: a qualitative study using the theoretical domains framework. Osteoarthritis Cartilage Open. 2022;4(4):100305.
King LK, Waugh EJ, MacKay C, Stanaitis I, Krystia O, Stretton J, et al. Formulating knee osteoarthritis management plans taking type 2 diabetes into account: qualitative study of arthritis therapists using theoretical domains framework. J Rheumatol. 2022;9(12):1365–1.
Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37.
Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12:77.
Michie S, Johnston M, Rothman AJ, de Bruin M, Kelly MP, Carey RN, et al. Health services and delivery research. Developing an evidence-based online method of linking behaviour change techniques and theoretical mechanisms of action: a multiple methods study. Southampton: NIHR Journals Library; 2021.
Carey RN, Connell LE, Johnston M, Rothman AJ, de Bruin M, Kelly MP, et al. Behavior change techniques and their mechanisms of action: a synthesis of links described in published intervention literature. Ann Behav Med. 2019;53:693–707.
Michie S, Atkins L, West R. The behaviour change wheel: a guide to designing interventions. London: Silverback Publishing; 2014.
International Diabetes Federation. Recommendations for managing type 2 diabetes in primary care, 2017. www.idf.org/managing-type2-diabetes. Accessed 30 Aug 2022.
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ (Clinical research ed). 2014;348:g1687.
Presseau J, McCleary N, Lorencatto F, Patey AM, Grimshaw JM, Francis JJ. Action, Actor, Context, Target, Time (AACTT): a framework for specifying behaviour. Implement Sci. 2019;14:102.
Davis R, Campbell R, Hildon Z, Hobbs L, Michie S. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychol Rev. 2015;9:323–44.
Dziedzic KS, Healey EL, Porcheret M, Afolabi EK, Lewis M, Morden A, et al. Implementing core NICE guidelines for osteoarthritis in primary care with a model consultation (MOSAICS): a cluster randomised controlled trial. Osteoarthritis Cartilage. 2018;26:43–53.
Østerås N, Blaker IB, Hjortland T, Cottrell E, Quicke JG, Dziedzic KS, et al. Improving osteoarthritis management in primary healthcare: results from a quasi-experimental study. BMC Musculoskelet Disord. 2021;22:79.
Smink AJ, Bierma-Zeinstra SM, Schers HJ, Swierstra BA, Kortland JH, Bijlsma JW, et al. Non-surgical care in patients with hip or knee osteoarthritis is modestly consistent with a stepped care strategy after its implementation. Int J Qual Health Care. 2014;26:490–8.
Allen KD, Oddone EZ, Coffman CJ, Jeffreys AS, Bosworth HB, Chatterjee R, et al. Patient, provider, and combined interventions for managing osteoarthritis in primary care: a cluster randomized trial. Ann Intern Med. 2017;166:401–11.
Concannon TW, Grant S, Welch V, Petkovic J, Selby J, Crowe S, et al. Practical guidance for involving stakeholders in health research. J Gen Intern Med. 2019;34:458–63.
van Meijel B, Gamel C, van Swieten-Duijfjes B, Grypdonck MH. The development of evidence-based nursing interventions: methodological considerations. J Adv Nurs. 2004;48:84–92.
Leask CF, Sandlund M, Skelton DA, Altenburg TM, Cardon G, Chinapaw MJM, et al. Framework, principles and recommendations for utilising participatory methodologies in the co-creation and evaluation of public health interventions. Res Involv Engagem. 2019;5:2.
The Improved Clinical Effectiveness through Behavioural Research G. Designing theoretically-informed implementation interventions. Implement Sci. 2006;1:4.
O’Cathain A, Croot L, Duncan E, Rousseau N, Sworn K, Turner KM, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9:e029954.
Birken SA, Powell BJ, Shea CM, Haines ER, Alexis Kirk M, Leeman J, et al. Criteria for selecting implementation science theories and frameworks: results from an international survey. Implement Sci. 2017;12:124.
Acknowledgements
We would like to acknowledge and thank the members of our user advisory panel for providing their feedback and assistance during the intervention development process and to Linda Li, Leigh Caplan and Gloria Lourido for their contributions to this project. We also would like to recognize the Community Care Support Services, Ontario Health Central, that provides support for AREP.
Funding
This study was funded by a Project Grant from the Canadian Institutes of Health Research (CIHR). The funder had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; or the decision to submit the manuscript for publication. Lauren King is supported by a CIHR doctoral research award and the University of Toronto Department of Medicine Eliot Phillipson Clinician Scientist Training Program.
Author information
Authors and Affiliations
Contributions
LKK and GAH conceived the study. LKK, NMI, EJW, CM, IS, OK, JS, SM, AW, ZB, SR, SB, MS, TS, NG, PA, JP, LL and GAH contributed to the study design. LKK and EJW contributed to the data collection. LKK, EJW, CM, IS and OK were involved in the data analysis. LKK drafted the article. All authors critically revised the article and approved the final version for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the Research Ethics Boards at Women’s College Hospital (2019–0170-E) and University of Toronto (#00039525). All participants provided written or oral informed consent.
Consent for publication
Not applicable.
Competing interests
Gillian Hawker has received research support as the Sir John and Lady Eaton Professor and Chair of Medicine, Department of Medicine, University of Toronto. Lorraine Lipscombe receives salary support as the Director of the Novo Nordisk Network for Healthy Populations, University of Toronto. Susan Ross and Shawn Brady are employees of the Arthritis Society Canada. All other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table A.
Our initial list of behavioural change techniques (BCTs), mapped to each relevant theoretical domains framework (TDF) domain for A) Patients, B) Health professionals, and C) Arthritis therapists with either a confirmed link or inconclusive evidence for a link according to the Theory and Technique Tool (https://theoryandtechniquetool.humanbehaviourchange.org/) (70). Those in bold font indicates the BCTs selected in the research process as potentially operationalizable and feasible.
Additional file 2: Table B.
Interview Guide: Patients with Diabetes and Osteoarthritis. Table C. Interview Guide: Physicians and Diabetes Educators. Table D. Interview Guide: Arthritis Therapists.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
King, L.K., Ivers, N.M., Waugh, E.J. et al. Improving diagnosis and treatment of knee osteoarthritis in persons with type 2 diabetes: development of a complex intervention. Implement Sci Commun 4, 20 (2023). https://doi.org/10.1186/s43058-023-00398-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43058-023-00398-3