Abstract
Aims/hypothesis
This study examined the relationship between hip/knee osteoarthritis and incident diabetes. We hypothesised that hip/knee osteoarthritis would be independently related to an increased risk of incident diabetes and that this relationship would be due, at least in part, to walking difficulty. We also hypothesised a stronger relationship with incident diabetes for knee than hip osteoarthritis because of the higher prevalence in the former of obesity/the metabolic syndrome.
Methods
A population cohort aged ≥55 years recruited from 1996 to 1998 was followed through provincial health administrative data to 2014. Participants with baseline diabetes were excluded. Hip/knee osteoarthritis was defined as swelling, pain or stiffness in any joint lasting 6 weeks in the past 3 months and indication on a joint homunculus that a hip/knee was ‘troublesome’. Walking limitation was defined as self-reported difficulty standing or walking in the last 3 months (yes/no). Using Cox regressions, we examined the relationship of baseline hip/knee osteoarthritis with incident diabetes as defined from health administrative data, controlling for age, sex, BMI, income, prior hypertension, cardiovascular disease and primary care exposure. We tested whether the observed effect was mediated through walking limitation.
Results
In total, 16,362 participants were included: median age 68 years and 61% female. Of these, 1637 (10%) individuals met the criteria for hip osteoarthritis, 2431 (15%) for knee osteoarthritis and 3908 (24%) for walking limitation. Over a median follow-up of 13.5 years (interquartile range 7.3–17.8), 3539 individuals (22%) developed diabetes. Controlling for confounders, a significant relationship was observed between number of hip/knee joints with osteoarthritis and incident diabetes: HR for two vs no osteoarthritic hips 1.25 (95% CI 1.08, 1.44); HR for two vs no osteoarthritic knees 1.16 (95% CI 1.04, 1.29). From 37% to 46% of this relationship was explained by baseline walking limitation.
Conclusions/interpretation
In a large population cohort aged ≥55 years who were free of diabetes at baseline, and controlling for confounders, the presence and burden of hip/knee osteoarthritis was a significant independent predictor of incident diabetes. This association was partially explained by walking limitation. Increased attention to osteoarthritis and osteoarthritis-related functional limitations has the potential to reduce diabetes risk.
Similar content being viewed by others

Introduction
Osteoarthritis and type 2 diabetes are common chronic health conditions that frequently co-occur [1, 2]. In meta-analyses performed by Louati and colleagues on 1,040,175 individuals, the risk of diabetes in people with osteoarthritis compared with individuals without osteoarthritis was 40% higher (unadjusted OR 1.41 [95% CI 1.21, 1.65; p < 0.001]) [1].
Potential explanations for the frequent coexistence of these two conditions include shared risk factors (ageing, obesity, lack of physical activity and socioeconomic disadvantages) [3, 4], common pathogenetic mechanisms (inflammation, oxidative stress and endothelial dysfunction) [5, 6] and the effects of osteoarthritis-related functional limitations on these diabetes risk factors (e.g. sedentary behaviour exacerbates the metabolic syndrome) [7,8,9]. Further, knee and hip osteoarthritis may have differential relationships with diabetes development. Specifically, obesity/the metabolic syndrome have been linked more strongly with knee osteoarthritis than hip osteoarthritis, whereas genetic factors affecting bone shape have been linked more strongly with hip osteoarthritis than knee osteoarthritis [10,11,12]. Given the relationship of diabetes incidence to obesity/the metabolic syndrome, one might expect the relationship between incident diabetes and knee osteoarthritis to be stronger, because of common risk factors, than the relationship with hip osteoarthritis.
However, current evidence of a causal relationship between osteoarthritis and diabetes is limited. Only two studies have investigated the longitudinal relationship between osteoarthritis and diabetes [13, 14]. Rahman and colleagues used physician claims and hospital discharge abstract data to identify people with osteoarthritis and incident diabetes from 1991 to 2009 [13]. Individuals with osteoarthritis were matched with control individuals without osteoarthritis by age, sex and year of administrative records. Over a mean follow-up of 12 years, the adjusted RRs for diabetes were significantly higher in most individuals with osteoarthritis, ranging from 1.16 to 1.27 for younger men and both younger and older women. Given the risk of misclassification bias using diagnostic codes that have not been validated to identify osteoarthritis and diabetes, this finding warrants confirmation. A second study, published in abstract form only, which used self-reported diabetes as the outcome, found no association [14].
In prior qualitative research [15,16,17] we identified that the high prevalence of comorbidities (e.g. hypertension) in people with osteoarthritis was a major barrier to osteoarthritis care. People with osteoarthritis tended to reduce their physical activity (i.e. moving, walking) to manage their osteoarthritis symptoms rather than use ‘risky painkillers’ that might exacerbate these conditions. Given that lack of physical activity is a known risk factor for diabetes and heart disease, we used existing data from a population cohort to examine the relationship between osteoarthritis and incident diabetes and to determine whether the relationship, if found, was explained by reduced mobility as measured by walking difficulty. We hypothesised that hip and knee osteoarthritis would be independently related to increased risk of incident diabetes and that this relationship would be due, at least in part, to walking difficulty. We also hypothesised a stronger relationship with incident diabetes for knee than hip osteoarthritis because of the higher prevalence in the former of obesity/the metabolic syndrome.
Methods
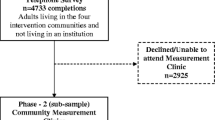
A population-based cohort study was conducted using linked data from a prospective community-based cohort followed from 1996 to 1998, and retrospectively collected provincial health administrative data from 1991 to 2014 (electronic supplementary material [ESM] Fig. 1).
Data sources
Information on demographics, self-reported height and weight, joint complaints, functional limitations and self-reported comorbidity was collected through a standardised mail/telephone survey (72.3% response rate) of all individuals aged 55+ years who lived in two regions of Ontario, Canada—one rural and one urban—between 1996 and 1998 [18]. These baseline data were linked to provincial health administrative databases housed at the Institute for Clinical Evaluative Sciences (ICES). Probabilistic matching (AUTOMATCH 4.022, 23) using the participant’s name, address, month/year of birth and sex was used to match the 28,451 survey respondents with records in Ontario’s healthcare registry, the Registered Persons Database, to obtain their unique health card numbers (HCNs). An encryption of the HCN was used to link the survey data with the ICES databases of interest. Overall, 25,388 of 28,451 individuals (89%) were successfully linked to provincial health administrative data.
The ICES data repository consists of high-quality individual-record-level coded and linkable longitudinal databases (www.ices.on.ca/Data-and-Privacy/ICES-data [accessed 7 June 2018]). It encompasses most publicly funded health services for the Ontario population (about 13 million people) eligible for universal health coverage since 1986. Legislation prohibits the private delivery of services covered under the Ontario Health Insurance Plan (OHIP), including laboratory testing (www.ontario.ca/page/what-ohip-covers [accessed 7 June 2018]). These databases include information on outpatient visits, discharge summaries of emergency department visits and hospital stays and, for those 65 years and older, medical drug claims to the Ontario Drug Benefit Program. The Registered Persons Database was used to document deaths. An additional database used for this analysis, the Ontario Diabetes Database (ODD), was developed to estimate population-based incidence and prevalence of diabetes in Ontario [19, 20]. Details on databases used and variables included are available from the ICES data repository at https://datadictionary.ices.on.ca/Applications/DataDictionary/Default.aspx (accessed 7 June 2018). These datasets were linked using unique, encoded identifiers and analysed at ICES.
The study was conducted in accordance with the Declaration of Helsinki and guidelines for good clinical practice, and was approved by the institutional ethics review boards at Sunnybrook Health Sciences Centre and Women’s College Hospital, Toronto, ON, Canada. ICES is a prescribed entity under section 45 of Ontario’s Personal Health Information Protection Act. Section 45 authorises ICES to collect personal health information, without consent, for the purposes of analysis and compiling statistical information about the health system. While data-sharing agreements prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria (available at www.ices.on.ca/DAS [accessed 7 June 2018]) for confidential access. The full dataset creation plan is available from the authors on request.
Study participants
Screening survey respondents who were unable to self-complete the screening questionnaire, who self-reported lower-limb amputation or wheelchair use, or with baseline rheumatic diseases (based on self-report or health administrative data) were excluded (ESM Fig. 2).
To define our diabetes-free cohort, we also excluded individuals with diabetes defined as: (1) physician-diagnosed diabetes based on the validated case definition from the ODD; (2) self-reported diabetes on the survey; or (3) use of diabetes medications (oral glucose-lowering agents or insulin) prescribed during a 1 year period prior to enrolment date.
Participant involvement
As noted above, this study was directly informed by prior qualitative research on participants with osteoarthritis (focus groups and one-to-one interviews) by our group [15,16,17].
Exposures
We defined symptomatic hip or knee osteoarthritis as: (1) self-reported swelling, pain or stiffness in any joint lasting ≥6 weeks in the past 3 months; and (2) indication on a joint homunculus that a hip or knee was ‘troublesome’. In a random subset of cohort participants with and without osteoarthritis, as we defined it, 96% met American College of Rheumatology (ACR) criteria for hip or knee osteoarthritis [21, 22] based on self-reported joint pain, age >50 years and findings on joint examination (sensitivity of 74% and specificity of 76%) (unpublished data, Principal Investigator: G. A. Hawker) and 66% met ACR criteria for hip or knee osteoarthritis based on joint pain and radiographs (sensitivity of 78% and specificity of 25%) [18]. Osteoarthritis burden was assessed by the number of hips or knees affected (0–2 for each of hip or knee osteoarthritis). In secondary analyses, we considered the total number of joints (knees or hips) affected by osteoarthritis as an exposure.
Outcomes
The primary outcome was time from baseline to incident physician-diagnosed diabetes derived from the ODD [19]. In this database, people with diabetes were identified using a validated algorithm as those having at least one hospitalisation or at least two outpatient visits bearing a diagnosis of diabetes within a 2 year period (sensitivity of 86%, specificity of 97% and positive predictive value of 80%) [19]. For validation, diagnostic data abstracted from the primary care charts (n = 3317) of 57 randomly selected physicians were linked to the administrative data cohort, and sensitivity and specificity were calculated. We considered the first service date as the incident diabetes date. Participants were followed from baseline to the end of March 2014 or the occurrence of the primary outcome or all-cause death, whichever occurred first.
Risk factors and confounders
Potential baseline risk factors and confounders considered were age, BMI and sex defined from clinical data, and hypertension, cardiovascular diseases (CVD) and neighbourhood income status defined from health administrative data [23, 24]. The severity of comorbidities at baseline was approximated using an aggregated score, the Johns Hopkins’ Aggregated Diagnosis Group (ADG) categories (using the Johns Hopkins ACG System, Version 10; https://www.hopkinsacg.org/). Other factors considered were location (rural vs urban region) and number of outpatient visits to primary care physicians in the 2 years prior to the baseline assessment as a measure of healthcare utilisation. Baseline walking limitation was considered a potential mediator of the relationship between osteoarthritis and incident diabetes. Walking limitation was defined as self-reported difficulty standing or walking in the last 3 months (yes/no). Details of definitions are provided in ESM Table 1.
Analyses
Baseline cohort characteristics were summarised overall, by presence of hip or knee osteoarthritis, and by outcome using means (SD), medians (interquartile range [IQR]) and proportions as appropriate. Unadjusted diabetes-free survival was estimated using the Kaplan–Meier method, and strata defined by the number of hips or knees affected (0–2 for each of hip or knee osteoarthritis) were compared using the logrank test.
For the primary analysis we used Cox proportional hazards regressions to assess the relationship between baseline self-reported knee or hip osteoarthritis, separately (by the number of hips or knees affected by osteoarthritis), and incident diabetes, controlling for covariates selected based on the literature review and expert opinion: age, BMI, sex, prior hypertension and CVD, income status, region and prior healthcare utilisation. Given potential differential relationships with incident diabetes, we considered hips and knees separately in our main analytic approach. The Cox proportional hazards regression assumptions for each variable were tested using traditional approaches [25]. Interactions between osteoarthritis, sex, age and BMI, specified a priori, were also evaluated. The main-effects-only models were compared with the full models that included interactions using likelihood ratio tests.
To investigate whether functional limitations explained the association between osteoarthritis and incident diabetes, we examined the effect of including walking limitation in our final models, and also separately assessed the effect of walking limitation on the risk of incident diabetes controlling for confounders. The interaction between functional limitation and affected joint (hip/knee) was tested to see if there was any evidence of a differential impact associated with the joint. To test if the observed association between hip or knee osteoarthritis and incident diabetes was mediated through walking limitation, we used the methods proposed by Lange and colleagues [26] and presented by Rochon and colleagues [27] to assess mediation in survival data. This approach is based on the counterfactual framework [28] and allows decomposition of the total effect of a given exposure A on the outcome Y into a natural direct effect (A → Y) and a natural indirect effect through a mediator M (A→M→Y). In the case of a time-to-event outcome Y, a binary exposure A, a binary mediator M and a number of baseline confounders C, Lange and colleagues showed that unbiased estimates for the direct and indirect effect may be obtained from Cox regression [26]. The corresponding code written in the R statistical programming language was used, as published by Rochon and colleagues [27].
To account for the competing risk of death, we also investigated the effect of hip/knee osteoarthritis and walking limitation on incident diabetes using Fine and Gray’s competing-risk regressions [29]. As we expected there to be high all-cause mortality in our population, death was considered as a competing event that might preclude individuals from being diagnosed with diabetes or alter the chances of observing it, resulting in a biased estimate of the risk of diabetes development as a standalone outcome [30].
Missing data were observed on income status (0.1%), height (18.0%) and weight (7.2%). To address missing values, we previously used two approaches: (1) considering missing baseline values as a ‘missing’ category; and (2) multivariate imputation by chained equations (details are presented in ESM Methods) [31, 32]. As the results were similar for both approaches [33], for uniform presentation, we used the first approach in the current study.
Analyses were conducted using R Version 3.1.2: a language and environment for statistical computing (www.r-project.org).
Results
Diabetes-free cohort
Of 25,388 individuals linked to provincial health administrative data to enable assessment of healthcare use from 1991 to 2014, 16,362 participants free of diabetes at baseline were included after applying exclusion criteria (ESM Fig. 2). Participants’ median baseline age was 68 years (IQR 61–75), 61% were female and median BMI was 25.3 kg/m2 (IQR 22.9–28.0) (Table 1). 1637 (10%) individuals met criteria for hip osteoarthritis, 2431 (15%) for knee osteoarthritis, and 3908 (24%) for walking limitation. Individuals with hip or knee osteoarthritis were more likely than those without osteoarthritis to be female with higher BMI, to live in a low-income quintile neighbourhood, to be hypertensive, to have comorbidities and to report walking limitation (Table 1).
Primary analyses
Over a median follow-up of 13.5 years (7.3–17.8), 3539 individuals (21.6%) experienced incident diabetes, giving an overall diabetes incidence in our cohort of 17.8 per 1000 person-years. Individuals who developed diabetes were more likely to be men living in a low-income area, to have higher BMI, to be hypertensive, and to have comorbidities and symptomatic knee and hip osteoarthritis with walking limitation (ESM Table 2).
In unadjusted analyses, individuals with knee or hip osteoarthritis were significantly more likely to develop diabetes (ESM Table 2). Diabetes-free survival at 10 years ranged from 85.9% (85.2–86.5) among individuals without knee osteoarthritis to 82.0% (79.9–84.2) in individuals with bilateral knee osteoarthritis (Fig. 1), and from 85.7% (85.1–86.3) among individuals without hip osteoarthritis to 80.8% (77.7–84.0) in individuals with bilateral hip osteoarthritis (Fig. 2). Diabetes-free survival at 15 years ranged from 75.8% (75.0–76.7) among individuals without knee osteoarthritis to 69.8% (67.1–72.5) in individuals with bilateral knee osteoarthritis (Fig. 1), and from 75.5% (74.7–76.3) among individuals without hip osteoarthritis to 68.1% (64.2–72.2) in individuals with bilateral hip osteoarthritis (Fig. 2). Compared with individuals with no hip/knee osteoarthritis, a dose–response relationship was observed between number of joints affected by knee/hip osteoarthritis and incident diabetes in the univariable model (ESM Table 2).
Unadjusted Kaplan–Meier estimates of diabetes-free survival by the number of joints affected by knee osteoarthritis with 95% CIs: solid line, no knee osteoarthritis (NKOA); dotted line, unilateral knee osteoarthritis (UKOA); dotted–dashed line, bilateral knee osteoarthritis (BKOA). The numbers at risk are presented below the x-axis
Unadjusted Kaplan–Meier estimates of diabetes-free survival by the number of joints affected by hip osteoarthritis with 95% CIs: solid line, no hip osteoarthritis (NHOA); dotted line, unilateral hip osteoarthritis (UHOA); dotted–dashed line, bilateral hip osteoarthritis (BHOA). The numbers at risk are presented below the x-axis
Controlling for baseline age, sex, income, BMI, pre-existing hypertension and CVD, region and prior primary care exposure, a significant dose–response relationship was observed between number of hip/knee joints with osteoarthritis and incident diabetes: HR for two vs no osteoarthritic hips 1.25 (95% CI 1.08, 1.44; p < 0.01); HR for two vs no osteoarthritic knees 1.16 (95% CI 1.04, 1.29; p < 0.01). Further adjustment for walking limitation resulted in attenuation of these relationships, which became non-significant (Table 2 and ESM Table 3). No significant improvement in model fit was observed between the main-effects-only models and full models with interactions. The interactions between osteoarthritis and walking limitation were not significant (p > 0.4 for both).
Taking into account the baseline confounders included in the full model, the overall adjusted HR of incident diabetes associated with the presence of hip or knee osteoarthritis was 1.16 (95% CI 1.07, 1.26). The proportion of individuals who reported walking limitation was 61% in individuals with hip or knee osteoarthritis and 15% in those without any hip or knee osteoarthritis (adjusted OR 8.28 [95% CI 7.56, 9.06]). The total HR of 1.16 was decomposed into a direct HR of 1.10 and an indirect HR of 1.05, which corresponds to the mediator effect. This suggests that about 37% of the effect of hip or knee osteoarthritis on incident diabetes was mediated by difficulty walking. Applying similar statistical techniques, about 37% of the effect of bilateral hip osteoarthritis and 46% of the effect of bilateral knee osteoarthritis was mediated by difficulty walking.
Secondary analyses
When the number of joints (0 to 4) affected by osteoarthritis was considered as an ordinal variable, we found that risk of incident diabetes increased with each additional joint affected: HR per one joint 1.06 (95% CI 1.02, 1.09; p < 0.01) (Table 2).
Among 8164 individuals who died in follow-up, 6690 (81.9%) died without developing diabetes and 1474 died after developing diabetes. When analysed using a competing-risk approach, after further adjustment of the full model for walking limitation, the relationship between bilateral hip/knee osteoarthritis and diabetes remained significant (adjusted HR for bilateral hip osteoarthritis vs none, 1.21 [95% CI 1.04, 1.41]; adjusted HR for bilateral knee osteoarthritis vs none, 1.14 [95% CI 1.02, 1.28]) (ESM Table 4).
Discussion
In a large population cohort aged ≥55 years and free of diabetes at baseline, bilateral hip or knee osteoarthritis was associated with a 16–25% increased hazard of developing incident diabetes after controlling for known risk factors. A dose–response relationship was observed; individuals with a higher number of affected hips or knees experienced a higher risk for developing diabetes. From 37% to 46% of this relationship was explained by walking limitation at baseline. The effects of hip/knee osteoarthritis were consistent in a model adjusting for the competing risk of all-cause mortality. These findings provide compelling evidence to suggest that hip/knee osteoarthritis is a clinically relevant and potentially modifiable risk factor for the development of type 2 diabetes.
The overall diabetes incidence in our cohort of 17.8 per 1000 person-years is at the upper limits of prior population estimates. Incidence rates of diabetes among individuals aged 55 years and older in Canada in 2008/09 ranged between 11.2 (55–59 years) and 17.9 (75–79 years) per 1000 individuals [34]. The diabetes incidence was significantly higher among those with hip or knee osteoarthritis (21.3 per 1000 person-years).
Our results are consistent with those of Rahman and colleagues and with proposed pathophysiological mechanisms linking osteoarthritis to diabetes [13]. However, contrary to our hypothesis, walking limitation explained only 37% of the effect of bilateral hip osteoarthritis and 46% of the effect of bilateral knee osteoarthritis on incident diabetes, suggesting that factors other than functional limitation play an important role. Among other factors, chronic inflammation and pain from osteoarthritis may play a significant role in diabetes development. Low-grade inflammation has been shown to be associated with insulin resistance and diabetes development [5]. Further, individuals with progressively painful osteoarthritis may restrict weight-bearing activities, including walking, to manage their symptoms, contributing to weight gain and sedentary behaviour and thus risk for diabetes.
Future prospective studies and, ultimately, clinical trials are needed to confirm the effects of symptomatic hip/knee osteoarthritis on diabetes development [35]. Clinical trials to elucidate the impact of interventions designed to reduce osteoarthritis pain and disability, such as with therapeutic exercise, biomechanical interventions [36], topical non-steroidal anti-inflammatory drugs (NSAIDs), duloxetine and, ultimately, joint replacement surgery, on diabetes development should be considered.
Study strengths include reliance on a large population cohort, long and near complete follow-up, use of a validated case definition for our outcome using health administrative data and validated measures of self-reported hip/knee osteoarthritis and disability, careful control for known risk factors for diabetes development and use of a competing-risk approach to account for the competing risk of death. Thus, we believe our findings are generalisable to the broader population of older adults living with osteoarthritis.
Some study limitations should be noted. First, as in all observational studies, there is the potential effect of unmeasured confounders (e.g. lack of information on physical activity, diet, smoking status, ethnic group or a family history of diabetes) [23, 24]. We did not adjust for changes over time in osteoarthritis symptom severity or other covariates, as we were interested in the effect of presence of hip or knee osteoarthritis at baseline on incident diabetes. The presence of walking limitation was self-reported, which may over- or underestimate an individual capacity; however, concordance between self-reported and performance-based measures of mobility is high [37]. Further, we were unable to distinguish between type 2 and type 1 diabetes using the ODD. However, given the age of our cohort we expect the vast majority of diabetes to be type 2. Although we used validated algorithms to define incident diabetes and prior comorbidities from health administrative data, these algorithms are characterised by certain specificity and sensitivity resulting in possible misclassification bias. If differential, this bias could go in either direction, while if non-differential, the estimated effect of osteoarthritis on incident diabetes is more likely to fall below the true value [38, 39]. There is also potential for misclassification bias given the sensitivity/specificity of our osteoarthritis definition [40].
In a large population cohort aged ≥55 years free of diabetes at baseline and after controlling for multiple confounders, the presence and burden of hip and knee osteoarthritis was a significant independent predictor of incident diabetes. This association was explained in part by osteoarthritis-related walking limitation. Increased attention to management of hip and knee osteoarthritis with a view to improving mobility has the potential to reduce risk of incident diabetes.
Data availability
While data-sharing agreements prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria (available at www.ices.on.ca/DAS [accessed 7 June 2018]) for confidential access. The full dataset creation plan is available from the authors on request.
Abbreviations
- ACR:
-
American College of Rheumatology
- ADG:
-
Johns Hopkins’ Aggregated Diagnosis Group
- CVD:
-
Cardiovascular disease
- HCN:
-
Unique health card number
- ICES:
-
Institute for Clinical Evaluative Sciences
- IQR:
-
Interquartile range
- ODD:
-
Ontario Diabetes Database
References
Louati K, Vidal C, Berenbaum F, Sellam J (2015) Association between diabetes mellitus and osteoarthritis: systematic literature review and meta-analysis. RMD Open 1:e000077
Williams MF, London DA, Husni EM, Navaneethan S, Kashyap SR (2016) Type 2 diabetes and osteoarthritis: a systematic review and meta-analysis. J Diabetes Complicat 30:944–950
Piva SR, Susko AM, Khoja SS, Josbeno DA, Fitzgerald GK, Toledo FG (2015) Links between osteoarthritis and diabetes: implications for management from a physical activity perspective. Clin Geriatr Med 31:67–87
Centers for Disease Control and Prevention (2009) Arthritis as a potential barrier to physical activity among adults with heart disease—United States, 2005 and 2007. MMWR Morb Mortal Wkly Rep 58:165–169
Duncan BB, Schmidt MI, Pankow JS et al (2003) Low-grade systemic inflammation and the development of type 2 diabetes: the atherosclerosis risk in communities study. Diabetes 52:1799–1805
Berenbaum F, Eymard F, Houard X (2013) Osteoarthritis, inflammation and obesity. Curr Opin Rheumatol 25:114–118
Wang X, Hunter D, Xu J, Ding C (2015) Metabolic triggered inflammation in osteoarthritis. Osteoarthr Cartil 23:22–30
Yoshimura N, Muraki S, Oka H, Kawaguchi H, Nakamura K, Akune T (2011) Association of knee osteoarthritis with the accumulation of metabolic risk factors such as overweight, hypertension, dyslipidemia, and impaired glucose tolerance in Japanese men and women: the ROAD study. J Rheumatol 38:921–930
Velasquez MT, Katz JD (2010) Osteoarthritis: another component of metabolic syndrome? Metab Syndr Relat Disord 8:295–305
Jiang L, Rong J, Wang Y et al (2011) The relationship between body mass index and hip osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine 78:150–155
Jiang L, Tian W, Wang Y et al (2012) Body mass index and susceptibility to knee osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine 79:291–297
Reijman M, Pols HA, Bergink AP et al (2007) Body mass index associated with onset and progression of osteoarthritis of the knee but not of the hip: the Rotterdam Study. Ann Rheum Dis 66:158–162
Rahman MM, Cibere J, Anis AH, Goldsmith CH, Kopec JA (2014) Risk of type 2 diabetes among osteoarthritis patients in a prospective longitudinal study. Int J Rheum: 620920
Cleveland R, Renner J, Jordan J, Callahan L (2017) Knee and hip OA as risk factors for development of CVD and diabetes in a community based longitudinal study. Osteoarthr Cartil 25:S192 (Abstract)
Hawker GA, Stewart L, French MR et al (2008) Understanding the pain experience in hip and knee osteoarthritis—an OARSI/OMERACT initiative. Osteoarthr Cartil 16:415–422
Gignac MA, Davis AM, Hawker G et al (2006) “What do you expect? You’re just getting older”: A comparison of perceived osteoarthritis-related and aging-related health experiences in middle- and older-age adults. Arthritis Rheum 55:905–912
Sale JE, Gignac M, Hawker G (2006) How “bad” does the pain have to be? A qualitative study examining adherence to pain medication in older adults with osteoarthritis. Arthritis Rheum 55:272–278
Hawker GA, Wright JG, Coyte PC et al (2001) Determining the need for hip and knee arthroplasty: the role of clinical severity and patients’ preferences. Med Care 39:206–216
Hux JE, Ivis F, Flintoft V, Bica A (2002) Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care 25:512–516
Lipscombe LL, Hux JE (2007) Trends in diabetes prevalence, incidence, and mortality in Ontario, Canada 1995-2005: a population-based study. Lancet 369:750–756
Altman R, Asch E, Bloch D et al (1986) Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 29:1039–1049
Altman R, Alarcon G, Appelrouth D et al (1991) The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum 34:505–514
Stiglic G, Pajnkihar M (2015) Evaluation of major online diabetes risk calculators and computerized predictive models. PLoS One 10:e0142827
Collins GS, Mallett S, Omar O, Yu LM (2011) Developing risk prediction models for type 2 diabetes: a systematic review of methodology and reporting. BMC Med 9:103
Harrell F (2001) Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. Springer, New York
Lange T, Vansteelandt S, Bekaert M (2012) A simple unified approach for estimating natural direct and indirect effects. Am J Epidemiol 176:190–195
Rochon J, du Bois A, Lange T (2014) Mediation analysis of the relationship between institutional research activity and patient survival. BMC Med Res Methodol 14:9
Pearl J (2009) Causality: models, reasoning, and inference, 2nd edn. Cambridge University Press, Cambridge
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Austin PC, Lee DS, Fine JP (2016) Introduction to the analysis of survival data in the presence of competing risks. Circulation 133:601–609
Azur MJ, Stuart EA, Frangakis C, Leaf PJ (2011) Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res 20:40–49
Rubin D (1987) Multiple imputation for nonresponse in surveys. Wiley, New York
Kendzerska T, Juni P, King LK, Croxford R, Stanaitis I, Hawker GA (2017) The longitudinal relationship between hand, hip and knee osteoarthritis and cardiovascular events: a population-based cohort study. Osteoarthr Cartil 25:1771–1780
Public Health Agency of Canada. Diabetes in Canada: Facts and figures from a public health perspective – Burden; Public Health Agency of Canada: 2011. Available from www.canada.ca/en/public-health/services/chronic-diseases/reports-publications/diabetes/diabetes-canada-facts-figures-a-public-health-perspective/chapter-1.html. Accessed 17 Jan 2018
Hawker GA, Gignac MA, Badley E et al (2011) A longitudinal study to explain the pain-depression link in older adults with osteoarthritis. Arthritis Care Res (Hoboken) 63:1382–1390
McAlindon TE, Bannuru RR, Sullivan MC et al (2014) OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr Cartil 22:363–388
Capistrant BD, Glymour MM, Berkman LF (2014) Assessing mobility difficulties for cross-national comparisons: results from the World Health Organization Study on Global AGEing and Adult Health. J Am Geriatr Soc 62:329–335
Brenner H, Gefeller O (1993) Use of the positive predictive value to correct for disease misclassification in epidemiologic studies. Am J Epidemiol 138:1007–1015
Wacholder S, Hartge P, Lubin JH, Dosemeci M (1995) Non-differential misclassification and bias towards the null: a clarification. Occup Environ Med 52:557–558
Braun HJ, Gold GE (2012) Diagnosis of osteoarthritis: imaging. Bone 51:278–288
Acknowledgements
The authors thank A. Wall (Department of Medicine, Women’s College Hospital, Canada) for her substantial role in cohort recruitment and project management. We also express our sincere thanks to all participants in the Ontario Hip and Knee Cohort, without whom this research could not have taken place. We thank IMS Brogan for use of their drug information database.
The severity of comorbidities at baseline was approximated using an aggregated score, the Johns Hopkins’ Aggregated Diagnosis Groups categories (The Johns Hopkins ACG® System, Version 10).
Some of the data were presented as an oral presentation at the 2016 ACR/Association of Rheumatology Health Professionals (ARHP) Annual Meeting (Washington, DC, 12-16 November 2016) and the 2017 Canadian Rheumatology Association (CRA) Annual Scientific Meeting & Arthritis Health Professions Association (AHPA) Annual Meeting (Ottawa, ON, Canada, 8-11 February 2017).
Funding
This study was funded by an operating grant from the Canadian Institutes of Health Research (grant #MOP-15468). The study was also supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). No endorsement by ICES or the Ontario MOHLTC is intended nor should be inferred. ICES had no role in the: design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; or decision to submit the report for publication. Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources and CIHI.
Author information
Authors and Affiliations
Contributions
All authors contributed to study design and interpretation of data. TK, RC and GAH were responsible for the statistical analysis. TK and GAH drafted the manuscript. All authors critically revised the manuscript for important intellectual content, read and approved the final manuscript and approved the decision to submit for publication. TK and GAH are the guarantors and had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis.
Corresponding author
Ethics declarations
GAH has received research support as the Sir John and Lady Eaton Professor and Chair of Medicine, Department of Medicine, University of Toronto. All other authors declare that there is no duality of interest associated with this manuscript.
Electronic supplementary material
ESM
(PDF 136 kb)
Rights and permissions
About this article
Cite this article
Kendzerska, T., King, L.K., Lipscombe, L. et al. The impact of hip and knee osteoarthritis on the subsequent risk of incident diabetes: a population-based cohort study. Diabetologia 61, 2290–2299 (2018). https://doi.org/10.1007/s00125-018-4703-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4703-2